Professional Documents
Culture Documents
10.18.11 Foii
Uploaded by
Eddie MillsOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10.18.11 Foii
Uploaded by
Eddie MillsCopyright:
Available Formats
10.18.
11 FOII notes
I just want to finish up on the different modifications that we can incorporate into the appliances and then we are going to move into how to try and put some of this together into a coherent prescription which, of course as you will see has to be based on some knowledge of what it is that we are trying to treat. Just keep that in the back of your minds. You dont treat forefoot varus. What you are going to treat is a consequence of the forefoot varus. You treat the plantar fasciitis that the pt came in with. Which, by the way pts do not come in and say I have plantar fasciitis. They may well have been told this by other doctors and it may turn out to be a true case. But they will come in and say my heel hurts, my arch hurts on and on and on which we will then discover to be as a result of a plantar fasciitis, heel spur, nerve entrapment and so on. So as we are developing this, keep it all in the context. You have to discover the reason why they are there complaining of pain in the foot, narrow it down to a specific diagnosis based on in our world of biomechanics if it is a biomechanical etiology, what factors are causing this foot to break down to lead to this diagnosis causing that pain. And then we will go ahead and be able to neutralize as many of these influences as we can keeping in mind that some are controllable or capable of being neutralized and some are not. The end result of which hopefully will be a pt that maybe we cant eliminate ALL of their pain but pts, if you give them 5% relieve god bless you and you are their best friend. So this has to be a stages approach. Dispersion padding traditionally those of you that are in medicine if you have a lesion sub 2 usually you construct a little wing pad or a U-pad and often times,. If you are going to disperse say 2 or 3 you are going to disperse weight off of 3, traditionally the U pad will extend over. If you are looking to disperse 3, the wing pad will go over 2 and 4. If you have your apt/home and your responsible for painting it any holes you have to spackle. In a sense that is what you are trying to do with balance or dispersion padding.
You are trying to disperse as much of those GRFs across as broad a cross sectional area as possible. If I have you hold up your hands and if you take you opposite hand with one finger and you press into the palm of your hand as hard as you can, very quickly it starts to become uncomfortable as opposed to if you were be able to register how much pressure it took to become uncomfortable, back off, open up the hand and then go palm to palm with the same amount of pressure, you will barely be aware of it. Schuster used to call this expansion of forces snowshoeing the expansion or the post. It is basically strapping a tennis area to your shoe. The point is you have dispersed the pressure under your food 3-5 fold, which, if everything works out well, you will only sink a few inches into the snow as opposed to without the snow shoe, if its powder, all the way down to your waste or deeper. When you disperse, if you look at the lower R hand side of the slide, when you have an area that you want to disperse by the lab we get this all of the time. The doc will send in the prescription and say they would like to offload 2 or 3 or 1 and 5. It is certainly not that the technicians are incapable. They are certainly really good at looking at models of the feet and surprisingly better than the docs sending the prescription in and pointing things out about the anatomy of the foot based on that positive model. BUT to make their life easier and ultimately the success of your orthotic better, a nice trick is, if you are working in plaster take a cast marking pencil and any of the labs you work with will give them to you. When you dip this into water you can outline the area to be dispersed on the plantar aspect of the foot when you apply the plaster it transfers over as a negative. If you are working with the STS stocking material, the fiberglass socks, as you know you need to put a plastic bag over the foot before the fiber glass goes on. Also, do not ever activate the cast with warm to hot water. It is a very exothermic reaction. When you put the plastic on the foot you cannot use this technique to demarcate an area to disperse. So what you do is take a piece of inch felt and cut it into the shape of the lesion you want to disperse, peel and stick it directly to the foot. When you apply the fiber glass sock, as it is setting take your hand and for a moment of 2 take your hand away from stabilizing the TN joint and from loading the foot plantarly and just kind of massage the fiberglass while it is curing around that inch dispersion and you will create a little dimple in that area and if you want you can even enhance it on the inside with a regular sharpie or felttipped marker. But now when they pour the positive they will know where it needs to go. With dispersion padding as well as with the crest pads and met pads, keep in mind that in particularly feet that have hyper mobility what is the definition of hyper mobility? It is mobility when it aught to be stable. The term defines what often is the reason why; again we sometimes get calls from mad customers asking if the technicians were drinking the night before. Again, pull the positive, take the orthotic, line it right off and balance the pad to disperse the area that is marked. BUT a hyper mobile foot implies an unstable foot, a foot which tends to change appearance from off to on weight and in particular the length of the foot and more in particular the relative length of the forefoot relative to the stable heel there is only one heel bone. So it cant really elongate itself, but distal to it you have lots of joints that can unlock and open. If this is the off weight foot that I have taken the cast of and marked and dispersed, the pt hits the ground, here is where I edged
off my dispersion and sometimes the pts will say (just like with met pads) it feels as if it aught to be (and you can insert 9/10) more distal. In Europe they do a lot of semi-weight bearing casting. So I usually get asked the question, why dont we use semi-weight bearing casting for this because you would anticipate the full or partially weight bearing part of the foot or anatomy or location in this semi weight bearing position. The answer is YES but what is the purpose of an orthotic? Remember the definition. Orthos from the Greek means to change or to alter. You are looking to change the functionality of that foot. The way you are going to do that is by repositioning certain key bones of the foot in particular the calcaneus and the met heads in an effort to effect STJ mobility and MTJ alignment. The problem is you have to do that through the interface of the plantar fat pad. Yes, semi weight casting will capsure a more anatomically accurate position of those abnormally located met heads but what you will sacrifice is critical contouring and an ability to realign the STJ and MTJs. So one balances off the other and if you again. This is the art of medicine. There is a certain amount of science to this but they still refer tot his as the art of medicine. You will get a sense of which pts have these extreme ranges of motion and with that being the case there is nothing that says you cannot stage the therapusis. The pts love this. It sounds great. You are staging the therapusis. What do I mean by this? What it means is that I am going to create a basic design on the orthotic. You will then wear it from 2-3 weeks at which time you are going to come back. Based on that wear pattern I will then send it to the lab for completion where it will come back with the cover and everything. So there are 2 ways which you can approach this and both of which will work.
Heel spur pads it is interesting. When pts have pain in the heel, all heel pain becomes heel spurs. my friend Shlomey had a heel spur. If you have a bunion, I have a bunion. All things are not created equal. All heel pain does not necessarily mean heel spur. One of the most difficult things that you will have to be able to explain to your pts is that many times some of the most acute heel pain when you see in your office, when you shoot that lateral projection you cannot find the spur. As we know, the presence of a spur simply means that this process has been going on, in some cases a heck of a lot longer 3
than the pt has even been aware. What is a spur? A spur is very simply one attempt by the body to resolve this problem. What is the problem? The problem is that the arch is changing too much from the off to the on weight bearing position. We are only born with a plantar fascial band of x amount of mms or cms in length. Once you stop growing and once the foot stops elongating that is it. I can not get any bigger. The problem is, from my off to my on weight bearing position and you do not have to go from a CMT type foot to a flat as the table foot it is just that IF the off to on weight bearing arch contour is exceeding the ability of the fascia to comfortably elongate, it wills tart to tear away from both its insertion as well as its origin. If you look at the insertion and origin of the fascia, which is more defined? The origin. It comes off the tubercles of the calcaneus. Where as distally it fans out and encompasses the MPTJs. So the point is that even if a spur is present, which tubercle generally produces the spur? Medial or lateral? Medial. Why? Due to the rotation of the calcaneus. It calls all the way back to FUI. That horrible course. And then FUII is not much better. Origins, insertions, axes of motion, varus, valgus, up, down, L, R it is awful to go through but now, put it together. By the way, when you have pts that have lateral tubercle calcaneal pain, push off on the fasciitis for a moment but classically it is medial tubercle. Why? When the STJ pronates where does the calcaneus move? Everts. It all comes back to the basics. So everything on the medial side of that foot, including the fascial band is going to get tighter. It is going to pull primarily away from its medial tubercle. You divide heel pain into tractional and impact. Under tractional is facial type pain. So in this instance though, when we look at pts even that have a plantar enphysiophyte (spur) the location of this opening is WRONG. What good does the U-pad do? That is where the spur is residing, why are you opening the center. Some swear that these help. Schuster had a theory that said the presence of a heel spur pad just acts like a very odd looking heel lift and by elevating the heel it relieves the equinus which is causing he foot to break in the 1st place. If you do go with a heel spur pad, you aught to combine it with a deeper heel seat. The other name for a heal seat is a heel cup. The reason being is that you want to encompass the calcaneus. The more stuff, as you will see in a second that you put into the heel cup the more obliterated or superficial the heel cup becomes until finally the pts are standing ON the devise rather than IN it and they start to then complain of pain around the medial and lateral rim of the devise.
There is a modification of that that became very popular and is probably more popular now than it was. It is a heel cushion, which is just a solid piece of material. Generally we use poron or some of the docs with pts with fibromyalgia you can use pink plastazote and they seem to respond better to that. It is a solid, solid application of poron into the heal seat area. If the pts have a tendency toward excessive inferior heel shock, if its a higher arched foot for example with a restriction of STJ pronation this modification seems to work very well. Again, you should compensate for that by deepening the heel seat BUT the deeper the seat the wider the orthotic is going to become. Docs want a devise that fits loafers and on and on and on and they want it all. BUT you cant do that. There are certain restrictions to these design restraints.
Heel raises when you put a lift on an orthotic they are very potent modifications that are useful for not only the most obvious, which if Im short on one size I can try to equalize that leg length but they are also very effective if you want to alter the phasic activity of gait meaning if I want to get them out of the contact phase quicker. If I have a pt who has STJ arthritis and it is painful when you move it and for whatever reason either they are not ready for surgery or they are not surgical candidates, one possible way that I can effect them in a very positive, meaningful manor is, if I reduce the amount of time that
the STJ participates with the ground there will be less STJ movement and therefore less pain in that joint. So, just take it to its very ridiculous extreme, does the STJ work longer or shorter as I elevate the heel? Take it to the ridiculous extreme I am right now almost in full extension or PF at the ankle SO the higher you bring the heel off of the ground the less time the calcaneus spends in contact with the supporting surface which means the STJ will NOT have to move the calcaneus against the talus. And if there are arthritities within it or if there is a suspected coalition you can use this. This is one modification that often comes into the package for designing an orthotic for kids that have suspected coalitions. Bring their heels up a little bit. It reduces the amount of time that the STJ has to interact with the ground. One thing you should be aware of and it is harder for me to show you but visualize for a second, if I have 1 limb that is substantially shorter than the other or it doesnt necessarily have to be get rid of that substantially. If one limb is shorter than the other, one way to compensate for a short leg is what? If I am shorter on this side and I need to get this foot down to the ground, if I PF the ankle I will bring the forepart of that foot to the ground. If I simply fill in that gap under with a HEEL LIFT, Yeah I have contact of that foot back down on the ground BUT the problem is that I have that foot maintained in a PFed position. And then you have to ask yourself, is it really normal to walk around with a foot PFed, even though the bottom of the foot is contacting the ground by virtue of this heel lift, is this a normal way to walk? The answer is NO. So sometimes, in the past we were taught if the LLD was > of an inch that the lift needs to be extended from the heel out to the met heads. You dont want to go distal because they you are interfering with MTPJ rotation. But if you bring that heel lift out to the met heads now you have maintained the foot in a more parallel arrangement in relation to the floor rather than maintaining them in equinus. Do you see the diff? There are people in Michigan at the college of osteopathy where they have linked a lot of our understanding of the foot to low back dysfunction. Pts with as little as 2 and 3 mm LLD, they are suggesting to modify that or neutralize that limb length.
Obvi, if you have a contracted heel cord. Remember, if I have a pt who presents with an arch that is obliterated through the MTJ, until proven otherwise, if they ask you on your 6
externships what is the most likely etiology for that mechanism or for the appearance of that foot, think EQUINUS until proven otherwise. Equinus is the most commonly occurring deformity that is going to directly attack the MTJ. So heel raises, if we are going to try to produce an orthotic devise that in theory the pt is going to be able to tolerate depends on, again, if you use a somewhat controllable material, it doesnt necessarily have to be acrylic, BUT if the reason for the collapse of the MTJ isnt neutralized remember all this devise is doing is contouring the corrected position of the foot. If I take my eye glass frames and pop the lenses and put the glasses back on the frames, I wouldnt be able to see beyond the 2nd or 3rd row. I need the lenss to correct my vision. If it is a sagittal plane problem, this devise MUST have some heel platform, the amount of which will depend on the severity of the equnius in order to neutralize enough of that so when the pt stands on this doesnt have a scenario whereby they have a MTJ that is broken. The irresistible force is the immobile object. It should start to click. It stars in the 80s. Lots of the stuff that you see: orthotic combos of materials of things are discovered by accident. Usually what ends up happening, the use of poron as a heel lift, was just one of those instances where the doc had specked out a heel lift and someone mis-read what was said, PPT was interpreted and added and they found out it doesnt work as bad as you think. You would think it would be a little on the compressible side. Well, there are times where that may be desirable. You would want the ability to add a little bit more of dampening of shock or dissipation of shock at strike. SO you can be creative. You are only as limited as your mind when you design orthotic devises. The worst thing you do when you get into practice is doing 03Rs. Everyone gets a spot devise with a 0 forefoot post and a 3 varus rear foot to the met heads. BOOM. And it doesnt matter. L foot, R foot doesnt matter. Diagnosis doesnt matter. Age, sex, shoe doesnt matter 03R. There are lots of other people out there who are buying for the attention of the podiatrically/biomechanically challenged public.
We will finish with a couple of things on covers. By way of definition, extensions and top covers sound alike but they are still different. There are consequences if you ask for the wrong thing. The diff is that a cover covers the entire shell. The length of which you can vary. But it begins back here at the heel cup and extends distally. So with a cover you cover the entire devise. You can end it at the met heads. You can bring it out at the sulcus or you can go full length. Thickness is standard 1/16th to 1/8th but I have pts who comes up even thicker. The more stuff you add to the dorsal aspect of the appliance, the more likely you are obliterate its contours and render the devise not as effective as it could be.
Shoe gear. Lets look at a loafer. Unfortunately it has a removable foot bed. BUT think for a minute, if the pt wants to wear a loafer, just a standard loafer, if you send me Now look at the toe box. Some shoe anatomy: The counter of the shoe is what holds the heel. The area right under here, this is called the tongue of the shoe. It is easily to see it when you have a toe shoe. It is right under the laces that flaps around. It is to protect the dorsum of the foot from being bound up by the laces. If you have a pt that complains that the tongue of the shoe is always shifting off to the side, think for a second what is going on in that pts foot is there is a significant amount of MTJ movement going on and what is happening is the foot is going this inside the shoe and literally shifting the tongue off to the side. The pt barely is in the chair and you have 8
3 things in the back of your head. That is impressive when you are on externships. This equinus or a complensated forefoot varus. One of those 2. Everytime. Pt has just taken their shoes off and you have 3 things ready to throw in an attendings face. It would impress me. But the point is, with extensions the toe box, which is up here covers the forepart of the foot. You look at the shape. In order for a shoe to be a loafer it needs to be shallow and narrow in an area where unfortunately where you design orthotic devises it needs to be a little bit wider and deeper. The toe box, many times in these shoes I cant for the most part extend this devise much past the mets heads. Which means if I have a problem where I was going to try to add a crest pad for whatever reason it is NOT happening UNLESS they alter their shoes. Certain requests for orthotic modifications, it is not going to fly. I hate having to say this over again, play Doctor. I tell you this because there are situations where if you dont stand up and say look it has to be this way and even this way may not give us what we are looking for when you start to compromise, your orthotic design, because of their wants will haunt you later on. You have to be willing to say Im sorry. At some point you have to be able to say Sorry, you are not following what we are telling you and we have to move you on.
You can laminate materials. Most commonly you will see us downstairs laminate plastizote over poron. It never goes the other way. If it comes back from the lab where the poron is on top of the plastazote they were deff on a bender last weekend. The poron is used BENEATH the plastazote. Some doctors love plastazote sandwiches for wound pts. It is designed for implosion of that material. They are designed to keep compressing and compressing and compressing. If you take even a thin layer of poron and put it under the plastizote, the plastizoe implodes as you want it to but as a much slower rate which translates to a devise which you can extend out as long as its life span. You see even in pts that do not walk that much how quickly the plastazote (especially pink) compresses. This is a good thing but you dont have longevity.
Certain things, it is much better if the location of the modification is done dynamically. This is one. I can only tell you that if you order a toe crest pad directly at the time you send the cast to the lab you are going to be disappointed. You can use these crest pads both mechanically (in medicine we see the contracted claw and mallet toe deformities) where you put a crest pad in there and you can lift that part of the anatomy off of the foot bed. You can also use these pads very effectively neurologically. There were some neurophysiologist in the 50s that started some work and continues through the 70s, Dunkin and Manfreidy using these types of crest pads (they did not call them crest pads but this is what they are) to inhibit excessive clawing of the lesser toes in spastic pts and how it reduces the tone of some of the proximal musculature as evidence by EMG analysis, specifically in spastic pts where the over activity of the gastroc muscles, the adducturs and the hip flexors can be dramatically reduced by just sticking a stupid little crest pad under the lesser digits. We will show you in ortho how in the right pt this can be achieved. In pts with movement disorders you can spec a device out with this modification and you will be amazed as to how well this positively effects gait. You need to put these modifications in ACCURATLY. If you follow my pointer (37:07) this is how often they orientate if you ask them to do this at the lab. Dont ask me why. I have tried to explain this over and over and over and they end up sticking them on so they are perpendicular to the long axis of the foot. We have one downstairs to show you. This is very typical of all of the labs and we cant figure it out. SO spec it out without a top cover and locate it later.
10
Just to make a comment: an extension begins at the distal end of the shell so there will be nothing over the shell other than the vinyl or leather covering system, the padding when you ask for an extension only begins here. So are there cases where you would ask for an extension vs. a top cover? Sure. Where maximum contouring of the shell may be critical, bulk. Many times we will put a very thin extension of 1/16th PPT beginning at the shell and ending at the sulcus with the intent of, on a low profile design if I want to install either a dispersion system, a met pad or something of that nature OR if I want to just provide minimum shock absorption to the met heads. So I want to keep the profile down. So just so you understand the difference, a cover starts at the heel seat and moves distally to the length you spec. An extension begins at the edge of the shell.
This is the same devise and what I did was I covered the top 1st with 1/16th PPT and I am trying to get you to look at the diff between the heel seat. You see here there is more of a heel cup in this. Up here you see how it becomes obliterated? It is just simple logic. I have a standard heel seat from the labs and it is 3/8ths of an inch deep. Deep heel seat is specked out at 5/8ths of an inch. If I have 3/8th and I apply 1/8th, it is not that you subtract the 1/8th from the 3/8th and you are left with 2/8ths or because remember it is a circumference so it is an additive effect. It closes the heel cup down very quickly. So if you put a lot of stuff in the heel and again, I just think of this 1 customer every orthotic he orders he specks it out with 3/8th of an inch of stuff and when the devises go out you barely see a heel cup. He has so much stuff built in. We quietly many years ago 11
increased his heel cup to 3/4s of an inch to off set that because he kept sending these things back because the pt was complaining that they were standing on the edge of the devise. They were literally being lifted right up out of the devise. So you have to be careful about the amount of stuff that you add.
We have a material called Spenco. It is a green material manufactured by a company in Texas started by a guy names Spence. Spenco is neoprene with a nylon cover over it. A wetsuit allows a certain amount of water into the suit which is heated by your bodys core temp and you have that insulating thin layer of water which works fairly well. It keeps you fairly warm. The prob with Spenco is if you use it as a final expression as the top cover, the layer closest to the foot, and if they happen to be feet that are hyperhydrotic, OH BOY within a week, these things stink. It will knock your head off. You want to be very cautious when you use Spenco as a top covering system. You need to make certain that the pt is not hyperhydrotic. Also, you should not use this as a top cover if its a construction worker or someone whose occupation may permit them to get wet. Also, when it rains, runners dont care. They are out running. Even if its a dry climate, your feet sweat when you are inside the shoe. So the use of Spenco I do use Spenco many times in conjunction as a sandwich combining it with heat, plastazote and poron as a tri-laminar sandwich. It works nice in the elderly foot. But as I said, I know there is a tendency to jump on Spenco because it does feel very cushiony and it is, but it is awful because it is an open cell system and it absorbed perspiration. It is also not very durable. The nylon tends to delaminate very quickly.
12
Orthotic prescription Writing, Problem Solving: Putting it all together What we are going to try and do is explain this process. When you try to design an appliance for a pt there is an overwhelming feeling. You have the pt, you have arrived at a diagnoses, Randy hands you a prescription and he says fill this out and even on the 1st choice line which is a reduced portion of the full Langer where the heck do I start?
No, this is not going to be on the test but this is for your own edification. I put 2 slides in order for you to understand. This is where its at. The nature of medicine is changing.
This was an excerpt from an article in last months current podiatrists management magazine. We have kind of just let go of biomechanics. There are some very imp thoughts here. This was from a seminar that was held here March of this eyar. It was a 3-day, dawn to dusk residency hash it out. Many of the directors from programs got
13
together and discussed ways that they could improve the programs form the teaching aspect and what concerns do you have as attendings. There were reps from the various schools of podiatric medicine. One of the things that was voiced was that in many cases, but I will tell you, which wasnt in the article, thanks to the fact that you are suffering through this and apparently retaining it, because one of the things that did come out which they did not mention in the article is that the people coming out of NYCPM for the most part have absolutely blown away the competition from many of the other schools in their ability to articulate at least some of the basic foot mechanics and an understanding of how a foot works. But as a whole, most of the residency directors said that the skill set of most of these students BM skills set has deff eased down the line in a negative direction. It is trending downward. At that seminar there were only two 20-minute lectures on BM. A need was expressed for additional training in BM of the LE. But as I said, what wasnt expressed in that article was the fact that many of the directors was expressing an interest in the fact and a curiosity as to why the people coming out of here seem to be ahead of their colleagues.
When we have these lectures at continuing education seminars look at what is offered at most of these major programs. It is generally sx and wound care, sx and wound care, sx and wound care. However, when they are offered, you cannot get in. Usually when it is a separate workshop, BAM they are closed. If you limit the number to 30 because its hands on, it closes within days. One thing, if that doesnt get you excited then take a look. He reads second bullet. Thats a big chunk of change folks. If you think you are going to get wealthy just doing sx, think twice. In order to be successful in doing this, you have to have your understanding.
14
I just want you to understand something here. Who else is doing this stuff? He reads down the list. The point I am trying to make here is WHY YOU? You have all of this competition. Why should they come to you? Why you is because once you set yourself up in your area you will be able to very quickly demonstrate both to your own pt population and if you go into a group you will introduce yourself to all of the diff types of docs in your area and what it is you can provide those pts. Very quickly you will see that your end of the practice will grow. Some talk about revenue in working in a group..
What are you trying to accomplish? So how do you successfully write a prescription that leads to a successful outcome. Well, what are your goals? Remember, I told you at the very beginning of this program 2 types of appliances: those that alter the function of the foot and those that just wave the white flag and just accommodate the deformity where you are not looking to change anything. Are you looking to alter, whether you are trying to enhance or restrict movement? Remember, of the 2 it is easier to restrict excessive mobility than to enhance motion that isnt there. It is very difficult to artificially provide what the STJ does anatomically. This is a real tough nut to crack.
15
Are you looking to work posturally, specifically the pt that the local orthopedist that took a liking to you sent you a pt with patello-femoral syndrome medially? Because of the fact that the orthopod recognized that the pt has a pronating type of a foot and perhaps that is the etiology. He did his job and evaluated the pt and found no intrinsic damage of the knee. Remember, you are in practice and a 1st time pt walks in with knee pain and you look at that foot and you see that the foot is pronating, technically you cant directly treat that knee pain. That is out of your scope. In my practice, what I often will do is say look, Mr. and Mrs. Pt I suspect that the etiology is down here but lets be sure, I want you to see a colleague of mine and depending on where they live I send them to a referral source. You have to be certain that it is not something else. I am the podiatrist. If their sole complaint is knee pain and they have no foot pain whatsoever, keep in mind, there is no foot complaints you are on thin ice if you jump in and you do something podiatrically, biomechanically and it also happens to turn out that the pt also had a partially torn ACL manifesting as medial knee pain. Because the pt didnt seek orthopedic care for 3 months because they were wearing your CFOs and it wasnt getting any better now the grade I ACL tear is a grade III, you better believe there will be a letter in the mail or a knock at the door.
The idea is to take a look at all of these factors that are contributing to the abnormal function of the foot and within the context of what we are capable of effecting, try to negate or neutralize. We try to neutralize the effect of these abnormalities. What we use for that, as you will see later, is we will take all sorts of different treatment modalities; certainly orthotics will be in the mix.
16
The brand new current podiatric management magazine has this article in it. Blake wrote it and there is a cast technique called the Blake inverted technique. He and Kirby were classmates. Rich has an article called the top 15 orthotics/shoe modifications that are useful in your office. This is a really nifty magazine to read. Rich had an interesting article once. This is interesting because over the last couple of years the basis of your training has been based on the things put forth by Root. Root and Reed and ORyan combination normal and abnormal function of the foot. One of the things that I spoke about at the conference was the fact that you should understand over the past several years, Root and his tenets of foot function and approach to treating the foot have been scrutinized and in some cases morphed. You can see that the way that Root visualized how the foot worked was maybe not necessarily occurring in every case. HOWEVER, one of the things that no one denies is the fact that Roots basis of understanding how this foot works is without fail the best entry level approach to understanding foot function. The one thing with Root is that most of the stuff is based on an understanding of the STJ movement on the frontal plane: STJ pronation and STJ supination. As I spoke to the people at the conference, along comes Dannonburg, who really is the one who is credited with articulating the concept of this hypermobile first with a resultant momentary or functional locking of the 1st MTPJ functional hallux limitus. Grossly speaking, as much as Root got us to look at the foot from the frontal perspective, specifically the posterior frontal perspective in calcaneal movement, Dannonburg got us to turn the foot around and look at it from the side and get a better appreciation of the sagittal plane mechanics. The one thing you should understand is that you are going to be assailed with all kinds of theories moving forward after finishing FUII and NYCPM and your residency and you are in [practice. That is ok because some of the stuff that you will be hit with, as far as a new way of controlling the foot, some of it might have merit and some of it might be complete Whooey. But as Rich was saying you have to test out the waters a little bit and see what works. There may be elements of a particular theory that work well and there may be some of those elements where you want to run like hell and stay away from. But dont think for a minute that everything I am telling you is Gospel. Here is a classic case: the strappings. Doc has a really cool way on that LowDye where those 1st 2 straps you encompass the heel and you get it to PF under the 1st. To this day, I still cannot do it. I cannot get those straps to cross plantarly. In theory it would work really well if I could do it because it helps to drop the 1st and the 5th ray. So it is not that when I stay medial or doc goes plantar, one is wrong. It is just if you can get it, if it
17
works in your hands, go with it. But the underlying theory is the same.
So when you take a look at these feet and these are 4 case scenarios that we will examine, the whole purpose of approaching therapy programs or protocol or designing an appropriate therapusis is to get at the basis for it and in order to that that we have to perform an examination.
I cant tell you how many times pts come to me with sometimes 1 pair and sometimes a bag full and as I am performing the exam, doing the most rudimentary measurements as I am drawing a couple of the lines to set it up I often play a game with the pts. It keeps me entertained. I tell them, as I am drawing the lines, I have them prone so I can draw my calcaneal bisections and so on and I will apologize to the pt: I am really sorry, I am SURE this has all been done already but when you take measurements we all measure a little differently and I need to get my own measurements
18
This is what you hear. If anyone ever bothered to take even a rudimentary ROM what so ever then the pts get all riled up. They say he came in and he did this to my foot and he said you have a heel spur, you need orthotics, he walked out and the net thing you know the secretary that was collecting my co-pay comes in and starts molding my feet. Then when they get the orthotics, of course, they didnt work. What you find is as you get better at this, your office will become the dumping ground. They come to you with a bag. They have spend hundreds and sometimes thousands already and nothing is working. I told you about a pt that came to me with equinus with a bag full of orthotics and not one of them had a 1/16th heel lift on it. What does that tell you? No one bothered to look at the foot to recognize that something as grossly apparent as an ankle equinus was present and therefore should have been neutralized in those orthotic devises. So if you are going to take on that responsibility, provide the service. This is a secret to be successful. YOU, the doctor provides the service, NOT your chair aid. You get in the pts face and you put your hands on and do the work and you will be more compensated. Bringing Doc back, he talked a little bit about this dominant plane theory that has been put forth many times. It becomes so simple sometimes it is madness. If you just keep an open mind you will see how very simple it is sometimes to arrive at a proper prescription. You only have 3 choices. There are only 3 body planes and the influence that is destroying the foot resulting in the abnormal strain not
19
we will use PTTD, has to come from 1 of 3 body planes, or like a Chinese menu: a little from column a, b and c. It could be all 3. But also, there could be a dominant plane, which is imp because if the dominant plane is sagittal then the dominant approach to offset that had better be on the sagittal plane. If you do it this way you will be very successful.
This is very simple. If I look at this foot. This is out of Scarlados (spelling?) book which is in the lib. He was out at the Cali College during the days of Root. It is called the California compendium of podiatric biomechanics. It is long out of print. It is an awful book because it was never indexed. It was a series of articles and this is an illustration from one of them. It is very interesting and very apparent. Remember, if you see a calcaneus that is everted, not only relative to the leg bisection by relative to the floor, most likely that is a result of a compensation for a forefoot varus. SO if I need to offset a varus deformity I need to apply something that will neutralize.
You want to inhibit, if you will or certainly reduce the need for the foot to have to
20
collapse so much. So when we look on the frontal plane we have issues in the forefoot, in the rearfoot in a varus or valgus direction. In this instance, on the lower left, I have the foot in a neutral position. Here is the 1st because of the sesamoids. I placed the foot in a neutral position and we trying to illustrate a calcaneal varus issue a deformity. Upper Right again, STJ has been manipulated and stabilized and you can see that relative to the heel bisection I have dotted it, put an arrow, tried to make it as apparent as I could notice the inverted attitude of the forefoot a forefoot varus. Lower right this is the one that sometimes get confusing. When we were students we would sometimes call this a California valgus. Remember, a true forefoot valgus, is it clinically possible its like when I ask you the Q, is the STJ possibly able to compensate for an equinus. If they say COULD it be used? You say yes, but it is not a good joint as we have discussed many times. Could you have a true forefoot valgus? The answer is sure, but a true forefoot valgus where the entire forefoot is everted is not all the common. You often see it in conjunction with a spasticity of the peroneus brevis muscle. You see it many times in equinovalgus feet, UMN. More commonly what you see is a rigidly PFed 1st ray that normal foot type doc eluted to. When in your eye, when you bisect the 1st and the 5th ray you see, relative to that heel bisection you see the foot gives you an appearance of a forefoot valgus. When we were students we used to call this California valgus. So a rigidly PFed 1st. You have other frontal plane issues that you have to keep in mind as well when you have genu varum or genu valgum. Both of these can be pronating influences on the foot if the STJ ROM is available. Particularly genu valgum because, as I have shown some of you, with genu valgum grossly speaking it places the foot everted to the entire floor. Genu valgum is a wicked extrinsic pronating influence on the foot, particularly extrinsic.
Here you go: I have an obese 54 year old peri-menopausal F with unilateral medial ankle pain which you suspect is a partial tear of the post tib tendon. She has sever genu valgum and a unilaterally, asymmetrically, much greater pronated foot. The MM area is warm to 21
touch. There is pain along the course of the post tib tendon. Well, we get our MRI and YES it is confirmed. It is a stage 2 tear. We CAM boot her for a while, whatever. We calm it down. BUT we cant CAM boot for the rest of our lives. We have to get it back into a shoe. For a moment, think. She says, here is the shoes that I like to wear this in and again, she produces a very non-descript but orthotic un-friendly slip on loafer. It has to be able to fit these. These are the shoes she wears. The answer to that is, NO those are the shoes you used to wear. Why? Because I cannot tell you how many doc call in in tears because they went ahead and they made a devise to fit that shoe, which is generally what they did was they took a piece of 3/5 carbon fiber with an intrinsic post. Remember the intrinsic post is just a shell and we angle the correction to the thickness of the shell but 3 mm, how much correction on the frontal plane can you get? The answer is just about 0. The other thing I told you about an intrinsic vs. an extrinsically posted orthotic as far as stability is that it is LESS stable on the frontal plane if its intrinsically posted. Why? Because extrinsic posting spreads out the frontal plane width of the devise. SO lets say she is 54, 240 lbs with severe genu valgum. Are you getting the picture? She puts the orthotic in the shoe and WOW it fit the shoe. Great. She puts her foot in, she steps up on it, stands up and what? SAME THING. The foot goes right over the shoe. Should you have been surprised? NOPE. And nor should you be surprised when she starts screaming at you because she just dropped 6 bills on your because it is not a covered idem in her insurance plan. So BETTER to recognize that here are these extrinsic factors that you MUST take into account in your orthosis design.
this is a fully compensated foot in the R side. Notice the diff between the 2. The right foot is in the RCSP (relaxed calcaneal stance position). Notice, relative to the floor the heel has now been brought perpendicular. The foot has no reason to go any reason, which tells us there is almost likely NO forefoot imbalance causing that STJ to have to pronate any further than that. L foot is also in its neutral position.
22
What I did is I had this foot relax as well to neutralize the effect of, in this case that lower tibial varum. You have to look at the ROM of the various joints of the foot. Doc showed you the week he did the calcaneovarus and then he had fully, partially and uncompensated. If you have a lot of frontal plane issues: calcaneal varus, tibial varum and so on. And the STJ anatomically doesnt move all that well in a pronating direction what you may end up with is when the foot is maximally pronating it still may look like this. So the symptoms may be much different. So this is why we have to get into looking at what is going on with the foot.
By large, what we would like to do, as DAmico said is you like to try and neutralize some of the effects of those frontal plane imbalances. In this case, since this forefoot had no imbalance, most of the pathology resided in the rear foot I will apply a buildup to the rear part of the orthoses, specifically a rear foot varus post. How much will be determined by the deformity we will measure. When doc kept saying that the measurements arent all that critical, this is probably one area where I disagree a little bit because I like to take measurements. One thing you will find though is that measurements are an art. Measurements take years to fine tune. 23
However, when you get good at measuring these deformities and at this stage I think the key would be to discern if there is an asymmetry in the total amount of a varus deformity of one extremity vs. another and perhaps offset that a little bit asymmetrically in the correction. BUT it is a good idea to fine tune a prescription if you can take the measurements because you are now telling the lab, much like the diopter on these lenses where my R eye is much weaker than my L, to balance out the vision or to balance out the function of those feet. Basically what we are going is we are going to offset. We are holding this foot closer to that neutral position.
There is what I often refer to as a paradox of the foot. Very simply speaking here is a foot in its neutral position and you can see and I have hopefully made it easier for you to visualize, look at the angle that the fore part of the foot makes when you place the hind foot back into a stable or neutral position. This is the paradox, meaning the consequence (think of it that way) of as a fetal creature we are occupying a studio apartment that has all rounded walls. You are living in a pear for 9 months. What it tends to do is it tends to bow all of the extremities of the upper and certainly the lower extremity. The problem is now, when you are born, if those frontal plane twists and torques have not fully derotated you essentially have a problem relating all of those twists and turns and torques to a flat surface. At all costs, the body will attempt to bring as much as itself to the supporting surface as possible. So in this instance, if there is a significant frontal plane imbalance, well you can walk around with your foot in this position. However, if you look carefully, see right here see the bulging? Which muscles is this? Tib ant and EHL are firing like mad to hold the fore part of that foot up, which is one possibility. You are off sometimes. Pts with fasciitis or shin splints syndromes runners will say this a lot they say they find that if they are running on the outside of their feet it doesnt hurt as badly. What they are doing is they are way overcorrecting themselves. They are trying to hold themselves in a corrected position. This is what is going to happen. When I say to this pt, ok, let your feet go and relax. BOOM the muscles stop contracting and BOOM what happens? Gravity kicks in and by virtue of the mechanics of the STJ, where in the calcaneus everts, the talus adducts and PFs, the leg internally rotates and BOOM the medial side of the foot hits the ground. That is the paradox of the foot. 24
So in that instance where there is an obvious forefoot imbalance I have to find a way to support, if you will or neutralize that effect so the foot doesnt have to bring itself all the way to the ground and we are going to use a forefoot post in this case. If it is a varus imbalance I will fill it in thicker on the medial side then the lateral side. Same thing before, if it is a relatively valgus relationship that you have, whether its the California valgus where the 1st is rigidly PFed OR in fact a TRUE forefoot valgus, SAME thing, diff direction. Back 1 slide, moving from here to here, how does the STJ move to get from L to R? Does it supinate or pronate? It pronates. Now take it the opposite way. A rigid PFed 1st how do I bring the lateral side of that foot to the ground? You have to supinate. If the only part of that forefoot is on the ground (think of it that way) is my 1st met head, it is the same thing. Remember, I told you the paradox is that in that instance the only part of that forefoot is the 1st. That body is going to try and put the rest of that foot in the ground, which on this case is the lateral. If I pronate that foot it is going to get worse. So it has to supinate. So to prevent that, we will fill in the lateral side of the forefoot post in this case.
25
You might also like
- Surgery IIExam 1 REVIEWDocument6 pagesSurgery IIExam 1 REVIEWEddie MillsNo ratings yet
- Medial Column Flatfoot SurgeryDocument2 pagesMedial Column Flatfoot SurgeryEddie MillsNo ratings yet
- Calcaneal Varus, Forfootvarus, PF1 Stray, EquinusDocument2 pagesCalcaneal Varus, Forfootvarus, PF1 Stray, EquinusEddie MillsNo ratings yet
- Surgery 1 - 1st ray-MTPJ (1-25-08)Document3 pagesSurgery 1 - 1st ray-MTPJ (1-25-08)Eddie MillsNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Olympic Sports Evolution Over TimeDocument6 pagesOlympic Sports Evolution Over TimeJr FloresNo ratings yet
- Halo Fleet Battles FAQ Errata and Clarifications PDFDocument4 pagesHalo Fleet Battles FAQ Errata and Clarifications PDFSam VeeversNo ratings yet
- Physical Fitness: Group 3 Members: Ali, Mycah Therese Hibuton, Jessa Sanguila, Aminah Canque, Nicole Ombawa, OmayyahDocument13 pagesPhysical Fitness: Group 3 Members: Ali, Mycah Therese Hibuton, Jessa Sanguila, Aminah Canque, Nicole Ombawa, OmayyahjessaNo ratings yet
- Land Cruiser V8 Towbar Wiring Kit InstallDocument31 pagesLand Cruiser V8 Towbar Wiring Kit InstallVladimir TereshchenkoNo ratings yet
- Export SapDocument10 pagesExport SapLuisNo ratings yet
- Dominate Sports BettingDocument38 pagesDominate Sports Bettingmaximaurelian50% (2)
- Pipeline Design and ConstructionDocument47 pagesPipeline Design and ConstructionSaber Abdel Moreid100% (5)
- Nutrition 3Document2 pagesNutrition 3azszahNo ratings yet
- 1616 ToDocument4 pages1616 TohamzajmorshedNo ratings yet
- NP + TV (E12) (Key Lien)Document41 pagesNP + TV (E12) (Key Lien)Linh HoàngNo ratings yet
- Correlated Subqueries: Mona KhalilDocument40 pagesCorrelated Subqueries: Mona Khalilanubhav582No ratings yet
- 01 Viktor Korchnoi - WikipediaDocument8 pages01 Viktor Korchnoi - WikipediaAThaddeusAntonioNo ratings yet
- RFP 28 Day Pilates Challenge 2024Document1 pageRFP 28 Day Pilates Challenge 2024Carol ChanNo ratings yet
- Pinoy TambayanDocument33 pagesPinoy TambayanPinoy TvNo ratings yet
- Understanding Muscle PhysiologyDocument88 pagesUnderstanding Muscle Physiologyandre andreNo ratings yet
- Despiece Ensobradora Pitney Bowes Di380 PDFDocument132 pagesDespiece Ensobradora Pitney Bowes Di380 PDFLuis GuerreroNo ratings yet
- Resident Evil 4 - Wii Edition (USA) (En, De)Document5 pagesResident Evil 4 - Wii Edition (USA) (En, De)Valentino RaynaldiNo ratings yet
- King of Ears Torture DemonDocument1 pageKing of Ears Torture DemonMatt AmorosoNo ratings yet
- Auto Trans Diagnosis - Aw03-72Le Article TextDocument15 pagesAuto Trans Diagnosis - Aw03-72Le Article TextLeonardo SilvaNo ratings yet
- Parts List of Engine Assy of FMX 440 (PC-24) - TP-836Document1 pageParts List of Engine Assy of FMX 440 (PC-24) - TP-836Cws0% (1)
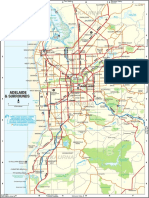
- Map Adelaide SuburbsDocument1 pageMap Adelaide SuburbsJitender YadavNo ratings yet
- DC09 072A. 289-358 KW (329-405 kVA) : Fuel OptimizedDocument2 pagesDC09 072A. 289-358 KW (329-405 kVA) : Fuel OptimizedJulio SullaymeNo ratings yet
- IOCL World Cup Contest Winner Match 34 35 36 37Document59 pagesIOCL World Cup Contest Winner Match 34 35 36 37JaminiNo ratings yet
- P.E. 7 - Q1 - Module1bDocument17 pagesP.E. 7 - Q1 - Module1breymilyn zuluetaNo ratings yet
- Cyl LinerDocument3 pagesCyl LinerAkang OntohodNo ratings yet
- Pro StarDocument263 pagesPro StarLuis EduardoNo ratings yet
- The Lost Battalion EssayDocument2 pagesThe Lost Battalion Essayapi-336625608100% (1)
- Air StarterDocument6 pagesAir StarterParvizNo ratings yet
- SBOKC2023 Bulletin 3.0Document22 pagesSBOKC2023 Bulletin 3.0Andi YusufNo ratings yet
- Tenses Class 11Document4 pagesTenses Class 11harshitaNo ratings yet