Professional Documents
Culture Documents
Patho - Dses of The Kidney1
Uploaded by
Kate MendozaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Patho - Dses of The Kidney1
Uploaded by
Kate MendozaCopyright:
Available Formats
PATHOLOGY: DISEASES OF THE KIDNEY PART1
Components of the normal kidney Blood vessels Glomeruli o Components of the Glomerulus Endothelial cells- line the glomerular capillaries GBM- composed of collagen, laminin, proteoglycan, fibronectin; effective filtration barrier Lamina rara interna Lamina densa Lamina rara externa Visceral epithelial cells (podocytes) Foot processes- enclose/ wrap around capillaries Filtration slits- b/w foot processes Slit diaphragm- made up of CHONs Mesangial cells- contractile, phagocytic, secrete mediators, capable of proliferation Tubules Interstitium Features of the Filtration Barrier Highly permeable to water and solutes Impermeable to CHONs o Size of CHONs o Charge of CHONs o Slit diaphragm AZOTEMIA Biochemical abnormality Elevated BUN Elevated creatinine o d/t decreased GFR: pre-renal (CHF, shock) post-renal (obstruction) UREMIA Azotemia + clinical s/sxs Failure of renal fxn Metab and endo d/o 2ndary involvement of GIT, peripheral NS, CVS 4. ARF- acute azotemia assoc with oliguria/anuria 5. CRF- prolonged uremia, END STAGE of all renal dse 6. Manifestations of renal tubular defects- polyuria, nocturia, electrolyte imbalance 7. UTI- pyuria, bacteuria 8. Nephrolithiasis- renal colic, hematuria 9. Urinary tract obstruction and renal tumors NEPHRITIC Hematuria Mild to moderate proteinuria HPN NEPHROTIC Heavy proteinuria Hypoalbuminemia Severe edema Hyperlipidemia Lipiduria
Stages of CRF STAGE Diminished renal reserve Renal insufficiency Renal failure End-stage renal dse
GFR 50% 20-50% <2025% <5%
CHARACTERISTIC Susceptible to developing azotemia Azotemia assoc with anemia and HPN Edema, metab acidosis, uremia Kidney doesnt become fxnal at all
Clinical presentations of Renal Dses 1. Acute nephritic syndrome- acute onset of gross hematuria, mild to moderate proteinuria, HPN 2. Nephrotic syndrome- marked hematuria, hyperlipidemia 3. Asymptomatic hematuria/ proteinuria
I.
GLOMERULAR DSES A. Primary (kidney itself) vs. Secondary (d/t a 10 systemic d/o~ eg: DM, SLE)
B. Manifestations of Glomerular Dse (Glomerular Syndromes)
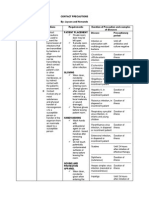
- Additional syndromes (not discussed): CRF, Asymptomatic Hematuria/ proteinuria SYNDROME NEPHRITIC SYNDROME (Acute RPGN(Rapidly Progressive GN; Crescentic) Proliferative Glomerulonephritis) CHARACTERIS - Inflammatory changes in the glomeruli - Crescents and rapid loss of renal fxn TIC and acute nephritis - Severe oliguria and death within wks/ - Hematuria, azotemia, variable mos if left untreated proteinuria, oliguria, edema (not - May be idiopathic (50%)/ assoc with severe), HPN other renal/ extrarenal dse - 95% recover - <1% RPGN - Clinical course is not as good in adults TYPE 1. Post- Streptococcal (prototype) 1. Type I- Anti-GBM Ab-induced (IgG and 2. Post- Infectious C3 in GBM) IF: linear a. Renal limited- idiopathic b. Goodpastures Syndrome- d/t vasculitis, changes seen both in kidneys and lungs 2. Type II- Immune Complex IF: granular a. Idiopathic b. Post- infectious- manifests as nephritic syndrome c. SLE, etc. 3. Type III- Pauci- Immune (no immune complex/ anti-GBM Ab) IF: none a. ANCA- associated b. Idiopathic c. Wegeners granulomatosisvasculitis d. Microscopic polyangitisvasculitis DESCRIPTION Post- Streptococcal --- 6-10y/o - 1-4wks after strep infxn - GABHS (type1, 4, 12) MECHANISM - Ab to planted Ag --- Deposition of circulating immune complexes NEPHROTIC SYNDROME
Massive proteinuria (3.5g or more/day) Hypoalbuminemia (>3g/dl) Generalized edema Hyperlipidemia and lipiduria
---
---
Increased permeability of glom. capillary wall escape of plasma CHONs (proteinuria) depletion of serum albumin (hypoalbuminemia) edema
MORPHOLOGY Enlarged, hypercellular glomeruli o Diffuse leukocyte infiltration (neutrophils and monocytes) o Proliferation of endothelial and mesangial cells (swelling of endothelial cells) o Crescent formation in severe cases Obliteration of glomerular capillary lumina IF: granular deposits in mesangium and GBM (IgG, IgM and C3) EM: subepithelial humps Elevated ASO Decreased serum complement (activation of complement system and consumption of complement components)
Enlarged kidneys, pale, petechiae Crescents with fibrin srands EM: ruptures in the GBM causes transudation into the bowmans capsule
d/t oncotic pressure (pitting/periorbital/generalized ) Na and water retention aggravates edema Increased hepatic synthesis of lipoproteins, abn lipid transport, decreased lipid catabolism hyperlipidemia lipiduria Loss of Ig susceptibility to infxns Loss of anticoagulant factors thrombotic and thromboembolic cx ---
Dx
---
---
Glomerular Dse presenting as Nephrotic Syndrome DISEASE MEMBRANOUS MINIMAL CHANGE DSE (Nils Dse GLOMERULOPATHY Nil means cannot see anything under light microscope)
FOCAL SEGMENTAL GLOMERULOSCLEROSIS (FSGS)
MEMBRANOPROLIFERATIVE GN (MPGN)
DESCRIPTIO N
MOST COMMON CAUSE OF NEPHROTIC SYNDROME IN ADULTS Diffuse thickening of the glomerular capillary wall Sub-epithelial deposits of electron-dense material 85%- idiopathic/ some are 2ndary
MOST FREQUENT CAUSE OF NEPHROTIC SYNDROME IN CHILDREN (2-6y/o) Diffuse effacement of epithelial foot processes Glomeruli look normal by LM Dramatic response to corticosteroids
Sclerosis of a portion of the glomerular tuft (segmental) in some glomeruli (focal) Occurs in the ff settings: o In assoc with HIV, heroin addiction, sickle cell dse and obesity o 20 event in other GN o Part of adaptive response to loss of renal tissue o Hereditary NS with gene mutations o Idiopathic- 10% of NS in children; 35% of NS in adults Hallmark: degeneration and disruption of visceral epithelial cells May represent an accentuation of changes in minimal change dse
Nephrotic syndrome in 10-20% of children and adults Changes in BM Proliferation of glomerular cells (predominantly mesangial) Leukocyte infiltration
CAUSES
Assoc with: drugs, malignancies, SLE, infxns, other autoimmune d/os Autoimmune dse linked to susceptibility genes Caused most likely by Ab to a renal autoAg
---
Elaboration of cytokine that damages visceral epithelial cells Mutations in genes that encode for CHONs which are component of the slit diaphragm (nephrin and podocin)
Type I (more common) Immune complexes and activation of complement pathway Ag may be planted/ part of immune complexes deposited in glomeruli Ag are believed to be derived from infectious agents (hep C/B) Subendothelial electron-dense deposits (C3, IgG, early complement components) Type II (dense-deposit dse) Activation of alternative complement pathway Deposition of unknown dense material in the GBM proper (lamina densa) Absent IgG and early- acting complement components 2ndary MPGN Chronic immune complex dse: SLE, hep B/ C, HIV, schistosomiasis 1- ATD malignancy (CLL, lymphoma) hereditary dse of complement regulatory processes ---
In-situ immune complex deposition
PATHOGENE SIS/ MECHANISM
C5b-C9 activates glomerular epithelial cells and mesangial cells cells are induced to liberate proteases and oxidants capillary wall injury leakage
Unknown; probably r/t a cytokine that damages visceral epithelial cells and cause proteinuria Features pointing to immunologic basis: o Clinical assoc with respiratory infxn and prophylactic immunization o Response to corticosteroids o Asso with atopic dse o Genetic predisposition o Increased incidence in px with Hodgkin dse Mechanisms of CHON leakage: o Defects in change barrier o Passage thru residual spaces b/w remaining podocytes o Leakage thru areas where epithelial cells have been detached o Transcellular passage o Mutation in podocyte CHONs (nephrin and podocin)
In renal ablation (compensatory hypertrophy of glomeruli hemodynamin changes epithelial and endothelial cell injury) Gene mutations: - NPHS1 (nephrin) - NPHS2 (podocin) - Gene encoding for actinbinding CHON - actinin 4 - TRPC6 gene destroys integrity of slit diaphragm exudation of fluids
---
MORPHOLO GY
Diffuse thickening of the capillary wall EM: subepithelial electron- dense deposits o Effacement of foot processes o Basement membrane material laid down b/w deposits (spikes) o Spikes later thicken and close over the deposits IF: granular IgG and C3
EM: no deposits; uniform and diffuse effacement of podocytes/ foot processes Proximal tubular epithelial cells are laden with lipid and CHON
EM: Visceral epithelial cell damage: o Effacement of foot processes o Detachment of epithelial cells o Denudation of underlying BM Insudation of plasma CHONs along capillary wall (hyalinosis) CHONs in mesangiumproliferation of mesangial cells; elaboration of more matrix (sclerosis) IF: IgM and C3 may be present in sclerotic areas or in mesangium
CLINICAL FEATURES
Non-selective proteinuria Poor response to corticosteroids Indolent clinical course
Highly selective proteinuria (albumin) Rapid response to corticosteroids (90%) Excellent long-term prognosis
---
LM: same for type I and II o Large, hypercellular glomeruli o Mesangial cells o Endothelial cells o Leukocytes o Parietal epithelial cells (crescents) o Increased mesangial matrix o Thickened GBM Duplication of BM (d/t interpostition of mesangial cell processes) TRAM TRACK (type II) Cellular elements within the BM EM and IF: o Type I- subendothelial electron dense deposits; granular pattern (C3, IgG, C1q, C4) o Type II- electron dense material in lamina densa of GBM (unknown composition) Manifests as: - Nephrotic syndrome - Hematuria only - Proteinuria only - Nephrotic-nephritic manifestations CF: - In children and young adults: nephrotic syndrome - Usually with hematuria - Slowly progressive, unremitting course - 50% with CRF in 10yrs
C. Histologic Changes
1. Hypercellularity a. Cellular proliferation (mesangial/ endothelial cells) b. Leukocytic infiltration c. Crescents (parietal epithelial cells) - RPGN
2. BM thickening a. Deposition of electron dense material immune complex b. Thickening of the BM proper 3. Hyalinosis- plasma CHONs
4. Sclerosis- collagenous material in mesangium and capillary loops; can obliterate glomerulus Distribution of Changes Diffuse- ALL glomeruli Focal- only a PROPORTION of the glomeruli Global- ENTIRE glomerulus Segmental- only a PART of the glomerulus Mesangial- affecting the MESANGIAL REGION D. Immune Mechanisms (pathogenesis) 1. Antibody- mediated a. In-situ immune complex deposition- Ab react with intrinsic Ag in the glomerulus or with Ag planted in the glomerulus from the circulation b. Circulating immune complex deposition i. Ag.-Ab complexes are trapped in the glomeruli ii. Ags may be endo/exogenous c. Cytotoxic Ab to glomerular cells 2. Cell- mediated
3. Activation of the alternative complement pathway Localization of Deposits Subepithelial/ epimembranous- beneath the podocyte/ above BM BM Subendothelial Mesangial
E. Mediators of Glomerular Injury
1. Cells: a. Neutrophils and monocytes b. Macrophages, T-lymphocytes and NK cells c. Platelets d. Glomerular cells- may produce inflammatory mediators 2. Chemical Mediators: a. Chemotactic factors b. Cytokines c. Chemokines d. Eicosanoids, NO, angiotensin and endothelin e. Coagulation system TUBULO- INTERSTITIAL FIBROSIS ---
Markers of Progressive Renal Damage: MARKER FOCAL SEGMENTAL GLOMERULOSCLEROSIS (FSGS) PATHOGENESIS Compensatory glomerular hypertrophy hemodynamic changes: increase glom bld flow filtration, capillary HPN, systemic HPN endothelial and epithelial cell injury increase permeability to CHONs CHONs accumulate in mesangium proliferation of mesangial cells, infiltrations by macrophages, increase extracellular matrix GLOMERULAR SCLEROSIS CONTRIBUTING Visceral epithelial cells cannot proliferate after injury remaining epithelial FACTOR cells are stretched and eventually denuded abn filtration, loss of structural support for glomerular capillary walls
Ischemia of tubules Acute and chronic inflammation in adjacent interstitium Damage and loss of peritubular capillary supply Proteinuria- direct injury and activation of tubular cells expression of mediators that contribute to interstitial fibrosis
Isolated Urinary Abnormalities DISEASE IgA NEPHROPATHY (BERGER DSE) DESCRIPTION Recurrent gross/ microscopic hematuria IgA deposits in the mesangium Isolated dse Assoc with Henoch- Schonlein purpura 20- liver and intestinal dses
ALPORTS SYNDROME Defective GBM synthesis d/t production of abn collagen type IV Alternating thin and thick areas in the GBM With nerve deafness and eye d/o (cataract, lens dislocation, corneal dystrophy)
BENIGN FAMILIAL HEMATURIA Diffuse thinning of the GBM (thin BM dse) Defective genes encoding 3 and 4 chains of type IV collagen
MECHANISMS PATHOGENESI S Circulating immune complex deposition (IgA- containing complexes) in the mesangium - Activation of alternative complement pathway Genetic/ acquired abnormality in immune regulation increased IgA synthesis in response to exposure to environmental Ag formation of IgA-containing immune complexes complexes are trapped in glomeruli activation of alternative complement pathway glomerular injury LM: may be normal; mesangial widening and proliferation IF: mesangial deposition of IgA EM: mesangial electron dense deposits - Older children and young adults - Gross haematuria after respiratory/ GIT infxn - With/ without proteinuria -
X- linked (female carrier), may be autosomal recessive/ dominant -----
-----
MORPHOLOGY
---
---
CLINICAL FEATURES
---
---
Chronic GN 1. RPGN- 90% 2. FSGS- 50-80% 3. Membranoproliferative GN- 50% 4. Membranous GN- 30-50% 5. IgA nephron[athy- 30-50% 6. Post-streptococcal GN- 1-2% Morphology: - Symmetrically contracted kidneys - Diffusely granular cortical surface - Thinned-out cortex - Hyaline obliteration of the glomeruli - Arterial and arteriolar sclerosis - Tubular atrophy (thyroidization) Glomerular Lesions in Systemic Dse DISEASE SLE DESCRIPTI - Kidney is involved in 60-70% of ON cases - Deposition of immune complexes
Interstitial fibrosis Leukocytic infiltration (mononuclears)
CGN Dialysis: - Arterial intimal thickening - Deposition of Ca oxalate crystals in tubules and interstitium - Acquired cystic dse - Increased risk for renal adenomas and adenocarcinomas Uremic Cx: 1. Uremic pericarditis 2. Gastroenteritis 3. 20 hyperparathyroidism 4. Nephrocalcinosis 5. Left ventricular hypertrophy d/t HPN DIABETIC NEPHROPATHY Linked with generalized diabetic microangiopathy Metab defects are responsible for the biochemical changes in the GBM AGE form cross-linkages with collagen molecules in the GBM structural and fxnal defects in the GBM enhanced CHON deposition AGE bind to receptors in many cells increased synthesis of ECM Hemodynamic effects and glomerular hypertrophy AMYLOIDOSIS Renal involvement is the most serious form
MORPHOLO GY
Class 1: Normal by LM, EM, IF Class 2: Mesangial lupus GNproliferation of mesangial cells, mildest form Class 3: Focal proliferatie GN20%, affects 50% of glomeruli, generally segmental Class 4: Diffuse proliferative GNmost serious, subendothelial deposit, wireloop lesions Class 5: Membranous GNthickening of the capillary walls; 15%
Glomerular lesions are assoc with 3 glomerular syndromes: o Non-nephrotic proteinurira o Nephrotic syndrome o CRF Capillary BM thickening Diffuse mesangial sclerosis- diffuse increase in mesangial matrix Nodular glomerulosclerosis- intercapillary glomerulosclerosis, Kimmelsteil- Wilson lesion; ball- like deposits of laminated matrix enlarge and compress capillaries renal ischemia and tubular atrophy Renal atherosclerosis. Arteriosclerosis Pyelonephritis, necrotizing papillitis
Amyloid deposits in: Glomeruli Interstitial peritubular tissue Arteries and arterioles
Katemendoza2014 ^_^
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- CPT Coding Practice QuestionsDocument10 pagesCPT Coding Practice QuestionsTannu SamadNo ratings yet
- Testicular TumorsDocument42 pagesTesticular TumorsarhamNo ratings yet
- Epidemiology of Diabetes MellitusDocument72 pagesEpidemiology of Diabetes MellitusAnonymous RRkF0x67% (3)
- APPROACH TO MANAGING JOINT PAINDocument44 pagesAPPROACH TO MANAGING JOINT PAINKavya Anoop100% (1)
- HAAD Exam For Nurses Questions 2018Document46 pagesHAAD Exam For Nurses Questions 2018Asif Newaz100% (6)
- AHA Vs ERC GuidelinesDocument39 pagesAHA Vs ERC GuidelinesYoel Harianto100% (2)
- Soft Tissue InjuryDocument72 pagesSoft Tissue InjuryCucu Ne Eyang Kakung75% (8)
- Nursing Care Plan Assessment Nursing Diagnosis Planning Implementation Rationale Evaluation Subjective: Objective: STG: at The End of 1 DependentDocument1 pageNursing Care Plan Assessment Nursing Diagnosis Planning Implementation Rationale Evaluation Subjective: Objective: STG: at The End of 1 DependentThomas FarrishNo ratings yet
- Lesions of Oral Soft Tissues in Children PedoDocument74 pagesLesions of Oral Soft Tissues in Children PedoFourthMolar.comNo ratings yet
- NCP AidsDocument16 pagesNCP AidstferdianingsihNo ratings yet
- NCLEX Practice Exam For Pharmacology - Musculoskeletal Medications - RNpediaDocument8 pagesNCLEX Practice Exam For Pharmacology - Musculoskeletal Medications - RNpediaKristine SingsonNo ratings yet
- Nursing Care Plan for Hiatal Hernia ReliefDocument3 pagesNursing Care Plan for Hiatal Hernia ReliefLalaine Nadulpit100% (2)
- Antiviral AgentsDocument14 pagesAntiviral AgentsKate MendozaNo ratings yet
- Pharma Ans3Document18 pagesPharma Ans3Kate MendozaNo ratings yet
- Blood Transfusion (CP)Document15 pagesBlood Transfusion (CP)Kate MendozaNo ratings yet
- Sbo2 - PathoDocument7 pagesSbo2 - PathoKate MendozaNo ratings yet
- Sbo1 - PathoDocument11 pagesSbo1 - PathoKate MendozaNo ratings yet
- Journal Club: DR Meera Nandan 3 Year MD ClinicalyogaDocument54 pagesJournal Club: DR Meera Nandan 3 Year MD ClinicalyogaMeera NandanNo ratings yet
- Contact PrecautionsDocument2 pagesContact PrecautionsCristina L. JaysonNo ratings yet
- BIO K 211 TDS (EN) Fasciola Hepatica SeroDocument4 pagesBIO K 211 TDS (EN) Fasciola Hepatica SeroPia Loreto Cid TroncosoNo ratings yet
- Freelance Interactive Medical Advisor TestDocument2 pagesFreelance Interactive Medical Advisor TestNiki Erista AyudiaNo ratings yet
- Health Screening Form For EmployeesDocument5 pagesHealth Screening Form For EmployeesArun MmohantyNo ratings yet
- Psych EnhancementDocument4 pagesPsych EnhancementRalph Elvin MacanlalayNo ratings yet
- Analisis Metode Certainty Factor Pada Sistem Pakar Diagnosa Penyakit THTDocument6 pagesAnalisis Metode Certainty Factor Pada Sistem Pakar Diagnosa Penyakit THTryuzen000No ratings yet
- Lash Lift Waiver and File SheetDocument2 pagesLash Lift Waiver and File SheettiffyoloNo ratings yet
- Dengue Virus Infection - Prevention and Treatment - UpToDateDocument32 pagesDengue Virus Infection - Prevention and Treatment - UpToDateAnderson SilvaNo ratings yet
- Head Injury and concussion-ENDocument5 pagesHead Injury and concussion-ENJasly SafeerNo ratings yet
- Shan AsfDocument2 pagesShan AsfM.Fizan JavedNo ratings yet
- Pressure Ulcers Project - EditedDocument6 pagesPressure Ulcers Project - EditedZeera MohamadNo ratings yet
- VAERS Report Details Deaths and Adverse Events Following COVID VaccinesDocument234 pagesVAERS Report Details Deaths and Adverse Events Following COVID VaccinesbeneNo ratings yet
- Test Description Revid TesDocument4 pagesTest Description Revid Tesjoe andarestaNo ratings yet
- NitrofurantoinDocument3 pagesNitrofurantoinapi-3797941No ratings yet
- StudentsDocument756 pagesStudentsxxx xNo ratings yet
- Complications of Systemic Lupus Erythematosus A ReviewDocument8 pagesComplications of Systemic Lupus Erythematosus A ReviewIrsanti SasmitaNo ratings yet
- Vulvar and Vaginal Benign LesionsDocument8 pagesVulvar and Vaginal Benign LesionsKristine VanzuelaNo ratings yet