Professional Documents
Culture Documents
Lap Lavage
Uploaded by
Mark SolimanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lap Lavage
Uploaded by
Mark SolimanCopyright:
Available Formats
ORIGINAL CONTRIBUTION
A Ten-Year Audit of Perforated Sigmoid Diverticulitis: Highlighting the Outcomes of Laparoscopic Lavage
Stephen I. White, M.B.B.S., F.R.A.C.S.1,2 Brett Frenkiel, B.B.Sc.3 Peter J. Martin, M.B.B.S., F.R.A.C.S.1,2
1 Department of General Surgery, The Tweed Hospital, Tweed Heads, New South Wales, Australia 2 Department of General Surgery, John Flynn Private Hospital, Tugun, Queensland, Australia 3 Bond University, Robina, Queensland, Australia
PURPOSE: This study was designed to review the results of laparoscopic lavage for the management of perforated sigmoid diverticulitis. METHODS: A 10-year retrospective review was conducted
further symptoms. Eleven patients were observed without further symptoms with a mean follow-up of 20 months (range, 6 60 mo).
CONCLUSIONS: Laparoscopic washout is an emerging
of 78 consecutive cases of sigmoid diverticulitis warranting emergency surgical intervention (1999 2008).
RESULTS: Hinchey grades were I (12 patients), II (31 patients), III (29 patients), and IV (6 patients). The patients mean age was 72 years. Procedures performed were laparoscopic washout (35), Hartmann procedure (31), percutaneous drainage of abscess (4), and resection and primary anastomosis (8). Overall mortality was 5 of 78 (7%); all of these patients were in the Hartmann group. Washout was successful in 27 of 35 cases, meaning recovery from the initial episode of peritonitis without resection. The short-term failures of washout in 8 patients were because of perforated cancer (1), fecal fistula formation (2), and inadequate washout and ongoing sepsis (5). In long-term follow-up, 8 patients in the washout group developed symptoms of recurrent complicated diverticulitis, including painful phlegmon (3), stricture (1), fistulas (3), and repeat perforation (1); all 8 patients underwent delayed resection. Eight patients underwent early planned resection without experiencing
technique that is particularly applicable to the management of Hinchey III perforated peritonitis. Shortand long-term problems exist with the technique that may be overcome with further improvement in technique and case selection. Resection and radiological drainage remain widely used in managing perforated sigmoid diverticulitis.
KEY WORDS: Laparoscopic washout; Hartmann;
Diverticulitis; Perforation. he management of perforated sigmoid diverticulitis has traditionally been immediate surgical resection. The current consensus statements and practice guidelines from the US1 and European2 organizations recommend Hartmann rectosigmoidectomy with end colostomy. However, diverticular perforations are variable by nature and the pathophysiology of perforation is poorly understood. In most resected cases, neither the surgeon nor pathologist can determine the actual site of perforationtherefore, is resection really necessary? In support of nonresection, in 1978 Hinchey et al3 reviewed 95 emergency operations for diverticulitis; 58 patients with grade I, II, and III sepsis were treated by laparotomy, debridement, and drainage without resection; whereas all 7 patients with grade IV sepsis underwent resection. The authors noted that the site of perforation was not evident in most cases. It is clear that many cases of perforated diverticulitis do not require immediate resection. However, nonresection therapy based on antibiotics alone is often inadequate,
Financial Disclosure: None reported. Presented at the meeting of the Royal Australian College of Surgeons, Brisbane, Australia, May 6 to 9, 2009. Correspondence: Stephen I White, M.B.B.S., F.R.A.C.S., John Flynn Medical Centre, Inland Drive, Tugun, Qld 4224, Australia. E-mail: staff@swhite.com.au Dis Colon Rectum 2010; 53: 15371541 DOI: 10.1007/DCR.0b013e3181f2ee2a The ASCRS 2010
DISEASES OF THE COLON & RECTUM VOLUME 53: 11 (2010)
1537
1538
WHITE ET AL: LAPAROSCOPIC LAVAGE FOR DIVERTICULITIS
and percutaneous drainage of an abscess is only popular for those patients without peritonitis. The operation of laparoscopic lavage allows for accurate Hinchey staging, detection of luminal communication, active debridement, and drainage of all varieties and number of intra-abdominal collections and an immediate decision regarding need for resection. Laparoscopic washout for perforated diverticulitis was first described by OSullivan et al4 in 1996, and in 2009 OSullivan and colleagues5 published a review of 100 consecutive laparoscopic lavages with a success rate of 93%. This article, our second on this topic,6 is a single-unit, 10-year audit of 78 consecutive patients with perforated diverticulitis and it highlights our experience with laparoscopic lavage.
METHODS AND PATIENTS
The John Flynn Private and The Tweed Public Hospitals are adjacent centers totaling 500 beds, staffed by a group of 4 general surgical visiting medical officers, training registrars, and fellows who were all heavily involved in patient management, including operations. Surgical management decisions were at the discretion of the treating surgical team; no protocols existed. All surgeons had established skills in open colorectal resection and anastomosis, whereas a learning curve existed for laparoscopic lavage. A retrospective review was performed of the charts of all patients undergoing emergency surgical intervention for perforated diverticulitis in the 10-year period from January 1999 through December 2008. The database for each patient consisted of age, ASA score, comorbidities, past history, CT findings, clinical abdominal findings, choice and timing of surgical intervention, complications, length of stay, transfer to intensive care unit (ICU), survival plus follow-up to time of publication. Patients were included who presented with 4-quadrant peritonitis and free gas on imaging or 2-quadrant peritonitis and collections 3 cm on CT. All patients in the series met the usual criteria for intervention; ie, medical and conservative therapy had failed for all of them. Patients were excluded who presented with small 3-cm collections, with minor local free gas perforations, or with single-quadrant peritonitis. Patients were also excluded who underwent emergency or urgent surgery for a diverticular phlegmonous mass or inflamed stricture with obstruction including stercoral obstruction and perforation. Also excluded were 3 patients who underwent successful washout for generalized purulent peritonitis where no definite cause was found; sigmoid diverticulae were found in all 3 patients, although the surgeon was not convinced they represented the site of perforation. Over the 10-year period of this audit, treatment protocols for perforated sigmoid diverticulitis have evolved. Lessons were learned from cases early in the audit where clinical, radiological, and intraoperative findings did not
seem to correlate. Open resection clearly represented an overtreatment for many patients until laparoscopic lavage became available in 2001. The initial results of washout were mixed and resorting to salvage Hartmann procedure was common. Refinements to our technique and improvements in case selection have resulted in laparoscopic lavage becoming an essential tool in our treatment of perforated sigmoid diverticulitis. Improvements in the availability and reliability of percutaneous drainage have also been welcomed in our institution, and cases of simple abscess without peritonitis that were successfully managed by laparoscopic lavage before 2005 would now be referred for attempted percutaneous drainage. The role of resection had obviously diminished owing to the improvements in nonresection therapy. Therefore, our current protocol, based on a combined clinical/radiological Hinchey grade, is as follows: patients with Hinchey I and II abscesses undergo percutaneous drainage; patients with Hinchey III abscesses undergo laparoscopic lavage; and patients with Hinchey IV abscesses require resection.
Technique
Laparoscopic lavage is performed with the patient in the lithotomy position with Trendelenburg and left-up tilt. The surgeon and assistant are on the patients right side with a 10-mm angled laparoscopic camera plus 3 5 mm ports. The average operating time for a laparoscopic washout is 50 minutes. No patients were converted to open surgery, although one patient required a hand-assisted laparoscopy to completely drain a large recurrent mesocolic abscess, after an initial washout. A single inadvertent intraoperative small-bowel enterotomy was successfully repaired laparoscopically. The sigmoid colon is approached medially. All omental, small-bowel, pelvic structures, and inflammatory abdominal wall attachments are mobilized away from the inflamed sigmoid colon. A thorough debridement and suction aspiration of all abscess contents should be performed with minimal bleeding. By this stage all preoperative clinical radiological findings should have been confirmed. Mesocolic Hinchey I abscess can require patient, yet determined probing of the intact sigmoid mesocolon before satisfactory drainage is achieved. Pelvic Hinchey II abscesses are often more difficult because of densely attached small bowel. Small abscesses may be encountered before the main large abscess is entered, which can be misleading. Hinchey III widespread purulent peritonitis is somewhat easier because inflammatory adhesions have rarely formed. In this situation, a larger volume of saline lavage is used, although rarely more than 1 L. After all the fluid is drained, fibrinopurulent membrane often remains. Hinchey IV abscesses have macroperforations unlike the microperforations of all other cases. Communication with
DISEASES OF THE COLON & RECTUM VOLUME 53: 11 (2010)
1539
TABLE 1. Patient data on an intention-to-treat basis
Laparoscopic lavage (n 35) Age range, y (mean) ASA III or above Hinchey grades I II III IV LOS, d (mean) ICU Complications Deaths 3686 (61) 11/35 (31%) 2 20 11 2 349 (14) 17/35 (48%) 19/35 (54%) 0 Resection (n 39) 5289 (74) 28/39 (71%) 8 11 18 4 190 (19) 31/39 (80%) 28/39 (74%) 5 Total (n 78) 5889 (72) 43/78 (55%) 10 31 29 6 190 (17) 48/78 (61%) 47/78 (60%) 5 P .002 .016
.200 .002 .330 .019
The data does not include 4 cases of percutaneous drainage. LOS length of stay; ICU intensive care unit.
the colonic lumen is easily demonstrated. Patch, suture, or glue is not attempted and resection is always performed. Drains are placed adjacent to the sigmoid colon in all cases. In the latter part of the series, the operation was completed by submersing the sigmoid colon in irrigation fluid, then gently insufflating it through the rectum via a rigid sigmoidoscope, looking for bubbles until the team was satisfied that no luminal communication existed. This also allows visualization should a tumor be suspected. In particular, in septic patients who were likely to spend several days in ICU receiving inotropic and ventilatory support, it became our practice to conduct a second-look laparoscopy on day 2 or 3 to check progress. A phlegmonous sigmoid was usually encountered, but little else. In the resection group, the Hartmann procedure was performed laparoscopically in one patient; the standard open technique was used in all other members of the group. Eight patients underwent laparotomy with resection and primary anastomosis, 4 with and 4 without diverting ileostomy. In the percutaneous drainage technique, a 10 Fg Pigtail catheter was inserted under CT guidance. The drain was removed when drainage ceased, usually in 3 or 4 days, although drainage for up to 2 weeks was seen. Antibiotics were used for 10 days, usually 5 days intravenously and 5 days orally.
RESULTS
A total of 78 consecutive patients required emergency intervention for septic complications of acute sigmoid diverticulitis during the 10-year study period. Table 1 details, on an intention-to-treat basis, the patient data, and results of laparoscopic lavage compared with the resection group and total audit group. Note that the age and ASA scores and ICU admission rarely are lower in the laparoscopic lavage group. Of the 35 laparoscopic lavage cases, 8 were so-called failures and required inpatient resection (Hartmann
rectosigmoidectomy in 6, resection primary anastomosis in 2). The clinical scenarios were as follows: 2 patients developed fecal fistulas, 1 cancer developed obstruction soon after washout, 2 collections were missed at initial washout, and 3 patients reported ongoing phlegmon. Furthermore, 8 of 27 outpatients within a mean of 6 months (range, 212 mo) developed symptoms requiring resection. The 3 earliest recurrences were all phlegmons that had persisted before re-presenting for further treatment. The one obstructive recurrence was another with ongoing phlegmon with fibrosis. The 3 colovesical fistulas re-presented nearly 12 months later after a long, apparently disease-free interval. Another patient had a reperforation in a fashion similar to the first presentation 12 months earlier; in that case, washout was again successful, and was followed by a semielective resection 3 months later. All 16 failures were managed by resection; 10 resections and primary anastomoses (8 laparoscopic, 2 open) and 6 open Hartmann procedures. Of the initial 27 laparoscopic successes, 4 patients required a second additional laparoscopic washout during the same admission. Two patients were in ICU to receive inotropes; the re-look laparoscopy at 48 hours found only minimal contamination after which both patients recovered and were discharged. The other 2 re-look laparoscopies were on day 7 for an abscess that had recollected; both were successfully redrained. Early in the series 8 elective resections were performed 2 to 3 months after successful washout before any symptoms of recurrence. In the later part of the series, patients were observed until symptoms demanded intervention; 12 patients remained symptom free after an average follow-up of 20 months (range, 6 60 mo).
DISCUSSION
Mayo7 in 1907 first described washout alone for perforated diverticulitis; subsequently, Killingback8 in 1970 reported 15 cases of debridement and drainage without resection for
1540
WHITE ET AL: LAPAROSCOPIC LAVAGE FOR DIVERTICULITIS
perforated diverticulitis with 0% mortality. Often combined with diverting colostomy and as the first part of a 3-stage resection, washout remained the treatment of choice until replaced by the more modern 2-stage resection in the 1980s.9 Since that time, the operative mortality for Hartmann emergency rectosigmoidectomy has remained approximately 10% with the added operative mortality rate for reversal of Hartmann of approximately 5% and a nonreversal rate of approximately 25%.10 Strict inclusion criteria for laparoscopic washout have yet to be described. OSullivan and colleagues5 were able to select 100 consecutive patients for laparoscopic washout, all with free gas on imaging and all with generalized peritonitis, although in that series 25% had only a local abscess at operation. Faranda et al,11 in an article presenting 18 laparoscopic washouts, also described 25% of patients, who were thought to have generalized peritonitis on clinical examination and preoperative imaging, but had only a localized abscess at operation. Our inclusion criteria for washout therefore encompasses any patient who does not respond to conservative management, comprising intravenous antibiotics and gut rest. Washout required immediately on arrival would be indicated in a patient with severe septic shock. In this situation, Hinchey IV fecal peritonitis should be suspected and managed appropriately (4 of 35 washouts were performed on day 1). Septic but stable patients, even those with generalized peritonitis on examination, can be initially managed with broad-spectrum antibiotics. Eighty-five percent or 28 of 35 washouts in our series occurred on day 2 or 3 after presentation. Failure to control pain and further clinical deterioration were the main indication for surgical intervention. Hinchey III purulent peritonitis was noted in 29 of 78 patients in this series, whereas Hinchey IV fecal peritonitis was found in only 6 of 78 patients. Three of 35 washouts were performed on day 7 for abscesses that could not be managed any other way. In 4 of 35 patients, perforated diverticulitis was first diagnosed intraoperatively. In 3 young males, appendicitis was the provisional diagnosis and no CT had been arranged. In another, laparoscopy was performed after ultrasound showed gallstones. Washout was particularly useful for these patients where no consent had been obtained for bowel resection and colostomy. Mortality in our series was 5 of 78 or 8%. All deaths occurred in the resection group. Four deaths occurred in cases of Hinchey IV fecal peritonitis, and the fifth death resulted from a Hinchey II pelvic abscess. After a successful washout, the issue of long-term recommendations arises. Should an episode of complicated diverticulitis be treated any differently from that of simple diverticulitis that was settled with antibiotics alone? Most authorities recommend a wait-and-see approach. Janes et al12 estimated that only 1% would develop recurrent
symptoms. Myers et al5 followed up 100 washouts without any developing recurrent symptoms. In the latter part of our series, we also adopted a wait-and-see approach after successful washout. Perforated sigmoid cancers do occur; in our series, 1 of 35, whereas in the series of Myers et al, 2 of 100.5 Clues may be obtained from the preoperative scan or the relative lack of phlegmonous change in the sigmoid colon seen at laparoscopy. The use of limited rigid sigmoidoscopy in this situation could be helpful. The technique of laparoscopic washout varies. Most other authors describe leaving omental attachments in place and using large-volume lavage.11,1316 We describe breaking down all adhesions, loculations, and interloop attachments with minimal lavage. Once the sigmoid colon is found to be intact, the aim is to drain all collections. Early in our experience, 2 washouts were found to be inadequate because persistent collections were missed initially. A single small-bowel enterotomy successfully repaired at the time was the only intraoperative injury. Despite the lack of any level I surgical evidence, percutaneous drainage of Hinchey I and II diverticular abscess is popular. Our experience with Hinchey I and II abscesses treated by washout involved 22 cases with an initial success of 86% (19/22), an average length of stay of 8 days, and lasting resolution of symptoms in 66%. The remaining 19 abscesses were managed by percutaneous drain,4 resection primary anastomosis,8 and Hartmann procedures.7 Ambrosetti and the University of Geneva team have published 20 years of experience on nonoperative management of diverticular abscess without peritonitis.17,18 Overall, nonoperative management failed in 32 of 137 (25%) patients in that series and immediate surgery was required; and another 53 of 109 (50%) patients required resection within a mean of 4 months. In our series, the abscesses in 2 of 4 patients undergoing percutaneous drainage did not fully settle and required resection within a month. The role of resection in perforated diverticulitis has been extensively studied. A meta-analysis in 2006 of acute surgical management of diverticulitis by Constantinides et al19 compared 417 Hartmann procedures with 547 resections and primary anastomoses. The overall mortality of Hartmann procedure was 15%. In the 189 Hinchey III and IV patients, the mortality was 14% in both resection options. In our institution, like all others, resection is appropriate when all other treatment options have failed. For these few selected patients with genuine fecal peritonitis, only 6 of 78 in our series and only 8 of 100 in OSullivans series, resection is clearly necessary.
CONCLUSION
Laparoscopic lavage for perforated sigmoid diverticulitis is a new technique. Careful case selection and attention to
DISEASES OF THE COLON & RECTUM VOLUME 53: 11 (2010)
1541
technical aspects are important to outcome. In Hinchey III purulent peritonitis, laparoscopic lavage can successfully help avoid resection. In Hinchey I and II with abscess formation, resection can usually be avoided by percutaneous drainage, although in our institution laparoscopic lavage was widely used. In Hinchey IV, resection is advised.
10. 11.
12.
REFERENCES
1. Wong WD, Wexner SD, Lowry A, et al. Practice parameters for the treatment of sigmoid diverticulitissupporting documentation. The Standards Task Force. The American Society of Colon and Rectal Surgeons. Dis Colon Rectum. 2000;43:290 297. 2. Kohler L, Sauerland S, Neugebauer E. Diagnosis and treatment of diverticular disease: results of a consensus development conference. The Scientific Committee of the European Association for Endoscopic Surgery. Surg Endosc. 1999;13:430 436. 3. Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85109. 4. OSullivan GC, Murphy D, OBrien MG, Ireland A. Laparoscopic management of generalized peritonitis due to perforated colonic diverticula. Am J Surg. 1996;171:432 434. 5. Myers E, Hurley M, OSullivan GC, Kavanagh D, Wilson I, Winter DC. Laparoscopic peritoneal lavage for generalized peritonitis due to perforated diverticulitis. Br J Surg. 2008;95:97101. 6. Taylor CJ, Layani L, Ghusn M, White SI. The perforated diverticulitis managed by laparoscopic lavage. ANZ J Surg. 2006;76: 962965. 7. Mayo WJ. Acquired diverticulitis of the large intestine. Surg Gynaecol Obstet. 1907;5:8. 8. Killingback MJ. Acute diverticulitis: progress report, Australasian survey (19671969). Dis Colon Rectum. 1970;13:444 447. 9. Krukowski ZH, Matheson NA. Emergency surgery for divertic13.
14.
15.
16.
17.
18.
19.
ular disease complicated by generalized and faecal peritonitis: a review. Br J Surg. 1984;71:921927. Seah DW, Ibrahim S, Tay KH. Hartmann procedure: is it still relevant today? ANZ J Surg. 2005;75:436 440. Faranda C, Barrat C, Catheline JM, Champault GG. Two-stage laparoscopic management of generalized peritonitis due to perforated sigmoid diverticular: eighteen cases. Surg Laparosc Endosc Percutan Tech. 2000;10:135141. Janes S, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg. 2005;92:133142. Chouillard E, Maggiori L, Ata T, et al. Laparoscopic two-stage left colonic resection for patients with peritonitis caused by acute divericulitis. Dis Colon Rectum. 2007;50:11571163. Mutter D, Bouras G, Forgione A, Vix M, Leroy J, Marescaux J. Two-stage totally minimally invasive approach for acute complicated diverticulitis. Colorectal Dis. 2008;8:501505. Bretagnol F, Pautrat K, Mor C, Benchellal Z, Huten N, de Calan L. Emergency laparoscopic management of perforated sigmoid diverticulitis: a promising alternative to more radical procedures. J Am Coll Surg. 2008;11:654 657. Franklin ME Jr, Dorman JP, Jacobs M, Plasencia G. Is laparoscopic surgery applicable to complicated colonic diverticular disease? Surg Endosc. 1997;11:10211025. Ambrosetti P, Chautems R, Soravia C, Peiris-Waser N, Terrier F. Long-term outcome of mesocolic and pelvic diverticular abscesses of the left colon: a prospective study of 73 cases. Dis Colon Rectum. 2005;48:787791. Brandt D, Gervaz P, Durmishi Y, Platon A, Morel P, Poletti PA. Percutaneous CT scan-guided drainage vs antibiotherapy alone for Hinchey II diverticulitis: a case-control study. Dis Colon Rectum. 2006;49:15331538. Constantinides VA, Tekkis PP, Athanasiou T, et al. Primary resection with anastomosis vs. Hartmanns procedure in nonelective surgery for acute colonic diverticulitis: a systemic review. Dis Colon Rectum. 2006;49:966 981.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Kriya For Balancing The ChakrasDocument5 pagesKriya For Balancing The ChakrasFedra Fox Cubeddu100% (2)
- Pest Control Risk Assessment Indoor and OutdoorDocument72 pagesPest Control Risk Assessment Indoor and OutdoorarmkarthickNo ratings yet
- ResumeDocument7 pagesResumeRonald Fuéntes EndómaNo ratings yet
- Gambaran CT SCAN: (Kasus: Edh, SDH, Ich, Sah, Infark Cerebri, IvhDocument44 pagesGambaran CT SCAN: (Kasus: Edh, SDH, Ich, Sah, Infark Cerebri, Ivhfahmi rosyadiNo ratings yet
- Basic Load (Individual) Veterinarian Field PackDocument3 pagesBasic Load (Individual) Veterinarian Field PackJohn MillerNo ratings yet
- FEVER Approach (Paeds)Document3 pagesFEVER Approach (Paeds)NorFarah Fatin AnuarNo ratings yet
- This Just In!: Queen Pin Carla!Document10 pagesThis Just In!: Queen Pin Carla!BS Central, Inc. "The Buzz"No ratings yet
- IRB Definitions (Is It Research? and Definitions of Exempt, Expedited and Full)Document4 pagesIRB Definitions (Is It Research? and Definitions of Exempt, Expedited and Full)analyn123No ratings yet
- District Sales Manager in Los Angeles CA Resume Ronald FoxDocument2 pagesDistrict Sales Manager in Los Angeles CA Resume Ronald FoxRonaldFoxNo ratings yet
- Archives of Gerontology and GeriatricsDocument7 pagesArchives of Gerontology and GeriatricsAna ArhipNo ratings yet
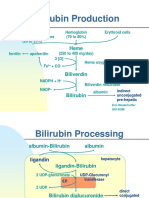
- Bilirubin Production: Hemoglobin (70 To 80%) Erythroid Cells Heme Proteins Myoglobin, Cytochromes (20 To 25%)Document5 pagesBilirubin Production: Hemoglobin (70 To 80%) Erythroid Cells Heme Proteins Myoglobin, Cytochromes (20 To 25%)Daffa Samudera Nakz DoeratipNo ratings yet
- Hospital Floor Plan Checklist ReviewDocument5 pagesHospital Floor Plan Checklist Reviewjherica baltazarNo ratings yet
- Resume 2018Document2 pagesResume 2018api-396582921No ratings yet
- Dermoid CystDocument8 pagesDermoid CystMohamed Hazem ElfollNo ratings yet
- How To Avoid Medication ErrorsDocument2 pagesHow To Avoid Medication ErrorsLorenn AdarnaNo ratings yet
- Integrating Modern Dermatology and AyurvedaDocument25 pagesIntegrating Modern Dermatology and AyurvedachandusgNo ratings yet
- Sage Char-Lee ResumeDocument2 pagesSage Char-Lee Resumeapi-510197139No ratings yet
- Leadership Development PlanDocument5 pagesLeadership Development Planapi-262531856No ratings yet
- Scrotal HerniaDocument9 pagesScrotal HerniaReymart BolagaoNo ratings yet
- Gardens For Patients With Alzheimer's DiseaseDocument3 pagesGardens For Patients With Alzheimer's DiseaseKritikou1547No ratings yet
- Brain SyncDocument3 pagesBrain Syncjbone918No ratings yet
- Pacemaker - Mayo ClinicDocument15 pagesPacemaker - Mayo ClinicShehab AhmedNo ratings yet
- Influence of The Quality of The FinishedDocument6 pagesInfluence of The Quality of The Finishedmehdi chahrourNo ratings yet
- Pulmonary EmbolismDocument93 pagesPulmonary EmbolismRakesh PanchalNo ratings yet
- Spring 2011 21st AnniversaryDocument56 pagesSpring 2011 21st AnniversaryRajesh SekhriNo ratings yet
- Project1 NewDocument43 pagesProject1 NewSharad DholeNo ratings yet
- Psychological Point of ViewDocument3 pagesPsychological Point of ViewForam PatelNo ratings yet
- Older Adults Group PlanDocument31 pagesOlder Adults Group Planapi-316614503No ratings yet
- 05thjan Assignment Abroad TimesDocument8 pages05thjan Assignment Abroad TimesSameer ShaikNo ratings yet
- Child Development Mannualfinal-SinhalaDocument250 pagesChild Development Mannualfinal-SinhalaAshhara FazalNo ratings yet