Professional Documents
Culture Documents
Cardiovascular
Uploaded by
MabesOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cardiovascular
Uploaded by
MabesCopyright:
Available Formats
The Heart Functions: 1.
Transports nutrients, hormones, waste materials, respiratory gases using blood by the pumping of the heart. 2. Ensure one way direction of blood flow. 3. Generates Blood Pressure 4. Routing Blood 5. Regulates Blood Supply Anatomy of the Heart Fist size; Hollow, cone shape; located in the thorax and flanked on each side of the lungs; Apex at 5th intercostals space mid clavicular line; Base is beneath the 2nd rib.
Importance of Knowing the Location of Heart 1. Physical Examination 2. Electrocardiogram (ECG) 3. Cardio Pulmonary Resuscitation (CPR) Covering of the Heart Pericardium Double sac of serous membrane that ENCLOSES THE HEART. Secretes PERICARDIAL FLUID that allows heart to beat easily without friction. a. Visceral Pericardium or Epicardium outermost layer; part of heart wall b. Parietal Pericardium protects the heart and attached it to diaphragm and sternum.
Serosa General Covering Pericarditis: Inflammation of Pericardium; Decrease of serous fluids that bind Pericardial Layers and interferes their movement. 3 Walls of the Heart (Outer to Inner) 1. Epicardium or Visceral Pericardium (Outermost) 2. Myocardium Middle Layer that contracts Bulk of Cardiac muscle reinforced by the Skeleton of the Heart 3. Endocardium Inner Layer that lines the heart chambers to allow smooth blood flow. 4 Heart Chambers 1. Right Atrium and Left Atrium (Superior Chamber) Receiving Chambers Blood flows under LOW PRESSURE from the main veins (SVC and IVC) to fill the Ventricles.
2. Right Ventricle and Left Ventricle (Inferior Chamber) Discharging Chambers; Actual Pumps of heart When ventricles contract, blood is pumped out from heart and goes into circulation under HIGH PRESSURE. Septum -Divides the heart longitudinally a. Interventricular Septum divides RV & LV b. Interatrial Septum divides RA and LA 4 Heart Valves
Prevents backflow of blood; ensure one way direction of flow of blood 1. Atrioventricular Valve Separates Atrium and Ventricles Prevents backflow of blood into Atrium when ventricles contract Opens during heart relaxation and closed when ventricles contract a. Tricuspid Valve or Right AV Valve Has 3 Cusps ; Prevents backflow of blood from RV to RA b. Bicuspid Valve of Left AV Valve Has 2 Cusps; Prevents backflow of blood from LV to LA Chordae Tendinae heart strings; white cord that attaches the cusps to ventricle walls
2. Semilunar Valve Separates Ventricles and Blood Vessel (Artery) Prevents backflow of blood into Ventricles when heart is relaxing Closed during heart relaxation and opens when ventricles contract a. Pulmonary Semilunar Valve or Right SV Valve Separates RV and Pulmonary Trunk Going to the Lungs b. Aortic Semilunar Valve or Left SV Separates LV and Aorta Going to Systemic Circulation at the base of Aorta
Blood Flow through the Heart 1.) First Circuit or Pulmonary Circulation Function: For Gas Exchange in the Lungs Blue: Deoxygenated Blood (VEINS) 1. 2. 3. 4. 5. 6. 7. Super Vena Cava and Inferior Vena Cava receives deoxygenated blood from the body. Right Atrium Tricuspid Valve (Right AV Valve) Right Ventricle Pulmonary Semilunar Valve or Right SV Valve (closes to prevent backflow to RV) Pulmonary Trunk Pulmonary Artery
2.) Second Circuit or Systemic Circulation Function: Supply Oxygen to Body Organs Red: Oxygenated Blood (ARTERY; Pulmonary Vein is exempted) 8. Lungs (Gas Exchange Oxygenated Blood) 9. Thru Pulmonary Vein (oxygenated blood back to Heart) 10. Left Atrium (receives oxygenated Blood) 11. Bicuspid Valve or Left SV Valve 12. Left Ventricle 13. Aortic Semilunar Valve or Left SV Valve 14. Aorta 15. Systemic Circulation (Body Organs) Arteries Capillaries Veins SVC and IVC Aorta Largest artery At the base of aorta (systemic) starts the blood supply to heart muscle (cardiac circulation)
Arterioles Smallest arteries
Arteries Largest blood vessel; takes oxygenated blood away from heart
Capillaries Smallest Blood Vessels
Venules Smallest veins
Superior and Inferior Vena Cava Largest veins; Main Veins Carries blood back to heart
CARDIAC CIRCULATION 1. Left and Right Coronary Arteries (oxygenated blood) Oxygenates and Nourishes the Heart Fills when heart relaxes Checked during Andiogram 2. Cardiac Veins (deoxygenated blood) 3. Coronary Sinus (deoxygenated blood) Enlarged blood vessel at the back of heart Blood coming from the heart 4. Right Atrium (deoxygenated blood) Conduction System of the Heart 1. Atrial Cells 60 bpm 2. Ventricular Cells 20 to 40 bpm 2 Controlling Systems to Regulate Heart Activity 1. Autonomic Nervous System (ANS) brakes and accelerators to increase & decrease heart rate 2. Intrinsic Conduction System Causes muscle depolarization in 1 direction; Sets basic heart rhythm Normal Contraction: 75 bpm Electrical Impulses 1. Sinoatrial Node (SA Node) Pacemaker of Heart located at Right Atrium; stimulate muscle to contract
2. 3. 4. 5. 6.
Atrioventricular Node (AV Node) Bundle of His Right andLeft bundle branches to Interventricular Septum Purkinje Fibers Wringing Contractions of Ventricles
Conditions that Interferes Electrical Impulses 1. 2. 3. 4. 5. 6. Heart Block impaired transmission of impulse from Atrium to Ventricle. Any Damage to Sinoatrial Node lowers heart rate Ischemia lack of oxygen to heart muscle that leads to Fibrillation. Fibrillation rapid and uncoordinated shuddering of heart muscle. Tachycardia increased HR (HR > 100 bmp); leads to Fibrillation Bradycardia decreased HR (HR < 60bmp)
Cardiac Cycle Events of 1 complete heartbeat when atria and ventricles contract and relax. Systole - heart contraction (ventricles contract) / Diastole - heart relaxes (ventricles relaxes) Average Heart Beat: 75 bpm Cardiac Cycle Length: 0.8 seconds 1. Mid to Late Diastole heart is in complete relaxation 2. Ventricular Systole ventricular contraction begins (systole) 3. Early Diastole ventricles relax Heart Sounds during Cardiac Cycle 1. Lub or S1 (SYSTOLE) closing of AV valves; ventricles contract sound is longer and louder 2. Dub or S2 (DIASTOLE) closing of SV valves ; ventricles relaxes sound is sharp and short Murmurs Abnormal heart sound (Swishing sound); Indicates valve problems Cardiac Output Amount of blood pumped by each side of the heart in one minute. Product of Heart Rate and Stroke Volume (HR x SV) Normal Cardiac Output: 5,000 ml Ex. Heart Rate is 75 bpm / Stroke Volume is 70ml / heart beat = 75 bpm x 70 ml / heart beat = 5,250 ml / min Average Adult Cardiac Output
Stroke Volume Volume of blood pumped out by a ventricle with each heartbeat Normal Stroke Volume: 5 6 L of blood per minute
Regulation of Stroke Volume 1. Starling Law of Heart The more cardiac muscles is stretched, the stronger contraction. 2. Venous Return Important factor in stretching of heart muscle. The amount of blood entering the heart and distending its ventricles. Factors affecting Heart Rate Increases Heart Rate SNS Stimulation (4Es) Epinephrine d/t SNS Stimulation Thyroxine Fever / Heat d/t low BP Loss of Blood or Hypovolemia d/t to low BP Fetus (highest heart rate of 140 160 bpm) Decreases Heart Rate PNS Stimulation Electrolyte Imbalance Cold Medicine (Cardiotonics) Age heart rate decreases with age Gender or Sex - after puberty, male pulse rate is lower than females
You might also like
- Physiology of The Cardiovascular System-CVSDocument56 pagesPhysiology of The Cardiovascular System-CVSAmanuel MaruNo ratings yet
- Cardiogenic ShockDocument14 pagesCardiogenic ShockZellanien hdNo ratings yet
- A Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisFrom EverandA Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisRating: 5 out of 5 stars5/5 (1)
- Heart PathophysiologyDocument20 pagesHeart PathophysiologyDoctorDrapion100% (2)
- Cardiovascular SystemDocument14 pagesCardiovascular SystemAthena Huynh100% (1)
- Hypnotherapy Scripts 6 Steve G Jones Ebook PDFDocument66 pagesHypnotherapy Scripts 6 Steve G Jones Ebook PDFjohannes2212100% (10)
- Lecture Notes on Anatomy and Physiology of the Cardiovascular SystemDocument18 pagesLecture Notes on Anatomy and Physiology of the Cardiovascular SystemLudwigJayBarayuga100% (5)
- Anatomy and Physiology of The Cardiovascular System Medical Surgical NursingDocument68 pagesAnatomy and Physiology of The Cardiovascular System Medical Surgical NursingFelix NjakeNo ratings yet
- Physiology of The Cardiovascular System-CVSDocument56 pagesPhysiology of The Cardiovascular System-CVSAmanuel MaruNo ratings yet
- Assignment On Anatomy and Physiology of Heart: Submitted By: Submitted To: Jayita Gayen Madam S. PoddarDocument10 pagesAssignment On Anatomy and Physiology of Heart: Submitted By: Submitted To: Jayita Gayen Madam S. PoddarJayita Gayen DuttaNo ratings yet
- Cardiovascular SystemDocument10 pagesCardiovascular Systemsurviving nursing school100% (2)
- Tongue in Complete DentureDocument8 pagesTongue in Complete DentureAman SachdevaNo ratings yet
- Anti Psychotic DrugsDocument2 pagesAnti Psychotic DrugscalfornianursingacadNo ratings yet
- Parenteral Therapy:: Intravenous Therapy (IVT) or VenipunctureDocument3 pagesParenteral Therapy:: Intravenous Therapy (IVT) or VenipunctureMabes100% (1)
- Therapeutic Diet NutritionistDocument3 pagesTherapeutic Diet NutritionistMabesNo ratings yet
- PainDocument3 pagesPainMabesNo ratings yet
- PositioningDocument3 pagesPositioningMabesNo ratings yet
- Acute Service Pain Handbook 2011Document116 pagesAcute Service Pain Handbook 2011Iskandar414No ratings yet
- Tumor ImmunologyDocument3 pagesTumor ImmunologyStaz Reiya KiraNo ratings yet
- Cardionursing 110207023802 Phpapp01Document18 pagesCardionursing 110207023802 Phpapp01arvinnnnNo ratings yet
- Heart Anatomy: LocationDocument45 pagesHeart Anatomy: LocationZaira100% (1)
- CHN GapuzDocument23 pagesCHN GapuzMabes100% (1)
- Taste and SmellDocument1 pageTaste and SmellMabesNo ratings yet
- Tonsillectomy Slides 050427Document62 pagesTonsillectomy Slides 050427Aidiel FikriNo ratings yet
- Basic or InstrumentsDocument21 pagesBasic or InstrumentsMabes100% (1)
- Cardiovascular System: Presented by DR Aparna Ramachandran Mds 1 Dept of Public Health DentistryDocument73 pagesCardiovascular System: Presented by DR Aparna Ramachandran Mds 1 Dept of Public Health DentistryAparna RamachandranNo ratings yet
- NPTE CArdio NotesDocument27 pagesNPTE CArdio NotesAubrey Vale SagunNo ratings yet
- B SCAN PPPDocument92 pagesB SCAN PPPSiva Wurity100% (1)
- Case Report Consent Form TemplateDocument2 pagesCase Report Consent Form TemplateDaniel Antonio Valderrama Merejildo100% (1)
- Prof Ad BON and NursesDocument7 pagesProf Ad BON and NursesMabesNo ratings yet
- Asepsis and InfectionDocument6 pagesAsepsis and InfectionMabes100% (1)
- Nervous SystemDocument11 pagesNervous SystemMabesNo ratings yet
- Lesson 3Document71 pagesLesson 3Angel joyce ValenciaNo ratings yet
- Suture and NeedlesDocument5 pagesSuture and NeedlesMabesNo ratings yet
- Patho - 21 HeartAdv - 211005 - 230536Document91 pagesPatho - 21 HeartAdv - 211005 - 230536Puranjay ChandelNo ratings yet
- The Heart: Basis of Life .?Document94 pagesThe Heart: Basis of Life .?Diksha AgrawalNo ratings yet
- The HeartDocument65 pagesThe HeartMichael SamaniegoNo ratings yet
- TM 8 TM 8only Clinical Exam of Heart and Circulatory System AGWEnglishDocument66 pagesTM 8 TM 8only Clinical Exam of Heart and Circulatory System AGWEnglishcellin rubianti azzharaNo ratings yet
- Cardiovascular System BSN 1Document16 pagesCardiovascular System BSN 1Arianne Jen GenotivaNo ratings yet
- Components of The Cardiovascular SystemDocument23 pagesComponents of The Cardiovascular SystemMr. DummyNo ratings yet
- Chapter 12 Card WPS OfficeDocument19 pagesChapter 12 Card WPS OfficeKaye CepedaNo ratings yet
- Cardio Notes 1Document8 pagesCardio Notes 1Lindsay Grace MandarioNo ratings yet
- The Cardiovascular SystemDocument13 pagesThe Cardiovascular SystemCaraDeleNo ratings yet
- The Anatomy of HeartDocument46 pagesThe Anatomy of HeartPrincess NavarroNo ratings yet
- EKG Study Guide RevisedDocument29 pagesEKG Study Guide Revisedflashyboy506No ratings yet
- Cardiovascular Oral Examination ReviewDocument6 pagesCardiovascular Oral Examination ReviewJewel BerbanoNo ratings yet
- Circulation NotesDocument2 pagesCirculation NotesBhkti MittalNo ratings yet
- Cardiovascular System Study GuideDocument11 pagesCardiovascular System Study GuideS. MartinezNo ratings yet
- Heart and Neck Vessels AssessmentDocument4 pagesHeart and Neck Vessels AssessmentAndrei PedrajetaNo ratings yet
- NCLEX Cardiac ReviewDocument8 pagesNCLEX Cardiac ReviewKaren HutchinsonNo ratings yet
- The Heart of The Matter by AseenDocument33 pagesThe Heart of The Matter by AseenSyedali FathimaNo ratings yet
- Ila College of Health Kuje: Cardiovascular SystemDocument24 pagesIla College of Health Kuje: Cardiovascular SystemDaniel DendaNo ratings yet
- Cardiovascular SystemDocument101 pagesCardiovascular SystemBanessa Mae GarcianoNo ratings yet
- The Circulatory SystemDocument53 pagesThe Circulatory SystemVera June RañesesNo ratings yet
- 2015A&PIntro CardiovascularHandoutDocument16 pages2015A&PIntro CardiovascularHandoutMaggieHameedNo ratings yet
- Cardiac Anatomy and Physiology: Iris Ken R. Rico, OTRPDocument90 pagesCardiac Anatomy and Physiology: Iris Ken R. Rico, OTRPAndra HijratulNo ratings yet
- Broc PatBrocENG 01 Us EpDocument16 pagesBroc PatBrocENG 01 Us EpAchmad Deddy FatoniNo ratings yet
- Chapter 2 - CardiovascularDocument74 pagesChapter 2 - CardiovascularNoriani ZakariaNo ratings yet
- Intercellular Control: The CirculationDocument16 pagesIntercellular Control: The CirculationHUAWEI HUAWEINo ratings yet
- Salcedo ANPH111 The Cardiovascular System23Document46 pagesSalcedo ANPH111 The Cardiovascular System23ajline.esto23No ratings yet
- T8-EIN-Klp 2 - Cardiovascular SystemDocument32 pagesT8-EIN-Klp 2 - Cardiovascular SystemninikchoirinidahNo ratings yet
- Cardiovascular SystemDocument41 pagesCardiovascular Systemmoneer chanceNo ratings yet
- Care of Patient With 1Document12 pagesCare of Patient With 1jrjr88No ratings yet
- CARDIOVASCULAR PHYSIOLOGY NOTESDocument20 pagesCARDIOVASCULAR PHYSIOLOGY NOTESVivek ChaudharyNo ratings yet
- Cardiology Study Guide SummaryDocument6 pagesCardiology Study Guide SummaryApril Danielle TeschNo ratings yet
- 8 Transport in AnimalsDocument24 pages8 Transport in AnimalsMariam ShehabNo ratings yet
- Cardiovasular SystemDocument5 pagesCardiovasular SystemAsher Eby VargeeseNo ratings yet
- Physiology of The Cardiovascular System-CVSDocument56 pagesPhysiology of The Cardiovascular System-CVSAmanuel MaruNo ratings yet
- The Cardiovascular System Parts of The Cardiovascular SystemDocument7 pagesThe Cardiovascular System Parts of The Cardiovascular SystemBrent AnosNo ratings yet
- Anatomy and Physiology of The HeartDocument21 pagesAnatomy and Physiology of The HeartNina OaipNo ratings yet
- Transport in Humans 2 Heart and Cardiac CycleDocument74 pagesTransport in Humans 2 Heart and Cardiac Cycleloycoy008No ratings yet
- Functions of Cardiovascular System:: The Gross AnatomyDocument6 pagesFunctions of Cardiovascular System:: The Gross AnatomyShreyasi PatankarNo ratings yet
- 1 Heart Anatomy and FunctionDocument38 pages1 Heart Anatomy and Functionsyanita dwi nanda Sulistyani putriNo ratings yet
- Circulatory Response To ExerciseDocument31 pagesCirculatory Response To ExerciseFarhad GulNo ratings yet
- Cardio PulmonaryDocument4 pagesCardio PulmonaryAyessa CortesNo ratings yet
- Circulatory System IIDocument13 pagesCirculatory System IIsmbdy tbhhhNo ratings yet
- First Question: Student's Name: Adel Sulaiman SectionDocument5 pagesFirst Question: Student's Name: Adel Sulaiman SectionDental LecturesMMQNo ratings yet
- Cardiovascular Assessment LectureDocument116 pagesCardiovascular Assessment LectureJohnryl FranciscoNo ratings yet
- Immediate Life Support for healthcare Practitioners: A Step-By-Step GuideFrom EverandImmediate Life Support for healthcare Practitioners: A Step-By-Step GuideNo ratings yet
- Bowel Diversion: Parameter Colostomy IleostomyDocument1 pageBowel Diversion: Parameter Colostomy IleostomyMabesNo ratings yet
- Commonly Asked Emergency DrugsDocument17 pagesCommonly Asked Emergency DrugsrianneNo ratings yet
- Pentagon CompilationDocument20 pagesPentagon CompilationMabesNo ratings yet
- Respiratory DiagnosticDocument3 pagesRespiratory DiagnosticMabesNo ratings yet
- Triage PrinciplesDocument2 pagesTriage PrinciplesMabesNo ratings yet
- Route of ParenteralDocument3 pagesRoute of ParenteralMabes100% (1)
- Decubitus Ulcer / Pressure SoresDocument1 pageDecubitus Ulcer / Pressure SoresMabesNo ratings yet
- Enema Administration: Size of Rectal TubeDocument3 pagesEnema Administration: Size of Rectal TubeMabesNo ratings yet
- DocumentationDocument3 pagesDocumentationMabesNo ratings yet
- Mabes Fluid and Electrolyte ImbalancesDocument15 pagesMabes Fluid and Electrolyte ImbalancesMabesNo ratings yet
- Blood Transfusion Purpose: 9. Check Blood For Presence of BubblesDocument2 pagesBlood Transfusion Purpose: 9. Check Blood For Presence of BubblesMabes100% (1)
- Bowel Elimination MabesDocument2 pagesBowel Elimination MabesMabesNo ratings yet
- Prof Ad JurisprudenceDocument7 pagesProf Ad JurisprudenceMabesNo ratings yet
- All Nursing TheoriesDocument26 pagesAll Nursing TheoriesMabesNo ratings yet
- Water Soluble VitaminsDocument6 pagesWater Soluble VitaminsMabesNo ratings yet
- Roses Are Red, Violets Are Blue, Without Your Lungs Your Blood Would Be, Too.Document249 pagesRoses Are Red, Violets Are Blue, Without Your Lungs Your Blood Would Be, Too.MabesNo ratings yet
- Nagrik Suraksha Individual Policy SummaryDocument10 pagesNagrik Suraksha Individual Policy SummarypayalNo ratings yet
- Ivf StudyDocument2 pagesIvf StudyDanePepitoNo ratings yet
- Katsuura 2016Document6 pagesKatsuura 2016Wahyu InsanNo ratings yet
- Disclosures: Kori Dewing, DNP, ARNP Virginia Mason Medical Center October 29, 2013Document3 pagesDisclosures: Kori Dewing, DNP, ARNP Virginia Mason Medical Center October 29, 2013Alexander Diaz ZuletaNo ratings yet
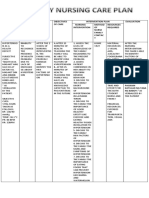
- Nursing Care Plan for a Client with Acute Gouty ArthritisDocument4 pagesNursing Care Plan for a Client with Acute Gouty ArthritisTikTok TrendzNo ratings yet
- MED - Post Review ExamDocument8 pagesMED - Post Review ExamFrederick BallesterosNo ratings yet
- Avi Kremer Case AnalysisDocument2 pagesAvi Kremer Case AnalysisSurya BakshiNo ratings yet
- Richard Zoumalan MD, FACSDocument3 pagesRichard Zoumalan MD, FACSBarney LivingstoneNo ratings yet
- Nebrasel Deen Othman - OriginalDocument3 pagesNebrasel Deen Othman - OriginalNebras OthmanNo ratings yet
- ICNCDRS Blindness Registry FormDocument4 pagesICNCDRS Blindness Registry FormAprilAngeliRobleNo ratings yet
- Antimicrobial ChemotherapyDocument160 pagesAntimicrobial Chemotherapyokumu atanas0% (1)
- Jurnal Pendukung 2Document13 pagesJurnal Pendukung 2Eko PrasNo ratings yet
- SOAP Handout 2010Document4 pagesSOAP Handout 2010wawanNo ratings yet
- Nelson FNCPDocument2 pagesNelson FNCPDenisse Shazz Mae MaretNo ratings yet
- Stages of Development of A Therapeutic RelationshipDocument3 pagesStages of Development of A Therapeutic RelationshipJoher Bolante MendezNo ratings yet
- Shëndeti Mendor I Fëmijlve Dhe Adoleshentëve Prizren Naim FanajDocument1 pageShëndeti Mendor I Fëmijlve Dhe Adoleshentëve Prizren Naim Fanajlulkuqe029No ratings yet
- Antifungal LectureDocument62 pagesAntifungal LectureVandana TayalNo ratings yet
- Rivotril 0.5mg Tablets Rivotril 2mg TabletsDocument4 pagesRivotril 0.5mg Tablets Rivotril 2mg TabletsМаргарет ВејдNo ratings yet
- Parotid Tumors and Other Salivary Gland TumorsDocument41 pagesParotid Tumors and Other Salivary Gland Tumorsdrhiwaomer100% (9)
- Assessing Body TemperatureDocument6 pagesAssessing Body TemperatureemailNo ratings yet
- Neurological Disorders Practice Test QuestionsDocument6 pagesNeurological Disorders Practice Test QuestionsBenedict AlvarezNo ratings yet
- Wiley Milbank Memorial FundDocument22 pagesWiley Milbank Memorial FundRob21aNo ratings yet
- TNM Staging Colorectal CADocument2 pagesTNM Staging Colorectal CAbubbrubb20063998No ratings yet