Professional Documents
Culture Documents
Lecture 11 Oct 25th-Respiratory
Uploaded by
api-26938624Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lecture 11 Oct 25th-Respiratory
Uploaded by
api-26938624Copyright:
Available Formats
October 25th, 2006
Respiratory conditions
Conditions of the respiratory system
Insidious onset=How a condition started is unknown
NAD=No Acute Distress (circulatory, systemic, respiratory)
PND= Paroxismal Nocturnal Dyspnea
Chronic Bronchitis/lung cancer not about how long patient has smoked (ie. 1/2 pack/day
for 20 years) but how much they smoke (50 packs/year for 3 years)
3 pillow orthopnea: sleeps with 3 pillows in order to be able to breathe
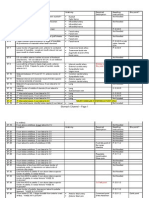
Case 2: 58-year old woman with insidious onset chronic cough of 3 month duration.
Cough keeps waking her up at night. She is currently unemployed, lives in cooperative
housing (subsidized) with boyfriend. She is reliable, interacts well, NAD, W/N
Px denies SOB on exertion, weight loss, fever, diarrhea, anorexia, bouts of confusion or
memory loss.
Smoker, 20 pks/year, PND and 3 pillow orthopnea.
Physical exam:
Height: 163 cm
Weight: 142 lbs
BP: 151/98
68 bpm
37.3 C
14 rpm
No central/peripheral cyanosis, no clubbing, no delayed capillary refill.
No rales bilaterally, + rhonchi, + expiratory wheeze, clear to percussion.
What is going on?
Do you need to ask more questions? Why?
Are there any red flags in this case?
How would you manage this case in your office?
Ddx.
Lung cancer (no fever, chronic cough)
• Chronic bronchitis (more gradual onset) history says, no probably not 3m, probably
5-10 years. Also, CB lets you sleep at night. Takes >3 months to develop.
• Emphysema (takes >3 months to develop), not disturbing because it has a gradual
onset.
DDX LECTURE 11, OCTOBER 25TH – PAGE 1
• Remember that there can be many things happening at the same time (eg. Chronic
bronchitis, lung cancer)
How long has the patient been living in a co-op? Might be mold.
NOTE: Pathology is not on exam
LARYNGOTRACHEOBRONCHITIS (CROUP)
• Abnormal malformation of glottis
ACUTE EPIGLOTTITIS
• Can be fatal: must go to hospital
• Not good if not intubated
PERTUSSIS (WHOPPING COUGH)
• Happens to children and adults
• Typically builds up and may end with vomiting
• Scary to see: the patient can’t get enough air.
• www.whoopingcough.net/symptoms.htm Can listen to sounds.
• After bout, patient is fine.
• Respiratory distress always requires action.
• Coughing can cause hemorrhage (eg. in conjunctiva)
• If you are new to practice and haven’t seen this a lot, have someone else involved
that HAS seen it a lot.
• Antibiotics do not affect course of disease
• Contagious
• Note: afebrile for DDx
ASTHMA
• Inflammatory disorder characterized by:
• Hyperactivity of immune system (to dust derivatives, smoke)
• Air flow obstruction
• If not addressed, inflammation will produce fibrosis of lung.
• Most children with asthma improve during adolescence.
• Hypochlorhydria (low stomach HCl) may be contributing problem (improper
digestion?)
• Pthophysiology is very important in asthma.
• Exposure to allergen local mediator release inflammatory compound release
local constriction of smooth muscle chemotaxic factor release epithelial and
neural damage widespread effect.
• (from list above: inflammatory compound release also causes increase capillary
permeability)
DDX LECTURE 11, OCTOBER 25TH – PAGE 2
• If the immune response is engaged with 1 thing, others may get through, leading to
pneumonia (squawk that precedes crackle: sounds like a chicken)
• Chest X-ray for asthma: history is important (patient coughing?).
o In a normal chest x-ray, rib markings are visible
o In asthma attack, no rib markings can be seen
o Lung is hyperinflated
o Diaphragmatic margin pushed down due to inflated lung.
• In asthma, problem is with exhalation, during acute attack.
• Sputum is produced because the immune system thinks you have an infection
• Important to know red flags, to be comfortable managing an asthma case.
• Disappearance of wheeze: patient may not be breathing anymore
• Red flags are missed all the time because the doctor’s belief in the treatment blinds
them to patient symptoms
• Good way to assess treatment is with a peak flow meter. Should be above 70%.
• Asthma causes serious damage, people die form untreated asthma. Take it very
seriously.
• Usually, asthma attacks are not concerning. Red flags are very concering. Do no
harm = death. Have epinephrine for auto-injection, emergency medications on
hand.
• Many things look like asthma, it is very difficult to diagnose. Best to test breathing
capacity, give patient a dose of universal irritant. Patient’s FEV will be reduced by
more than 20% after challenge.
• Every time a provocation test isn’t done = misdiagnosis
• Children can compensate a lot, loss of symptoms may not mean 70% PFR,
important to manage case properly, even if PFR is 80-90%
• Important to coach /encourage patient during use of spirometer for assessment.
• Normal lungs exhale most of the air in 1st second. Not measuring force, but amount
of air.
• PFM: Peak flow meter: measure speed of air. Done with asthma.
Confirmatory evaluation:
Do bronchial lavage when REALLY confused. TB cells, cancer cells, show up in
bronchial lavage.
ELISA can be done if looking for disease
This type of evaluation: not really part of DDx. Need to understand DDx on its own.
If the test won’t affect the management of the condition, it may not be worth it to do the
test.
Better to ask for opinions, not tests (invasive).
(PFT is the same as spirometry. PFT is a better term.)
DDX LECTURE 11, OCTOBER 25TH – PAGE 3
Difference between obstructive and restrictive pulmonary disease is usually on NPLEX.
ACUTE BRONCHITIS
• Should go away in about 3 weeks.
• Cold, cough
• Rhonchi sounds bubbly or gurgly.
• Crackles: alveoli that are closed, opening with a “snap!”
• Obstruction due to infection
BRONCHIECTASIS
• Sputum, pus accumulates. Lung fills up when patient stands
• Needs to be resolved/cured, not “managed”.
• Causes irreversible destruction of bronchi/alveoli
• Can lead to respiratory failure.
COR PULMONALE
• Capillaries are “narrow sieve” that blood goes through to lungs
• Heart tries to help, increases BP
• Pulmonary hypertension occurs
• Right heart having trouble, left okay. Right ventricular problem.
• Asthma can lead to bronciectasis death
• Eventually get left ventricular failure because LV compensates by sucking harder
• On CXR: see whiteness (should be clear), pus and fibrosis all over
TUBERCULOSIS
• On the rise in Canada
• “creeps up” on patient: slow onset
• Patient comes to doctor because they have a general feeling of ill health
• Easy to miss: important to know risk factors
• With alcoholism, cilia not beating properly
• Look at history: tree planting is risk factor
• Generally patient has a clue in their history (exposure) and has a weakened immune
system
• Can be associated with community health centres
• TB incubates inside host cell. Multiplies. Immune system realizes, but the pathogen
is now encapsulated.
• Immune system expends energy (calories) to get to TB inside capsule, but TB is
safe, continues to multiply. Patient experiences weight loss
• Most of us have already been exposed to TB. Can be tested to make sure that we
don’t have it. If well nourished, can fight it.
• Be competent in what your community tends to present with
DDX LECTURE 11, OCTOBER 25TH – PAGE 4
• Cough for >2 months? Screen for TB. Mantoux test (indirect assessment)
• TB is Type IV hypersensitivity
• Can exist in eye in unexplained clear/light spot.
DDX LECTURE 11, OCTOBER 25TH – PAGE 5
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Chinese Medicine PsychologyDocument315 pagesChinese Medicine PsychologyPaco Ladera100% (5)
- B0dfbaf2 Beed 4ca7 99fb Ff3588d75dc0Document3 pagesB0dfbaf2 Beed 4ca7 99fb Ff3588d75dc0api-26938624No ratings yet
- Endocrine System IDocument2 pagesEndocrine System Iapi-26938624No ratings yet
- 13ffd1fa Eda0 4eb8 Bb3a 7802feec40daDocument40 pages13ffd1fa Eda0 4eb8 Bb3a 7802feec40daapi-26938624No ratings yet
- c1fd6bbd Ff7a 480d A20e C93bd3a3cedfDocument35 pagesc1fd6bbd Ff7a 480d A20e C93bd3a3cedfapi-26938624No ratings yet
- Lecture 47 April 13th-EndocrineDocument1 pageLecture 47 April 13th-Endocrineapi-26938624No ratings yet
- Lecture 50 April 20th-DiabetesDocument2 pagesLecture 50 April 20th-Diabetesapi-26938624No ratings yet
- Lecture 46 April 11th-EndocrineDocument3 pagesLecture 46 April 11th-Endocrineapi-26938624No ratings yet
- Lecture 31 January 31st-GIDocument3 pagesLecture 31 January 31st-GIapi-26938624No ratings yet
- Lecture 44 March 30th - NO NOTESDocument1 pageLecture 44 March 30th - NO NOTESapi-26938624No ratings yet
- Lecture 42 March 23rd-NervousDocument2 pagesLecture 42 March 23rd-Nervousapi-26938624No ratings yet
- Conditions of The Musculoskeleltal SystemDocument4 pagesConditions of The Musculoskeleltal Systemapi-26938624No ratings yet
- Lecture 40 March 14th-MSKDocument5 pagesLecture 40 March 14th-MSKapi-26938624No ratings yet
- DDX - Gastrointestinal Disorders ChartDocument21 pagesDDX - Gastrointestinal Disorders Chartapi-26938624100% (2)
- Lecture 29 January 24th-GIDocument3 pagesLecture 29 January 24th-GIapi-26938624No ratings yet
- Lecture 28 January 19th-GIDocument3 pagesLecture 28 January 19th-GIapi-26938624No ratings yet
- DDX HT RemedyDocument1 pageDDX HT Remedyapi-26938624No ratings yet
- Lecture 24 December 8th-CV ND LectureDocument3 pagesLecture 24 December 8th-CV ND Lectureapi-26938624No ratings yet
- Lecture 22 December 1st - CLASS CANCELLEDDocument1 pageLecture 22 December 1st - CLASS CANCELLEDapi-26938624No ratings yet
- Chapter - 014 Student HandoutsDocument16 pagesChapter - 014 Student Handoutsebiniyam2021No ratings yet
- Contents (Continued) : Chapter 5. Nondestructive Inspection (Ndi)Document3 pagesContents (Continued) : Chapter 5. Nondestructive Inspection (Ndi)blackhawkNo ratings yet
- Icare Pivc GuidelineDocument26 pagesIcare Pivc GuidelineCarissa CkNo ratings yet
- Virtual Long Bone DissectionDocument2 pagesVirtual Long Bone Dissectionapi-438665079No ratings yet
- A Case Study On Ascites of Hepatic OriginDocument4 pagesA Case Study On Ascites of Hepatic OriginFaisal MohommadNo ratings yet
- Concept Map 3 MM (Abdominal Pain)Document2 pagesConcept Map 3 MM (Abdominal Pain)Matt McKinleyNo ratings yet
- Brodil LevoDocument2 pagesBrodil LevoAziza KhairunNo ratings yet
- Uptd Puskesmas Sindar Raya: Pemerintah Kabupaten Simalungun Dinas KesehatanDocument2 pagesUptd Puskesmas Sindar Raya: Pemerintah Kabupaten Simalungun Dinas KesehatanulfayuliNo ratings yet
- Guterbock Hittite MedicineDocument6 pagesGuterbock Hittite MedicineTarek AliNo ratings yet
- MSDS Pupuk Haracoat PDFDocument4 pagesMSDS Pupuk Haracoat PDFAnonymous UQVygYg3lfNo ratings yet
- Name: Shafiq Ur Rahman Class No. 36 BSN Year-Iii, Semester-Vi Topic: "Reflection On Subject of Mental Health Nursing"Document3 pagesName: Shafiq Ur Rahman Class No. 36 BSN Year-Iii, Semester-Vi Topic: "Reflection On Subject of Mental Health Nursing"Shafiq Ur RahmanNo ratings yet
- What Is Personal HygieneDocument4 pagesWhat Is Personal HygieneAnonymous 0FWhoTu100% (1)
- Degnala DiseaseDocument12 pagesDegnala DiseaseSantosh Bhandari100% (1)
- Genetic Disorders Screening and PreventionDocument36 pagesGenetic Disorders Screening and PreventionManovaPrasannaKumarNo ratings yet
- Fiji Times Jan 7Document48 pagesFiji Times Jan 7fijitimescanadaNo ratings yet
- Asymptomatic HyperuricemiaDocument46 pagesAsymptomatic HyperuricemiaDivya Shree100% (1)
- Nasya Treatment: DefinitionDocument4 pagesNasya Treatment: DefinitionkaukabNo ratings yet
- Organon of Medicine All Years 2marks Question Viva Questions AnswersDocument12 pagesOrganon of Medicine All Years 2marks Question Viva Questions Answersabcxyz15021999No ratings yet
- Care PlanDocument4 pagesCare Planapi-217086261No ratings yet
- Johns Hopkins Dean - Reflections On Medical School AdmissionsDocument4 pagesJohns Hopkins Dean - Reflections On Medical School AdmissionstheintrepiddodgerNo ratings yet
- IonnyDocument4 pagesIonnyLu KaNo ratings yet
- Stock Per 2 Nov 20 HargaDocument13 pagesStock Per 2 Nov 20 HargaLutfi QamariNo ratings yet
- Physical Capabilities of Instructors at The End of Hot Fire Training (0305) (158529)Document42 pagesPhysical Capabilities of Instructors at The End of Hot Fire Training (0305) (158529)Onion PapaNo ratings yet
- Damolo, Jules Aldrich C. October 30, 2021 Bsit 1 Year Block - A Instructor: Jerson CamayDocument3 pagesDamolo, Jules Aldrich C. October 30, 2021 Bsit 1 Year Block - A Instructor: Jerson CamayAldrich Dos DamoloNo ratings yet
- Assessment of Time Perception The Effect of AgingDocument10 pagesAssessment of Time Perception The Effect of AgingYuki ChongNo ratings yet
- Cardioversion of Atrial Fibrillation and AtrialDocument13 pagesCardioversion of Atrial Fibrillation and AtrialLabontu IustinaNo ratings yet
- FB-08 05 2023+furtherDocument100 pagesFB-08 05 2023+furtherP Eng Suraj Singh100% (1)
- Machupo VirusDocument15 pagesMachupo VirusiggyNo ratings yet
- Common Sports InjuryDocument71 pagesCommon Sports InjuryGlen Dizon100% (1)