Professional Documents
Culture Documents
OBGYN History Form
Uploaded by
Sandeep GhosthOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
OBGYN History Form
Uploaded by
Sandeep GhosthCopyright:
Available Formats
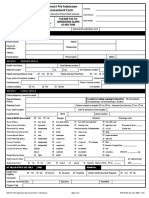
OB/GYN HISTORY
Name______________________________ Date of Birth __________ Date __________
Reason for Visit / Chief Complaint _______________________________________________
______________________________________________________________________________
Primary Care Physician ________________________________________________________
Menstrual History
Age when started first menstrual cycle _______ Fist day of last menstrual period __________
Number of days from the first day of one cycle to the first day of next cycle __________
Duration (how many days of flow?) _______ Amount (light, moderate, heavy) ______________
Cramping (mild, moderate, severe?) __________ Helped with medication __________________
What type of contraceptive (birth control device) do you use? ____________________________
When was your last Pap smear? __________ Where? __________ Was it normal? __________
When was your last Mammogram? __________ Where? __________
When was your last Dexa (bone density scan)? __________ Where? __________
Menopausal History
Age of onset of menopause _______
Are you experiencing menopausal symptoms? _______
Are you currently on hormone replacement therapy? _______
Obstetrical History
_______ Number of living children
_______ Number of premature deliveries
_______ Number of full term births
_______ Number of miscarriages/abortions
_______ Number of vaginal deliveries
_______ Number of Cesarean section
Surgical History
List all surgeries you have every had (include C-sections, tonsillectomy, gallbladder, oral, etc.)
Date of surgery:
Type of surgery:
_______________
______________________________________________________
_______________
______________________________________________________
_______________
______________________________________________________
_______________
______________________________________________________
Have you ever had a colonoscopy? _______ If yes, When? _______ Where? ________________
Family History
Father (circle one) Living Deceased
List any known illnesses, medical conditions, cause of death. ______________________
______________________________________________________________________________
Mother (circle one) Living Deceased
List any known illnesses, medical conditions, cause of death. ______________________
______________________________________________________________________________
Please complete reverse side of form. OVER
Family History Contd
Do you have any sibling with any medical problems. If so, please list. (Circle which sibling)
Brother
Sister (Living / Deceased) ___________________________________________
Brother
Sister (Living / Deceased) ___________________________________________
Brother
Sister (Living / Deceased) ___________________________________________
Is there any family history of cancer? _______. Please list which relative and type of caner.
(Please specify if maternal or paternal relative.)
Relative
Type of Cancer
_______________ (Living/Deceased)
__________________________________________
_______________ (Living/Deceased)
__________________________________________
_______________ (Living/Deceased)
__________________________________________
Social History
Marital Status _______________
Occupation ____________________________________________________________________
Do you smoke?_______ How many packs per day? __________ How many years? __________
Do you drink alcohol? _______ How much? __________ How often do you drink? __________
How many caffeinated drinks do you have in a day (coffee, tea, soda)? ____________________
Do you exercise? _______ What type? ________________ How many days per week? _______
Spouses name and occupation ____________________________________________________
What is your preferred Pharmacy___________________________ Location________________
Medications
List all medications that you are currently taking (include birth control, creams, aspirin, vitamins,
hormones, and other supplements).
Name of Medication
Strength
How often you take it
______________________
______________________
______________________
______________________
______________________
______________________
______________________
______________________
______________________
______________________
______________________
______________________
______________________
______________________
______________________
______________________
______________________
______________________
Medication Allergies (Include Latex allergies)
Drug
Your Reaction
____________________
___________________________________
____________________
___________________________________
____________________
___________________________________
Medical Conditions
List any medical conditions that you have (diabetes, asthma, hypertension, high cholesterol, etc.)
____________________
____________________
____________________
____________________
____________________
____________________
____________________
____________________
____________________
Any history in you or your sexual partner(s) of syphilis, sores, gonorrhea, herpes, blisters,
trichomonas, warts, pelvic or tubal inflammation (PID), or other sexually transmitted diseases?
If yes, indicate which STDs. ______________________________________________________
______________________________________________________________________________
**Please remember to bring this form in with you to your appointment.**
You might also like
- WARDWORK TemplateDocument9 pagesWARDWORK TemplateColeen NeyraNo ratings yet
- Subsequent Inpatient Visit NoteDocument4 pagesSubsequent Inpatient Visit NoteJanu easwarNo ratings yet
- MRN: - Weight: - KG AgeDocument2 pagesMRN: - Weight: - KG AgeElaina Gonçalves Silva FurlanNo ratings yet
- Assessment - Critical CareDocument1 pageAssessment - Critical CareMartini ListrikNo ratings yet
- Clinical Skills Handbook 2015 MEDN40060 2Document66 pagesClinical Skills Handbook 2015 MEDN40060 2Wilson KhawNo ratings yet
- Krisis HipertensiDocument12 pagesKrisis HipertensiDani NurseNo ratings yet
- Patient Case Presentation StructureDocument30 pagesPatient Case Presentation StructureAmira HelayelNo ratings yet
- Choosing Wisely Bullets To Primary CareDocument10 pagesChoosing Wisely Bullets To Primary CareaayceeNo ratings yet
- 32-Week OB CheckDocument4 pages32-Week OB CheckG. Crusor-PriceNo ratings yet
- One Point Acupressure Treatment AllDocument23 pagesOne Point Acupressure Treatment AllPraveen Kumar100% (1)
- DEMENTIA - Information For Carers, Families and Friends of People With Severe and End Stage Dementia PDFDocument44 pagesDEMENTIA - Information For Carers, Families and Friends of People With Severe and End Stage Dementia PDFSuerte MpNo ratings yet
- Irene's Flow SheetDocument1 pageIrene's Flow SheetmrpatrickrnNo ratings yet
- KWC Antimicrobial Therapy HandbookDocument149 pagesKWC Antimicrobial Therapy HandbookJoyceNo ratings yet
- 99 Topics StudynotesDocument138 pages99 Topics StudynotesM.Dalani100% (1)
- Review of SystemsDocument3 pagesReview of SystemsCarrboro Family Medicine100% (1)
- Lab Values Cheat SheetDocument3 pagesLab Values Cheat Sheetmadison61404No ratings yet
- History Taking FormDocument2 pagesHistory Taking FormMaria Santiago100% (1)
- Herbal PlantsDocument14 pagesHerbal Plantsapi-3739910100% (2)
- Human Behavior & Victimology FactorsDocument25 pagesHuman Behavior & Victimology FactorsAyessa Maycie Manuel OlgueraNo ratings yet
- Guide To Case Presentation-1Document36 pagesGuide To Case Presentation-1Amanda Rodriguez TejedaNo ratings yet
- National Practice SAMP 2018Document57 pagesNational Practice SAMP 2018Kmërgim BinNo ratings yet
- 10 GP ConsultationsDocument4 pages10 GP ConsultationsDev KumarNo ratings yet
- PT: Code:: 07 08 Vs 09 10 Pager # 07 09 10 Pager #Document1 pagePT: Code:: 07 08 Vs 09 10 Pager # 07 09 10 Pager #Yadile D BenoitNo ratings yet
- AK Tripathi - Essentials of Medicine For Dental Students, 2nd EditionDocument310 pagesAK Tripathi - Essentials of Medicine For Dental Students, 2nd EditionCassie Von Peenq79% (14)
- Strategies To Deal With Uncertainty in Medicine 20Document2 pagesStrategies To Deal With Uncertainty in Medicine 20Emilio AssisNo ratings yet
- How To Make An Oral Case Presentation To Healthcare ColleaguesDocument5 pagesHow To Make An Oral Case Presentation To Healthcare ColleaguesYuliana Citra AnggraeniNo ratings yet
- Guidelines initiation switching combined oral contraceptionDocument3 pagesGuidelines initiation switching combined oral contraceptionbrossdavis100% (1)
- Prenatal Assessment GuideDocument17 pagesPrenatal Assessment GuideCyndryl SampotonNo ratings yet
- Task 2 - Ethical Principle ApplicationDocument4 pagesTask 2 - Ethical Principle ApplicationJeslin MattathilNo ratings yet
- Gyno & Obs HXDocument68 pagesGyno & Obs HXJason SteelNo ratings yet
- OBGYN HistoryDocument1 pageOBGYN Historysgod34No ratings yet
- Patient Safety Incident Report Form SummaryDocument9 pagesPatient Safety Incident Report Form SummaryJhun SantiagoNo ratings yet
- MMP Handy Chart October 2011 V2Document69 pagesMMP Handy Chart October 2011 V2Icha IchaNo ratings yet
- Guide To Diabetes MedicationsDocument2 pagesGuide To Diabetes MedicationsJianhua ShiNo ratings yet
- Chapter 22 - Transition To ParenthoodDocument16 pagesChapter 22 - Transition To ParenthoodJill HillNo ratings yet
- Screening Test Sensitivity vs SpecificityDocument7 pagesScreening Test Sensitivity vs SpecificityKinuPatel100% (2)
- Isuog Guideline IugrDocument15 pagesIsuog Guideline IugrericNo ratings yet
- Solomon Sallfors: Ambulatory Morning Report 1: AcneDocument3 pagesSolomon Sallfors: Ambulatory Morning Report 1: AcneSolomon Seth SallforsNo ratings yet
- FibroidsDocument16 pagesFibroidsJiaYee GoNo ratings yet
- Clinical Nursing Judgement PaperDocument6 pagesClinical Nursing Judgement Paperapi-401649778No ratings yet
- Pelvic Exam History and Examination GuideDocument14 pagesPelvic Exam History and Examination GuideMateo GlNo ratings yet
- Abnormal Uterine BleedingDocument8 pagesAbnormal Uterine BleedingEcbNo ratings yet
- C 21Document23 pagesC 21jackNo ratings yet
- Patient Admission Assessment FormDocument1 pagePatient Admission Assessment Formprasanna_326avanthiNo ratings yet
- Essentials 2021Document84 pagesEssentials 2021sanjeev thadaniNo ratings yet
- Bedside Shift Report and Utilizing The EhrDocument9 pagesBedside Shift Report and Utilizing The Ehrapi-349480325No ratings yet
- Vaccine Safety Surveillance Methods and CommunicationDocument16 pagesVaccine Safety Surveillance Methods and Communicationrakesh meherNo ratings yet
- 5 6231116747487838836Document466 pages5 6231116747487838836Indah Siti SopiahNo ratings yet
- ROS: Sick Contacts, Fever, Chills, WT LossDocument1 pageROS: Sick Contacts, Fever, Chills, WT Lossluck2livNo ratings yet
- PDFDocument70 pagesPDFPaul Benjomin AgregadoNo ratings yet
- Oral Contraceptive Reference ChartDocument6 pagesOral Contraceptive Reference Chartpdoan85No ratings yet
- Obstetrics and Gynecology Clerkship OverviewDocument16 pagesObstetrics and Gynecology Clerkship Overviewselvie8750% (2)
- AspatDocument113 pagesAspatSridhar BabuNo ratings yet
- Nurse Practitioner Wound Management Clinical ProtocolsDocument29 pagesNurse Practitioner Wound Management Clinical ProtocolsBrian HarrisNo ratings yet
- Blood Pressure Screening Form 0907Document2 pagesBlood Pressure Screening Form 0907Meganne Walsh100% (2)
- Book Guide For Clincal Rotations - Revised by ASODocument5 pagesBook Guide For Clincal Rotations - Revised by ASOOscar HotelNo ratings yet
- Downtime Daily Nursing Assessment & Care Plan: 1 of 5 Date: TimeDocument5 pagesDowntime Daily Nursing Assessment & Care Plan: 1 of 5 Date: TimerupaliNo ratings yet
- SOAP NotesDocument4 pagesSOAP Notesemmag79No ratings yet
- Legal and Ethical Issues in Psychiatric NursingDocument38 pagesLegal and Ethical Issues in Psychiatric NursingElizabeth McKee100% (2)
- Travel Nurse Pdf1Document2 pagesTravel Nurse Pdf1Med NetNo ratings yet
- South University College of Nursing Nursing Process Worksheet STUDENT: - Erica Clipps - NSG 3038 - FACULTY - Baby PlaceDocument3 pagesSouth University College of Nursing Nursing Process Worksheet STUDENT: - Erica Clipps - NSG 3038 - FACULTY - Baby PlaceErica ClippsNo ratings yet
- High Risk Antepartum Nursing Care 4Document51 pagesHigh Risk Antepartum Nursing Care 4Wendy EvansNo ratings yet
- The Nurse Practitioner in UrologyFrom EverandThe Nurse Practitioner in UrologyMichelle LajinessNo ratings yet
- Brochure - Future Health Suraksha Family FloaterDocument2 pagesBrochure - Future Health Suraksha Family FloaterSandeep GhosthNo ratings yet
- Trading Account Opening Form: Mandatory Documents Document Significance Page NumberDocument11 pagesTrading Account Opening Form: Mandatory Documents Document Significance Page NumberSandeep GhosthNo ratings yet
- bbm:978 88 470 5421 9/1/1Document2 pagesbbm:978 88 470 5421 9/1/1Sandeep GhosthNo ratings yet
- Brochure - Future Health Suraksha Family FloaterDocument2 pagesBrochure - Future Health Suraksha Family FloaterSandeep GhosthNo ratings yet
- 6Document9 pages6Sandeep GhosthNo ratings yet
- Silver Health BrochureDocument2 pagesSilver Health BrochureSandeep GhosthNo ratings yet
- 6Document9 pages6Sandeep GhosthNo ratings yet
- Trading Account Opening Form: Mandatory Documents Document Significance Page NumberDocument11 pagesTrading Account Opening Form: Mandatory Documents Document Significance Page NumberSandeep GhosthNo ratings yet
- TRADEPLUS - Electronic Contract Notes For MCXDocument1 pageTRADEPLUS - Electronic Contract Notes For MCXSandeep GhosthNo ratings yet
- bbm:978 88 470 5421 9/1/1Document2 pagesbbm:978 88 470 5421 9/1/1Sandeep GhosthNo ratings yet
- Brochure - Future Health Suraksha IndividualDocument2 pagesBrochure - Future Health Suraksha IndividualSandeep GhosthNo ratings yet
- Brochure - Future Health Suraksha IndividualDocument2 pagesBrochure - Future Health Suraksha IndividualSandeep GhosthNo ratings yet
- Harvard Medical School: Exclerk Application InformationDocument2 pagesHarvard Medical School: Exclerk Application InformationSandeep GhosthNo ratings yet
- What Do You Need To Know About OsteoarthritisDocument2 pagesWhat Do You Need To Know About OsteoarthritisSandeep GhosthNo ratings yet
- 16Document50 pages16Sandeep GhosthNo ratings yet
- FutureHealthSuraksha Individual EBrochureDocument6 pagesFutureHealthSuraksha Individual EBrochureSandeep GhosthNo ratings yet
- Brochure - Future Health Suraksha Family FloaterDocument2 pagesBrochure - Future Health Suraksha Family FloaterSandeep GhosthNo ratings yet
- Health Guard Brochure 2013 R6Document2 pagesHealth Guard Brochure 2013 R6Sandeep GhosthNo ratings yet
- 16Document50 pages16Sandeep GhosthNo ratings yet
- Special Sensory - Smell: Somatic Motor Somatic MotorDocument7 pagesSpecial Sensory - Smell: Somatic Motor Somatic MotorSandeep GhosthNo ratings yet
- Brochure - Future Health Suraksha Family FloaterDocument2 pagesBrochure - Future Health Suraksha Family FloaterSandeep GhosthNo ratings yet
- Class of 2014 - USMLE Step 1 ResourcesDocument21 pagesClass of 2014 - USMLE Step 1 Resourcesashr97No ratings yet
- Vs Malpractice ChecklistDocument2 pagesVs Malpractice ChecklistSandeep GhosthNo ratings yet
- Chintamani PHCDocument2 pagesChintamani PHCSandeep GhosthNo ratings yet
- 20100325000237Document13 pages20100325000237Sandeep GhosthNo ratings yet
- Health Guard Brochure 2013 R6Document2 pagesHealth Guard Brochure 2013 R6Sandeep GhosthNo ratings yet
- Brochure - Future Health Suraksha IndividualDocument2 pagesBrochure - Future Health Suraksha IndividualSandeep GhosthNo ratings yet
- What Do You Need To Know About OsteoarthritisDocument2 pagesWhat Do You Need To Know About OsteoarthritisSandeep GhosthNo ratings yet
- Silver Health BrochureDocument2 pagesSilver Health BrochureSandeep GhosthNo ratings yet
- Information For Prospective Foreign Visiting StudentsDocument3 pagesInformation For Prospective Foreign Visiting StudentsSandeep GhosthNo ratings yet
- ERPM Viva Long Cases III v2.0Document17 pagesERPM Viva Long Cases III v2.0Bhagya Pramodh AriyarathnaNo ratings yet
- Lymph Node EnlargementDocument6 pagesLymph Node Enlargementlucas mansanoNo ratings yet
- Preoperative Testing and Medication ManagementDocument27 pagesPreoperative Testing and Medication ManagementWidya JelitaNo ratings yet
- The GPHC Question List Jun17-Mch21Document35 pagesThe GPHC Question List Jun17-Mch21Patrick MathewNo ratings yet
- Policy Analysis ReportDocument16 pagesPolicy Analysis ReportGhelvin Auriele AguirreNo ratings yet
- The 25 Golden Rules of RunningDocument10 pagesThe 25 Golden Rules of RunningvivektonapiNo ratings yet
- IMCIDocument11 pagesIMCIJoshua Villarba100% (1)
- Screening For Microalbuminuria in Patients With Diabetes: How? Why?Document2 pagesScreening For Microalbuminuria in Patients With Diabetes: How? Why?Abhishek SenNo ratings yet
- World Hunger Web QuestDocument5 pagesWorld Hunger Web Questapi-313403351No ratings yet
- Osteoarthritis: Causes, Symptoms, Diagnosis and TreatmentDocument34 pagesOsteoarthritis: Causes, Symptoms, Diagnosis and TreatmentRosmana PuteraNo ratings yet
- Esophagus: DrzaiterDocument37 pagesEsophagus: DrzaiterdrynwhylNo ratings yet
- List Nama Cantik & Kel. Yel-Yel 2022Document3 pagesList Nama Cantik & Kel. Yel-Yel 2022Daffa RamadhaniNo ratings yet
- GERD Algorithm Review Definition and Pathophysiology: NO YESDocument3 pagesGERD Algorithm Review Definition and Pathophysiology: NO YESdianyNo ratings yet
- PAFP Consensus Guidelines On Preparation and Resumption of Clinic Services - FINALDocument17 pagesPAFP Consensus Guidelines On Preparation and Resumption of Clinic Services - FINALPatricia Franco-VillaNo ratings yet
- Drug StudyDocument3 pagesDrug StudyKorina FranciscoNo ratings yet
- Headache in ChildrenDocument34 pagesHeadache in Childrensai saiNo ratings yet
- Pediatric Pneumonia - Practice Essentials, Background, PathophysiologyDocument1 pagePediatric Pneumonia - Practice Essentials, Background, PathophysiologyShiferaw TesfayeNo ratings yet
- AEF2e TB4 VP 2Document2 pagesAEF2e TB4 VP 2Minji LeeNo ratings yet
- Idea DisabilitiesDocument6 pagesIdea Disabilitiesapi-425284294No ratings yet
- Bronchial AsthmaDocument3 pagesBronchial AsthmaSabrina Reyes0% (1)
- Chapter 21 DigestionDocument96 pagesChapter 21 DigestionJwnsbdhdNo ratings yet
- Growing in Vitro Diagnostics (IVD) Market To Set New Business Opportunities For Start Up CompanyDocument2 pagesGrowing in Vitro Diagnostics (IVD) Market To Set New Business Opportunities For Start Up CompanyPR.comNo ratings yet
- Morgellons DiseaseDocument5 pagesMorgellons Diseasenotyourakiko18No ratings yet
- Animal Health and Welfare Module 1Document127 pagesAnimal Health and Welfare Module 1prevosterfuturemwampweNo ratings yet