Professional Documents
Culture Documents
Progress Lipid Research 2
Uploaded by
WheeezzOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Progress Lipid Research 2
Uploaded by
WheeezzCopyright:
Available Formats
Progress in Lipid Research 50 (2011) 357371
Contents lists available at ScienceDirect
Progress in Lipid Research
journal homepage: www.elsevier.com/locate/plipres
Review
Cholesterol metabolism in neurons and astrocytes
Frank W. Pfrieger , Nicole Ungerer
CNRS UPR 3212, University of Strasbourg, Institute of Cellular and Integrative Neurosciences (INCI), 67084 Strasbourg Cedex, France
a r t i c l e
i n f o
a b s t r a c t
Cells in the mammalian body must accurately maintain their content of cholesterol, which is an essential membrane component and precursor for vital signalling molecules. Outside the brain, cholesterol homeostasis is guaranteed by a lipoprotein shuttle between the liver, intestine and other organs via the blood circulation. Cells inside the brain are cut off from this circuit by the bloodbrain barrier and must regulate their cholesterol content in a different manner. Here, we review how this is accomplished by neurons and astrocytes, two cell types of the central nervous system, whose cooperation is essential for normal brain development and function. The key observation is a remarkable cell-specic distribution of proteins that mediate different steps of cholesterol metabolism. This form of metabolic compartmentalization identies astrocytes as net producers of cholesterol and neurons as consumers with unique means to prevent cholesterol overload. The idea that cholesterol turnover in neurons depends on close cooperation with astrocytes raises new questions that need to be addressed by new experimental approaches to monitor and manipulate cholesterol homeostasis in a cell-specic manner. We conclude that an understanding of cholesterol metabolism in the brain and its role in disease requires a close look at individual cell types. 2011 Elsevier Ltd. All rights reserved.
Article history: Received 17 March 2011 Received in revised form 11 June 2011 Accepted 22 June 2011 Available online 1 July 2011 Keywords: Neuroglia Membrane lipids Steroids Apolipoproteins Lipoproteins Neurodegenerative diseases
Contents 1. 2. 3. Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Neurons and astrocytes: some background . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Cell-autonomous supply of cholesterol. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3.1. Cholesterol synthesis in the brain . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3.2. Cholesterol synthesis in neurons and astrocytes. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . External supply of cholesterol . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.1. Cholesterol secretion via lipoproteins . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.1.1. Expression of apolipoproteins in the brain . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.1.2. Lipoprotein secretion by astrocytes. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.1.3. Properties of astrocytic lipoproteins . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.1.4. Mechanisms of lipoprotein secretion by astrocytes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.2. Receptor-mediated uptake of lipoproteins . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.2.1. Expression of lipoprotein receptors in the brain . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.2.2. Receptor-mediated lipoprotein uptake by neurons . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.3. Intracellular redistribution of lipoprotein-derived cholesterol . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Handling surplus cholesterol . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5.1. Storage after esterification . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5.2. Elimination of cholesterol . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 358 358 359 359 359 360 360 360 360 361 361 362 362 362 362 363 363 363
4.
5.
Abbreviations: 24OHC, 24S-hydroxycholesterol; ABC, ATP binding cassette; CSF, cerebrospinal uid; CNS, central nervous system; DRG, dorsal root ganglion; ER, endoplasmic reticulum; LXR, liver x receptor; RGCs, retinal ganglion cells; VLDL, very low density lipoproteins. Corresponding author. Address: CNRS UPR 3212, University of Strasbourg, Institute of Cellular and Integrative Neurosciences (INCI), 5, rue Blaise Pascal, 67084 Strasbourg Cedex, France. Tel.: +33 388456645; fax: +33 388601664. E-mail addresses: fw-pfrieger@gmx.de, pfrieger@neurochem.u-strasbg.fr (F.W. Pfrieger). 0163-7827/$ - see front matter 2011 Elsevier Ltd. All rights reserved. doi:10.1016/j.plipres.2011.06.002
358
F.W. Pfrieger, N. Ungerer / Progress in Lipid Research 50 (2011) 357371
6.
5.2.1. Conversion to an oxysterol . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5.2.2. Secretion via ABC transporters . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Conclusion and outlook . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Acknowledgements . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
364 364 365 365 365
1. Introduction Cholesterol is an indispensible component of biological membranes and precursor to numerous signalling molecules including steroid hormones. Its provision and disposal in all organs of the mammalian body except for the brain relies on dietary uptake by the intestine, on de novo synthesis in every organ, and on lipoprotein-mediated transport via the blood circulation. Cells in the brain are cut off from this elaborate system by the bloodbrain barrier, which prevents lipoprotein exchange [1,2]. Therefore, cells in the brain have implemented their specic way to handle cholesterol turnover. Here, we summarize current knowledge of cholesterol metabolism in the central nervous system (CNS) with a focus on two cell types, namely neurons and astrocytes (Fig. 1). Their cooperation is essential for normal brain function, and a disturbance of their interactions can provoke pathologic changes. Complementary overviews focus on cholesterol metabolism in the nervous system [38] and possible links to brain injury and diseases [4,918].
Fig. 2. Spatial arrangement of astrocytic processes and chemical synapses. The electron micrograph of the molecular layer of the monkey cerebellum shows astrocytic processes (red) and synaptic connections between a presynaptic neuron that forms vesicle-lled terminals (blue) and a postsynaptic neuron with receptorbearing spines (green). Scale bar, 200 nm. Reprinted with permission from [337].
2. Neurons and astrocytes: some background The brain consists of neurons and glial cells. Neurons specialize in the generation and transmission of electrical signals that represent the basis of all brain functions. To accomplish this, they form elaborate processes called axons and dendrites and complex intercellular connections called synapses (Fig. 2). Glial cells, which comprise astrocytes, oligodendrocytes, ependymal and microglial cells,
Fig. 1. Neurons and astrocytes. The drawing by the Spanish neuroscientist and Nobel prize winner Santiago Ramn y Cajal illustrates human hippocampal protoplasmic astrocytes (A and B) that embrace cell bodies and dendrites of pyramidal neurons (C and D). The drawing was made after light microscopic study of an autopsy sample subjected to histologic gold chloride-sublimate staining. Reprinted with permission from [336].
provide structural and logistic support to neurons, which allows them to develop and function properly [19,20]. Among the glial cells, we focus on astrocytes, which form a complex fabric that enwraps neurons (Fig. 2) and ensure that neurons can generate and transmit electrical signals [21]. To this end, astrocytes regulate the extracellular potassium concentration [22], maintain the neuronal transmitter pool of glutamate by the glutamineglutamate cycle [23], provide neurons with energy substrates and antioxidative substances [24,25] and mediate the activity-dependent regulation of cerebral blood ow [26,27]. Moreover, astrocytes promote the formation of synapses [28] and sense or even inuence their activity [2934]. Last but not least, there is evidence that astrocytes play a role in neurodegeneration [21,3538]. Neurons and astrocytes have a very high demand for cholesterol. Neurons need to build the enormous membrane surface of their axons, dendrites and synapses [39,40]. For example, the membrane area of cerebellar Purkinje cells, namely their dendrites, reaches up to 150,000 lm2 [41], whereas myocyte membranes comprise only 5000 lm2 [42]. Synapses contain large amounts of membrane in postsynaptic spines and presynaptic vesicles, which have a particularly high cholesterol content (40 mol%) [43]. Individual astrocytes require large amounts of membrane, as they occupy immense non-overlapping volumes and touch up to 100,000 synapses through ne, micrometer sized processes [4448]. The demand of neurons and astrocytes for cholesterol in the adult brain cannot be measured directly. Previous studies indicated that the half-life of cholesterol in the brain lasts between two to six months [49,50], which indicated that there is little turnover of cholesterol in the brain. However, the bulk of cholesterol in the brain is contained in myelin, and therefore estimates of the metabolic stability of cholesterol in whole brain samples are largely determined by this pool [2]. The turnover of cholesterol in individual neurons and astrocytes may in fact be very high and reach an estimated 20% per day depending on the brain area and the neuronal cell type [2]. Support for this conclusion comes from the fact that the turnover of cholesterol is proportional to the metabolic rate across different tissues and animal species [2]. Since neurons have an intense
F.W. Pfrieger, N. Ungerer / Progress in Lipid Research 50 (2011) 357371
359
metabolic activity to generate action potentials and synaptic signals [5153], their cholesterol turnover should be high as well. 3. Cell-autonomous supply of cholesterol All cholesterol contained in the CNS must be formed in situ, because brain cells have no access to the hepatic or dietary supply of cholesterol due to the bloodbrain barrier. In general, mammalian cells can synthesize cholesterol from acetyl coenzyme A by a complex series of reactions that are catalyzed by more than 20 enzymes and that require energy and molecular oxygen [54]. In the following, we will describe, whether and how neurons and astrocytes use de novo synthesis to meet their need for cholesterol. 3.1. Cholesterol synthesis in the brain First evidence that brain cells synthesize cholesterol has been published 60 years ago by the group of Heinrich Waelsch. Their pioneering use of heavy water to study lipid synthesis in rats indicated that cholesterol is synthesized in the brain and that the rate of synthesis is higher during early postnatal development than in adult animals [55,56]. Using similar methods and thorough quantication, Quan and colleagues revealed that cholesterol synthesis in the developing mouse brain peaks during the second postnatal week and varies across regions. In adults, it falls to a tenth of the peak value and remains unaffected by gender or the cholesterol concentration in the blood [57]. Post-mortem examination of human brains reported an age-related decline of specic cholesterol precursors and concluded that cholesterol synthesis decreases with age [58]. A pioneering study indicated that the extent of cholesterol synthesis changes after brain injury [59]. Following a lesion of the entorhinal cortex of adult rats, the activity of 3hydroxy-3-methylglutaryl-coenzyme A reductase (HMGCR), which catalyzes the rate-limiting step in cholesterol synthesis, declined within eight days and returned to a normal level within a month. At the same time, proteins involved in cholesterol release and uptake were upregulated, which suggested that post-lesion recycling rather than synthesis of cholesterol is required for the regeneration of synaptic connections [59]. The importance of cholesterol synthesis for brain function is underlined by the fact that genetic defects in enzymes that mediate the post-squalene biosynthesis of cholesterol cause neurologic symptoms [60]. The most frequent and best studied disease is the SmithLemliOpitz syndrome, an autosomal recessive disorder that is characterized by malformation of several organs, neurologic symptoms and behavioral abnormalities. The genetic defect concerns 7-dehydrocholesterol reductase, which catalyzes a last step in cholesterol biosynthesis [61] (Fig. 3). 3.2. Cholesterol synthesis in neurons and astrocytes The extent of cholesterol synthesis in neurons and astrocytes in vivo remains unknown, because existing methods like metabolic labeling or pharmacologic manipulations do not allow to study cholesterol formation in specic cell types. Within the last 5 years, a new approach has appeared on the scene, which is based on the cell type-specic ablation of squalene synthase (farnesyl diphosphate farnesyl transferase 1, SQS/FDFT1) using the Cre/loxP system [6264]. SQS/FDFT1 catalyzes the rst committed step in sterol biosynthesis [65]. Saito and colleagues used this approach to block cholesterol biosynthesis in neuronal precursor cells during embryonic development by a Cre recombinase expressing mouse line, which targets progenitor cells in the ventricular zone and their progeny using the Nestin promoter. Mutant mice showed reduced brain size and perinatal lethality and newly generated neurons, but not their precursors, died of apoptosis. This indicated that new-
Fig. 3. Cholesterol synthesis in neurons and astrocytes. The diagram illustrates distinct features of cholesterol synthesis in neurons (blue) and astrocytes (red). Selected enzymatic steps and precursors in the biosynthesis of cholesterol that show cell-specic distribution based on in vitro data. The two pathways of cholesterol synthesis differ in the sequence of enzymatic steps and the resulting precursors. Enzymes: 1, SQS/FDFT1, squalene synthase (EC 2.5.1.21); 2, DHCR24, 24-dehydrocholesterol reductase (EC 1.3.1.72); 3, CYP51, cytochrome P450, family 51 (lanosterol 14-demethylase; EC 1.14.13.70); 4, NSDHL, NAD(P) dependent steroid dehydrogenase-like (EC 1.1.1.170, part of C4-demethylation enzyme complex). Precursors: 7D, 7-dehydro-cholesterol (KEGG entry C01164); CH, cholesterol (C00187); DE, desmosterol (C01802); LA, lanosterol (C01724); LT, lathosterol (C01189); ZN, zymostenol (C03845); ZY, zymosterol (C05437).
born neurons must synthesize cholesterol cell-autonomously in order to survive [64]. Fnfschilling and colleagues used a similar approach to ablate Sqs/Fdft1 in the adult brain using the Tg(Malpha6-Cre) line [63]. The transgenic mice targeted virtually all postmitotic, postmigratory cerebellar granule cells as well as neurons in brainstem nuclei. Absence of SQS/FDFT1 from these neurons had no effect on cerebellar morphology or function, and the mice showed normal motor control. Notably, absence of Sqs/Fdft1 expression in granule cells did not change the protein content of SQS/FDFT1 in cerebellar lysates indicating that these cells do not produce the enzyme at the adult stage. Sterol synthesis in neurons and astrocytes in vivo may be estimated from transcript proles of cholesterol synthesizing enzymes. A recent analysis of in situ hybridization data from the Allen Mouse Brain Atlas (http://www.brain-map.org) suggests that transcript levels of many cholesterol biosynthetic enzymes are higher in neurons compared to astrocytes [66]. However, these data should be interpreted with caution, as correlations between mRNA and protein abundance [67] and between protein levels and enzymatic activity are unknown. Cell culture experiments can address aspects of cholesterol biosynthesis in neurons and astrocytes that cannot be studied in vivo, although we note that culture conditions can inuence cholesterol homeostasis. Several groups compared sterol synthesis in neuronal and glial cell preparations using metabolic labeling with radioactive precursors. Their studies reported marked, albeit conicting, differences in terms of efcacy and regulation [6873]. Nieweg and colleagues used serum-free cultures of highly puried CNS neurons and glial cells from postnatal rats. They detected different proles of post-squalene precursors in neurons compared to glial cells (Fig. 3) [73]. Neurons contained mainly sterols of the socalled KandutschRussel pathway, whereas astrocytes contained precursors of the Bloch
360
F.W. Pfrieger, N. Ungerer / Progress in Lipid Research 50 (2011) 357371
pathway (Fig. 3). The accumulation of desmosterol in cultured astrocytes has been described previously [72,74,75] suggesting that desmosterol allows to trace sterol synthesis by this glial cell type. The high desmosterol content of the brain during postnatal development [57,76] may reect sterol formation by newborn astrocytes during this period. Notably, Nieweg and colleagues observed a lower rate of sterol synthesis in neurons compared to glial cells. In neurons, radioactive label was mainly found in lanosterol, whereas in glial cells it accumulated predominantly in cholesterol (Fig. 3) [73]. The accumulation of lanosterol in neurons is in line with previous reports [72,77]. Nieweg and colleagues detected very low levels of lanosterol-converting enzymes, 24-dehydrocholesterol reductase (seladin-1, DHCR24) and lanosterol 14-alpha demethylase (cytochrome P450, family 51, CYP51) suggesting that neurons cannot convert lanosterol efciently (Fig. 3) [73]. Moreover, inhibition of FDFT1 induced a much weaker up-regulation of biosynthetic enzymes in neurons compared to astrocytes. This suggests that neurons have a lower capacity to compensate for a cholesterol decit by de novo synthesis compared to astrocytes. Another question that cannot be addressed in vivo is whether axons and dendrites synthesize cholesterol autonomously. This was studied in so-called compartmented cultures, where neuronal axons and somata can be analyzed separately. Using such cultures of sympathetic neurons from newborn rats, Vance and colleagues showed that cholesterol synthesis is restricted to neuronal somata and does not occur in axons, whereas formation of phospholipids occurred in both compartments [78]. The distribution and activity of cholesterol-synthesizing enzymes in axons and dendrites still needs to be elucidated. Both compartments contain endoplasmic reticulum (ER) [79], where cholesterol synthesizing enzymes are located. Previous studies indicated a rapid intracellular redistribution of newly synthesized cholesterol in neurons and astrocytes. Metabolic labeling of cultured rat retinal ganglion cells (RGCs) and astrocytes revealed that newly synthesized cholesterol and precursors are transferred to the plasma membrane [73]. A study on compartmented cultures of rat sympathetic neurons revealed that newly synthesized cholesterol is transported from the soma to the axon [80]. In general, the subcellular dispatch of newly synthesized cholesterol from the ER to the plasma membrane is mediated by non-vesicular mechanisms that may involve direct membrane contact or specialized cytosolic carriers [8184]. At present, it remains to be studied whether and how neurons and astrocytes implement this transport system. Their complex morphology may demand elaborate mechanisms for the distribution of newly synthesized cholesterol into their vast cellular space. In summary, studies on cell-specic knockout-mice indicate that during embryonic development, newborn neurons must produce cholesterol in a cell-autonomous manner to survive, whereas in the adult brain, they acquire cholesterol from other sources. In vitro experiments suggest that neurons and astrocytes differ in the precursor prole of cholesterol synthesis and that astrocytes produce cholesterol at higher rates (Fig. 3). 4. External supply of cholesterol As alternative to de novo synthesis, mammalian cells can import cholesterol from an external source. To this end, providing cells secrete cholesterol as lipoproteins, which are taken up by target cells via specic receptors [83]. The following paragraphs summarize, whether and how neurons and astrocytes use this form of cholesterol provision. 4.1. Cholesterol secretion via lipoproteins If cells in the brain rely on the import of cholesterol, there must be a cell type that secretes cholesterol-containing lipoproteins.
There is strong experimental evidence that astrocytes fulll this role in the CNS. 4.1.1. Expression of apolipoproteins in the brain The expression of apolipoproteins should identify cells that secrete lipids via lipoproteins. The mammalian brain contains a subset of the apolipoproteins that are present in the blood. This includes apolipoprotein E (APOE) [85,86], apolipoprotein J/clusterin (APOJ/ CLU) [87,88] and apolipoprotein D (APOD) [89]. Apolipoprotein A1 (APOA1) is synthesized by endothelial cells of brain capillaries and by cells of the choroid plexus epithelium, but not by astrocytes or neurons [85,9092]. It is present in cerebrospinal uid [93,94], but barely detectable in lysates of rodent brain [95,96]. There is solid evidence that under normal conditions, APOE is produced exclusively by astrocytes and by astroglial cells like cerebellar Bergmann glia, tanycytes and retinal Mller cells [95,9799]. Moreover, astrocytes express APOJ/CLU and APOD [100], which have also been detected in subsets of neurons in rodents and humans [89,101111]. At present, it is unclear, whether APOD binds cholesterol. Its expression is highly upregulated in mice lacking APOE suggesting its involvement in lipoprotein metabolism [112]. Previous studies have shown that various forms of injury and disease cause upregulation of APOE, APOD and APOJ/CLU in the mammalian CNS [103,106,110,113120]. The increase in APOE occurred mainly in glial brillary acidic protein (GFAP)-positive cells [113,121126], but it was also observed in neurons [127]. The appearance of APOE in neurons after injury or disease could be due to increased uptake rather than enhanced expression [128,129]. Direct evidence for lesion-induced neuronal expression of APOE comes from a study on a transgenic knock-in mouse, where the expression of green uorescent protein is controlled by the Apoe promoter. Administration of kainic acid induced APOE expression in hippocampal neurons [98]. Interestingly, APOE expression was decreased in primary astrocytes derived from a mouse model of Huntingtons disease [130]. An injury- or disease-induced increase in APOD was observed in astrocytes and neurons [106,109,131133]. Arraybased transcript proling and behavioral testing in rats revealed an age-dependent impairment of performance in a spatial memory task that was accompanied by increasing levels of APOE in hippocampal astrocytes [134]. Possible correlations between cholesterol transport and age-related cognitive decline need to be further explored. 4.1.2. Lipoprotein secretion by astrocytes There is good evidence that astrocytes secrete lipoproteins in vivo. In a pioneering study, Amaratunga and colleagues showed that retinal Mller cells, which represent a subtype of astroglial cells, produce and secrete APOE in vitro, and that injection of radiolabeled amino acids in the retinal vitreous led to accumulation of labeled APOE in the optic nerve [135]. These results suggested that APOE secreted by retinal Mller cells in vivo is taken up by RGCs, whose axons form the optic nerve. Other studies detected lipoproteins that contain APOE in cerebrospinal uid (CSF) of rodents and humans [8,93,94,136140]. In humans, the APOE level in CSF is less than 5% of its concentration in plasma [93,94,140]. Since blood-derived lipoproteins cannot enter the brain and since APOE is made exclusively by astrocytes, these cells are most likely the source of the particles. Further support comes from a study on transgenic mice, which express human isoforms of APOE under the control of the human GFAP promoter. This promoter drives expression in subsets of astrocytes and neuronal precursors [141,142]. The CSF of these mice contained lipoproteins with human isoforms of APOE indicating their provenance from astrocytes [139]. In cultured astrocytes, APOE deciency abolished lipoprotein secretion [143,144], but its impact on lipoprotein secretion in vivo remains to be claried. Studies on APOE-decient mice [145,146] revealed
F.W. Pfrieger, N. Ungerer / Progress in Lipid Research 50 (2011) 357371
361
normal cholesterol content [112,147,148] and turnover in various brain regions [57]. On the other hand, mice lacking APOE showed signicantly reduced levels of cholesterol and selected precursors including desmosterol in the hippocampus compared to control mice, when maintained in a normal environment, but enhanced levels when maintained in an enriched environment [149]. This indicated an inuence of APOE on cholesterol metabolism and its modication by sensory stimulation. Interestingly, APOE-decient mice show behavioral and neurologic symptoms [150158] and defects in sensory systems [159163]. At the cellular level, APOE deciency causes an agedependent loss of synapses and dendrites [164,165] and a shift in the transbilayer distribution of cholesterol at synaptic membranes [166]. It remains unknown, whether these changes are caused by reduced lipoprotein secretion from astrocytes or by defects in APOE signaling that are independent from cholesterol. APOJ/CLU-decient mice show no overt changes in the nervous system [167], but reduced damage due to hypoxiaischemia-induced brain injury suggesting that this protein contributes to neuronal cell death [168]. 4.1.3. Properties of astrocytic lipoproteins Studies of astrocyte-derived lipoproteins formed in vitro revealed that their chemical and physical properties differ substantially from those present in plasma [74,94,138,139,143,169173]. Lipoproteins secreted by cultured astrocytes contain cholesterol and phospholipids, but comparatively little esteried cholesterol or triglycerides. The presence of cholesterol precursors, namely lathosterol and desmosterol, in glia-derived lipoproteins [74,75] suggests that astrocytes secrete precursors that are taken up by neurons and converted to cholesterol. Such partial outsourcing may be very efcient, as it circumvents inefcient steps in neurons like the conversion of lanosterol. Astrocyte-derived lipoproteins are disc-shaped with sizes ranging from 8 to 17 nm, and their densities are similar to those of high-density lipoproteins [138]. They contain only APOE and APOJ/CLU, which are present on distinct particles [104,138,139,143,169]. APOE particles are larger and contain more lipid than those harboring APOJ/CLU [139,143]. Cultures prepared from knockout mice showed that expression of APOE, but not of APOJ/CLU is required for lipid secretion [139,143,144]. So far, only one study showed that cultured astrocytes secrete APOD associated with lipids [105] and therefore, APOD-containing complexes should be characterized further. The properties of lipoproteins that are produced by astrocytes in vivo are currently unknown due to the lack of suitable isolation methods. They may differ from those produced in vitro for two reasons. First, cultured astrocytes are mainly surrounded by medium, whereas astrocytes in vivo are embedded in a narrow and tortuous extracellular space, which may inuence the size and composition of their lipoproteins. Second, cultured astrocytes are generated from precursors in vitro in the presence of serum, and may not fully recapitulate the differentiation of astrocytes in vivo as indicated by a recent transcript analysis [174]. The properties of astrocytic lipoproteins produced in vivo may also differ from those present in CSF. The CSF harbors a variety of lipoproteins with distinct physical and chemical properties, which may be modied by the isolation methods [94,138140]. A subclass of CSF lipoproteins loosely resembles those secreted by astrocytes in vitro [138,139] suggesting their astrocytic origin [175]. Astrocyte-derived particles may undergo modications in the parenchym or in the CSF [176]. This includes esterication of cholesterol by secreted lecithin cholesterol acyltransferase (LCAT), which allows the molecule to enter the hydrophobic core of lipoproteins. This enzyme was found to be expressed by neurons and glial cells in adult rhesus monkeys [101] and by cultured neurons and astrocytes from embryonic and postnatal mice [177]. LCAT activity was detected in human CSF [178180], and its absence
in knockout mice lowered the concentration of cholesteryl esters in the brain compared to wildtype controls [181]. A recent in vitro study showed that despite its expression in neurons and astrocytes, LCAT was only present in astrocyte-conditioned medium [182]. The enzyme esteried preferentially cholesterol in culture medium from astrocytes rather than from neurons and APOE activated the enzyme. Finally, lipoprotein particles from glial cells of LCAT-decient mice were smaller than those secreted by glial cells from wildtype mice [182]. In agreement with these data, cholesterol esterication was detected only in astrocyte-, but not in neuron-conditioned culture medium [73].
4.1.4. Mechanisms of lipoprotein secretion by astrocytes It is unclear, how lipoproteins are assembled and secreted by astrocytes. The mechanisms may be similar to those employed by hepatocytes to secrete lipoproteins, i.e. assembly of a core particle in the ER, transfer to the Golgi apparatus for further modications and subsequent secretion [183]. These nascent lipoproteins may be directly taken up by neighboring neurons or they may acquire additional cholesterol by similar mechanisms as high-density lipoproteins [184]. Lipidation of nascent particles is mediated by specic subtypes of the ATP binding cassette (ABC) transporters. ABCA1 transfers cellular cholesterol to acceptors like APOA1 [185], and ABCG1 is thought to charge high-density lipoproteins with lipids [83,186188]. Immunohistochemical staining showed that in adult rodents ABCA1 is predominantly expressed by neurons and at lower levels by glial cells [189191]. The same appears to be true for ABCG1 and ABCG4 as shown by analysis of knock-in mice, where betagalactosidase replaces endogenous ABC transporters [192,193]. Cultured astrocytes express all three transporters at the transcript and protein level [75,144,191,192,194,195]. ABCG1 and ABCG4 colocalize in endosomal vesicles of cultured astrocytes, but are absent from the Golgi apparatus, the ER and from lysosomes [192]. Therefore, the pool of cholesterol that is accessible to these transporters, remains to be identied. Several studies have shown that efux of cholesterol from cultured astrocytes can be enhanced by treatment with agonists of liver x receptors (LXRs) [144,191,194,196]. These nuclear receptors control expression of proteins that mediate cellular cholesterol release including APOE, ABCA1 and APOA1 [197,198]. The contribution of ABCA1 to cholesterol efux from cultured astrocytes was indicated by the increased expression after treatment with a LXR agonist [191,194,196,199]. Studies on transgenic mice lacking or over-expressing ABCA1 support the idea that the transporter contributes to the lipidation of APOE-containing lipoproteins, although its role in astrocytes remains to be claried. ABCA1 deciency in mice reduced the cholesterol content and size of APOE-containing CSF lipoproteins [200] and the cholesterol concentration in culture medium of astrocytes [200,201]. Conversely, overexpression of ABCA1 in the mouse brain increased the size of CSF lipoproteins and enhanced the cholesterol to APOE ratio in lipoproteins from cultured astrocytes [202]. ABCA1 deciency also caused a strong reduction of APOE in the brain and CSF [96,200,201]. This may signify enhanced catabolism of APOE due to insufcient lipidation. The extent, to which ABCA1 deciency decreased APOE levels, was highest in the hippocampus and lowest in the cerebellum [201] suggesting that the contribution of ABCA1 to APOE lipidation varies across brain regions. A genetic study on humans showed that a single nucleotide polymorphism in the Abca1 gene correlates highly with the level of cholesterol in the CSF [203]. Finally, absence of APOE enhanced the transcript level of Abca1 in the brain indicating that ABC transporters can compensate for the loss of APOE-mediated cholesterol release [112].
362
F.W. Pfrieger, N. Ungerer / Progress in Lipid Research 50 (2011) 357371
The residual efux of cholesterol from astrocytes lacking ABCA1 may be mediated by ABCG transporters. Astrocytes from mice lacking both ABCG1 and ABCG4 showed reduced release of cholesterol and desmosterol onto high-density lipoprotein particles [75] and in cultured cerebellar glia, the extent of cholesterol efux correlated with the expression level of ABCG1, but not of ABCA1 [144]. On the other hand, overexpression of ABCG1 in the CNS did not affect the APOE content in the brain or the cholesterol efux from cultured glial cells [204]. Interestingly, increasing the levels of ABCG1 in glial cells enhanced the ability of glia-derived lipoproteins to stimulate axonal growth in vitro [205]. Overexpression and reduction of ABCA1 or ABCG transporters decrease and enhance the levels of cholesterol precursors in the brain [75,96,193,204] suggesting a direct or indirect inuence of ABC transporters on cholesterol synthesis or precursor efux. At present, it is unclear, whether astrocytes secrete cholesterol at a constant level or whether the release is modied by external or internal factors. Previous studies revealed various molecules that modulate the release of APOE and cholesterol from cultured astrocytes. This includes steroids [206], cytokines [207], growth factors [208,209] and the cAMP-, protein kinase C- and phosphoinositide3-kinase/extracellular signal-regulated kinase 1/2-dependent pathways [210,211]. 4.2. Receptor-mediated uptake of lipoproteins The cellular uptake of lipoproteins is mediated by specic receptors. They form an ancient family of structurally related membrane-spanning proteins that bind APOE and other ligands [212] and that fulll transport and signaling functions [213]. Among the different family members, two receptors are most likely involved in cholesterol transport in the brain, the prototypic lowdensity lipoprotein receptor (LDLR) and the low-density lipoprotein receptor-related protein 1 (LRP1). 4.2.1. Expression of lipoprotein receptors in the brain In situ hybridization and immunohistochemical staining revealed that LDLR is expressed by neurons and glial cells [94,214], whereas LRP1 is predominantly expressed by neurons [215221]. In vitro studies showed that dorsal root ganglion (DRG) cells and hippocampal neurons express more LRP1 than LDLR [222,223], whereas sympathetic neurons expressed LDLR but not LRP1 [224]. At the protein level, cultured astrocytes contained 2-fold more LDLR than LRP1 [223]. Pathologic conditions change the level and cell-specic expression pattern of lipoprotein receptors. In the sciatic nerve, LDLR is expressed at a low level under normal conditions, but strongly upregulated on regenerating axons after injury [225]. Moreover, LRP1 expression has been observed in glial cells including astrocytes in autopsy samples from Alzheimers patients [217,220] and following brain injury or neoplastic transformation [226]. Entorhinal cortex lesion in adult rats enhances the density of low density lipoprotein binding sites in granule cells, and in the molecular layer of the dentate gyrus in parallel with astrocyte proliferation [59]. The subcellular distribution of lipoprotein receptors in neurons has been studied in vitro. At a premature stage, LDLR is present in axons and somata of sympathetic [224] and hippocampal neurons with strong expression on growth cones [227]. Studies on compartmented cultures revealed that axons of sympathetic neurons [80] and RGCs [228] take up cholesterol via lipoproteins to support axon regeneration. In mature neurons, LDLR and LRP1 are located in the somatodendritic compartment [229232]. Notably, LRP1 colocalizes partially with proteins of the postsynaptic density, namely NMDA receptor subunits, which prompted the idea that this receptor is involved in plasticity-related phenomena [232].
4.2.2. Receptor-mediated lipoprotein uptake by neurons Evidence that neurons take up lipoproteins via dedicated receptors comes from in vitro and in vivo studies. Pioneering work showed that monoclonal antibodies against LDLR block the uptake of uorescently labeled lipoproteins from regenerating sciatic nerves by neurons from dorsal root ganglia of embryonic rats [233] and the enhancement of neurite outgrowth by very low density lipoproteins (VLDL) in cultured rabbit DRG cells. The latter effect required the presence of lipids, as APOE alone showed no effect [222,234]. Studies on puried rat RGCs showed that low density lipoprotein receptor-related protein associated protein 1 (LRPAP1), an antagonist of lipoprotein receptors [235], inhibits the effects of glia-conditioned medium on synapse number [236] and axonal growth [228]. Similarly, LRPAP1 and antibodies to LRP1 inhibited the growth of neurites and dendrites in cultured neurons induced by a feeding layer of cortical astrocytes [230,237] or by blood-, CSFor glia-derived lipoproteins [205,238,239]. Lipoprotein uptake by astrocytes has received little attention, probably because the cells are considered to export rather than import lipids. Interestingly, a recent study showed that neurons and astrocytes express distinct splice variants of the VLDL receptor, which differ in their capacity to bind lipoproteins [240]. This observation suggests that the lipoprotein transfer between brain cells is ne-tuned. The relevance of lipoprotein receptors for cholesterol and APOE transport in vivo has been studied in transgenic mice. Complete elimination of LDLR in knockout mice enhances the level of APOE in the CSF by 50% [241], although the cells responsible for this change remained unknown. Neuron-specic ablation of LRP1 using the Cre/loxP system also increased the APOE level and decreased the cholesterol content in the forebrain [242,243]. Conversely, overexpression of a LRP1 fragment with binding activity decreased the APOE level in the brain by 25% [244]. Importantly, neuron-specic ablation of LRP1 causes age-dependent loss of spines and synapses [243] and impairs motor function and memory [232,243]. 4.3. Intracellular redistribution of lipoprotein-derived cholesterol Externally acquired cholesterol exits from the endosomal/lysosomal system and reaches subcellular membrane compartments [8184]. This pathway is relevant in neurons, because dysfunction of two components of late endosomes/lysosomes that mediate the exit of cholesterol, namely Niemann-Pick type C1 (NPC1) and C2 (NPC2), cause neurologic symptoms in patients with Niemann-Pick type C (NPC) disease, an inherited and ultimately fatal human lysosomal storage disorder [14,245250]. NPC1 is a transmembrane protein with a sterol-sensitive domain [251] and NPC2 is an intralumenal component that binds cholesterol [84,252]. Based on structural data, Kwon and colleagues proposed that NPC2 transfers unesteried cholesterol from endocytosed lipoproteins to NPC1, which then mediates the exit from the endosomal/lysosomal system [253]. The dysfunction of either protein causes accumulation of unesteried cholesterol in the late endosome/lysosome [254 257]. Mice lacking NPC1 show marked defects in the CNS including formation of meganeurites and ectopic dendrites, axonal degeneration and progressive loss of specic neuronal cell types and glial cells [155,159,258,259], in particular cerebellar Purkinje cells [260,261]. Moreover, the mice show physiopathologic changes in the retina including photoreceptor degeneration, impaired lightevoked responses and changes of the autophagy pathway in RGCs [262]. In situ hybridization and immunohistochemical staining indicated that NPC1 and NPC2 are expressed by both neurons and glial cells [258,263266]. Accordingly, NPC1 deciency causes accumulation of unesteried cholesterol and pathologic changes in neurons and glial cells [257,258,267]. Recent studies suggest that the degeneration of neurons in NPC disease is a cell-autonomous
F.W. Pfrieger, N. Ungerer / Progress in Lipid Research 50 (2011) 357371
363
process: In mice with mosaic expression of NPC1, individual Purkinje cells lacking NPC1 degenerated, whereas those expressing intact NPC1 or those having glial neighbors lacking NPC1 did not [268]. Selective elimination of NPC1 in Purkinje cells in conditional knockout mice was sufcient to induce age-dependent motor deficits and Purkinje cell degeneration [269] and rescue of NPC1-deciency in neurons prevented neuronal degeneration, whereas rescue in glial cells did not [270]. Notably, NPC1 deciency did not impair cholesterol secretion by cultured astrocytes [74,173]. Evidence for the opposing view that NPC1 is relevant in glial cells came from the observation that expression of NPC1 under the control of the human GFAP promoter prolongs the life-span of NPC1decient mice [271]. However, this promoter also drives expression in neuronal precursor cells [141] and thus the rescued lifespan could be due to neuronal expression of NPC1. A possible contribution of glial cells to neurodegeneration and reduced life span in NPC1-decient mice and humans remains to be dened. Why does NPC1 deciency cause the cell-autonomous demise of specic neurons? The neurons may depend strongly on the import of external cholesterol via lipoproteins. Support for this idea comes from the appearance of autophagosomes in Purkinje cells [268,272,273] and RGCs of NPC1-decient mice [262]. These neurons may experience a cholesterol decit due to the accumulation of cholesterol in the late endosome/lysosome, which they try to compensate by salvaging internal membranes. Alternatively, these neurons may require functions of the endosomal/lysosomal system that are independent from cholesterol import and disturbed by NPC1 deciency. This includes release and recycling of synaptic vesicles in presynaptic terminals, which is impaired in NPC1-decient hippocampal neurons in vitro [274277]. Finally, NPC1 deciency may cause the demise of neurons by impairing their response to growth factors [278], their mitochondrial function [279] or the structural integrity of axons [280,281]. The cell-spe-
cic vulnerability of neurons to NPC1 deciency may depend on high activity of lysosomal enzymes [282]. In summary, there is good evidence that astrocytes secrete cholesterol via APOE-containing lipoproteins, which have distinct properties from those found in blood and which are possibly lipidated by ABC transporters (Fig. 4). The molecular mechanisms of cholesterol remain to be claried. In vivo and in vitro studies indicate that LDLR and LRP1 mediate uptake of cholesterol- and APOE-containing lipoproteins in CNS neurons and that neuronal cholesterol uptake helps to maintain synaptic integrity (Fig. 4). The age-related degeneration of specic types of neurons lacking NPC1 indicates their strong dependency on an external supply of cholesterol. 5. Handling surplus cholesterol Based on our current knowledge of cholesterol metabolism in neurons and astrocytes, we surmise that only neurons need to deal with cholesterol overload, because they import the component, whereas astrocytes produce cholesterol in excess for its release via APOE-containing lipoproteins. 5.1. Storage after esterication Cells can store surplus cholesterol intracellularly within socalled lipid droplets [283,284]. To this end, cholesterol is esteried by acyl-coenzyme A:cholesterol acyltransferase 1, also called sterol O-acyltransferase 1 (ACAT1/SOAT1), which is located in the ER [285]. Cholesterol esterifying activity was detected in the brains of humans [286], rats [287], chicken [288] and mice [289] at about 1% of the total cholesterol content [289,290]. Transcripts of Acat1/Soat1 are present in the adult mouse brain at region-specic levels, whereas Acat2/Soat2 is expressed in very low amounts except for the thalamus [289,291]. In the rat brain, the concentration of cholesterol esters and the number of Acat1/Soat1 transcripts increase with age [292]. Pharmacologic and genetic reduction of ACAT1/SOAT1 activity in mice decreased the concentration of cholesterol esters in the brain by 86% [293] and ablated cholesterol esterication in homogenates from different brain regions [289], respectively. A genetic association study in humans revealed that a variant of the Acat1/Soat1 gene is associated with lower levels of cholesterol in the CSF [294], which corroborates the idea that ACAT1/SOAT1 activity inuences cholesterol metabolism in the CNS. Which cells in the brain show ACAT1/SOAT1 activity? Immunohistochemical staining revealed that the enzyme is present in neurons, but not in glial cells [295]. This is further supported by in situ hybridization data on adult mice, which reveal a complementary distribution of cholesterol esterifying enzymes in the cerebellum, where LCAT is expressed by Bergmann glia, whereas ACAT is expressed by Purkinje cells (Allen Mouse Brain Atlas. Seattle (WA): Allen Institute for Brain Science. 2011. Available from: http://mouse.brain-map.org). Experiments on primary cultures showed that the enzyme is active in neurons: Inhibition of ACAT1/SOAT1 in cultured mouse neurons enhanced the ratio of free to esteried cholesterol [296] and incubation of highly puried RGCs with radioactively labeled cholesterol led to intracellular accumulation of cholesterol esters [73]. Notably, cultured astrocytes esterify cholesterol via ACAT1/SOAT1, when they lack APOE and when they are charged with exogenous cholesterol [144]. At present, it remains to be tested, whether neurons or astrocytes store cholesterol in its esteried form. 5.2. Elimination of cholesterol Storage is a possible way to handle surplus cholesterol, but there is good evidence that neurons command specic means for its elimination.
Fig. 4. Neuronal cholesterol homeostasis requires astrocytes. The diagram illustrates the cell-specic distribution of proteins involved in the release, intercellular transport and storage/elimination of cholesterol in neurons (blue) and astrocytes (red). Proteins present in both cell types are indicated in black. The expression patterns suggest that neurons depend on the supply of cholesterol by astrocytes via the LDLR- and LRP1-mediated endocytosis of APOE-containing lipoproteins, and that neurons handle surplus cholesterol by hydroxylation, storage and excretion. Lipoproteins mediating the elimination of cholesterol and 24OH may reach the bloodbrain barrier (BBB) via the CSF or astrocytes.
364
F.W. Pfrieger, N. Ungerer / Progress in Lipid Research 50 (2011) 357371
5.2.1. Conversion to an oxysterol Research within the last decade revealed that neurons employ a unique way to get rid of cholesterol, namely the conversion to 24Shydroxycholesterol (24OHC), which is also called cerebrosterol [7]. The presence of this oxysterol in the human brain has been uncovered more than 50 years ago [297], but its function has remained obscure until its implication in cholesterol elimination from the brain was discovered. Pioneering work by the Bjorkhem group revealed synthesis of 24OHC in the brain in vivo, a continuous ux from the brain to blood and its elimination as bile [50,298301]. Moreover, the group showed that the concentration of 24OHC in the CSF and blood declines with age [298]. Hydroxylation of cholesterol at C24 strongly accelerates its translocation between lipophilic compartments and thereby facilitates the passage across the bloodbrain barrier [302]. A recent study showed that genetic elimination of ACAT1/SOAT1 in a triple transgenic mouse model of Alzheimers disease decreases cholesterol synthesis and enhances the 24OHC level in the brain [289]. These ndings suggest that if neurons loose the ability to store cholesterol as esters, they eliminate excess amounts by conversion to 24OHC. There is evidence that 24OHC plays a dual role. Besides being metabolite for elimination of cholesterol, it may act as a signaling molecule that regulates cholesterol homeostasis [303] and developmental processes like neurogenesis [304] by activating LXRs. Neuron-derived 24OHC may signal to astrocytes the neuronal cholesterol levels. Such a dual role raises the question, whether the intra- and intercellular transport of 24OHC is purely diffusion-driven, or whether there are mechanisms for a targeted transport. Kim and colleagues showed that 24OHC release from cultured neurons is enhanced by the presence of APOE [305] suggesting that the oxysterol hitchhikes on lipoproteins. A pharmacologic study in adult rats in vivo indicated that the transport of 24OHC across the bloodbrain barrier is mediated by an organic anion transporter [306]. The intracellular transport of 24OHC may involve oxysterol-binding proteins [307]. These components are expressed in the brain [308], but their functions in neurons or astrocytes remain to be unexplored. The formation of 24OHC is catalyzed by a member of the cytochrome P450 family, cholesterol 24-hydroxylase (CYP46A1) [309]. This enzyme is mainly found in the gray matter of the CNS and its level increases steadily during postnatal development to reach a constant plateau in the adult [309,310]. Immunohistochemical staining showed its expression in neurons of different regions of the embryonic and adult rodent brain including cerebellar cortex, thalamus, hippocampus and retina [309,311,312], but not by astrocytes [311]. Interestingly, the staining intensity differs among neuronal cell types with large neurons like pyramidal cells, Purkinje cells and RGCs showing high levels of expression. This supports the idea that the rate of cholesterol turnover differs among neurons [313]. Immunocytochemical staining of cultured neurons revealed that CYP46A1 is located in the ER and present in somata and dendrites, but not in axons or presynaptic terminals [311]. Several studies suggest that brain injury or disease shift CYP46A1 expression from neurons to microglia [314] or astrocytes [315318], but the functional relevance remains unclear. The promoter region of Cyp46a1 contains binding sites for transcription factors that regulate housekeeping enzyme and shows relative insensitivity to gene regulatory pathways [310,319]. These observations indicate that neurons express Cyp46a1 at a fairly constant level. Neuronal synthesis of 24OHC from radioactively labeled cholesterol and its secretion were conrmed in primary cultures of fetal human neurons [305] and of highly puried RGCs from postnatal rats [73]. The latter study also conrmed exclusive expression of CYP46A1 in neurons, but not astrocytes. Further hydroxylation of 24OHC at C25 has been observed in cultured neurons and astrocytes [320,321], but the relevance of this compound remains unknown.
The physiologic importance of 24OHC was revealed by CYP46A1 knockout mice. These mice develop normally, but show strongly reduced levels of 24OHC in the brain, which conrmed ablation of enzymatic activity [322]. The rate of cholesterol synthesis in the brain of CYP46A1 knockout mice is reduced by 40% probably to compensate for the reduced elimination. This relatively strong reduction indicates that CYP46A1-expressing neurons command a considerable fraction of cholesterol turnover in the adult brain [322,323]. It was also shown that CYP46A1 deciency in mice reduces the efux of cholesterol from the brain by two thirds [323]. This important nding points to CYP46A1-dependent and independent modes of cholesterol excretion from the brain. Further evidence for a CYP46A1-independent pathway comes from a thorough quantitative analysis of cholesterol accretion and synthesis rates in mice. This study showed that pharmacological activation of LXRs in adult mice enhanced cholesterol excretion from the brain independently from an increase in transcript levels of Cyp46a1 [324]. 5.2.2. Secretion via ABC transporters A CYP46A1-independent pathway for cholesterol elimination from neurons may be the direct release onto APOA1-containing lipoproteins that are present in the CSF [93,94,140]. If neurons employ such a mode of release, they must express ABC transporters that mediate cellular sterol efux, namely ABCA1, ABCG1 and ABCG4 [188]. In situ hybridization and immunohistochemical staining revealed that ABCA1 is expressed by neurons in embryonic and adult rodents [189191,262,325], with high expression levels in large cells like hippocampal pyramidal cells and Purkinje cells [190,191]. The regional and cell-specic distribution of ABCG1 and ABCG4 has been determined using knock-in mice, which express beta-galactosidase under the control of the endogenous Abcg1 and Abcg4 promoters [326]. The studies showed strong neuronal expression of both transporters in the embryonic and adult brain and their colocalization in specic neuronal cell types like hippocampal pyramidal cells, cerebellar Purkinje cells and RGCs [75,192,193]. Studies on primary cultures revealed that basal levels of ABCA1, ABCG1 and ABCG4 are ve times higher in neurons compared to astrocytes [192] and that pharmacologic activation of the LXR pathway induces an increase in mRNA levels of ABCG1, but not of ABCG4 in neurons and astrocytes [192,204]. The subcellular distribution of the transporters has been studied in primary cultures and cell lines by immunocytochemical staining and by transfection with tagged proteins. ABCA1 was present in perinuclear compartments of neurons and on the surface of axons, somata and dendrites [189,191], whereas ABCG1 and ABCG4 colocalized in endosomal vesicles, which were predominantly present in axons [192]. Do ABC transporters mediate cholesterol efux from neurons? So far, answers come solely from in vitro studies. Treatment of primary neuronal cultures from embryonic rats with an LXR agonist, enhanced ABCA1 expression and, with the same time course, cholesterol efux onto externally applied apolipoproteins [191]. In an earlier paper, Whitney and colleagues did not observe a LXR-induced increase in cholesterol efux from cultured neurons even in the presence of external apolipoproteins, although the treatment increased Abca1 and Abcg1 transcripts [194]. The divergent results are probably due to different experimental protocols. A more direct proof that ABCA1 mediates neuronal cholesterol efux was provided recently [327]. Downregulation of ABCA1 levels by RNA interference in cultured neurons reduced the efux of cholesterol and phospholipids onto externally supplied APOE, whereas pharmacologic enhancement of ABCA1 levels enhanced the lipid release [327]. So far, there is no direct evidence that neurons excrete cholesterol in vivo. Pharmacologic enhancement of ABCA1 and ABCG1 levels in mice increases cholesterol excretion from the brain by
F.W. Pfrieger, N. Ungerer / Progress in Lipid Research 50 (2011) 357371
365
1.6-fold [324], but the cellular source remains to be dened. Cellspecic elimination or overexpression of ABC transporters remains to be accomplished. The idea that neurons dispose of cholesterol directly via preformed APOA1-containing lipoproteins raises the question, how these lipoproteins are then eliminated from the brain. This could involve LRP1 or scavenger receptor class B1, which are both expressed by brain capillary endothelial cells [328,329]. LRP1 binds APOE, which may also be present on these lipoproteins, and mediates the clearance of beta-amyloid from the brain [330]. SCARB1 has been shown to promote efux of cholesterol via brain capillary endothelial cells in vitro [328]. The APOA1-containing lipoproteins carrying surplus cholesterol from neurons may pass through astrocytes, which express SCARB1 [331333], and whose endfeet are in touch with the capillary endothelial cells (Fig. 4). We note that absence of SCARB1 in mice does not affect sterol turnover or APOE levels [57,334], but may induce age-related synaptic defects and memory decits [335]. Taken together, neurons may handle excess cholesterol by esterication and subsequent intracellular storage, by direct excretion via ABC transporters and by conversion to 24OHC (Fig. 4). 6. Conclusion and outlook The investigation of cholesterol metabolism in the brain has a long history, but it is only within the last decade that this eld has gained momentum (Fig. 5), probably because cholesterol is implied in neurodegenerative disease. It is evident that cells in the CNS employ their proper system to maintain their cholesterol content, which is very different from the way cholesterol metabolism is organized in the rest of the body. Our focus on neurons and astrocytes, whose cooperation is necessary for brain development and function, exposes several peculiarities. First, there is a remarkable cell-specic distribution of proteins that are involved in cholesterol metabolism (Figs. 3 and 4). For example, astrocytes, but not neurons, express APOE and secrete lipoproteins. On the other hand, neurons, but not astrocytes, express CYP46, which enables removal of surplus cholesterol from the brain. Second, cell-specic gene ablation in transgenic mice revealed that neurons must synthesize cholesterol to survive during early development, but not in the adult, and that neuronal lipoprotein uptake affects APOE and cholesterol levels and is necessary for spine integrity and brain function. Notably, there is evidence that several pathways mediate cholesterol excretion from the brain, one of which is cholesterol hydroxylation by neurons. Third, in vitro studies revealed that
astrocytes and neurons synthesize cholesterol by different pathways and at different rates. Together, these observations insinuate that cholesterol turnover in neurons depends on close metabolic cooperation with astrocytes. New questions arise. For example, how high is the cholesterol turnover in neurons during development and in the adult? Do all neurons rely on cholesterol from astrocytes? How do axons, dendrites and synapses build and maintain their cholesterol content? Where and how is the transport of cholesterol from astrocytes to neurons accomplished? Does the intra- and intercellular transport of oxysterols involve dedicated carriers? Why are components of cholesterol metabolism upregulated after injury and disease? Answering these questions requires new experimental approaches to map the cellular and subcellular distribution of cholesterol and of proteins involved in its homeostasis and new mouse models to monitor and interfere with cholesterol metabolism in a cell-specic manner. Whatever lies ahead in this exciting eld, we predict that an understanding of cholesterol metabolism in the brain and its role in disease requires meticulous study of individual cell types in the CNS. Acknowledgements The authors gratefully acknowledge previous and ongoing support by Abbott/Laboratoires Fournier, Agence Francaise Contres les Myopathies, Agence National de la Recherche, Ara Parseghian Medical Research Foundation, Centre National de la Recherche Scientique, Deutsche Forschungsgemeinschaft, ELTEM, European Commission Coordination Action ENINET (contract number LSHM-CT-2005-19063), Fondation NRJ-Institut de France, Fondation pour la Recherche Medicale, Max-Planck Society, Merck-Serono, Miltenyi Biotec, Ministre de lEnseignement Suprieur et de la Recherche, Neurex, Rgion Alsace, Retina France, Sano-Aventis and Universit de Strasbourg. References
[1] Linton MF, Gish R, Hubl ST, Butler E, Esquivel C, Bry WI, et al. Phenotypes of apolipoprotein B and apolipoprotein E after liver transplantation. J Clin Invest 1991;88:27081. [2] Dietschy JM, Turley SD. Thematic review series: brain lipids. Cholesterol metabolism in the central nervous system during early development and in the mature animal. J Lipid Res 2004;45:137597. [3] Camargo N, Smit AB, Verheijen MH. SREBPs: SREBP function in glianeuron interactions. FEBS J 2009;276:62836. [4] De Chaves EP, Narayanaswami V. Apolipoprotein E and cholesterol in aging and disease in the brain. Future Lipidol 2008;3:50530. [5] Dietschy JM. Central nervous system: cholesterol turnover, brain development and neurodegeneration. Biol Chem 2009;390:28793. [6] Mulder M. Sterols in the central nervous system. Curr Opin Clin Nutr Metab Care 2009;12:1528. [7] Russell DW, Halford RW, Ramirez DM, Shah R, Kotti T. Cholesterol 24hydroxylase: an enzyme of cholesterol turnover in the brain. Annu Rev Biochem 2009;78:101740. [8] Vance JE, Hayashi H. Formation and function of apolipoprotein E-containing lipoproteins in the nervous system. Biochim Biophys Acta 2010;1801:80618 [9] Ikonen E. Mechanisms for cellular cholesterol transport: defects and human disease. Physiol Rev 2006;86:123761. [10] Valenza M, Cattaneo E. Cholesterol dysfunction in neurodegenerative diseases: is Huntingtons disease in the list? Prog Neurobiol 2006;80:16576. [11] Carter CJ. Convergence of genes implicated in Alzheimers disease on the cerebral cholesterol shuttle: APP, cholesterol, lipoproteins, and atherosclerosis. Neurochem Int 2007;50:1238. [12] Hirsch-Reinshagen V, Wellington CL. Cholesterol metabolism, apolipoprotein E, adenosine triphosphate-binding cassette transporters, and Alzheimers disease. Curr Opin Lipidol 2007;18:32532. [13] Bu G. Apolipoprotein E and its receptors in Alzheimers disease: pathways, pathogenesis and therapy. Nat Rev Neurosci 2009;10:33344. [14] Karten B, Peake KB, Vance JE. Mechanisms and consequences of impaired lipid trafcking in Niemann-Pick type C1-decient mammalian cells. Biochim Biophys Acta 2009;1791:65970. [15] Martins IJ, Berger T, Sharman MJ, Verdile G, Fuller SJ, Martins RN. Cholesterol metabolism and transport in the pathogenesis of Alzheimers disease. J Neurochem 2009;111:1275308. [16] Fliesler SJ, Bretillon L. The ins and outs of cholesterol in the vertebrate retina. J Lipid Res 2010;51:3399413.
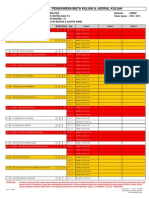
Fig. 5. Publications on cholesterol in selected organs during postwar decades. Number of publications during indicated periods normalized to paper counts during the last interval. The numbers of publications were extracted from boolean PubMed searches on cholesterol and the indicated organ. Numbers in legend indicate paper counts during last decade and the total number of publications. Note the stagnation of research on cholesterol in the brain during the 70s and 80s, and the 2-fold increase within the last decade. Based on total paper counts, research on brain represents a smaller eld compared to studies on blood or the liver.
366
F.W. Pfrieger, N. Ungerer / Progress in Lipid Research 50 (2011) 357371 [56] Waelsch H, Sperry WB, Stoyanoff VA. A study of the synthesis and deposition of lipids in brain and other tissues with deuterium as an indicator. J Biol Chem 1940;135:2916. [57] Quan G, Xie C, Dietschy JM, Turley SD. Ontogenesis and regulation of cholesterol metabolism in the central nervous system of the mouse. Brain Res Dev Brain Res 2003;146:8798. [58] Thelen KM, Falkai P, Bayer TA, Lutjohann D. Cholesterol synthesis rate in human hippocampus declines with aging. Neurosci Lett 2006;403:159. [59] Poirier J, Baccichet A, Dea D, Gauthier S. Cholesterol synthesis and lipoprotein reuptake during synaptic remodelling in hippocampus in adult rats. Neuroscience 1993;55:8190. [60] Waterham HR. Defects of cholesterol biosynthesis. FEBS Lett 2006;580:54429. [61] Kelley RI, Hennekam RC. The SmithLemliOpitz syndrome. J Med Genet 2000;37:32135. [62] Saher G, Brugger B, Lappe-Siefke C, Mobius W, Tozawa R, Wehr MC, et al. High cholesterol level is essential for myelin membrane growth. Nat Neurosci 2005;8:46875. [63] Fnfschilling U, Saher G, Xiao L, Mobius W, Nave KA. Survival of adult neurons lacking cholesterol synthesis in vivo. BMC Neurosci 2007;8:1. [64] Saito K, Dubreuil V, Arai Y, Wilsch-Brauninger M, Schwudke D, Saher G, et al. Ablation of cholesterol biosynthesis in neural stem cells increases their VEGF expression and angiogenesis but causes neuron apoptosis. Proc Natl Acad Sci USA 2009;106:83505. [65] Tansey TR, Shechter I. Squalene synthase: structure and regulation. Prog Nucleic Acid Res Mol Biol 2001;65:15795. [66] Valdez CM, Smith MA, Perry G, Phelix CF, Santamaria F. Cholesterol homeostasis markers are localized to mouse hippocampal pyramidal and granule layers. Hippocampus 2010;20:9025. [67] Maier T, Guell M, Serrano L. Correlation of mRNA and protein in complex biological samples. FEBS Lett 2009;583:396673. [68] Jones JP, Nicholas HJ, Ramsey RB. Rate of sterol formation by rat brain glia and neurons in vitro and in vivo. J Neurochem 1975;24:1236. [69] Volpe JJ, Hennessy SW. Cholesterol biosynthesis and 3-hydroxy-3-methylglutaryl coenzyme A reductase in cultured glial and neuronal cells. Regulation by lipoprotein and by certain free sterols. Biochim Biophys Acta 1977;486:40820. [70] Lopes-Cardozo M, Larsson OM, Schousboe A. Acetoacetate and glucose as lipid precursors and energy substrates in primary cultures of astrocytes and neurons from mouse cerebral cortex. J Neurochem 1986;46:7738. [71] Saito M, Benson EP, Saito M, Rosenberg A. Metabolism of cholesterol and triacylglycerol in cultured chick neuronal cells, glial cells, and broblasts: accumulation of esteried cholesterol in serum-free culture. J Neurosci Res 1987;18:31925. [72] Tabernero A, Bolanos JP, Medina JM. Lipogenesis from lactate in rat neurons and astrocytes in primary culture. Biochem J 1993;294(Pt 3):6358. [73] Nieweg K, Schaller H, Pfrieger FW. Marked differences in cholesterol synthesis between neurons and glial cells from postnatal rats. J Neurochem 2009;109:12534. [74] Mutka AL, Lusa S, Linder MD, Jokitalo E, Kopra O, Jauhiainen M, et al. Secretion of sterols and the NPC2 protein from primary astrocytes. J Biol Chem 2004;279:4865462. [75] Wang N, Yvan-Charvet L, Lutjohann D, Mulder M, Vanmierlo T, Kim TW, et al. ATP-binding cassette transporters G1 and G4 mediate cholesterol and desmosterol efux to HDL and regulate sterol accumulation in the brain. FASEB J 2008;22:107382. [76] Hinse CH, Shah SN. The desmosterol reductase activity of rat brain during development. J Neurochem 1971;18:198998. [77] Suzuki S, Kiyosue K, Hazama S, Ogura A, Kashihara M, Hara T, et al. Brainderived neurotrophic factor regulates cholesterol metabolism for synapse development. J Neurosci 2007;27:641727. [78] Vance JE, Pan D, Campenot RB, Bussiere M, Vance DE. Evidence that the major membrane lipids, except cholesterol, are made in axons of cultured rat sympathetic neurons. J Neurochem 1994;62:32937. [79] Ramirez OA, Couve A. The endoplasmic reticulum and protein trafcking in dendrites and axons. Trends Cell Biol; 2011. [80] de Chaves EI, Rusinol AE, Vance DE, Campenot RB, Vance JE. Role of lipoproteins in the delivery of lipids to axons during axonal regeneration. J Biol Chem 1997;272:3076673. [81] Soccio RE, Breslow JL. Intracellular cholesterol transport. Arterioscler Thromb Vasc Biol 2004;24:115060. [82] Prinz WA. Non-vesicular sterol transport in cells. Prog Lipid Res 2007;46:297314. [83] Ikonen E. Cellular cholesterol trafcking and compartmentalization. Nat Rev Mol Cell Biol 2008;9:12538. [84] Storch J, Xu Z. Niemann-Pick C2 (NPC2) and intracellular cholesterol trafcking. Biochim Biophys Acta; 2009. [85] Elshourbagy NA, Liao WS, Mahley RW, Taylor JM. Apolipoprotein E mRNA is abundant in the brain and adrenals, as well as in the liver, and is present in other peripheral tissues of rats and marmosets. Proc Natl Acad Sci USA 1985;82:2037. [86] Lorent K, Overbergh L, Moechars D, De Strooper B, van Leuven F, Van den Berghe H. Expression in mouse embryos and in adult mouse brain of three members of the amyloid precursor protein family, of the alpha-2-macroglobulin receptor/ low density lipoprotein receptor-related protein and of its ligands apolipoprotein E, lipoprotein lipase, alpha-2-macroglobulin and the 40,000
[17] Harris JR, Milton NG. Cholesterol in Alzheimers disease and other amyloidogenic disorders. Subcell Biochem 2010;51:4775. [18] Liu JP, Tang Y, Zhou S, Toh BH, McLean C, Li H. Cholesterol involvement in the pathogenesis of neurodegenerative diseases. Mol Cell Neurosci 2010;43:3342. [19] Kettenmann H, Ransom BR. Neuroglia. New York: Oxford University Press; 2004. [20] Kettenmann H, Verkhratsky A. Neuroglia: the 150 years after. Trends Neurosci 2008;31:6539. [21] Wang DD, Bordey A. The astrocyte odyssey. Prog Neurobiol 2008;86:34267. [22] Kofuji P, Newman EA. Potassium buffering in the central nervous system. Neuroscience 2004;129:104556. [23] Danbolt NC. Glutamate uptake. Prog Neurobiol 2001;65:1105. [24] Pellerin L, Bouzier-Sore AK, Aubert A, Serres S, Merle M, Costalat R, et al. Activity-dependent regulation of energy metabolism by astrocytes: an update. GLIA 2007;55:125162. [25] Giaume C, Koulakoff A, Roux L, Holcman D, Rouach N. Astroglial networks: a step further in neuroglial and gliovascular interactions. Nat Rev Neurosci 2010;11:8799. [26] Iadecola C, Nedergaard M. Glial regulation of the cerebral microvasculature. Nat Neurosci 2007;10:136976. [27] Koehler RC, Roman RJ, Harder DR. Astrocytes and the regulation of cerebral blood ow. Trends Neurosci 2009;32:1609. [28] Pfrieger FW. Role of glial cells in the formation and maintenance of synapses. Brain Res Rev 2010;63:3946. [29] Theodosis DT, Poulain DA, Oliet SH. Activity-dependent structural and functional plasticity of astrocyteneuron interactions. Physiol Rev 2008;88:9831008. [30] Fellin T. Communication between neurons and astrocytes: relevance to the modulation of synaptic and network activity. J Neurochem 2009;108:53344. [31] Fiacco TA, Agulhon C, McCarthy KD. Sorting out astrocyte physiology from pharmacology. Annu Rev Pharmacol Toxicol 2009;49:15174. [32] Nimmerjahn A. Astrocytes going live: advances and challenges. J Physiol 2009;587:163947. [33] Perea G, Navarrete M, Araque A. Tripartite synapses: astrocytes process and control synaptic information. Trends Neurosci 2009;32:42131. [34] Santello M, Volterra A. Synaptic modulation by astrocytes via Ca2+-dependent glutamate release. Neuroscience 2009;158:2539. [35] Giaume C, Kirchhoff F, Matute C, Reichenbach A, Verkhratsky A. Glia: the fulcrum of brain diseases. Cell Death Differ 2007;14:132435. [36] De Keyser J, Mostert JP, Koch MW. Dysfunctional astrocytes as key players in the pathogenesis of central nervous system disorders. J Neurol Sci 2008;267:316. [37] Wetherington J, Serrano G, Dingledine R. Astrocytes in the epileptic brain. Neuron 2008;58:16878. [38] Blackburn D, Sargsyan S, Monk PN, Shaw PJ. Astrocyte function and role in motor neuron disease: a future therapeutic target? GLIA 2009;57:125164. [39] Goritz C, Mauch DH, Pfrieger FW. Multiple mechanisms mediate cholesterolinduced synaptogenesis in a CNS neuron. Mol Cell Neurosci 2005;29:190201. [40] Pfenninger KH. Plasma membrane expansion: a neurons Herculean task. Nat Rev Neurosci 2009;10:25161. [41] Rapp M, Segev I, Yarom Y. Physiology, morphology and detailed passive models of guinea-pig cerebellar Purkinje cells. J Physiol 1994;474:10118. [42] Gabella G, Blundell D. Nexuses between the smooth muscle cells of the guinea-pig ileum. J Cell Biol 1979;82:23947. [43] Takamori S, Holt M, Stenius K, Lemke EA, Gronborg M, Riedel D, et al. Molecular anatomy of a trafcking organelle. Cell 2006;127:83146. [44] Grosche J, Matyash V, Moller T, Verkhratsky A, Reichenbach A, Kettenmann H. Microdomains for neuronglia interaction: parallel ber signaling to Bergmann glial cells. Nat Neurosci 1999;2:13943. [45] Bushong EA, Martone ME, Jones YZ, Ellisman MH. Protoplasmic astrocytes in CA1 stratum radiatum occupy separate anatomical domains. J Neurosci 2002;22:18392. [46] Ogata K, Kosaka T. Structural and quantitative analysis of astrocytes in the mouse hippocampus. Neuroscience 2002;113:22133. [47] Halassa MM, Fellin T, Takano H, Dong JH, Haydon PG. Synaptic islands dened by the territory of a single astrocyte. J Neurosci 2007;27:64737. [48] Witcher MR, Kirov SA, Harris KM. Plasticity of perisynaptic astroglia during synaptogenesis in the mature rat hippocampus. Glia 2007;55:1323. [49] Serougne-Gautheron C, Chevallier F. Time course of biosynthetic cholesterol in the adult rat brain. Biochim Biophys Acta 1973;316:24450. [50] Bjrkhem I, Lutjohann D, Breuer O, Sakinis A, Wennmalm A. Importance of a novel oxidative mechanism for elimination of brain cholesterol. Turnover of cholesterol and 24(S)-hydroxycholesterol in rat brain as measured with 18O2 techniques in vivo and in vitro. J Biol Chem 1997;272:3017884. [51] Attwell D, Laughlin SB. An energy budget for signaling in the grey matter of the brain. J Cereb Blood Flow Metab 2001;21:113345. [52] Alle H, Roth A, Geiger JR. Energy-efcient action potentials in hippocampal mossy bers. Science 2009;325:14058. [53] Jolivet R, Magistretti PJ, Weber B. Deciphering neuron-glia compartmentaliza tion in cortical energy metabolism. Front Neuroenergetics 2009;1:4. [54] Gaylor JL. Membrane-bound enzymes of cholesterol synthesis from lanosterol. Biochem Biophys Res Commun 2002;292:113946. [55] Waelsch H, Sperry WB, Stoyanoff VA. Lipid metabolism in brain during myelination. J Biol Chem 1940;135:297302.
F.W. Pfrieger, N. Ungerer / Progress in Lipid Research 50 (2011) 357371 molecular weight receptor-associated protein. Neuroscience 1995;65: 100925. May PC, Lampert-Etchells M, Johnson SA, Poirier J, Masters JN, Finch CE. Dynamics of gene expression for a hippocampal glycoprotein elevated in Alzheimers disease and in response to experimental lesions in rat. Neuron 1990;5:8319. Nuutinen T, Suuronen T, Kauppinen A, Salminen A. Clusterin: a forgotten player in Alzheimers disease. Brain Res Rev 2009;61:89104. Boyles JK, Notterpek LM, Wardell MR, Rall Jr SC. Identication, characterization, and tissue distribution of apolipoprotein D in the rat. J Lipid Res 1990;31:224356. Haddad IA, Ordovas JM, Fitzpatrick T, Karathanasis SK. Linkage, evolution, and expression of the rat apolipoprotein A-I, C-III, and A-IV genes. J Biol Chem 1986;261:1326877. Weiler-Guttler H, Sommerfeldt M, Papandrikopoulou A, Mischek U, Bonitz D, Frey A, et al. Synthesis of apolipoprotein A-1 in pig brain microvascular endothelial cells. J Neurochem 1990;54:44450. Mockel B, Zinke H, Flach R, Weiss B, Weiler-Guttler H, Gassen HG. Expression of apolipoprotein A-I in porcine brain endothelium in vitro. J Neurochem 1994;62:78898. Roheim PS, Carey M, Forte T, Vega GL. Apolipoproteins in human cerebrospinal uid. Proc Natl Acad Sci USA 1979;76:46469. Pitas RE, Boyles JK, Lee SH, Hui D, Weisgraber KH. Lipoproteins and their receptors in the central nervous system. Characterization of the lipoproteins in cerebrospinal uid and identication of apolipoprotein B, E(LDL) receptors in the brain. J Biol Chem 1987;262:1435260. Boyles JK, Pitas RE, Wilson E, Mahley RW, Taylor JM. Apolipoprotein E associated with astrocytic glia of the central nervous system and with nonmyelinating glia of the peripheral nervous system. J Clin Invest 1985;76:150113. Karasinska JM, Rinninger F, Lutjohann D, Ruddle P, Franciosi S, Kruit JK, et al. Specic loss of brain ABCA1 increases brain cholesterol uptake and inuences neuronal structure and function. J Neurosci 2009;29:357989. Lin CT, Xu YF, Wu JY, Chan L. Immunoreactive apolipoprotein E is a widely distributed cellular protein. Immunohistochemical localization of apolipoprotein E in baboon tissues. J Clin Invest 1986;78:94758. Xu Q, Bernardo A, Walker D, Kanegawa T, Mahley RW, Huang Y. Prole and regulation of apolipoprotein E (ApoE) expression in the CNS in mice with targeting of green uorescent protein gene to the ApoE locus. J Neurosci 2006;26:498594. Kurumada S, Onishi A, Imai H, Ishii K, Kobayashi T, Sato SB. Stage-specic association of apolipoprotein A-I and E in developing mouse retina. Invest Ophthalmol Vis Sci 2007;48:181523. Rassart E, Bedirian A, Do CS, Guinard O, Sirois J, Terrisse L, et al. Apolipoprotein D. Biochim Biophys Acta 2000;1482:18598. Smith KM, Lawn RM, Wilcox JN. Cellular localization of apolipoprotein D and lecithin:cholesterol acyltransferase mRNA in rhesus monkey tissues by in situ hybridization. J Lipid Res 1990;31:9951004. Provost PR, Villeneuve L, Weech PK, Milne RW, Marcel YL, Rassart E. Localization of the major sites of rabbit apolipoprotein D gene transcription by in situ hybridization. J Lipid Res 1991;32:195970. Danik M, Chabot JG, Hassan-Gonzalez D, Suh M, Quirion R. Localization of sulfated glycoprotein-2/clusterin mRNA in the rat brain by in situ hybridization. J Comp Neurol 1993;334:20927. Pasinetti GM, Johnson SA, Oda T, Rozovsky I, Finch CE. Clusterin (SGP-2): a multifunctional glycoprotein with regional expression in astrocytes and neurons of the adult rat brain. J Comp Neurol 1994;339:387400. Patel SC, Asotra K, Patel YC, McConathy WJ, Patel RC, Suresh S. Astrocytes synthesize and secrete the lipophilic ligand carrier apolipoprotein D. Neuroreport 1995;6:6537. Ong WY, He Y, Suresh S, Patel SC. Differential expression of apolipoprotein D and apolipoprotein E in the kainic acid-lesioned rat hippocampus. Neuroscience 1997;79:35967. Navarro A, Tolivia J, Astudillo A, Del Valle E. Pattern of apolipoprotein D immunoreactivity in human brain. Neurosci Lett 1998;254:1720. Ong WY, Lau CP, Leong SK, Kumar U, Suresh S, Patel SC. Apolipoprotein D gene expression in the rat brain and light and electron microscopic immunocytochemistry of apolipoprotein D expression in the cerebellum of neonatal, immature and adult rats. Neuroscience 1999;90:91322. Kalman J, McConathy W, Araoz C, Kasa P, Lacko AG. Apolipoprotein D in the aging brain and in Alzheimers dementia. Neurol Res 2000;22:3306. Thomas EA, Dean B, Pavey G, Sutcliffe JG. Increased CNS levels of apolipoprotein D in schizophrenic and bipolar subjects: implications for the pathophysiology of psychiatric disorders. Proc Natl Acad Sci USA 2001;98:406671. Navarro A, del Valle E, Tolivia J. Differential expression of apolipoprotein d in human astroglial and oligodendroglial cells. J Histochem Cytochem 2004;52:10316. Jansen PJ, Lutjohann D, Thelen KM, von Bergmann K, van Leuven F, Ramaekers FC, et al. Absence of ApoE upregulates murine brain ApoD and ABCA1 levels, but does not affect brain sterol levels, while human ApoE3 and human ApoE4 upregulate brain cholesterol precursor levels. J Alzheimers Dis 2009;18:31929. Poirier J, Hess M, May PC, Finch CE. Astrocytic apolipoprotein E mRNA and GFAP mRNA in hippocampus after entorhinal cortex lesioning. Brain Res Mol Brain Res 1991;11:97106.
367
[87]
[88] [89]
[90]
[91]
[92]
[93] [94]
[95]
[96]
[97]
[98]
[99]
[100] [101]
[102]
[103]
[104]
[105]
[106]
[107] [108]
[109] [110]
[111]
[112]
[113]
[114] Diedrich JF, Minnigan H, Carp RI, Whitaker JN, Race R, Frey W, et al. Neuropathological changes in scrapie and Alzheimers disease are associated with increased expression of apolipoprotein E and cathepsin D in astrocytes. J Virol 1991;65:475968. [115] Page KJ, Hollister RD, Hyman BT. Dissociation of apolipoprotein and apolipoprotein receptor response to lesion in the rat brain: an in situ hybridization study. Neuroscience 1998;85:116171. [116] Schauwecker PE, Cogen JP, Jiang T, Cheng HW, Collier TJ, McNeill TH. Differential regulation of astrocytic mRNAs in the rat striatum after lesions of the cortex or substantia nigra. Exp Neurol 1998;149:8796. [117] Terrisse L, Poirier J, Bertrand P, Merched A, Visvikis S, Siest G, et al. Increased levels of apolipoprotein D in cerebrospinal uid and hippocampus of Alzheimers patients. J Neurochem 1998;71:164350. [118] Terrisse L, Seguin D, Bertrand P, Poirier J, Milne R, Rassart E. Modulation of apolipoprotein D and apolipoprotein E expression in rat hippocampus after entorhinal cortex lesion. Brain Res Mol Brain Res 1999;70:2635. [119] Glockner F, Ohm TG. Hippocampal apolipoprotein D level depends on Braak stage and APOE genotype. Neuroscience 2003;122:10310. [120] Iwata A, Browne KD, Chen XH, Yuguchi T, Smith DH. Traumatic brain injury induces biphasic upregulation of ApoE and ApoJ protein in rats. J Neurosci Res 2005;82:10314. [121] Ali SM, Dunn E, Oostveen JA, Hall ED, Carter DB. Induction of apolipoprotein E mRNA in the hippocampus of the gerbil after transient global ischemia. Brain Res Mol Brain Res 1996;38:3744. [122] Zarow C, Victoroff J. Increased apolipoprotein E mRNA in the hippocampus in Alzheimer disease and in rats after entorhinal cortex lesioning. Exp Neurol 1998;149:7986. [123] Nathan BP, Nisar R, Randall S, Short J, Sherrow M, Wong GK, et al. Apolipoprotein E is upregulated in olfactory bulb glia following peripheral receptor lesion in mice. Exp Neurol 2001;172:12836. [124] Terai K, Iwai A, Kawabata S, Sasamata M, Miyata K, Yamaguchi T. Apolipoprotein E deposition and astrogliosis are associated with maturation of beta-amyloid plaques in betaAPPswe transgenic mouse: implications for the pathogenesis of Alzheimers disease. Brain Res 2001;900:4856. [125] Haasdijk ED, Vlug A, Mulder MT, Jaarsma D. Increased apolipoprotein E expression correlates with the onset of neuronal degeneration in the spinal cord of G93A-SOD1 mice. Neurosci Lett 2002;335:2933. [126] Seitz A, Kragol M, Aglow E, Showe L, Heber-Katz E. Apolipoprotein E expression after spinal cord injury in the mouse. J Neurosci Res 2003;71:41726. [127] Aoki K, Uchihara T, Sanjo N, Nakamura A, Ikeda K, Tsuchiya K, et al. Increased expression of neuronal apolipoprotein E in human brain with cerebral infarction. Stroke 2003;34:87580. [128] Kamada H, Sato K, Zhang WR, Omori N, Nagano I, Shoji M, et al. Spatiotemporal changes of apolipoprotein E immunoreactivity and apolipoprotein E mRNA expression after transient middle cerebral artery occlusion in rat brain. J Neurosci Res 2003;73:54556. [129] Nishio M, Kohmura E, Yuguchi T, Nakajima Y, Fujinaka T, Akiyama C, et al. Neuronal apolipoprotein E is not synthesized in neuron after focal ischemia in rat brain. Neurol Res 2003;25:3904. [130] Valenza M, Leoni V, Karasinska JM, Petricca L, Fan J, Carroll J, et al. Cholesterol defect is marked across multiple rodent models of Huntingtons disease and is manifest in astrocytes. J Neurosci 2010;30:1084450. [131] Franz G, Reindl M, Patel SC, Beer R, Unterrichter I, Berger T, et al. Increased expression of apolipoprotein D following experimental traumatic brain injury. J Neurochem 1999;73:161525. [132] Tao R, Aldskogius H. Glial cell responses, complement and apolipoprotein J expression following axon injury in the neonatal rat. J Neurocytol 1999;28:55970. [133] Belloir B, Kovari E, Surini-Demiri M, Savioz A. Altered apolipoprotein D expression in the brain of patients with Alzheimer disease. J Neurosci Res 2001;64:619. [134] Kadish I, Thibault O, Blalock EM, Chen KC, Gant JC, Porter NM, et al. Hippocampal and cognitive aging across the lifespan: a bioenergetic shift precedes and increased cholesterol trafcking parallels memory impairment. J Neurosci 2009;29:180516. [135] Amaratunga A, Abraham CR, Edwards RB, Sandell JH, Schreiber BM, Fine RE. Apolipoprotein E is synthesized in the retina by Muller glial cells, secreted into the vitreous, and rapidly transported into the optic nerve by retinal ganglion cells. J Biol Chem 1996;271:562832. [136] Borghini I, Barja F, Pometta D, James RW. Characterization of subpopulations of lipoprotein particles isolated from human cerebrospinal uid. Biochim Biophys Acta 1995;1255:192200. [137] Guyton JR, Miller SE, Martin ME, Khan WA, Roses AD, Strittmatter WJ. Novel large apolipoprotein E-containing lipoproteins of density 1.0061.060 g/ml in human cerebrospinal uid. J Neurochem 1998;70:123540. [138] LaDu MJ, Gilligan SM, Lukens JR, Cabana VG, Reardon CA, Van Eldik LJ, et al. Nascent astrocyte particles differ from lipoproteins in CSF. J Neurochem 1998;70:207081. [139] DeMattos RB, Brendza RP, Heuser JE, Kierson M, Cirrito JR, Fryer J, et al. Purication and characterization of astrocyte-secreted apolipoprotein E and J-containing lipoproteins from wild-type and human apoE transgenic mice. Neurochem Int 2001;39:41525. [140] Koch S, Donarski N, Goetze K, Kreckel M, Stuerenburg HJ, Buhmann C, et al. Characterization of four lipoprotein classes in human cerebrospinal uid. J Lipid Res 2001;42:114351.
368
F.W. Pfrieger, N. Ungerer / Progress in Lipid Research 50 (2011) 357371 [169] Shanmugaratnam J, Berg E, Kimerer L, Johnson RJ, Amaratunga A, Schreiber BM, et al. Retinal Muller glia secrete apolipoproteins E and J which are efciently assembled into lipoprotein particles. Brain Res Mol Brain Res 1997;50:11320. [170] Ito J, Zhang LY, Asai M, Yokoyama S. Differential generation of high-density lipoprotein by endogenous and exogenous apolipoproteins in cultured fetal rat astrocytes. J Neurochem 1999;72:23629. [171] Gong JS, Kobayashi M, Hayashi H, Zou K, Sawamura N, Fujita SC, et al. Apolipoprotein E (ApoE) isoform-dependent lipid release from astrocytes prepared from human ApoE3 and ApoE4 knock-in mice. J Biol Chem 2002;277:2991926. [172] Peng D, Song C, Reardon CA, Liao S, Getz GS. Lipoproteins produced by ApoE/ astrocytes infected with adenovirus expressing human ApoE. J Neurochem 2003;86:1391402. [173] Karten B, Hayashi H, Francis GA, Campenot RB, Vance DE, Vance JE. Generation and function of astroglial lipoproteins from Niemann-Pick type C1-decient mice. Biochem J 2005;387:77988. [174] Cahoy JD, Emery B, Kaushal A, Foo LC, Zamanian JL, Christopherson KS, et al. A transcriptome database for astrocytes, neurons, and oligodendrocytes: a new resource for understanding brain development and function. J Neurosci 2008;28:26478. [175] Fagan AM, Holtzman DM. Astrocyte lipoproteins, effects of apoE on neuronal function, and role of apoE in amyloid-beta deposition in vivo. Microsc Res Tech 2000;50:297304. [176] Yu C, Youmans KL, LaDu MJ. Proposed mechanism for lipoprotein remodelling in the brain. Biochim Biophys Acta 2010;1801:81923. [177] Hirsch-Reinshagen V, Donkin J, Stukas S, Chan J, Wilkinson A, Fan J, et al. Lecithin:cholesterol acyltransferase synthesized by primary astrocytes esteries cholesterol on glia-derived lipoproteins. J Lipid Res; 2008. [178] Johnson RC, Shah SN. Presence in human cerebrospinal uid of cholesterol esterifying enzyme utilizing free fatty acids. Brain Res 1979;162:3537. [179] Albers JJ, Marcovina SM, Christenson RH. Lecithin cholesterol acyltransferase in human cerebrospinal uid: reduced level in patients with multiple sclerosis and evidence of direct synthesis in the brain. Int J Clin Lab Res 1992;22:16972. [180] Demeester N, Castro G, Desrumaux C, De Geitere C, Fruchart JC, Santens P, et al. Characterization and functional studies of lipoproteins, lipid transfer proteins, and lecithin:cholesterol acyltransferase in CSF of normal individuals and patients with Alzheimers disease. J Lipid Res 2000;41:96374. [181] Hossain MA, Tsujita M, Akita N, Kobayashi F, Yokoyama S. Cholesterol homeostasis in ABCA1/LCAT double-decient mouse. Biochim Biophys Acta 2009;1791:1197205. [182] Hirsch-Reinshagen V, Donkin J, Stukas S, Chan J, Wilkinson A, Fan J, et al. LCAT synthesized by primary astrocytes esteries cholesterol on glia-derived lipoproteins. J Lipid Res 2009;50:88593. [183] Vance JE, Vance DE. The assembly of lipids into lipoproteins during secretion. Experientia 1990;46:5609. [184] Krimbou L, Marcil M, Genest J. New insights into the biogenesis of human high-density lipoproteins. Curr Opin Lipidol 2006;17:25867. [185] Oram JF, Heinecke JW. ATP-binding cassette transporter A1: a cell cholesterol exporter that protects against cardiovascular disease. Physiol Rev 2005;85:134372. [186] Vaughan AM, Oram JF. ABCA1 and ABCG1 or ABCG4 act sequentially to remove cellular cholesterol and generate cholesterol-rich HDL. J Lipid Res 2006;47:243343. [187] Kusuhara H, Sugiyama Y. ATP-binding cassette, subfamily G (ABCG family). Pugers Arch 2007;453:73544. [188] Kim WS, Weickert CS, Garner B. Role of ATP-binding cassette transporters in brain lipid transport and neurological disease. J Neurochem 2008;104:114566. [189] Fukumoto H, Deng A, Irizarry MC, Fitzgerald ML, Rebeck GW. Induction of the cholesterol transporter ABCA1 in central nervous system cells by liver x receptor agonists increases secreted abeta levels. J Biol Chem 2002;277:4850813. [190] Wellington CL, Walker EK, Suarez A, Kwok A, Bissada N, Singaraja R, et al. ABCA1 mRNA and protein distribution patterns predict multiple different roles and levels of regulation. Lab Invest 2002;82:27383. [191] Koldamova RP, Lefterov IM, Ikonomovic MD, Skoko J, Lefterov PI, Isanski BA, et al. 22R-hydroxycholesterol and 9-cis-retinoic acid induce ATP-binding cassette transporter A1 expression and cholesterol efux in brain cells and decrease amyloid beta secretion. J Biol Chem 2003;278:1324456. [192] Tarr PT, Edwards PA. ABCG1 and ABCG4 are coexpressed in neurons and astrocytes of the CNS and regulate cholesterol homeostasis through SREBP-2. J Lipid Res 2008;49:16982. [193] Bojanic DD, Tarr PT, Gale GD, Smith DJ, Bok D, Chen B, et al. Differential expression and function of ABCG1 and ABCG4 during development and aging. J Lipid Res 2010;51:16981. [194] Whitney KD, Watson MA, Collins JL, Benson WG, Stone TM, Numerick MJ, et al. Regulation of cholesterol homeostasis by the liver x receptors in the central nervous system. Mol Endocrinol 2002;16:137885. [195] Kim WS, Guillemin GJ, Glaros EN, Lim CK, Garner B. Quantitation of ATPbinding cassette subfamily-A transporter gene expression in primary human brain cells. Neuroreport 2006;17:8916. [196] Liang Y, Lin S, Beyer TP, Zhang Y, Wu X, Bales KR, et al. A liver X receptor and retinoid X receptor heterodimer mediates apolipoprotein E expression,
[141] Zhuo L, Theis M, Alvarez-Maya I, Brenner M, Willecke K, Messing A. HGFAPcre transgenic mice for manipulation of glial and neuronal function in vivo. Genesis 2001;31:8594. [142] Garcia AD, Doan NB, Imura T, Bush TG, Sofroniew MV. GFAP-expressing progenitors are the principal source of constitutive neurogenesis in adult mouse forebrain. Nat Neurosci 2004;7:123341. [143] Fagan AM, Holtzman DM, Munson G, Mathur T, Schneider D, Chang LK, et al. Unique lipoproteins secreted by primary astrocytes from wild type, apoE (/ ), and human apoE transgenic mice. J Biol Chem 1999;274:300017. [144] Karten B, Campenot RB, Vance DE, Vance JE. Expression of ABCG1, but not ABCA1, correlates with cholesterol release by cerebellar astroglia. J Biol Chem 2006;281:404957. [145] Piedrahita JA, Zhang SH, Hagaman JR, Oliver PM, Maeda N. Generation of mice carrying a mutant apolipoprotein E gene inactivated by gene targeting in embryonic stem cells. Proc Natl Acad Sci USA 1992;89:44715. [146] Plump AS, Smith JD, Hayek T, Aalto-Setala K, Walsh A, Verstuyft JG, et al. Severe hypercholesterolemia and atherosclerosis in apolipoprotein Edecient mice created by homologous recombination in ES cells. Cell 1992;71:34353. [147] Lomnitski L, Oron L, Sklan D, Michaelson DM. Distinct alterations in phospholipid metabolism in brains of apolipoprotein E-decient mice. J Neurosci Res 1999;58:58692. [148] Han X, Cheng H, Fryer JD, Fagan AM, Holtzman DM. Novel role for apolipoprotein E in the central nervous system. Modulation of sulfatide content. J Biol Chem 2003;278:804351. [149] Levi O, Lutjohann D, Devir A, von Bergmann K, Hartmann T, Michaelson DM. Regulation of hippocampal cholesterol metabolism by apoE and environmental stimulation. J Neurochem 2005;95:98797. [150] Gordon I, Grauer E, Genis I, Sehayek E, Michaelson DM. Memory decits and cholinergic impairments in apolipoprotein E-decient mice. Neurosci Lett 1995;199:14. [151] Krugers HJ, Mulder M, Korf J, Havekes L, de Kloet ER, Joels M. Altered synaptic plasticity in hippocampal CA1 area of apolipoprotein E decient mice. Neuroreport 1997;8:250510. [152] Oitzl MS, Mulder M, Lucassen PJ, Havekes LM, Grootendorst J, de Kloet ER. Severe learning decits in apolipoprotein E-knockout mice in a water maze task. Brain Res 1997;752:18996. [153] Anderson R, Barnes JC, Bliss TV, Cain DP, Cambon K, Davies HA, et al. Behavioural, physiological and morphological analysis of a line of apolipoprotein E knockout mouse. Neuroscience 1998;85:93110. [154] Fullerton SM, Strittmatter WJ, Matthew WD. Peripheral sensory nerve defects in apolipoprotein E knockout mice. Exp Neurol 1998;153:15663. [155] Raber J, Akana SF, Bhatnagar S, Dallman MF, Wong D, Mucke L. Hypothalamic-pituitary-adrenal dysfunction in Apoe(/) mice: possible role in behavioral and metabolic alterations. J Neurosci 2000;20:206471. [156] Hartman RE, Wozniak DF, Nardi A, Olney JW, Sartorius L, Holtzman DM. Behavioral phenotyping of GFAP-apoE3 and -apoE4 transgenic mice. apoE4 mice show profound working memory impairments in the absence of Alzheimers-like neuropathology. Exp Neurol 2001;170:32644. [157] Champagne D, Dupuy JB, Rochford J, Poirier J. Apolipoprotein E knockout mice display procedural decits in the Morris water maze: analysis of learning strategies in three versions of the task. Neuroscience 2002;114:64154. [158] Robertson J, Curley J, Kaye J, Quinn J, Pfankuch T, Raber J. ApoE isoforms and measures of anxiety in probable AD patients and Apoe/ mice. Neurobiol Aging 2005;26:63743. [159] Ong WY, Kumar U, Switzer RC, Sidhu A, Suresh G, Hu CY, et al. Neurodegeneration in Niemann-Pick type C disease mice. Exp Brain Res 2001;141:21831. [160] Ong JM, Zorapapel NC, Aoki AM, Brown DJ, Nesburn AB, Rich KA, et al. Impaired electroretinogram (ERG) response in apolipoprotein E-decient mice. Curr Eye Res 2003;27:1524. [161] Nathan BP, Yost J, Litherland MT, Struble RG, Switzer PV. Olfactory function in apoE knockout mice. Behav Brain Res 2004;150:17. [162] Guo Y, Zhang C, Du X, Nair U, Yoo TJ. Morphological and functional alterations of the cochlea in apolipoprotein E gene decient mice. Hear Res 2005;208:5467. [163] Hauser PS, Narayanaswami V, Ryan RO. Apolipoprotein E: from lipid transport to neurobiology. Prog Lipid Res 2011;50:6274. [164] Masliah E, Mallory M, Ge N, Alford M, Veinbergs I, Roses AD. Neurodegeneration in the central nervous system of apoE- decient mice. Exp Neurol 1995;136:10722. [165] Buttini M, Orth M, Bellosta S, Akeefe H, Pitas RE, Wyss-Coray T, et al. Expression of human apolipoprotein E3 or E4 in the brains of Apoe/ mice: isoform-specic effects on neurodegeneration. J Neurosci 1999;19:486780. [166] Igbavboa U, Avdulov NA, Chochina SV, Wood WG. Transbilayer distribution of cholesterol is modied in brain synaptic plasma membranes of knockout mice decient in the low-density lipoprotein receptor, apolipoprotein E, or both proteins. J Neurochem 1997;69:16617. [167] McLaughlin L, Zhu G, Mistry M, Ley-Ebert C, Stuart WD, Florio CJ, et al. Apolipoprotein J/clusterin limits the severity of murine autoimmune myocarditis. J Clin Invest 2000;106:110513. [168] Han BH, DeMattos RB, Dugan LL, Kim-Han JS, Brendza RP, Fryer JD, et al. Clusterin contributes to caspase-3-independent brain injury following neonatal hypoxia-ischemia. Nat Med 2001;7:33843.
F.W. Pfrieger, N. Ungerer / Progress in Lipid Research 50 (2011) 357371 secretion and cholesterol homeostasis in astrocytes. J Neurochem 2004;88:62334. Cao G, Bales KR, DeMattos RB, Paul SM. Liver X receptor-mediated gene regulation and cholesterol homeostasis in brain: relevance to Alzheimers disease therapeutics. Curr Alzheimer Res 2007;4:17984. Zhao C, Dahlman-Wright K. Liver X receptor in cholesterol metabolism. J Endocrinol 2010;204:23340. Abildayeva K, Jansen PJ, Hirsch-Reinshagen V, Bloks VW, Bakker AH, Ramaekers FC, et al. 24(S)-hydroxycholesterol participates in a liver X receptor-controlled pathway in astrocytes that regulates apolipoprotein Emediated cholesterol efux. J Biol Chem 2006;281:12799808. Wahrle SE, Jiang H, Parsadanian M, Legleiter J, Han X, Fryer JD, et al. ABCA1 is required for normal central nervous system ApoE levels and for lipidation of astrocyte-secreted apoE. J Biol Chem 2004;279:4098793. Hirsch-Reinshagen V, Zhou S, Burgess BL, Bernier L, McIsaac SA, Chan JY, et al. Deciency of ABCA1 impairs apolipoprotein E metabolism in brain. J Biol Chem 2004;279:41197207. Wahrle SE, Jiang H, Parsadanian M, Kim J, Li A, Knoten A, et al. Overexpression of ABCA1 reduces amyloid deposition in the PDAPP mouse model of Alzheimer disease. J Clin Invest 2008;118:67182. Wollmer MA, Streffer JR, Lutjohann D, Tsolaki M, Iakovidou V, Hegi T, et al. ABCA1 modulates CSF cholesterol levels and inuences the age at onset of Alzheimers disease. Neurobiol Aging 2003;24:4216. Burgess BL, Parkinson PF, Racke MM, Hirsch-Reinshagen V, Fan J, Wong C, et al. ABCG1 inuences the brain cholesterol biosynthetic pathway but does not affect amyloid precursor protein or apolipoprotein E metabolism in vivo. J Lipid Res 2008;49:125467. Matsuo M, Campenot RB, Vance DE, Ueda K, Vance JE. Involvement of lowdensity lipoprotein receptor-related protein and ABCG1 in stimulation of axonal extension by apoE-containing lipoproteins. Biochim Biophys Acta 2011;1811:318. Stone DJ, Rozovsky I, Morgan TE, Anderson CP, Hajian H, Finch CE. Astrocytes and microglia respond to estrogen with increased apoE mRNA in vivo and in vitro. Exp Neurol 1997;143:3138. Oropeza RL, Wekerle H, Werb Z. Expression of apolipoprotein E by mouse brain astrocytes and its modulation by interferon-gamma. Brain Res 1987;410:4551. Ueno S, Ito J, Nagayasu Y, Furukawa T, Yokoyama S. An acidic broblast growth factor-like factor secreted into the brain cell culture medium upregulates apoE synthesis, HDL secretion and cholesterol metabolism in rat astrocytes. Biochim Biophys Acta 2002;1589:26172. Ito J, Nagayasu Y, Lu R, Kheirollah A, Hayashi M, Yokoyama S. Astrocytes produce and secrete FGF-1, which promotes the production of apoE-HDL in a manner of autocrine action. J Lipid Res 2005;46:67986. Cedazo-Minguez A, Hamker U, Meske V, Veh RW, Hellweg R, Jacobi C, et al. Regulation of apolipoprotein E secretion in rat primary hippocampal astrocyte cultures. Neuroscience 2001;105:65161. Ballerini P, Ciccarelli R, Di Iorio P, Buccella S, DAlimonte I, Giuliani P, et al. Guanosine effect on cholesterol efux and apolipoprotein E expression in astrocytes. Purinergic Signal 2006;2:63749. Brown MS, Goldstein JL. A receptor-mediated pathway for cholesterol homeostasis. Science 1986;232:3447. Herz J. Apolipoprotein E receptors in the nervous system. Curr Opin Lipidol 2009;20:1906. Swanson LW, Simmons DM, Hofmann SL, Goldstein JL, Brown MS. Localization of mRNA for low density lipoprotein receptor and a cholesterol synthetic enzyme in rabbit nervous system by in situ hybridization. Proc Natl Acad Sci USA 1988;85:98215. Moestrup SK, Gliemann J, Pallesen G. Distribution of the alpha 2macroglobulin receptor/low density lipoprotein receptor-related protein in human tissues. Cell Tissue Res 1992;269:37582. Wolf BB, Lopes MB, VandenBerg SR, Gonias SL. Characterization and immunohistochemical localization of alpha 2-macroglobulin receptor (lowdensity lipoprotein receptor-related protein) in human brain. Am J Pathol 1992;141:3742. Rebeck GW, Reiter JS, Strickland DK, Hyman BT. Apolipoprotein E in sporadic Alzheimers disease: allelic variation and receptor interactions. Neuron 1993;11:57580. Bu G, Maksymovitch EA, Nerbonne JM, Schwartz AL. Expression and function of the low density lipoprotein receptor-related protein (LRP) in mammalian central neurons. J Biol Chem 1994;269:185218. Ishiguro M, Imai Y, Kohsaka S. Expression and distribution of low density lipoprotein receptor-related protein mRNA in the rat central nervous system. Brain Res Mol Brain Res 1995;33:3746. Tooyama I, Kawamata T, Akiyama H, Moestrup SK, Gliemann J, McGeer PL. Immunohistochemical study of alpha 2 macroglobulin receptor in Alzheimer and control postmortem human brain. Mol Chem Neuropathol 1993;18:15360. Tooyama I, Kawamata T, Akiyama H, Kimura H, Moestrup SK, Gliemann J, et al. Subcellular localization of the low density lipoprotein receptor-related protein (alpha 2-macroglobulin receptor) in human brain. Brain Res 1995;691:2358. Handelmann GE, Boyles JK, Weisgraber KH, Mahley RW, Pitas RE. Effects of apolipoprotein E, beta-very low density lipoproteins, and cholesterol on the extension of neurites by rabbit dorsal root ganglion neurons in vitro. J Lipid Res 1992;33:167788.
369
[197]
[198] [199]
[200]
[201]
[202]
[203]
[204]
[205]
[206]
[207]
[208]
[209]
[210]
[211]
[212] [213] [214]
[215]
[216]
[217]
[218]
[219]
[220]
[221]
[222]
[223] Rapp A, Gmeiner B, Huttinger M. Implication of apoE isoforms in cholesterol metabolism by primary rat hippocampal neurons and astrocytes. Biochimie 2006;88:47383. [224] Posse De Chaves EI, Vance DE, Campenot RB, Kiss RS, Vance JE. Uptake of lipoproteins for axonal growth of sympathetic neurons. J Biol Chem 2000;275:1988390. [225] Boyles JK, Zoellner CD, Anderson LJ, Kosik LM, Pitas RE, Weisgraber KH, et al. A role for apolipoprotein E, apolipoprotein A-I, and low density lipoprotein receptors in cholesterol transport during regeneration and remyelination of the rat sciatic nerve. J Clin Invest 1989;83:101531. [226] Lopes MB, Bogaev CA, Gonias SL, VandenBerg SR. Expression of alpha 2macroglobulin receptor/low density lipoprotein receptor-related protein is increased in reactive and neoplastic glial cells. FEBS Lett 1994;338:3015. [227] Silverman MA, Kaech S, Jareb M, Burack MA, Vogt L, Sonderegger P, et al. Sorting and directed transport of membrane proteins during development of hippocampal neurons in culture. Proc Natl Acad Sci USA 2001;98:70517. [228] Hayashi H, Campenot RB, Vance DE, Vance JE. Glial lipoproteins stimulate axon growth of central nervous system neurons in compartmented cultures. J Biol Chem 2004;279:1400915. [229] Brown MD, Banker GA, Hussaini IM, Gonias SL, VandenBerg SR. Low density lipoprotein receptor-related protein is expressed early and becomes restricted to a somatodendritic domain during neuronal differentiation in culture. Brain Res 1997;747:3137. [230] Narita M, Bu G, Holtzman DM, Schwartz AL. The low-density lipoprotein receptor-related protein, a multifunctional apolipoprotein E receptor, modulates hippocampal neurite development. J Neurochem 1997;68:58795. [231] Jareb M, Banker G. The polarized sorting of membrane proteins expressed in cultured hippocampal neurons using viral vectors. Neuron 1998;20:85567. [232] May P, Rohlmann A, Bock HH, Zurhove K, Marth JD, Schomburg ED, et al. Neuronal LRP1 functionally associates with postsynaptic proteins and is required for normal motor function in mice. Mol Cell Biol 2004;24:887283. [233] Rothe T, Muller HW. Uptake of endoneurial lipoprotein into Schwann cells and sensory neurons is mediated by low density lipoprotein receptors and stimulated after axonal injury. J Neurochem 1991;57:201625. [234] Nathan BP, Bellosta S, Sanan DA, Weisgraber KH, Mahley RW, Pitas RE. Differential effects of apolipoproteins E3 and E4 on neuronal growth in vitro. Science 1994;264:8502. [235] Herz J, Bock HH. Lipoprotein receptors in the nervous system. Annu Rev Biochem 2002;71:40534. [236] Mauch DH, Ngler K, Schumacher S, Gritz C, Mller EC, Otto A, et al. CNS synaptogenesis promoted by glia-derived cholesterol. Science 2001;294:13547. [237] Sun Y, Wu S, Bu G, Onifade MK, Patel SN, LaDu MJ, et al. Glial brillary acidic protein-apolipoprotein E (apoE) transgenic mice. astrocyte-specic expression and differing biological effects of astrocyte-secreted apoE3 and apoE4 lipoproteins. J Neurosci 1998;18:326172. [238] Holtzman DM, Pitas RE, Kilbridge J, Nathan B, Mahley RW, Bu G, et al. Low density lipoprotein receptor-related protein mediates apolipoprotein Edependent neurite outgrowth in a central nervous system-derived neuronal cell line. Proc Natl Acad Sci USA 1995;92:94804. [239] Fagan AM, Bu G, Sun Y, Daugherty A, Holtzman DM. Apolipoprotein Econtaining high density lipoprotein promotes neurite outgrowth and is a ligand for the low density lipoprotein receptor-related protein. J Biol Chem 1996;271:301215. [240] Sakai K, Tiebel O, Ljungberg MC, Sullivan M, Lee HJ, Terashima T, et al. A neuronal VLDLR variant lacking the third complement-type repeat exhibits high capacity binding of apoE containing lipoproteins. Brain Res 2009;1276:1121. [241] Fryer JD, DeMattos RB, McCormick LM, ODell MA, Spinner ML, Bales KR, et al. The low density lipoprotein receptor regulates the level of central nervous system human and murine apolipoprotein E but does not modify amyloid plaque pathology in PDAPP mice. J Biol Chem 2005;280:257549. [242] Liu Q, Zerbinatti CV, Zhang J, Hoe HS, Wang B, Cole SL, et al. Amyloid precursor protein regulates brain apolipoprotein E and cholesterol metabolism through lipoprotein receptor LRP1. Neuron 2007;56:6678. [243] Liu Q, Trotter J, Zhang J, Peters MM, Cheng H, Bao J, et al. Neuronal LRP1 knockout in adult mice leads to impaired brain lipid metabolism and progressive, age-dependent synapse loss and neurodegeneration. J Neurosci 2010;30:1706878. [244] Zerbinatti CV, Wahrle SE, Kim H, Cam JA, Bales K, Paul SM, et al. Apolipoprotein E and low density lipoprotein receptor-related protein facilitate intraneuronal Abeta42 accumulation in amyloid model mice. J Biol Chem 2006;281:361806. [245] Ikonen E, Holtta-Vuori M. Cellular pathology of Niemann-Pick type C disease. Semin Cell Dev Biol 2004;15:44554. [246] Garver WS, Francis GA, Jelinek D, Shepherd G, Flynn J, Castro G, et al. The National Niemann-Pick C1 disease database: report of clinical features and health problems. Am J Med Genet A 2007;143A:120411. [247] Imrie J, Dasgupta S, Besley GT, Harris C, Heptinstall L, Knight S, et al. The natural history of Niemann-Pick disease type C in the UK. J Inherit Metab Dis 2007;30:519. [248] Sevin M, Lesca G, Baumann N, Millat G, Lyon-Caen O, Vanier MT, et al. The adult form of Niemann-Pick disease type C. Brain 2007;130:12033. [249] Spiegel R, Raas-Rothschild A, Reish O, Regev M, Meiner V, Bargal R, et al. The clinical spectrum of fetal Niemann-Pick type C. Am J Med Genet A 2009;149A:44650.
370
F.W. Pfrieger, N. Ungerer / Progress in Lipid Research 50 (2011) 357371 metabolism and neurotrophin responsiveness. J Biol Chem 2000;275:2017987. Yu W, Gong JS, Ko M, Garver WS, Yanagisawa K, Michikawa M. Altered cholesterol metabolism in Niemann-Pick type C1 mouse brains affects mitochondrial function. J Biol Chem 2005;280:117319. Sawamura N, Gong JS, Garver WS, Heidenreich RA, Ninomiya H, Ohno K, et al. Site-specic phosphorylation of tau accompanied by activation of mitogenactivated protein kinase (MAPK) in brains of Niemann-Pick type C mice. J Biol Chem 2001;276:103149. Bu B, Li J, Davies P, Vincent I. Deregulation of cdk5, hyperphosphorylation, and cytoskeletal pathology in the Niemann-Pick type C murine model. J Neurosci 2002;22:651525. Amritraj A, Peake K, Kodam A, Salio C, Merighi A, Vance JE, et al. Increased activity and altered subcellular distribution of lysosomal enzymes determine neuronal vulnerability in Niemann-Pick type C1-decient mice. Am J Pathol 2009;175:254056. Goodman JM. Demonstrated and inferred metabolism associated with cytosolic lipid droplets. J Lipid Res 2009;50:214856. Olofsson SO, Bostrom P, Andersson L, Rutberg M, Perman J, Boren J. Lipid droplets as dynamic organelles connecting storage and efux of lipids. Biochim Biophys Acta 2009;1791:44858. Chang TY, Li BL, Chang CC, Urano Y. Acyl-coenzyme A:cholesterol acyltransferases. Am J Physiol Endocrinol Metab 2009;297:E19. Johnson RC, Shah SN. Cholesterol ester metabolizing enzymes in human brain: properties, subcellular distribution and relative levels in various diseased conditions. J Neurochem 1978;31:895902. Choi MU, Suzuki K. A cholesterol-esterifying enzyme in rat central nervous system myelin. J Neurochem 1978;31:87985. Marco C, Morillas LG, Garcia-Peregrin E. Acyl coenzyme A:cholesterol acyltransferase in neonatal chick brain. Biochim Biophys Acta 1986;875:599604. Bryleva EY, Rogers MA, Chang CC, Buen F, Harris BT, Rousselet E, et al. ACAT1 gene ablation increases 24(S)-hydroxycholesterol content in the brain and ameliorates amyloid pathology in mice with AD. Proc Natl Acad Sci USA 2010;107:30816. Liu B, Turley SD, Burns DK, Miller AM, Repa JJ, Dietschy JM. Reversal of defective lysosomal transport in NPC disease ameliorates liver dysfunction and neurodegeneration in the npc1/ mouse. Proc Natl Acad Sci USA 2009;106:237782. Uelmen PJ, Oka K, Sullivan M, Chang CC, Chang TY, Chan L. Tissue-specic expression and cholesterol regulation of acylcoenzyme A:cholesterol acyltransferase (ACAT) in mice. Molecular cloning of mouse ACAT cDNA, chromosomal localization, and regulation of ACAT in vivo and in vitro. J Biol Chem 1995;270:26192201. Mulas MF, Demuro G, Mulas C, Putzolu M, Cavallini G, Donati A, et al. Dietary restriction counteracts age-related changes in cholesterol metabolism in the rat. Mech Ageing Dev 2005;126:64854. Hutter-Paier B, Huttunen HJ, Puglielli L, Eckman CB, Kim DY, Hofmeister A, et al. The ACAT inhibitor CP-113, 818 markedly reduces amyloid pathology in a mouse model of Alzheimers disease. Neuron 2004;44:22738. Wollmer MA, Streffer JR, Tsolaki M, Grimaldi LM, Lutjohann D, Thal D, et al. Genetic association of acyl-coenzyme A: cholesterol acyltransferase with cerebrospinal uid cholesterol levels, brain amyloid load, and risk for Alzheimers disease. Mol Psychiatry 2003;8:6358. Sakashita N, Miyazaki A, Takeya M, Horiuchi S, Chang CC, Chang TY, et al. Localization of human acyl-coenzyme A: cholesterol acyltransferase-1 (ACAT1) in macrophages and in various tissues. Am J Pathol 2000;156:22736. Puglielli L, Konopka G, Pack-Chung E, Ingano LA, Berezovska O, Hyman BT, et al. Acyl-coenzyme A: cholesterol acyltransferase modulates the generation of the amyloid beta-peptide. Nat Cell Biol 2001;3:90512. FRISCO SDI, RUGGIERI PDE, ERCOLI A. Isolation of cerebrosterol from human brain.. Boll Soc Ital Biol Sper 1953;29:13512. Lutjohann D, Breuer O, Ahlborg G, Nennesmo I, Siden A, Diczfalusy U, et al. Cholesterol homeostasis in human brain: evidence for an age-dependent ux of 24S-hydroxycholesterol from the brain into the circulation. Proc Natl Acad Sci USA 1996;93:9799804. Bjorkhem I, Lutjohann D, Diczfalusy U, Stahle L, Ahlborg G, Wahren J. Cholesterol homeostasis in human brain: turnover of 24S-hydroxycholesterol and evidence for a cerebral origin of most of this oxysterol in the circulation. J Lipid Res 1998;39:1594600. Bjorkhem I, Andersson U, Ellis E, Alvelius G, Ellegard L, Diczfalusy U, et al. From brain to bile. Evidence that conjugation and omega-hydroxylation are important for elimination of 24S-hydroxycholesterol (cerebrosterol) in humans. J Biol Chem 2001;276:3700410. Bjorkhem I. Crossing the barrier: oxysterols as cholesterol transporters and metabolic modulators in the brain. J Intern Med 2006;260:493508. Meaney S, Bodin K, Diczfalusy U, Bjorkhem I. On the rate of translocation in vitro and kinetics in vivo of the major oxysterols in human circulation: critical importance of the position of the oxygen function. J Lipid Res 2002;43:21305. Wang Y, Muneton S, Sjovall J, Jovanovic JN, Grifths WJ. The effect of 24Shydroxycholesterol on cholesterol homeostasis in neurons: quantitative changes to the cortical neuron proteome. J Proteome Res 2008;7:160614. Sacchetti P, Sousa KM, Hall AC, Liste I, Steffensen KR, Theolopoulos S, et al. Liver X receptors and oxysterols promote ventral midbrain neurogenesis in vivo and in human embryonic stem cells. Cell Stem Cell 2009;5:40919.
[250] Vanier MT. Niemann-Pick disease type C. Orphanet J Rare Dis 2010;5:16. [251] Carstea ED, Morris JA, Coleman KG, Loftus SK, Zhang D, Cummings C, et al. Niemann-Pick C1 disease gene: homology to mediators of cholesterol homeostasis. Science 1997;277:22831. [252] Naureckiene S, Sleat D, Lackland H, Fensom A, Vanier MT, Wattiaux R, et al. Identication of HE1 as the second gene of Niemann-Pick C disease. Science 2000;290:2298301. [253] Kwon HJ, Abi-Mosleh L, Wang ML, Deisenhofer J, Goldstein JL, Brown MS, et al. Structure of N-terminal domain of NPC1 reveals distinct subdomains for binding and transfer of cholesterol. Cell 2009;137:121324. [254] Sokol J, Blanchette-Mackie J, Kruth HS, Dwyer NK, Amende LM, Butler JD, et al. Type C Niemann-Pick disease. Lysosomal accumulation and defective intracellular mobilization of low density lipoprotein cholesterol. J Biol Chem 1988;263:34117. [255] Liscum L, Faust JR. The intracellular transport of low density lipoproteinderived cholesterol is inhibited in Chinese hamster ovary cells cultured with 3-beta-[2-(diethylamino)ethoxy]androst-5-en-17-one. J Biol Chem 1989;264:11796806. [256] Zervas M, Dobrenis K, Walkley SU. Neurons in Niemann-Pick disease type C accumulate gangliosides as well as unesteried cholesterol and undergo dendritic and axonal alterations. J Neuropathol Exp Neurol 2001;60:4964. [257] Reid PC, Sakashita N, Sugii S, Ohno-Iwashita Y, Shimada Y, Hickey WF, et al. A novel cholesterol stain reveals early neuronal cholesterol accumulation in the Niemann-Pick type C1 mouse brain. J Lipid Res 2004;45:58291. [258] German DC, Liang CL, Song T, Yazdani U, Xie C, Dietschy JM. Neurodegeneration in the Niemann-Pick C mouse: glial involvement. Neuroscience 2002;109:43750. [259] Walkley SU, Suzuki K. Consequences of NPC1 and NPC2 loss of function in mammalian neurons. Biochim Biophys Acta 2004;1685:4862. [260] Yamada A, Saji M, Ukita Y, Shinoda Y, Taniguchi M, Higaki K, et al. Progressive neuronal loss in the ventral posterior lateral and medial nuclei of thalamus in Niemann-Pick disease type C mouse brain. Brain Dev 2001;23:28897. [261] Sarna JR, Larouche M, Marzban H, Sillitoe RV, Rancourt DE, Hawkes R. Patterned Purkinje cell degeneration in mouse models of Niemann-Pick type C disease. J Comp Neurol 2003;456:27991. [262] Claudepierre T, Paques M, Simonutti M, Buard I, Sahel J, Maue RA, et al. Lack of Niemann Pick type C1 induces age-related degeneration in the mouse retina. Mol Cell Neurosci 2010;43:16476. [263] Patel SC, Suresh S, Kumar U, Hu CY, Cooney A, Blanchette-Mackie EJ, et al. Localization of Niemann-Pick C1 protein in astrocytes: implications for neuronal degeneration in Niemann- Pick type C disease. Proc Natl Acad Sci USA 1999;96:165762. [264] Hu CY, Ong WY, Patel SC. Regional distribution of NPC1 protein in monkey brain. J Neurocytol 2000;29:76573. [265] Prasad A, Fischer WA, Maue RA, Henderson LP. Regional and developmental expression of the Npc1 mRNA in the mouse brain. J Neurochem 2000;75:12507. [266] Ong WY, Sundaram RK, Huang E, Ghoshal S, Kumar U, Pentchev PG, et al. Neuronal localization and association of Niemann Pick C2 protein (HE1/ NPC2) with the postsynaptic density. Neuroscience 2004;128:56170. [267] Baudry M, Yao Y, Simmons D, Liu J, Bi X. Postnatal development of inammation in a murine model of Niemann-Pick type C disease: immunohistochemical observations of microglia and astroglia. Exp Neurol 2003;184:887903. [268] Ko DC, Milenkovic L, Beier SM, Manuel H, Buchanan J, Scott MP. Cellautonomous death of cerebellar purkinje neurons with autophagy in Niemann-Pick type C disease. PLoS Genet 2005;1:8195. [269] Elrick MJ, Pacheco CD, Yu T, Dadgar N, Shakkottai VG, Ware C, et al. Conditional Niemann-Pick C mice demonstrate cell autonomous Purkinje cell neurodegeneration. Hum Mol Genet 2010;19:83747. [270] Lopez ME, Klein AD, Dimbil UJ, Scott MP. Anatomically dened neuron-based rescue of neurodegenerative Niemann-Pick type C disorder. J Neurosci 2011;31:436778. [271] Zhang M, Strnatka D, Donohue C, Hallows JL, Vincent I, Erickson RP. Astrocyte-only Npc1 reduces neuronal cholesterol and triples life span of Npc1/ mice. J Neurosci Res 2008;86:284856. [272] Liao G, Yao Y, Liu J, Yu Z, Cheung S, Xie A, et al. Cholesterol accumulation is associated with lysosomal dysfunction and autophagic stress in Npc1/ mouse brain. Am J Pathol 2007;171:96275. [273] Bi X, Liao G. Autophagic-lysosomal dysfunction and neurodegeneration in Niemann-Pick Type C mice. lipid starvation or indigestion? Autophagy 2007;3:6468. [274] Karten B, Campenot RB, Vance DE, Vance JE. The Niemann-Pick C1 protein in recycling endosomes of presynaptic nerve terminals. J Lipid Res 2006;47:50414. [275] Wasser CR, Ertunc M, Liu X, Kavalali ET. Cholesterol-dependent balance between evoked and spontaneous synaptic vesicle recycling. J Physiol 2007;579:41329. [276] Hawes CM, Wiemer H, Krueger SR, Karten B. Pre-synaptic defects of NPC1decient hippocampal neurons are not directly related to plasma membrane cholesterol. J Neurochem 2010;114:31122. [277] Xu S, Zhou S, Xia D, Xia J, Chen G, Duan S, et al. Defects of synaptic vesicle turnover at excitatory and inhibitory synapses in Niemann-Pick C1-decient neurons. Neuroscience 2010;167:60820. [278] Henderson LP, Lin L, Prasad A, Paul CA, Chang TY, Maue RA. Embryonic striatal neurons from niemann-pick type C mice exhibit defects in cholesterol
[279]
[280]
[281]
[282]
[283] [284]
[285] [286]
[287] [288]
[289]
[290]
[291]
[292]
[293]
[294]
[295]
[296]
[297] [298]
[299]
[300]
[301] [302]
[303]
[304]
F.W. Pfrieger, N. Ungerer / Progress in Lipid Research 50 (2011) 357371 [305] Kim WS, Rahmanto AS, Kamili A, Rye KA, Guillemin GJ, Gelissen IC, et al. Role of ABCG1 and ABCA1 in regulation of neuronal cholesterol efux to apolipoprotein E discs and suppression of amyloid-beta peptide generation. J Biol Chem 2007;282:285161. [306] Ohtsuki S, Ito S, Matsuda A, Hori S, Abe T, Terasaki T. Brain-to-blood elimination of 24S-hydroxycholesterol from rat brain is mediated by organic anion transporting polypeptide 2 (oatp2) at the blood-brain barrier. J Neurochem 2007;103:14308. [307] Raychaudhuri S, Prinz WA. The diverse functions of oxysterol-binding proteins. Annu Rev Cell Dev Biol 2010;26:15777. [308] Laitinen S, Olkkonen VM, Ehnholm C, Ikonen E. Family of human oxysterol binding protein (OSBP) homologues. A novel member implicated in brain sterol metabolism. J Lipid Res 1999;40:220411. [309] Lund EG, Guileyardo JM, Russell DW. cDNA cloning of cholesterol 24hydroxylase, a mediator of cholesterol homeostasis in the brain. Proc Natl Acad Sci USA 1999;96:723843. [310] Ohyama Y, Meaney S, Heverin M, Ekstrom L, Brafman A, Shar M, et al. Studies on the transcriptional regulation of cholesterol 24-hydroxylase (CYP46A1): marked insensitivity toward different regulatory axes. J Biol Chem 2006;281:381020. [311] Ramirez DM, Andersson S, Russell DW. Neuronal expression and subcellular localization of cholesterol 24-hydroxylase in the mouse brain. J Comp Neurol 2008;507:167693. [312] Bretillon L, Diczfalusy U, Bjorkhem I, Maire MA, Martine L, Joffre C, et al. Cholesterol-24S-hydroxylase (CYP46A1) is specically expressed in neurons of the neural retina. Curr Eye Res 2007;32:3616. [313] Pfrieger FW. Outsourcing in the brain: do neurons depend on cholesterol delivery by astrocytes? Bioessays 2003;25:728. [314] Cartagena CM, Ahmed F, Burns MP, Pajoohesh-Ganji A, Pak DT, Faden AI, et al. Cortical injury increases cholesterol 24S hydroxylase (Cyp46) levels in the rat brain. J Neurotrauma 2008;25:108798. [315] Bogdanovic N, Bretillon L, Lund EG, Diczfalusy U, Lannfelt L, Winblad B, et al. On the turnover of brain cholesterol in patients with Alzheimers disease. Abnormal induction of the cholesterol-catabolic enzyme CYP46 in glial cells. Neurosci Lett 2001;314:458. [316] Brown III J, Theisler C, Silberman S, Magnuson D, Gottardi-Littell N, Lee JM, et al. Differential expression of cholesterol hydroxylases in Alzheimers disease. J Biol Chem 2004;279:3467481. [317] He X, Jenner AM, Ong WY, Farooqui AA, Patel SC. Lovastatin modulates increased cholesterol and oxysterol levels and has a neuroprotective effect on rat hippocampal neurons after kainate injury. J Neuropathol Exp Neurol 2006;65:65263. [318] Tian G, Kong Q, Lai L, Ray-Chaudhury A, Liang Glenn LC. Increased expression of cholesterol 24S-hydroxylase results in disruption of glial glutamate transporter EAAT2 association with lipid rafts: a potential role in Alzheimers disease. J Neurochem; 2010. [319] Milagre I, Nunes MJ, Gama MJ, Silva RF, Pascussi JM, Lechner MC, et al. Transcriptional regulation of the human CYP46A1 brain-specic expression by Sp transcription factors. J Neurochem 2008;106:83549. [320] Zhang J, Akwa Y, el Etr M, Baulieu EE, Sjovall J. Metabolism of 27-, 25- and 24hydroxycholesterol in rat glial cells and neurons. Biochem J 1997;322(Pt 1):175-84. [321] Wong J, Quinn CM, Guillemin G, Brown AJ. Primary human astrocytes produce 24(S), 25-epoxycholesterol with implications for brain cholesterol homeostasis. J Neurochem 2007;103:176473.
371
[322] Lund EG, Xie C, Kotti T, Turley SD, Dietschy JM, Russell DW. Knockout of the cholesterol 24-hydroxylase gene in mice reveals a brain-specic mechanism of cholesterol turnover. J Biol Chem 2003;278:229808. [323] Xie C, Lund EG, Turley SD, Russell DW, Dietschy JM. Quantitation of two pathways for cholesterol excretion from the brain in normal mice and mice with neurodegeneration. J Lipid Res 2003;44:17809. [324] Repa JJ, Li H, Frank-Cannon TC, Valasek MA, Turley SD, Tansey MG, et al. Liver X receptor activation enhances cholesterol loss from the brain, decreases neuroinammation, and increases survival of the NPC1 mouse. J Neurosci 2007;27:1447080. [325] Tachikawa M, Watanabe M, Hori S, Fukaya M, Ohtsuki S, Asashima T, et al. Distinct spatio-temporal expression of ABCA and ABCG transporters in the developing and adult mouse brain. J Neurochem 2005;95:294304. [326] Tansley GH, Burgess BL, Bryan MT, Su Y, Hirsch-Reinshagen V, Pearce J, et al. The cholesterol transporter ABCG1 modulates the subcellular distribution and proteolytic processing of beta-amyloid precursor protein. J Lipid Res 2007;48:102234. [327] Minagawa H, Gong JS, Jung CG, Watanabe A, Lund-Katz S, Phillips MC, et al. Mechanism underlying apolipoprotein E (ApoE) isoform-dependent lipid efux from neural cells in culture. J Neurosci Res 2009;87:2498508. [328] Panzenboeck U, Balazs Z, Sovic A, Hrzenjak A, Levak-Frank S, Wintersperger A, et al. ABCA1 and scavenger receptor class B, type I, are modulators of reverse sterol transport at an in vitro bloodbrain barrier constituted of porcine brain capillary endothelial cells. J Biol Chem 2002;277:427819. [329] Gosselet F, Candela P, Sevin E, Berezowski V, Cecchelli R, Fenart L. Transcriptional proles of receptors and transporters involved in brain cholesterol homeostasis at the blood-brain barrier: use of an in vitro model. Brain Res 2009;1249:3442. [330] Zlokovic BV, Deane R, Sagare AP, Bell RD, Winkler EA. Low-density lipoprotein receptor-related protein-1: a serial clearance homeostatic mechanism controlling Alzheimers amyloid beta-peptide elimination from the brain. J Neurochem 2010;115:107789. [331] Husemann J, Silverstein SC. Expression of scavenger receptor class B, type I, by astrocytes and vascular smooth muscle cells in normal adult mouse and human brain and in Alzheimers disease brain. Am J Pathol 2001;158:82532. [332] Husemann J, Loike JD, Anankov R, Febbraio M, Silverstein SC. Scavenger receptors in neurobiology and neuropathology: their role on microglia and other cells of the nervous system. Glia 2002;40:195205. [333] Alarcon R, Fuenzalida C, Santibanez M, Von Bernhardi R. Expression of scavenger receptors in glial cells. Comparing the adhesion of astrocytes and microglia from neonatal rats to surface-bound beta-amyloid. J Biol Chem 2005;280:3040615. [334] Thanopoulou K, Fragkouli A, Stylianopoulou F, Georgopoulos S. Scavenger receptor class B type I (SR-BI) regulates perivascular macrophages and modies amyloid pathology in an Alzheimer mouse model. Proc Natl Acad Sci USA 2010;107:2081621. [335] Chang EH, Rigotti A, Huerta PT. Age-related inuence of the HDL receptor SRBI on synaptic plasticity and cognition. Neurobiol Aging 2009;30:40719. [336] Araque A, Carmignoto G, Haydon PG. Dynamic signaling between astrocytes and neurons. Annu Rev Physiol 2001;63:795813. [337] Pfrieger FW, Barres BA. New views on synapseglia interactions. Curr Opin Neurobiol 1996;6:61521.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Lampard Descent TreeDocument1 pageLampard Descent TreeWheeezzNo ratings yet
- Blue Brain Documentation 1Document24 pagesBlue Brain Documentation 1shamshad3579% (14)
- Kumpulan Quiz CourseraDocument13 pagesKumpulan Quiz CourseraNadya Azzahra Salsabilla SaragihNo ratings yet
- Christmas - We Three KingsDocument1 pageChristmas - We Three KingsWheeezzNo ratings yet
- No AirDocument1 pageNo AirWheeezzNo ratings yet
- Cat Power - SatisfactionDocument1 pageCat Power - SatisfactionWheeezzNo ratings yet
- R&J,,,CLRDocument3 pagesR&J,,,CLRWheeezzNo ratings yet
- Christmas - Jingle BellsDocument2 pagesChristmas - Jingle BellsWheeezzNo ratings yet
- Christmas - Oh Come All Ye FaithfulDocument1 pageChristmas - Oh Come All Ye FaithfulWheeezzNo ratings yet
- Christmas - Joy To The WorldDocument1 pageChristmas - Joy To The WorldWheeezzNo ratings yet
- Christmas - Jingle Bell RockDocument1 pageChristmas - Jingle Bell RockWheeezzNo ratings yet
- Christmas - The First NoelDocument1 pageChristmas - The First NoelWheeezzNo ratings yet
- Nothing reallyDocument1 pageNothing reallyWheeezzNo ratings yet
- It's Nothing There's Nothing in Here Really HuhDocument1 pageIt's Nothing There's Nothing in Here Really HuhWheeezzNo ratings yet
- It'sDocument1 pageIt'sWheeezzNo ratings yet
- It's Nothing There's Nothing in Here ReallyDocument1 pageIt's Nothing There's Nothing in Here ReallyWheeezzNo ratings yet
- It's Nothing There's Nothing in Here ReallyDocument1 pageIt's Nothing There's Nothing in Here ReallyWheeezzNo ratings yet
- Responses 2Document16 pagesResponses 2WheeezzNo ratings yet
- Responses 2Document16 pagesResponses 2WheeezzNo ratings yet
- InputDocument3 pagesInputWheeezzNo ratings yet
- Effect of Low Environmental Temperature On Performance and Blood System in Broiler Chickens (Gallus Domesticus)Document7 pagesEffect of Low Environmental Temperature On Performance and Blood System in Broiler Chickens (Gallus Domesticus)WheeezzNo ratings yet
- Effect of Low Environmental Temperature On Performance and Blood System in Broiler Chickens (Gallus Domesticus)Document7 pagesEffect of Low Environmental Temperature On Performance and Blood System in Broiler Chickens (Gallus Domesticus)WheeezzNo ratings yet
- Responses 2Document16 pagesResponses 2WheeezzNo ratings yet
- Modal SosialDocument10 pagesModal SosialWheeezzNo ratings yet
- An Integrated PR Media ModelDocument3 pagesAn Integrated PR Media ModelWheeezzNo ratings yet
- Modal SosialDocument10 pagesModal SosialWheeezzNo ratings yet
- Neuroplasticity - The Moldable BrainDocument24 pagesNeuroplasticity - The Moldable BrainWinnie Claire100% (1)
- Slideshare. Present YourselfDocument56 pagesSlideshare. Present YourselfGurpreet SinghNo ratings yet
- ITP ReviewerDocument8 pagesITP ReviewerBailey EtormaNo ratings yet
- Artificial Neural Networks Architecture ApplicationsDocument264 pagesArtificial Neural Networks Architecture ApplicationsRaamses Díaz75% (8)
- CH04 PPTDocument44 pagesCH04 PPTJalfeNo ratings yet
- Nervous System WorksheetDocument8 pagesNervous System WorksheetBeneNo ratings yet
- The Biochemistry of MemoryDocument9 pagesThe Biochemistry of Memoryfabrizio españaNo ratings yet
- SNNIM A 10T-SRAM Based Spiking-Neural-Network-In-Memory Architecture With Capacitance ComputationDocument5 pagesSNNIM A 10T-SRAM Based Spiking-Neural-Network-In-Memory Architecture With Capacitance ComputationPANTHADIP MAJINo ratings yet
- Exam 3 NotesDocument3 pagesExam 3 NotesStanley ChuNo ratings yet
- Genpsy 1ST SemDocument28 pagesGenpsy 1ST SemAubrey RosalesNo ratings yet
- Hormones and The Endocrine System: For Campbell Biology, Ninth EditionDocument106 pagesHormones and The Endocrine System: For Campbell Biology, Ninth EditionLaode Abdul KadirNo ratings yet
- From Neurons To Brain: Adaptive Self-Wiring of NeuronsDocument20 pagesFrom Neurons To Brain: Adaptive Self-Wiring of Neuronsgiulio141091No ratings yet
- Neuroscience Can Help To Build Personal Effectiveness: September 2016Document19 pagesNeuroscience Can Help To Build Personal Effectiveness: September 2016dgavrileNo ratings yet
- Neurons and Synapses: Essential Idea: Neurons Transmit The Message, Synapses Modulate The MessageDocument26 pagesNeurons and Synapses: Essential Idea: Neurons Transmit The Message, Synapses Modulate The MessageSeanLaiNo ratings yet
- The TETRA System - Mass UK Mind Control Technology and The Zombification of Britain's Police Is Now A RealityDocument2 pagesThe TETRA System - Mass UK Mind Control Technology and The Zombification of Britain's Police Is Now A RealityTimme de VuNo ratings yet
- Anatomy and Physiology of The Nervous SystemDocument5 pagesAnatomy and Physiology of The Nervous SystemNicole Anne TungolNo ratings yet
- NppcityDocument63 pagesNppcityMohammad JoharNo ratings yet
- 1st SemDocument158 pages1st SemSana chaudharyNo ratings yet
- Your Answers in The Corresponding Numbered Boxes ProvidedDocument8 pagesYour Answers in The Corresponding Numbered Boxes ProvidedHoàng NguyễnNo ratings yet
- The Connecting Mechanism of the Nervous SystemDocument11 pagesThe Connecting Mechanism of the Nervous SystemmitxieeeNo ratings yet
- BRAIN of TeensDocument36 pagesBRAIN of Teensfares HACIB100% (4)
- BENNETT, MAXWELL Virginia Woolf and Neuropsychiatry PDFDocument228 pagesBENNETT, MAXWELL Virginia Woolf and Neuropsychiatry PDFMaria Mercedes GodoyNo ratings yet
- Osmosis High-Yield Physiology - Medicalstudyzone - Com (Sürüklenen)Document87 pagesOsmosis High-Yield Physiology - Medicalstudyzone - Com (Sürüklenen)Dilay MercimekNo ratings yet
- Ncmb317 Lecture: Psychiatric Mental Health Nursing: Bachelor of Science in Nursing 3YBDocument5 pagesNcmb317 Lecture: Psychiatric Mental Health Nursing: Bachelor of Science in Nursing 3YB2 - GUEVARRA, KYLE JOSHUA M.No ratings yet
- Abnormal Psychology 8th Edition Oltmanns Test BankDocument62 pagesAbnormal Psychology 8th Edition Oltmanns Test BankWilliamGomezfsodk100% (1)
- Komunikasi Antar Sel: Donny Nauphar 2018 Fakultas Kedokteran Universitas Swadaya Gunung JatiDocument43 pagesKomunikasi Antar Sel: Donny Nauphar 2018 Fakultas Kedokteran Universitas Swadaya Gunung JatiMeliaNo ratings yet
- 2 - Neural NetworkDocument59 pages2 - Neural NetworkJitesh Behera100% (1)
- Copybook Physiology EnglishDocument143 pagesCopybook Physiology EnglishamrendraNo ratings yet