Professional Documents
Culture Documents
Postmortem Biochemistry of Vitreous Humor and Glucose Metabolism
Uploaded by
sbeyeforhireOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Postmortem Biochemistry of Vitreous Humor and Glucose Metabolism
Uploaded by
sbeyeforhireCopyright:
Available Formats
Article in press - uncorrected proof
Clin Chem Lab Med 2011;49(8):12651270 2011 by Walter de Gruyter Berlin Boston. DOI 10.1515/CCLM.2011.638
Minireview
Post-mortem biochemistry of vitreous humor and glucose metabolism: an update
Camille Boulagnon1,*, Roselyne Garnotel2, Paul Fornes1 and Philippe Gillery2
1
Department of Pathology, University Hospital, Reims, France 2 Laboratory of Pediatric Biology and Research, University Hospital, Reims, France
Abstract
Post-mortem biochemistry, also called thanatochemistry, has proved useful in forensics for estimating the time since death and assessing the cause of death. Ketoacidosis is a frequent complication of diabetes mellitus which can be lethal, with possible medicolegal implications. However, interpretation of biochemical analyses is difficult because of post-mortem blood alterations involving glucose metabolic pathways. Vitreous humor is better preserved than blood after death, and therefore is preferentially used in thanatochemistry. However, both the lack of experience of most biochemists with this matrix in clinical practice, and the paucity of post-mortem studies make interpretation of post-mortem analyses difficult. This review examines the recent advances in the knowledge of glucose metabolism in vitreous humor, and the methods used for the post-mortem diagnosis of diabetic complications. Keywords: biochemistry; diabetes mellitus; forensics; glucose; post-mortem; vitreous humor.
preserved than blood after death, and therefore is preferentially used in thanatochemistry (1, 35). Ketoacidosis is a frequent complication of diabetes mellitus which can be lethal, with possible medicolegal implications. Vitreous humor is the matrix of choice for this diagnosis because of post-mortem alterations involving glucose metabolic pathways. However, the lack of experience of most biochemists with this matrix in clinical practice and the paucity of post-mortem studies make interpretation of post-mortem analyses difficult. This review examines the recent advances in the knowledge of glucose metabolism in vitreous humor, and the methods used for the post-mortem diagnosis of complications of diabetes.
Vitreous humor
Vitreous humor is a crystal clear fluid located in the posterior part of the ocular bulb. It is composed of a complex network of cross-linked collagen fibers and hydrophilic glycosaminoglycan hyaluronan (6), which constitutes a hydrated gel containing few cells (4, 5). This well protected matrix is rarely subjected to bacterial contamination (4, 5, 7), and can easily be obtained by puncture (3, 4). Moreover, its composition is more stable and less affected by post-mortem changes than cerebrospinal fluid or blood (1). Vitreous humor is therefore preferentially used in thanatochemistry. After death, equilibrium of small molecule concentrations between blood and vitreous humor is slow, especially in case of high ante-mortem blood glucose concentrations (3, 4). In the early post-mortem period, vitreous humor has the same appearance as in vivo. With the development of body decomposition or in some ocular diseases, the vitreous humor becomes cloudy or brownish (1, 4). Because this matrix is rarely analyzed in clinical practice, no standardized methods have been validated, and no approved normal ranges are available. The only relevant clinical study performed in patients with diabetic retinopathy showed that vitreous glucose concentration in non-diabetic patients was 3.5"1.8 mmol/L vs. 6.9"3.6 mmol/L in type 2 diabetic patients, and 9.4"3.3 mmol/L in type 1 diabetic patients (8). Some authors have reported between-eye differences in the post-mortem concentrations of electrolytes (9). Among other reasons, ophthalmic diseases, such as retinal detachment, could explain these discrepancies (10). This finding has raised the question of whether vitreous humor should be
Introduction
Post-mortem biochemistry, also called thanatochemistry, has proved useful in forensics in estimating the time since death and assessing the cause of death (13). However, interpretation of biochemical analyses is difficult because of postmortem blood alterations. Consequently, standardized and validated methods, including well-defined preanalytical and analytical procedures used in clinical practice, cannot be applied to post-mortem assays. In particular, special attention must be paid to preanalytical procedures, since post-mortem changes are specific for each matrix. Vitreous humor is better
*Corresponding author: Camille Boulagnon, Laboratoire dAnatomie Pathologique, Hopital Robert Debre, CHU de Reims, Avenue du General Koenig, 51092 Reims Cedex, France Phone: q33 3 26 78 43 00, Fax: q33 3 26 78 43 11, E-mail: camille.boulagnon@etudiant.univ-reims.fr Received February 11, 2011; accepted April 5, 2011; previously published online June 11, 2011
2011/0080
Article in press - uncorrected proof
1266 Boulagnon et al.: Post-mortem vitreous humor glucose metabolism biochemistry
Figure 1 Schematization of post-mortem body changes wadapted from (14)x. Most post-mortem biochemical changes start during the early putrefactive phase. As a consequence, both PMI and body status are critical for the interpretation of biological analyses. These changes are influenced by environmental conditions, such as temperature variation and humidity.
collected from both eyes and analyzed separately (10). These between-eye differences have not been found with glucose (4).
Post-mortem changes
After death, major biochemical changes develop (4, 1114): Breakdown of cell membranes, Cessation of active transport and replacement by passive diffusion, Continuation of cell metabolism during agonal period and shortly after death, Anaerobic glycolysis in vitreous cells, ciliary and retinal epithelial cells. Moreover, bacterial metabolism, inducing glycolysis and proteolysis, occurs during the putrefaction phase. Body decomposition develops according to a sequence of events, whose duration depend on many factors, including environmental factors, such as temperature and humidity (Figure 1). A close collaboration between the pathologist and the biochemist is necessary in interpreting biochemical analyses. In particular, the estimation of the time since death is of paramount importance. Despite limitations, vitreous potassium concentration may be used for estimation of the postmortem interval (PMI) (11). As far as post-mortem changes involving glucose metabolism are concerned, an increase in the rate of glycolysis has been found in vitreous humor during the early post-mortem
period (4). The rate of glycolysis depends on environmental factors, such as temperature (1517) and initial glucose concentration (18), but is poorly correlated to PMI (4, 16, 18). With putrefaction, the catabolic activity of anaerobic bacteria generates high quantities of organic acids, such as lactate, acetoacetate and acetone (14). During the putrefactive phase, because of acidic conditions, acetoacetate is transformed into acetone (19). In almost all studies examining post-mortem glucose metabolism, vitreous humor was collected within 72 h after death, when early post-mortem changes predominated.
Preanalytical phase
The preanalytical phase is of paramount importance in interpreting biochemical analyses, both in clinical practice and thanatochemistry. First, aspiration of the vitreous humor through the outer can thus must be gentle and gradual to avoid contamination by retinal fragments or other tissues (1). Some authors have recommended aspiration of vitreous humor as completely as possible in order to avoid possible discrepancies between sites of higher or lower electrolyte/ glucose concentrations (1, 4). However, it was recently shown that glucose concentrations were similar in the different parts of the post-mortem vitreous body (4). The color and viscosity of the vitreous humor must be noted because this may indicate contamination, which would lead to misinterpretation of analytical results (4). The choice of the
Article in press - uncorrected proof
Boulagnon et al.: Post-mortem vitreous humor glucose metabolism biochemistry
1267
tubes used for collection of vitreous humor is another critical issue. Some authors have recommended tubes containing sodium fluoride (13, 20), whereas others have recommended plain tubes (21). As far as glucose and lactate are concerned, a recent study has shown that fluoride containing collection tubes do not affect results (4). The differences found by these authors were 0.17"0.19 mmol/L for glucose and 1.16"1.50 mmol/L for lactate (4). Effects of sample storage at ambient temperature are not known, but, as in clinical practice, transportation time between the autopsy room and the laboratory should be as short as possible. A study has shown that a 4-h duration between sample collection and analysis did not induce significant changes (4). Sample stability during refrigerated or frozen storage has been investigated in several studies. Peclet et al. have found that 12-day storage at 48C had no effect on vitreous glucose and lactate concentrations (20). Another study has shown a small but significant increase in electrolytes concentrations after 612-month refrigerated storage (5). Finally, the pathologist should provide the biochemist with clinical information, such as cause of death, agonal duration, medical drug therapy, environmental conditions and PMI (3). Vitreous humor is a highly viscous matrix, which requires a special preanalytical procedure (6, 21, 22). Various procedures have been proposed: centrifugation at various speeds, hyaluronidase digestion (22), heating (23), microfiltration (5), dilution (6, 21, 22) or ultrasonic bath (21). However, the usefulness of some of these procedures has been questioned, especially for investigations of glucose metabolism. Indeed, it has recently been shown that there was no difference in lactate and glucose concentrations between
supernatant or pellet (4). Moreover, results from heated samples did not differ from untreated samples (23). Nevertheless, lactate and glucose concentrations were higher in sonicated samples than in the supernatant of centrifuged samples (21).
Markers of glucose metabolism in post-mortem vitreous humor
Glucose
The diagnosis of fatal metabolic complications in diabetes mellitus is difficult because of the lack of autopsy and histological findings. Moreover, these complications can occur in persons with no known diabetes (16). Biochemistry is therefore the only method for diagnosis. Vitreous humor is the matrix of choice to avoid post-mortem blood glycolysis. In one study, ante-mortem serum glucose concentration were found correlated with post-mortem vitreous glucose concentrations (16). In another study involving living patients, vitreous glucose concentrations were found to be about half that of blood glucose concentration (8). Vitreous glucose concentrations tend to decrease in the early post-mortem period (4, 13), and then stabilize (4). Thus, low vitreous glucose concentration are not synonymous with hypoglycemia (13). High vitreous glucose concentrations may be found in three main circumstances (Figure 2): diabetic ketosis, hyperosmolar non-ketotic hyperglycemia and non-diabetic hyperglycemia. Ketoacidosis is the most frequent acute complication of diabetes, followed by hyperosmolar hyperglycemic non-ketotic coma (21).
Figure 2 Algorithm for the determination of the causes of a high glucose concentration in vitreous humor.
Article in press - uncorrected proof
1268 Boulagnon et al.: Post-mortem vitreous humor glucose metabolism biochemistry
Table 1 Different proposed thresholds for the diagnosis of severe or fatal hyperglycemia in vitreous humor. References Zilg et al., 2009 (4) Cases 3076 PMI before sampling -72 h (estimated from vitreous humor potassium concentration) Unknown -72 h -105 h Pre-analytical conditions Centrifugation 8000 g, 10 min or sonication 30 min. With or without NaF Diagnosis criterion Glucose )10 mmol/L
Chaturvedi et al., 2009 (24) Osuna et al., 2005 (16) Karlovsek, 2004 (17)
1335 453
Unknown Centrifugation 1500 g, 15 min Unknown
De Letter and Piette, 1998 (25) Coe, 1993 (1) Sippel and Mottonen, 1982 (26)
271 )6000 62
Unknown Unknown 112 days
Unknown Centrifugation Unknown
Glucose )7 mmol/L Glucose )11.1 mmol/L Glucose )13 mmol/L Sum value )23.7 mmol/L Sum value )23.7 mmol/L Glucose 11.1 mmol/L Sum value )22.7 mmol/L
Sum value is calculated as the sum of the concentration of glucose plus concentration of lactate divided by two. PMI, post-mortem interval.
Fatal high glucose concentrations in vitreous humor (Table 1) have been reported to range from 7.0 mmol/L to more than 13 mmol/L (1, 4, 16, 17, 2426). The authors have used vitreous and/or blood acetone and ketone body concentrations to differentiate deaths due to ketoacidosis from hyperosmolar non-ketotic deaths (16). During glycolysis, one glucose molecule is converted into two lactate molecules. For this reason, some authors have proposed calculating the sum of glucose plus lactate, divided by two for the diagnosis of hyperglycemia (21, 26). Post-mortem, high vitreous glucose concentrations can be found in the absence of diabetes. Various causes of nondiabetic hyperglycemia have been reported including asphyxia death, cerebral hemorrhage, congestive heart failure, electrocution, long agonal period, hypothermia death and cardiopulmonary resuscitation (1, 15, 16, 18). The latter cause has been controversial (16, 18). As far as death due to hypothermia is concerned, high glucose concentrations have been explained by inhibition of glycolysis due to cooling (13, 15) and hypothermia-induced stress (4). Moreover, alcoholic or ketoacidosis-induced hypothermia can be further aggravated by a cold environment leading to death. Fatal hypoglycemia is a difficult diagnosis because of post-mortem glycolysis. Karlovsek has proposed the following diagnostic criteria (17): Low glucose concentrations in the vitreous humor immediately after the death. Low glycated hemoglobin in treated diabetic patients, as a consequence of repeated hypoglycemic states. Low combined glucose and lactate values in vitreous humor (-8.9 mmol/L), even in case of poorly regulated diabetes (high HbA1c). Biochemical or toxicological findings indicating an overdose of antidiabetic drug.
Lactate
After death, vitreous humor lactate concentrations increase proportionately to PMI because of glycolysis (1, 4), and is further increased by a long agonal period (17). Consequently, lactic acidosis is a very difficult diagnosis in the absence of a suggestive context. Vitreous lactate concentrations are used mainly as an indicator of ante-mortem glycemia. A high potassium concentration, used as a PMI marker, in combination with a low lactate concentration are likely to indicate hypoglycemia (17). However, a high sum value of glucose concentrations plus lactate concentrations divided by two, is likely to indicate hyperglycemia (4, 20, 25, 26). However, the usefulness of this value has been discussed, because postmortem lactate production is not only due to glycolysis, but also to autolysis and bacterial catabolism in blood (14, 26, 27). Indeed, it has been shown that vitreous lactate increases are correlated to PMI, whereas a drop in vitreous glucose concentrations are not (4, 27).
Ketone bodies
Ketone bodies are produced in various pathological conditions, such as starvation, malnutrition, infection, diabetic or alcoholic ketoacidosis and hypothermia (19, 28). Among the three ketone bodies, beta-hydroxybutyrate seems to be the most specific post-mortem marker of ketoacidosis (4, 16, 19), and therefore has been well studied in vitreous humor (5, 16, 28). Acetone has been mostly studied in blood (4, 19, 28, 29). Acetoacetate is transformed into acetone due to postmortem acidic conditions (14, 19) and is often undetectable, whatever the matrix studied (5). For this reason, measurement of these two ketone bodies may only lead to misdiagnosis (5). Pre-analytical studies have shown no between-eye difference in concentrations of beta-hydroxybutyrate, and a
Article in press - uncorrected proof
Boulagnon et al.: Post-mortem vitreous humor glucose metabolism biochemistry
1269
Table 2 Vitreous fructosamine concentrations (mmol/L) in three comparative studies. References Diabetic patients n Vivero et al., 2008 (27) Osuna et al., 2005 (16) Osuna et al., 1999 (18) 96 111 49 Mean 0.8 0.88 1.5 SD 1.2 1.28 0.2 Median 0.3 0.3 1.5 Range 0.05.9 0.05.9 0.05.9 Non-diabetic patients n 281 342 43 Mean 0.2 0.16 0.5 SD 0.2 0.22 0.1 Median 0.1 0.13 0.7 Range 0.01.3 0.02.4 0.03.5
SD, standard deviation. Pre-analytical conditions: PMI -24 h, centrifugation 1500=g and supernatant storage at 808C. Analytical conditions: HITACHI 917 autoanalyzer with Roche Diagnosis kits (Hoffmann La Roche, Ldt., Basel, Switzerland), measurement range: 0.011 mmol/L.
tendency for concentrations to increase (0.6 mmol/L) during long refrigeration or frozen storage (5). Analytical studies have shown a good correlation between blood and vitreous humor total ketone body concentrations (29). Up to 72 h prior to the death, PMI does not influence vitreous betahydroxybutyrate concentration (16). High post-mortem betahydroxybutyrate blood concentrations have been found well correlated with medical histories of alcohol abuse, starvation or diabetic-induced ketoacidosis (19). In vitreous humor, high beta-hydroxybutyrate concentrations are correlated with high vitreous glucose concentrations (16), which suggest beta-hydroxybutyrate specificity. When a high acetone concentration is found in vitreous humor, glucose and ethanol assays should be performed to differentiate diabetic or alcoholic-related ketoacidosis from other causes.
Fructosamine
reous humor (16) (Figure 2). However, standardization of these assays in this unique fluid is required.
Conclusions
Thanatochemistry, especially in vitreous humor, is a useful tool for the diagnosis of metabolic death. Zilg et al. have shown that the frequency of diabetes mellitus-related deaths doubled, when they compared two study periods, one with systematic biochemical analyses (1.11%), vs. another without this approach (0.55%) (4). This study also demonstrates the usefulness of thanatochemistry for epidemiological purposes. A close collaboration between pathologists and biochemists is required to avoid misinterpretation of biochemical analyses. In particular, this review has shown the importance of medical history and PMI in interpreting biochemical analyses. As far as pre-analytical methods are concerned, harmonization of procedures should improve the reproducibility of results. Standardized analytical methods for vitreous humor assays should also be developed. For these purposes, further experimental and clinical studies are requires. This review focused on glucose metabolism-related deaths, but other metabolic or electrolytical disorders could be investigated using thanatochemistry.
In clinical practice, plasma fructosamine is measured to monitor glycemic status during 2 up to 3 weeks preceding the collection, generally as a surrogate for glycated hemoglobin (HbA1c), e.g., in case of hemoglobinopathy (16, 18, 27, 30). HbA1c cannot be measured in vitreous humor, because this matrix is not vascularized. In contrast, vitreous humor contains a sufficient concentration of proteins to measure their glycation rate under adapted analytical conditions. Protein concentrations in post-mortem vitreous humor have been reported to range from 0.3 to 5.3 g/L (18). In blood, fructosamine concentrations are well correlated with glycated hemoglobin (30), and remain stable after death because glycation is a cumulative process determined by the level of prevailing glucose concentrations during the lifespan of the protein (31). However, in post-mortem blood from healthy subjects, fructosamine deviation from the mean has been found to be larger than that of glycated hemoglobin (31). Only three studies have evaluated post-mortem vitreous fructosamine assay as an indicator of glycemic control during the weeks preceding death (16, 18, 27). The results are summarized in Table 2. In these studies, vitreous fructosamine has been found to be well correlated with ante-mortem serum glucose concentrations. Combined measurement of post-mortem vitreous glucose and fructosamine are likely to be the most sensitive tests for the diagnosis of pre-mortem diabetes (27). Thus, authors have proposed a protocol for the diagnosis of diabetes mellitus and its complications from post-mortem vit-
Highlights
Summarizing the literature reviewed above, it can be pointed out that: Vitreous humor is a good matrix for post-mortem biochemistry because it is better protected from post-mortem alterations and contamination than blood, and sampling is easy. The post-mortem interval and body status should be taken into account in interpreting post-mortem analyses. Vitreous fructosamine measured under standardized conditions may be a useful marker of ante-mortem glycemic state in combination with glycated hemoglobin dosage in blood. Severe hyperglycemic states can be diagnosed by vitreous glucose assay.
Article in press - uncorrected proof
1270 Boulagnon et al.: Post-mortem vitreous humor glucose metabolism biochemistry
Vitreous beta-hydroxybutyrate is an indicator of the severity of diabetic ketoacidosis. Hypoglycemic states must be interpreted carefully, taking into account the clinical context and other biological markers, such as a low lactate value and/or antidiabetic overdose. The sum value of glucose plus lactate divided by two can help in case of a low vitreous glucose value. Pre-analytical procedures are still to be standardized.
Conflict of interest statement
Authors conflict of interest disclosure: The authors stated that there are no conflicts of interest regarding the publication of this article. Research funding: None declared. Employment or leadership: None declared. Honorarium: None declared.
References
1. Coe JI. Post-mortem chemistry update. Emphasis on forensic application. Am J Forensic Med Pathol 1993;14:91117. 2. Basso C, Burke M, Fornes P, Gallagher PJ, de Gouveia RH, Sheppard M, et al. Guidelines for autopsy investigation of sudden cardiac death. Virchows Arch 2008;452:118. 3. Madea B, Musshoff F. Post-mortem biochemistry. Forensic Sci Int 2007;165:16571. 4. Zilg B, Alkass K, Berg S, Druid H. Post-mortem identification of hyperglycemia. Forensic Sci Int 2009;185:8995. 5. Gagajewski A, Murakami MM, Kloss J, Edstrom M, Hillyer M, Peterson GM, et al. Measurement of chemical analytes in vitreous humor: stability and precision studies. J Forensic Sci 2004;49:3714. 6. Stitt AW, Moore JE, Sharkey JA, Murphy G, Simpson DA, Bucala R, et al. Advanced glycation end products in vitreous: structural and functional implications for diabetic vitreopathy. Invest Ophtalmol Vis Sci 1998;39:251723. 7. Egger SF, Buxbaum A, Georgopoulos M, Scholda C, Vecsei VP, Huber-Spitzy V, et al. Bacterial growth in human vitreous humor. Exp Eye Res 1997;65:7915. 8. Lundquist O, Osterlin S. Glucose concentration in the vitreous of non-diabetic and diabetic human eyes. Graefes Arch Clin Exp Ophtalmol 1994;232:714. 9. Mulla A, Massey KL, Kalra J. Vitreous humor biochemical constituents: evaluation of between-eye differences. Am J Forensic Med Pathol 2005;26:1469. 10. Parson MA, Start RD, Forrest AR. Concurrent vitreous disease may produce abnormal vitreous humour biochemistry and toxicology. J Clin Pathol 2003;56:720. 11. Madea B. Is there recent progress in the estimation of the postmortem interval by means of thanatochemistry? Forensic Sci Int 2005;151:13949. 12. Saukko P, Knight B. The pathophysiology of death. In: Arnold E, editor. Knight forensic pathology, 3rd ed. Oxford University Press, 2004. pp. 5297.
13. Forrest AR. ACP Broadsheet no 137: April 1993. Obtaining samples at post mortem examination for toxicological and biochemical analyses. J Clin Pathol 1993;46:2926. 14. Beauthier JP. Quelques aspects biochimiques de levolution post mortem. In: De Boeck Universite, editor. Traite de mede cine legale. Bruxelles, 2008. pp. 71525. 15. Coe JI. Hypothermia: autopsy findings and vitreous glucose. J Forensic Sci 1984;29:38995. 16. Osuna E, Vivero G, Conejero J, Abenza JM, Martinez P, Luna A, et al. Post-mortem vitreous humor beta-hydroxybutyrate: its utility for the post-mortem interpretation of diabetes mellitus. Forensic Sci Int 2005;153:18995. 17. Karlovsek MZ. Diagnostic values of combined glucose and lactate values in cerebrospinal fluid and vitreous humour: our experiences. Forensic Sci Int 2004;146(Suppl):S1923. 18. Osuna E, Garca-Vllora A, Perez-Carceles MD, Conejero J, Abenza JM, Martnez P, et al. Vitreous humor fructosamine concentrations in the autopsy diagnosis of diabetes mellitus. Int J Legal Med 1999;112:2759. 19. Kanetake J, Kanawaku Y, Mimasaka S, Sakai J, Hashiyada M, Nata M, et al. The relationship of a high level of serum betahydroxybutyrate to cause of death. Leg Med 2005;7:16974. 20. Peclet C, Picotte P, Jobin F. The use of vitreous humor levels of glucose, lactic acid and blood levels of acetone to establish ante-mortem hyperglycemia in diabetics. Forensic Sci Int 1994;65:16. 21. Thierauf A, Musshoff F, Madea B. Post-mortem biochemical investigations of vitreous humor. Forensic Sci Int 2009;192: 7882. 22. Garg U, Althahabi R, Amirahmadi V, Brod M, Blanchard C, Young T. Hyaluronidase as a liquefying agent for chemical analysis of vitreous fluid. J Forensic Sci 2004;49:38891. 23. McNeil AR, Gardner A, Stables S. Simple method for improving the precision of electrolyte measurements in vitreous humor. Clin Chem 1999;45:1356. 24. Chaturvedi AK, Botch SR, Canfield DV, Forster EM. Vitreous fluid and/or urine glucose concentrations in 1335 civil aviation accident pilot fatalities. J Forensic Sci 2009;54:71520. 25. De Letter EA, Piette MH. Can routinely analysis of glucose and lactate in vitreous humour be useful in current forensic practice? Am J Forensic Med Pathol 1998;19:33542. 26. Sippel H, Mottonen M. Combined glucose and lactate value in vitreous humour for post-mortem diagnosis of diabetes mellitus. Forensic Sci Int 1982;19:21722. 27. Vivero G, Vivero-Salmeron G, Perez Carceles MD, Bedate A, Luna A, Osuna E. Combined determination of glucose and fructosamine in vitreous humor as a post-mortem tool to identify ante-mortem hyperglycemia. Rev Diabet Stud 2008;5:2204. 28. Teresinski G, Buszewicz G, Madro R. Acetonaemia as an initial criterion of evaluation of a probable cause of sudden death. Leg Med 2009;11:1824. 29. Pounder DJ, Stevenson RJ, Taylor KK. Alcoholic ketoacidosis at autopsy. J Forensic Sci 1998;43:8126. 30. Leutenegger M, Gillery P, Gross A, Pasqual C, Ostermann G, Durlach V. Assay of fructosamine. Value and limits in diabetology. Ann Biol Clin 1989;47:1215. 31. Uemura K, Shintani-Ishida K, Saka K, Nakajima M, Ikegaya H, Kikuchi Y, et al. Biochemical blood markers and sampling sites in forensic autopsy. J Forensic Leg Med 2008;15:3127.
Copyright of Clinical Chemistry & Laboratory Medicine is the property of De Gruyter and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
You might also like
- Level 7 User ManualDocument8 pagesLevel 7 User Manualblazaaaaaaaa100% (1)
- Paediatric Septic Shock Management GuideDocument37 pagesPaediatric Septic Shock Management GuideJavedgouri GouriNo ratings yet
- Non Surgical Management of Periapical Lesions Using Calcium HydroxideDocument6 pagesNon Surgical Management of Periapical Lesions Using Calcium HydroxideVinisha Vipin SharmaNo ratings yet
- Sleep Apnoea - Prof - DR K.K.PDocument44 pagesSleep Apnoea - Prof - DR K.K.PjialeongNo ratings yet
- Aim4aiims - In: Pathology Board ExaminationDocument72 pagesAim4aiims - In: Pathology Board ExaminationdorjeesengeNo ratings yet
- Gastrointestinal Diseases and Disorders Sourcebook, Fifth EditionFrom EverandGastrointestinal Diseases and Disorders Sourcebook, Fifth EditionNo ratings yet
- Diabetes OPD ดีมากกกDocument5 pagesDiabetes OPD ดีมากกกPonpimol Odee BongkeawNo ratings yet
- Biomechanics of The KneeDocument8 pagesBiomechanics of The KneeJorge LopezNo ratings yet
- Metabolic Syndrome Is Related Cardio-Cerebro Vascular DiseaseDocument40 pagesMetabolic Syndrome Is Related Cardio-Cerebro Vascular DiseaseSatya FitriansyahNo ratings yet
- PATHOPHYSIOLOGY OF SHOCKDocument56 pagesPATHOPHYSIOLOGY OF SHOCKDr. Haricharan ANo ratings yet
- Tirzepatide Significantly Reduced A1C and Body Weight in People With Type 2 Diabetes in Two Phase 3 Trials From Lilly's SURPASS ProgramDocument4 pagesTirzepatide Significantly Reduced A1C and Body Weight in People With Type 2 Diabetes in Two Phase 3 Trials From Lilly's SURPASS ProgramJOSÉ CARLOS ÁLVAREZ PAYARESNo ratings yet
- Infectious Diseases - Infective EndocarditisDocument41 pagesInfectious Diseases - Infective Endocarditisfire_n_iceNo ratings yet
- The Complications of DiabetesDocument1 pageThe Complications of DiabetesMiguel Cuevas DolotNo ratings yet
- Abdominal Aortic Aneurysms-EditDocument32 pagesAbdominal Aortic Aneurysms-EditrandikaNo ratings yet
- The Concept of Professional Ethics and BioethicsDocument20 pagesThe Concept of Professional Ethics and BioethicsMelchor Felipe Salvosa100% (1)
- Where To Get Help For Selective MutismDocument2 pagesWhere To Get Help For Selective MutismTee Kok KeongNo ratings yet
- Metabolism and NutritionDocument52 pagesMetabolism and NutritionAlex SaljayNo ratings yet
- Perioperative Management in Diabetes MellitusDocument20 pagesPerioperative Management in Diabetes MellitusChristopher RyalinoNo ratings yet
- The Hepatorenal SyndromeDocument26 pagesThe Hepatorenal SyndromeWaraBawanaNo ratings yet
- Management of Diabetes Mellitus in Surgical PatientsDocument12 pagesManagement of Diabetes Mellitus in Surgical PatientsAnggoro Bayu Agung DjangkaruNo ratings yet
- 2004-Case Study Diabetes in A Patient With Cirrhosis PDFDocument5 pages2004-Case Study Diabetes in A Patient With Cirrhosis PDFAnugrah ElfaNo ratings yet
- Manajemen Pre-Operatif Pasien Dengan DMDocument12 pagesManajemen Pre-Operatif Pasien Dengan DMyanayas28No ratings yet
- Endocrine Pancreas & Fuel Homeostasis: Learning ObjectivesDocument7 pagesEndocrine Pancreas & Fuel Homeostasis: Learning ObjectivesMaggieLockeNo ratings yet
- Diabetic KetoacidosisDocument22 pagesDiabetic KetoacidosispoktaviantiNo ratings yet
- Endocrine EmergencyDocument21 pagesEndocrine EmergencyThorsang ChayovanNo ratings yet
- Chronic Kidney Disease Stages, Risk Factors, and TreatmentDocument45 pagesChronic Kidney Disease Stages, Risk Factors, and Treatmentnaro ayosNo ratings yet
- PfutznerDocument41 pagesPfutznermina100% (1)
- Acute Kidney Injury Diagnosis and Management ApproachDocument45 pagesAcute Kidney Injury Diagnosis and Management ApproachAndika Yusuf RamadhanNo ratings yet
- Diabetic Ketoacidosis:: Evidence Based ReviewDocument4 pagesDiabetic Ketoacidosis:: Evidence Based ReviewgracedumaNo ratings yet
- DkaDocument38 pagesDkaHam SotheaNo ratings yet
- Diabetic Ketoacidosis in PaediatricDocument11 pagesDiabetic Ketoacidosis in PaediatricSana Anam JahanNo ratings yet
- HyperglycemiaDocument1 pageHyperglycemiaanon_262360776No ratings yet
- DKA management guidelinesDocument27 pagesDKA management guidelinesjun sianNo ratings yet
- Dr. Erlieza Roosdhania, SP - PD (CKD)Document38 pagesDr. Erlieza Roosdhania, SP - PD (CKD)Pon PondNo ratings yet
- Diabetic Neuropathy PPT FinalDocument54 pagesDiabetic Neuropathy PPT FinalJenny Juniora AjocNo ratings yet
- Cardiohepatic FinalDocument28 pagesCardiohepatic FinalAsep HrNo ratings yet
- Clinical Approach in NeuropathyDocument43 pagesClinical Approach in NeuropathyHayaNo ratings yet
- 3a Emergency Care DKA (UK) FINALDocument40 pages3a Emergency Care DKA (UK) FINALDrsarfaraz SiddiquiNo ratings yet
- Aravind 2012 Curr Med Res OpinDocument8 pagesAravind 2012 Curr Med Res OpinSastra WijayaNo ratings yet
- Gelofusine: Iso-Oncotic Gelatine Solution For Intravenous Volume Substitution. Modified GelatineDocument6 pagesGelofusine: Iso-Oncotic Gelatine Solution For Intravenous Volume Substitution. Modified GelatineAshish KhomaneNo ratings yet
- FLUID INTAKE AND HYDRATIONDocument17 pagesFLUID INTAKE AND HYDRATIONVhiny ChaNo ratings yet
- In Lieu of An IntroductionDocument11 pagesIn Lieu of An IntroductionJayanta BhattacharyaNo ratings yet
- Preoperative Assessment ChecklistDocument27 pagesPreoperative Assessment ChecklistHairina MazlanNo ratings yet
- Indications For Initiation of Dialysis in Chronic Kidney DiseaseDocument11 pagesIndications For Initiation of Dialysis in Chronic Kidney DiseaseLiliana WoodNo ratings yet
- Acute Treatment of Hypocalcaemia (Adults)Document2 pagesAcute Treatment of Hypocalcaemia (Adults)Ahed WarwarNo ratings yet
- Manajemen Anestesi Pada Uremic SyndromeDocument27 pagesManajemen Anestesi Pada Uremic SyndromeAdi Nugroho MelyanaNo ratings yet
- First AssessmentDocument3 pagesFirst AssessmentBianglala OkeNo ratings yet
- Treatment of Diabetic Nephropathy - UpToDateDocument43 pagesTreatment of Diabetic Nephropathy - UpToDateSihuar Fernando Abarca LozanoNo ratings yet
- Fellowship in DiabetesDocument2 pagesFellowship in DiabetesBenjamin NelsonNo ratings yet
- Hypertension Diagnosis and ManagementDocument54 pagesHypertension Diagnosis and ManagementdrsalilsidhqueNo ratings yet
- Diabetic Ketoacidosis (D.K.A) Beaumont Hospital Protocol: DiagnosisDocument1 pageDiabetic Ketoacidosis (D.K.A) Beaumont Hospital Protocol: Diagnosislouglee9174100% (1)
- Gap Co2 Cocc 2018Document9 pagesGap Co2 Cocc 2018Cesar Rivas CamposNo ratings yet
- Hyporeninemic HypoaldosteronismDocument12 pagesHyporeninemic HypoaldosteronismCésar Augusto Sánchez SolisNo ratings yet
- Fluid ResuscitationDocument3 pagesFluid ResuscitationAdam FnsNo ratings yet
- Contrast RXDocument4 pagesContrast RXAndrew EricksonNo ratings yet
- Analisis Faktor Resiko KatarakDocument12 pagesAnalisis Faktor Resiko KatarakindrawatiNo ratings yet
- Measuring renal function clinicallyDocument5 pagesMeasuring renal function clinicallyVijeyachandhar DorairajNo ratings yet
- Acute Kidney Injury (AKI)Document68 pagesAcute Kidney Injury (AKI)Alex beharuNo ratings yet
- WHS PR Symposium - Non-Alcoholic Fatty Liver DiseaseDocument63 pagesWHS PR Symposium - Non-Alcoholic Fatty Liver DiseaseWomen's Health SocietyNo ratings yet
- Diabetic Ketoacidosis in Pregnancy: Diagnosis of DKADocument7 pagesDiabetic Ketoacidosis in Pregnancy: Diagnosis of DKA123someone123No ratings yet
- Komplikasi Stroke PDFDocument7 pagesKomplikasi Stroke PDFJose Hady PuteraNo ratings yet
- Sepsis Power Point Slide Presentation - The Guidelines - Implementation For The FutureDocument25 pagesSepsis Power Point Slide Presentation - The Guidelines - Implementation For The Futuremontie13No ratings yet
- Evaluation of Liver FunctionDocument64 pagesEvaluation of Liver FunctionMustafa KhandgawiNo ratings yet
- Ketone Bodies 2012Document15 pagesKetone Bodies 2012Adhya MurugesanNo ratings yet
- Evaluation and Management of Elevated Intracranial Pressure in AdultsDocument28 pagesEvaluation and Management of Elevated Intracranial Pressure in AdultssandykumalaNo ratings yet
- MCMAPDocument110 pagesMCMAPAIWER103No ratings yet
- Supplemental Initial Brief of AppellantDocument7 pagesSupplemental Initial Brief of AppellantsbeyeforhireNo ratings yet
- Initial Brief of AppellantDocument106 pagesInitial Brief of AppellantsbeyeforhireNo ratings yet
- Nps D9 DDDocument297 pagesNps D9 DDsbeyeforhireNo ratings yet
- Salazar v. Buono, No. 08-472Document71 pagesSalazar v. Buono, No. 08-472SCOTUSblog2No ratings yet
- IVMS ICM-Heart MurmursDocument22 pagesIVMS ICM-Heart MurmursMarc Imhotep Cray, M.D.No ratings yet
- A Soft-Tissue Cephalometric Analysis and Its Use in Orthodontic Treatment Planning. Part IDocument28 pagesA Soft-Tissue Cephalometric Analysis and Its Use in Orthodontic Treatment Planning. Part IJorge Ramírez100% (1)
- HEYER VizOR 6 - Manual 1.0 EN PDFDocument128 pagesHEYER VizOR 6 - Manual 1.0 EN PDFkalandorka92No ratings yet
- Mnemonic Devices for Medical EducationDocument9 pagesMnemonic Devices for Medical EducationJhey MalanyaonNo ratings yet
- DP 50 BrochureDocument4 pagesDP 50 Brochurerca ieftinNo ratings yet
- Fdar Psychiatric DutyDocument2 pagesFdar Psychiatric DutyErica Maceo MartinezNo ratings yet
- Minimal Invasive Techniques in Porcelain Laminate Veneers: Case SeriesDocument4 pagesMinimal Invasive Techniques in Porcelain Laminate Veneers: Case Seriesfanny rizky andriyaniNo ratings yet
- Dental and Craniomaxillofacial Implant SurgeryDocument35 pagesDental and Craniomaxillofacial Implant SurgeryJean Carlos Barbosa FerreiraNo ratings yet
- English Meeting 2Document10 pagesEnglish Meeting 2Tya DwiNo ratings yet
- Disc Bulge Recovery LikelyDocument4 pagesDisc Bulge Recovery LikelyItai IzhakNo ratings yet
- Ayurvedic Management of Multiple SclerosisDocument4 pagesAyurvedic Management of Multiple SclerosisLife LineNo ratings yet
- Drug StudyDocument9 pagesDrug StudyStephanie ValerioNo ratings yet
- Abstract Construction of New Building For District HospitalDocument1 pageAbstract Construction of New Building For District HospitaldipinnediyaparambathNo ratings yet
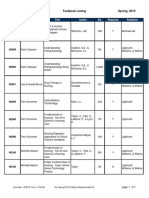
- BFLSON Course Textbook ListingDocument7 pagesBFLSON Course Textbook ListingWina ViqaNo ratings yet
- Aims and ObjectivesDocument13 pagesAims and Objectivesmamun183No ratings yet
- Principles of Pharmacokinetics and PharmacodynamicsDocument136 pagesPrinciples of Pharmacokinetics and PharmacodynamicsDidiNo ratings yet
- Leadership Shadowing ExperienceDocument2 pagesLeadership Shadowing Experienceapi-437270264No ratings yet
- Potassium Chloride (Ktab)Document2 pagesPotassium Chloride (Ktab)Marlisha D. BrinkleyNo ratings yet
- Jcthe Role of Abutment-Attachment Selection in Resolving Inadequate Interarch Distance: A Clinical ReportdDocument7 pagesJcthe Role of Abutment-Attachment Selection in Resolving Inadequate Interarch Distance: A Clinical ReportdSyed Noorani100% (1)
- Chap 05 Abdominal TraumaDocument24 pagesChap 05 Abdominal TraumaAndra SNo ratings yet
- The Effectiveness of Pre-Operative Deep BreathingDocument5 pagesThe Effectiveness of Pre-Operative Deep BreathingJulenda CintarinovaNo ratings yet
- Dorothy M. Adcock, MDDocument4 pagesDorothy M. Adcock, MDพอ วิดNo ratings yet
- KDIGO AKI Guideline DownloadDocument141 pagesKDIGO AKI Guideline DownloadSandi AuliaNo ratings yet