Professional Documents
Culture Documents
Case Report Non-infection Unit Β-Major Thalassemia
Uploaded by
imamkdOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case Report Non-infection Unit Β-Major Thalassemia
Uploaded by
imamkdCopyright:
Available Formats
1
Case Report Non-infection Unit -MAJOR THALASSEMIA Presenter Day/Date Supervisor : : : Imam Kukuh Darmawan Taufik Delfian Monday, July, 4th 2011 dr. Hj. Melda Deliana, Sp. A (K)
CHAPTER I 1.1 INTRODUCTION The thalassemias are inherited disorders of hemoglobin (Hb) synthesis. Their clinical severity widely varies, ranging from asymptomatic forms to severe or even fatal entities. The name Mediterranean anemia, which Whipple introduced, is misleading because the condition can be found in any part of the world. As described below, different types of thalassemia are more endemic to certain geographic regions. In 1925, Thomas Cooley, a Detroit pediatrician, described a severe type of anemia in children of Italian origin. He noted abundant nucleated red blood cells (RBCs) in the peripheral blood, which he initially thought was erythroblastic anemia, an entity that von Jaksh described earlier. Before long, Cooley realized that erythroblastemia is neither specific nor essential in this disorder and that the term erythroblastic anemia was nothing but a diagnostic catchall. Although Cooley was aware of the genetic nature of the disorder, he failed to investigate the apparently healthy parents of the affected children. 1 In Europe, Riette described Italian children with unexplained mild hypochromic and microcytic anemia in the same year Cooley reported the severe form of anemia
later named after him. In addition, Wintrobe and coworkers in the United States reported a mild anemia in both parents of a child with Cooley anemia. This anemia was similar to the one that Riette described in Italy. Only then was Cooley's severe anemia recognized as the homozygous form of the mild hypochromic and microcytic anemia that Riette and Wintrobe described. This severe form was then labeled as thalassemia major and the mild form as thalassemia minor. The word thalassemia is a Greek term derived from thalassa, which means "the sea" (referring to the Mediterranean), and emia, which means "related to blood." 1 1.2 EPIDEMIOLOGY Worldwide, 15 million people have clinically apparent thalassemic disorders. Reportedly, disorders worldwide, and people who carry thalassemia in India alone number approximately 30 million. These facts confirm that thalassemias are among the most common genetic disorders in humans; they are encountered among all ethnic groups and in almost every country around the world. 1 Certain types of thalassemia are more common in specific parts of the world. thalassemia is much more common in Mediterranean countries such as Greece, Italy, and Spain. Many Mediterranean islands, including Cyprus, Sardinia, and Malta, have a significantly high incidence of severe thalassemia, constituting a major public health problem. For instance, in Cyprus, 1 in 7 individuals carries the gene, which translates into 1 in 49 marriages between carriers and 1 in 158 newborns expected to have thalassemia major. As a result, preventive measures established and enforced by public health authorities have been very effective in decreasing the incidence among their populations. thalassemia is also common in North Africa, the Middle East, India, and Eastern Europe. Conversely, thalassemia is more common in Southeast Asia, India, the Middle East, and Africa. 1
1.3
CAUSES Thalassemias are inherited disorders caused by various gene mutations. The
clinical expression and severity are subject to numerous factors that may either mask the condition or exaggerate the symptoms, leading to a more severe disease. Many additional factors influence the clinical manifestations of disease. That is, the same mutations may have different clinical manifestations in different patients. The following factors are known to influence the clinical phenotype: Intracellular fetal Hb concentrations The level of expression of fetal Hb (ie, the expression level of the gamma-globin gene) determines, in part, the severity of the disease. Patients with high fetal Hb have milder disease. Co-inheritance of alpha thalassemia Patients with co-inheritance of alpha thalassemia have a milder clinical course because they have a less severe alpha-beta chain imbalance. The coexistence of sickle cell trait and beta thalassemia is a major and symptomatic hemoglobinopathy with most of the symptoms and complications of sickle cell disease. Unlike sickle cell trait, in which most Hb-on-Hb electrophoresis is Hb A (AS), S is the dominant Hb (SA) and usually constitutes about 60% of the circulating Hb. 2 1.4 PATHOPHYSIOLOGY The thalassemias are inherited disorders of Hb synthesis that result from an alteration in the rate of globin chain production. A decrease in the rate of production of a certain globin chain or chains (, , , ) impedes Hb synthesis and creates an imbalance with the other, normally produced globin chains. 1,2
In general, the globin chains are synthesized in erythrocytes of thalassemia is structurally normal. In form of thalassemia, a severe form of abnormal haemoglobin hemotetramer (4 or 4) but globin polypeptide component has a normal structure. Conversely, some abnormal haemoglobin also causes the changes of similar hematologi thalassemia. Thalassemia gene is very widely spread, and this abnormality is believed to be the most prevalent of humans genetic diseases. The main distribution areas include the Mediterranean Sea border, most of Africa, the Middle East, Indian subcontinent, and Southeast Asia. Form 3% to 8% of Americans are descendants of Italian or Greek and 0.5% of black Americans carry the gene for -thalassemia. In some areas of Southeast Asia, 40% of the population has one or more genes of thalassemia
1,2
Mutations in -thalassemia involve globin gene deletions, promoter region mutations, termination mutations, splice site mutations, and other rare mutations. The key feature is the fact that there is a globin chain imbalance. In the bone marrow the thalassemic mutations disrupt the maturation of the red cell, resulting in ineffective erythropoiesis; the marrow is hyperactive, but there are relatively few reticulocytes and
severe anemia. In -thalassemias there is an excess of -globin chains relative to - and -globin chains; -globin tetramers (4) are formed, and these inclusions interact with the red cell membrane and shorten red cell survival, leading to anemia and increased erythroid production. The -globin chains are produced in normal amounts, leading to an elevated Hb F (22). The -globin chains are also produced in normal amounts, leading to an elevated Hb A2 (22) in -thalassemia. 1,2 1.5 CLASSIFICATION A large number of thalassemic syndromes are currently known; each involves decreased production of one globin chain or more, which form the different Hbs normally found in RBCs. The most important types in clinical practice are those that affect either or chain synthesis. 1 Alpha () thalassemias The thalassemias involve the genes HBA1 and HBA2, inherited in a Mendelian recessive fashion. There are two gene loci and so four alleles. It is also connected to the deletion of the 16p chromosome. thalassemias result in decreased alpha-globin production, therefore fewer alpha-globin chains are produced, resulting in an excess of chains in adults and excess chains in newborns. The excess chains form unstable tetramers (called Hemoglobin H or HbH of 4 beta chains) which have abnormal oxygen dissociation curves. 1
Beta () thalassemias Beta thalassemias are due to mutations in the HBB gene on chromosome 11 also inherited in an autosomal-recessive fashion. The severity of the disease depends on the nature of the mutation. Mutations are characterized as either o or thalassemia major if they prevent any formation of chains, the most severe form of thalassemia. Alternatively they are characterized as + or thalassemia intermedia if they allow some chain formation to occur. In either case there is a relative excess of chains,
but these do not form tetramers: rather, they bind to the red blood cell membranes, producing membrane damage, and at high concentrations they form toxic aggregates. 1 In the thalassemias, production of the globin portion of the hemoglobin molecule is defective. Cooley's anemia (b-thalassemia major) presents with severe pallor usually between 6 and 12 months of age, as the fetal hemoglobin (HbF) level declines but the normal rise in adult hemoglobin (HbA) production fails to occur because of reduced or absent b-globin production. Children with thalassemia have a shorter red cell life, fetal hemoglobin in their red cells until an older age than normal, and red cells that are more sensitive to oxidative stress1 Delta () thalassemia As well as alpha and beta chains being present in hemoglobin about 3% of adult hemoglobin is made of alpha and delta chains. Just as with beta thalassemia, mutations can occur which affect the ability of this gene to produce delta chains.
1.6
CLINICAL MANIFESTATION These children usually become symptomatic from progressive hemolytic
anemia with profound weakness and cardiac decompensation during the second 6 months of life if not treated.1 As indicated in the genotype of affected patients can be b+ /b+ , b0 /b0 , or b0 /b+ . With all these genotypes, the anemia manifests 6 to 9 months after birth, as hemoglobin synthesis switches from HbF to HbA.2 Most infants and children have cardiac decompensation at hemoglobins of 4g/dL or less. Generally, fatigue, poor appetite, and lethargy are late findings of severe anemia in an infant or child.1 Children with thalassemia major usually develop a sallow complexion and increasing fatigue between the ages of 6 and 24 months.3 The classic presentation of children with severe thalassemic facies, pathologic fractures, marked hepatosplenomegaly, and cachexia is still seen in some developing countries. The spleen may become so enlarged that it causes mechanical discomfort and secondary
hypersplenism. These are features of ineffective erythropoiesis with compensatory bone marrow hyperplasia producing a characteristic overgrowth of the facial and skull bones, extramedullary hematopoiesis, and a huge caloric need.1
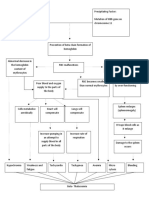
Picture 1. Clinical manifestation of Beta-major Thalassemia
The hepatosplenomegaly may interfere with nutritional support. Pallor, hemosiderosis, and jaundice may combine to produce a greenish brown complexion. Because of the anemia there is also an increase in iron absorption, with toxicity leading to further complications, if the child survives long enough to develop them. Many of these features became less severe and infrequent with transfusion therapy, but transfusional hemosiderosis is a consequent complication.1 1.7 LABORATORY FINDINGS The infant is born only with Hb F or, in some cases, Hb F and Hb E (heterozygosity for 0-thalassemia). Eventually in 0-thalassemia there is severe anemia, few reticulocytes, numerous nucleated red cells, and microcytosis with almost no normal-appearing red cells on the smear. The red cells are hypochromic and microcytic with striking variation in size and shape; nucleated red cells are present in the peripheral smear.3 The hemoglobin level falls progressively to lower than 5gr/dL unless transfusions are given. The unconjugated serum bilirubin level is usually elevated, but other chemistries may be normal at an early stage. Even if untransfused,
10
eventually there is iron accumulation with an elevated serum ferritin and saturation of the transferrin. Bone marrow hyperplasia can be seen on radiographs.1 Thalassemia major is readily distinguishable from severe nutritional iron deficiency. In the latter disorder, the dietary history is grossly abnormal, organomegaly is uncommon, changes in red cell morphology are less impressive, and nucleated red cells are rarely seen in the peripheral smear. The diagnosis of thalassemia major should be considered in a child with severe microcytic anemia and an appropriate ethnic background. Although severe anemia is extremely rare in heterozygous thalassemia disorders, thalassemia trait and concomitant iron deficiency may be particularly difficult to distinguish from a homozygous thalassemia disorder. In untransfused patients, hemoglobin levels range between 3 and 6 gm/dL. The peripheral blood smear shows severe red cell morphologic abnormalities, including marked anisocytosis and poikilocytosis (variation in size and shape, respectively), microcytosis (small size), and hypochromia (poor hemoglobinization).2
Picture 2. Laboratory findings of thalassemia : Morphologic of the cell
The major morphologic alterations, in addition to those found in all hemolytic anemias, involve the bone marrow and spleen. In the untransfused patient, there is striking expansion of hematopoietically active marrow, particularly in facial bones. This erodes existing cortical bone and induces new bone formation, giving rise to a
11
"crew-cut" appearance on X-rays. Both mononuclear phagocytic cell hyperplasia and extramedullary hematopoiesis contribute to enlargement of the spleen, which can weigh up to 1500 gm.2 1.8 IMAGING STUDIES In severely affected patients, a widening of the diploic space (medulla) with a thinning of the tables (cortices) occurs, frequently with complete obliteration of the outer table. New bone forms in response to marrow proliferation beneath the periosteum. These bony spicules may be seen radiographically and result in a classic "hair-on-end" appearance. Because it lacks hematopoietic marrow, the occipital bone usually is not involved. (See the image below.) 3
Picture 2. Bone Changes hair-on-end appearance of Beta-major Thalassemia (Facies Cooley)
Proliferation of marrow within the frontal and facial bones impedes pneumatization of the paranasal sinuses. This results in hypertrophy of osseous structures and a consequent prominence of the lateral margins of the malar eminences, together with anterior and medial displacement of developing teeth. These features
12
explain the clinical findings noted by Cooley. Characteristically, ethmoidal sinuses are not involved, a factor attributable to the absence of red marrow in the sinus walls.3 1.9 DIFFERENTIAL DIAGNOSIS -Thalassemia major is rarely confused with other disorders. Hemoglobin electrophoresis and family studies readily distinguish it from hemoglobin Ethalassemia, which is the other important cause of transfusion-dependent thalassemia.
1.10
TREATMENT
Transfusion Before initiating chronic transfusions, the diagnosis of 0-thalassemia should be confirmed and the parents counseled concerning this life-long therapy. Beginning transfusion and chelation therapy are difficult challenges for parents to face early in their child's life. Before beginning transfusion therapy, a red cell phenotype is obtained; blood products that are leukoreduced and phenotypically matched for the Rh and Kell antigens are required for transfusion. If there is the possibility of a bone marrow transplant, the blood should be negative for cytomegalovirus and irradiated. Transfusion therapy promotes general health and well-being and avoids the consequences of ineffective erythropoiesis. Iron overload is inevitable, and hypertransfusion should be avoided. A post-transfusion hemoglobin level of 9.5g/dL is the goal. Banked blood in developed countries is generally safe. Designated donors are not encouraged; some blood centers have partner programs, pairing donors and recipients, which decreases the exposure to multiple red cell antigens. As a child grows, more donors will be needed. 1.2
13
Severe forms of thalassemia are fatal if untreated. Chronic RBC transfusions are necessary for survival. However, iron overload eventually ensues, causing damage to liver, endocrine glands, and heart. Without chelation therapy, iron toxicity leads to death in the second or third decade of life. Depending on the mutation and degree of fetal hemoglobin production, transfusions in thalassemia major are necessary in the second month of life or the second year of life but rarely later. The decision to transfuse depends on the child's ability to compensate for the degree of anemia. Packed, leukodepleted RBC transfusions (10-20 ml/kg) should be given every 3 to 5 weeks to maintain hematocrit (Hct) at greater than 30% and to suppress reticulocytosis. This regimen allows normal growth. 7,8 Chelating Agents Transfusional hemosiderosis causes many of the complications of thalassemia major. Assessment of iron overloading is best achieved by liver biopsy, supplemented by ferritometry and the measurement of serum ferritin. Liver biopsy is the only method that is reproducible and should be available in centers caring for thalassemic patients. There are few available ferritometers. Ferritin can only provide an assessment of the trend of the iron status for a particular patient. 7,8 Transfusional hemosiderosis can be prevented by the use of deferoxamine (Desferal). Deferoxamine chelates iron and some other divalent cations, allowing their excretion in the urine and the stool. If used appropriately, a negative iron balance can be achieved. Deferoxamine (DF) chelation should be instituted when transferrin becomes fully saturated and a chelatable iron pool is demonstrated by DF challenge. This generally corresponds to a cumulative burden greater than 500 ml/kg of RBCs. Deferoxamine is given subcutaneously over 1012hr, 56 days a week and is given daily (30-50 mg/kg/day) over 10 to 12 hours by subcutaneous infusion pump. This therapy reduces iron-induced organ damage and prolongs survival if compliance is good.5 It should be used cautiously in young children. The side effects include
14
ototoxicity with high-frequency hearing loss, retinal changes, and bone dysplasia with truncal shortening. Oral iron chelators (deferiprone: L-1) have not been as effective as deferoxamine and there is a concern about causing neutropenia, arthritis, and hepatic fibrosis. Other iron chelators are being studied for oral and subcutaneous use. 7,8 Surgery Splenectomy may be indicated for patients with thalassemia intermedia who have a falling steady-state hemoglobin and for transfused patients with a rising transfusion requirement. However, splenectomy may have serious infectious consequences. Because of the increased risk of infection after splenectomy, all patients should be fully immunized against encapsulated bacteria before splenectomy, and they subsequently should be on long-term penicillin prophylaxis. Preliminary evidence that splenectomy may lead to pulmonary hypertension has led to anticoagulation being considered for some splenectomized patients. Bone marrow transplantation has successfully cured over a thousand patients who have thalassemia major. Most success has been in children younger than 15 year of age without iron overload and hepatomegaly who have HLA-matched siblings. All children who have an HLA-matched sibling should be offered the option of bone marrow transplantation. Early death from toxicity and graft-versus-host disease is low (<10%) in young patients without hepatic dysfunction. The risk of death is considerably higher for older patients, especially if liver function is already compromised by hemosiderosis. If an HLA-matched, healthy sibling is available, bone marrow transplantation should be considered, especially in a patient without symptoms of hemosiderosis. Introduction of abnormal beta-globin gene using gene therapy remains an area of active research.6 Other Medication
15
The moderate anemia usually apparent at presentation allows sufficient time for a careful diagnostic evaluation and outpatient transfusion therapy. However, when anemia is severe and congestive heart failure is present or imminent, the need for red cell transfusion may be urgent. In such instances, pretransfusion blood should be saved for appropriate diagnostic studies (hemoglobin electrophoresis) and initial red cell antigen typing. If transfusion is necessary, small aliquots of red cells (2 to 3 mL/kg) should be given. The administration of a rapid-acting diuretic (furosemide 1 mg/kg per dose) may diminish the risk of fluid overload. Partial exchange transfusion has also been recommended for patients with severe anemia to prevent further increases in intravascular volume and myocardial stress. Because patients with thalassemia major and severe anemia invariably have a lifelong dependence on red cell transfusions, the use of noncross-matched blood should be scrupulously avoided at the time of presentation to prevent sensitization to foreign red cell antigens.7 Folic acid (1 mg/day) should be prescribed to those in whom erythropoiesis is not suppressed by chronic transfusion, to prevent folate deficiency and megaloblastic crisis.5 1.11 COMPLICATIONS
Complications develop as a result of: 1. Chronic anemia in patients who are undertransfused or in untransfused thalassemia intermedia patients 2. Chronic transfusion with resultant hemosiderosis and hemochromatosis 3. Poor compliance with chelation therapy (generally). Even in carefully managed patients, the following complications may develop: 1. Endocrine disturbances (e.g., growth retardation, pituitary failure with impaired gonadotropins, hypogonadism, insulin-dependent diabetes mellitus, adrenal insufficiency, hypothyroidism, hypoparathyroidism) 2. Cirrhosis of the liver and liver failure
16
3. Cardiac failure due to myocardial iron overload (often associated with arrhythmias and pericarditis) 4. Extramedullary hematopoiesis, resulting in bony deformities 5. Marked osteoporosis is nearly uniformly present by the time patients reach adolescence. The causes of this include medullary expansion, deficiency of estrogen and testosterone, nutritional deficiency, and desferrioxamine toxicity. Manifestations include rickets, scoliosis, spinal deformities, nerve compression, fractures, and severe osteoporosis. Osteoporosis can be delayed by the early institution of chelation in childhood and sex hormone replacement early in adolescence. Many of the complications of thalassemia seen in developed countries today are the result of iron overload: in the liver, fibrosis and cirrhosis; in the beta cells of the pancreas, diabetes mellitus; in the pituitary, testis, and ovaries, growth retardation and hypogonadotropic hypogonadism; in the parathyroid, hypocalcemia and osteoporosis; and in the heart, arrhythmias, myocarditis, and intractable cardiac failure. Most, if not all, of these complications can be avoided by the consistent use of an iron chelator. However, chelation therapy also has associated complications.1,2 1.12 PREVENTION Counseling about thalassemia is very necessary for screening and understanding of the patient. Prenatal DNA testing has been available for several years. The decision to perform prenatal diagnosis in parents known to be at risk for having a child with thalassemia is complex and is usually influenced by several factors, such as religion, culture, education, and the number of children in the family. Genetic counseling by professionals that addresses the details of both the genetic risks and the testing risks involved is expected to help the parents make an informed and intelligent decision concerning the procedure. Unfortunately, such tests are not available in certain
17
areas of the world where they are needed most. Extensive screening programs and prenatal diagnosis has resulted in a significant decline in the incidence of thalassemia in some of the high-risk Mediterranean countries. 1,2 1.13 PROGNOSIS The prognosis depends on the type and severity of thalassemia. As stated above, the clinical course of thalassemia varies greatly from mild or even asymptomatic to severe and life threatening. 1,2 Individuals with thalassemia minor (thalassemia trait) usually have asymptomatic mild anemia. This state does not result in mortality or significant morbidity. The prognosis of patients with thalassemia major is highly dependent on the patient's adherence to long-term treatment programs, namely the hypertransfusion program and life-long iron chelation. Allogeneic bone marrow transplantation may be curative. 1,2
18
CHAPTER 2 OBJECTIVE The objective of this paper is to report a case of beta-majot thalassemia in a 6years-old boy that was admitted at the non-infectious unit of Haji Adam Malik General Hospital on June 5th, 2011 CASE F, a six years old boy, admitted to Adam Malik Hospital on June 5th 2011 with chief complaint of paleness since 3 days ago. Bleeding(-), history of bleeding(-), epistacsis(-). Fever since 3 days ago. Fever is characterised as increase and decrease, and fever is subfebrile which is relieved with fever relieving medication. Seizure and shivers were not found. Cough (-), vomite(-), diarrhea (-). This patient is a routine patient to this hospital and had already been diagnose with beta Thalasemia Major and had already taken blood transfusion for the last 3 years. His ferritin serum was previously counted 3 months ago to be more than 2000 ng/ml. History of past disease is beta thalasemia mayor. History of past medications are PRC transfusion, Desferral, Feriprox. Physical Examination
19
Generalised Status : Body Weight (BW) : 23 kg 117cm BW/BL : 104% (normoweight) Presens Status : Consciousness : Alert Temperature : 37,2 C Anemic (+), icteric (-), cyanosis (-), oedema (-), dyspnea (-) BW/Age : 100 % BL/Age : 97 % Body Length (BL) :
Localized Status : Head : Eye : Light reflex (+/+), isochoric pupil (Right = Left) , paleness of conjunctiva : Nose : Nasal flare (-) : Mouth: Mucous pale or cyanosis (-) : Ears : Secrete (-) Neck : Lymph node enlargement (-) Nuchal rigidity (-) RR: 20x/i, reguler, rales (-) Abdomen Extremities Urogenital : Soepel, normal peristaltic, normal skin turgor, Liver palpable 2cm below of arcus costa, spleen palpable hacket 2 Schuffner 3 : Pulse 98x/I, regular, adequate pressure and volume, warm, CRT < 3, BP : 80/50 mmHg : male, within normal limit Thorax : Symmetrical fusiform Retraction (-) HR: 98x/i, reguler, murmur (-) palpebra inferior (+/+), sclera icteric (-/-)
Laboratory Findings : (Adam Malik Hospital / 05/06/2011) Complete Blood Count : Hb Ht : 5.56 g% : 18% RBC : 2,68 x 106/mm3 neutrofil : 53,60 % limfosit : 33,90 %
WBC : 5600/mm3
20
PLT
: 192.000/mm3
monosit : 7,35% eosinofil : 4,12 % basofil : 1,020 % neutrofil absolut : 0,3 x 103/l
MCV : 67.20 fL MCH : 20.70 pg MCHC : 30.90 g % Differential Diagnosis : -
Beta Thalasemia Major + hemosiderosis Iron Deficiency Anemia + hemosiderosis
Working Diagnosis : Beta Thalasemia Major + hemosiderosis Treatment: PRC Transfusion 120cc/12hr Folic acid 1x1mg tab Vitamin E 1x100mg Desferral 1150mg in NaCl 0,9% 250cc 40 gtt/i
Planning Liver Function Test Renal Function Test Iron profile
21
Follow up June 6th 2011 S : paleness (+), fever (-). O : Consciousness : Alert ; Temperature : 37,0 C ; BW : 23 kg; BL : 117cm BW/BL : 104% (normoweight) Head : Eye : Light reflex (+/+), isochoric pupil (Right = Left) , paleness of conjunctiva palpebra inferior (+/+), sclera icteric (-/-) : Nose : Nasal flare (-) : Mouth: Mucous pale or cyanosis (-) : Ears : Secrete (-) Neck : Lymph node enlargement (-) Nuchal rigidity (-) Thorax : Symmetrical fusiform Retraction (-) HR: 82x/i, reguler, murmur (-) RR: 24x/i, reguler, rales (-) Abdomen : Soepel, normal peristaltic, normal skin turgor, Liver palpable 2cm below of arcus costa, spleen palpable hacket 2 Schuffner 3 Extremities : Pulse 82x/I, regular, adequate pressure and volume, warm, CRT < 3. BP : 80/50 mmHg Urogenital : male, within normal limit Laboratory Findings : (Adam Malik Hospital / 06/06/2011) Liver function Test : - Total bilirubin : 0,94 mg/dl Direct bilirubin : 0,21 mg/dl
22
Alkaliphosphatase : 130 U/L AST/SGOT : 57 U/L ALT/SGPT : 81 U/L
Renal Function Test : - Ureum : 16 mg/dl A P Creatinin 0,27 mg/dl Uric Acid : 5,1 mg/dl : Beta Thalasemia Major + hemosiderosis : Treatment: PRC Transfusion 120cc/12hr Folic acid 1x1mg tab Vitamin E 1x100mg Desferral 1150mg in NaCl 0,9% 250cc 40 gtt/i
Planning - Complete Blood Count Iron profile
Follow up June 7th 2011 S : paleness (+), fever (-). O : Consciousness : Alert ; Temperature : 36,7 C ; BW : 23 kg; BL : 117cm BW/BL : 104% (normoweight) Head : Eye : Light reflex (+/+), isochoric pupil (Right = Left) , paleness of conjunctiva palpebra inferior (+/+), sclera icteric (-/-) : Nose : Nasal flare (-) : Mouth: Mucous pale or cyanosis (-) : Ears : Secrete (-) Neck : Lymph node enlargement (-) Nuchal rigidity (-) Thorax : Symmetrical fusiform Retraction (-) HR: 88x/i, reguler, murmur (-) RR: 22x/i, reguler, rales (-) Abdomen : Soepel, normal peristaltic, normal skin turgor, Liver palpable 2cm below of arcus costa, spleen palpable hacket 2 Schuffner 3 Extremities : Pulse 98x/I, regular, adequate pressure and volume, warm, CRT < 3. BP : 80/50 mmHg
23
Urogenital
: male, within normal limit
Laboratory Findings : (Adam Malik Hospital / 07/06/2011) Hb : 11,9 g% RBC : 4,66 x 106/mm3 Ht : 34,80 % neutrofil : 77,60 % WBC : 10.110/mm3 limfosit : 13,60 % PLT : 183.000/mm3 monosit : 8,60% MCV : 74,70 fL eosinofil : 0,00 % MCH : 25,50 pg basofil : 0,200 % MCHC : 34.20 g % neutrofil absolut : 7,84 x 103/l Ferritin : >2000 ng/ml A : Beta Thalasemia Major + hemosiderosis P : Treatment: - IVFD D5% NaCl 0,45% 20 gtt/i Diet 1650 Kcal with 46gr protein Folic acid 1x1mg tab Desferral 1150mg in NaCl 0,9% 250 cc 40 gtt/i
Follow up June 8th 2011 S O : paleness (-), fever (-). : Consciousness : Alert ; Temperature : 37,1 C ; BW : 23 kg; BL : 117cm BW/BL : 104% (normoweight) Head : Eye : Light reflex (+/+), isochoric pupil (Right = Left) , paleness of conjunctiva palpebra inferior (+/+), sclera icteric (-/-) : Nose : Nasal flare (-) : Mouth: Mucous pale or cyanosis (-) : Ears : Secrete (-) Neck : Lymph node enlargement (-) Nuchal rigidity (-) Thorax : Symmetrical fusiform Retraction (-) HR: 94x/i, reguler, murmur (-) RR: 22x/i, reguler, rales (-) Abdomen : Soepel, normal peristaltic, normal skin turgor, Liver palpable 2cm below of arcus costa, spleen palpable hacket 2 Schuffner 3 Extremities : Pulse 98x/I, regular, adequate pressure and volume, warm, CRT < 3. BP : 100/60 mmHg Urogenital : male, within normal limit A : Beta Thalasemia Major + hemosiderosis
24
P -
: Treatment: IVFD D5% NaCl 0,45% 20 gtt/i Diet 1650 Kcal with 46gr proteinFolic acid 1x1mg tab
CHAPTER 3 DISCUSSION & SUMMARY DISCUSSION F, a six years old boy, admitted to Adam Malik Hospital on June 5th 2011 with chief complaint of paleness since 3 days ago. Bleeding(-), history of bleeding(-), epistacsis(-). Fever since 3 days ago. Fever is characterised as increase and decrease, and fever is subfebrile which is relieved with fever relieving medication. Seizure and shivers were not found. Cough (-), vomite(-), diarrhea (-). This patient is a routine patient to this hospital and had already been diagnose with beta Thalasemia Major and had already taken blood transfusion for the last 3 years. His ferritin serum was previously counted 3 months ago to be more than 2000 ng/ml. History of past disease is beta thalasemia mayor. History of past medications are PRC transfusion, Desferral, Feriprox. The thalassaemias are a group of heritable hypochromic anaemias varying in severity, caused by a defect in haemoglobin polypeptide synthesis. In b-thalassemia major, the most common of the homozygous thalassemia syndromes, the affected child
25
produces little or no hemoglobin A and is usually transfusion-dependent from early childhood. The b-thalassemia gene occurs commonly in countries that border the Mediterranean Sea as well as in Southeast Asia. Although most of the problems associated with these disorders are the result of long-term transfusion therapy, the severe anemia at the time of diagnosis may constitute a hematologic emergency.3 In the thalassemias, production of the globin portion of the hemoglobin molecule is defective. Cooley's anemia (b-thalassemia major) presents with severe pallor usually between 6 and 12 months of age, as the fetal hemoglobin (HbF) level declines but the normal rise in adult hemoglobin (HbA) production fails to occur because of reduced or absent b-globin production. Children with thalassemia have a shorter red cell life, fetal hemoglobin in their red cells until an older age than normal, and red cells that are more sensitive to oxidative stress. Before initiating chronic transfusions, the diagnosis of -thalassemia should be confirmed and the parents counseled concerning this life-long therapy. Beginning transfusion and chelation therapy are difficult challenges for parents to face early in their child's life. Before beginning transfusion therapy, a red cell phenotype is obtained; blood products that are leukoreduced and phenotypically matched for the Rh and Kell antigens are required for transfusion. Surgical method such as speenectomy and bone marrow transplantation may be indicated. SUMMARY Thalassemia is inherited disorder of hemoglobin production. Thalassemia is found scattered throughout the race in the Meditenaian, the Middle East, India, to South East Asia. Thalassemia has two main types based on the globin chains which is missing on the individual hemoglobin -thalassemia and -thalassemia, which will subdivided into several subtypes based on the degree of utation (gengetically) or severity of symptoms. Thalassemia is derived based in Mendels laws, recessive or dominant.
26
The heterozygotes are usually asymptomatic, whereas homozygous or compound heterozygous symptoms are more severe than -thalassemia and thalassemia. Treatment for this patient include transfusion theraphy, iron binding theraphy, surgical therapy, and also bone marrow transplantation. Each of them has a side effect of certain criteria and shuld be considered carefully. Counseling about thalassemia is very necessary for screening and understanding of the patient. Until now, patient with severe thalassemia usually not survive until adulthood, but a normal appearance is not impossible.
REFERENCES
1. Yaish, Hassan M. Pediatric Thalassemia. Updated April 30th, 2010 (Accessed June, 25th 2011). Available at : http://emedicine.medscape.com/article/958850overview 2. Takeshita, Ken. Beta-Thalassemia. Update September 27th, 2010 (Accessed June 24th, 2011). Available at : http://emedicine.medscape.com/article/206490overview#a0101 3. Lawson, Jack P. Beta-Thalassemia Imaging. Update May 25th, 2011 (Accessed June 25th 2011). Available at : http://emedicine.medscape.com/article/396792overview#a19 4. Bleibel, Samer A. Alpha-Thalasemia. Update August 26th, 2009 (Accessed June 24th, 2011) Available at : http://emedicine.medscape.com/article/206397overview
27
5. Richard E, Md. Behrman, Robert M.,Md Kliegman,Hal B.,Md Jenson, Nelson Textbook of Pediatrics 18th edition, USA : Elsevier. 2007. Chapter 454; Hemoglobin Disorders 6. Permono B, Sutaryo, dkk. Buku Ajar Hemotologi-Onkologi Anak Cetakan Kedua. Jakarta : Ikatan Dokter Anak Indonesia ; 2006 7. Brittenham ,Gary M. Iron-Chelating Theraphy for Transfusional Iron Overload. The New England Journal of Medicine: 2011 364:15, 1475-1477 8. Rund, Deborah. -Thalassemia. The New England Journal of Medicine: 2005 353:1135-1146
You might also like
- Narcissistic ParentDocument5 pagesNarcissistic ParentChris Turner100% (1)
- Scientific Writing VerbsDocument3 pagesScientific Writing VerbsNejdetEXn100% (1)
- Lesson 6 Intercultural ComDocument25 pagesLesson 6 Intercultural ComBrave MitraNo ratings yet
- G8DDocument61 pagesG8Dvivek1312100% (1)
- Thalassemia Case ReportDocument40 pagesThalassemia Case ReportGracelia DamanikNo ratings yet
- Opinion Essay: ECPE - Michigan Proficiency The (5) Types of ESSAYSDocument4 pagesOpinion Essay: ECPE - Michigan Proficiency The (5) Types of ESSAYSelpidavekriNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Rheumatic Endocarditis: o o o o oDocument5 pagesRheumatic Endocarditis: o o o o ogaratoh099No ratings yet
- A Case Study On ThalassemiaDocument20 pagesA Case Study On ThalassemiaCP Pineda ArolNo ratings yet
- Case StudyDocument42 pagesCase StudyChristine Joy Ilao PasnoNo ratings yet
- Radiology Developing Technique ChartsDocument4 pagesRadiology Developing Technique ChartsVarghese NellimoottilNo ratings yet
- Neonatal Hypoglycemia APNECDocument26 pagesNeonatal Hypoglycemia APNECyumicheongNo ratings yet
- Beta Thalassemia PathoDocument1 pageBeta Thalassemia PathoAngie LamoNo ratings yet
- Introduction To The Philosophy of The Human PersonDocument21 pagesIntroduction To The Philosophy of The Human Personanon_254928515No ratings yet
- Hyperbilirubinemia Case StudyDocument7 pagesHyperbilirubinemia Case Studyr_ramos0759No ratings yet
- DiarrheaDocument11 pagesDiarrheaMade DhamaNo ratings yet
- In Partial Fulfillment of The Requirements in Care of Mother and Child and Adolescent 217 Related Learning ExperienceDocument28 pagesIn Partial Fulfillment of The Requirements in Care of Mother and Child and Adolescent 217 Related Learning ExperienceAllyssa BunagNo ratings yet
- Minggu 5 LP THALASSEMIADocument14 pagesMinggu 5 LP THALASSEMIAMuhammad PanduNo ratings yet
- Beta ThalaDocument2 pagesBeta ThalaAngie LamoNo ratings yet
- Case Study Anemia-1Document6 pagesCase Study Anemia-1Melsya H UtamiNo ratings yet
- Jaundice NeonatalDocument26 pagesJaundice Neonatalhunk2662No ratings yet
- Premature Rupture of MembranesDocument12 pagesPremature Rupture of MembranesbafionitaNo ratings yet
- Care of HemophiliaDocument7 pagesCare of HemophiliaBasant karn100% (4)
- Tetralogy of FallotDocument38 pagesTetralogy of FallotJohn Paul MedalloNo ratings yet
- Case Study Asthma Group 2Document17 pagesCase Study Asthma Group 2Kennedy PelicoNo ratings yet
- Pyloric StenosisDocument5 pagesPyloric Stenosisensoooooooooo100% (1)
- Patient InformationDocument15 pagesPatient InformationPriyanjali SainiNo ratings yet
- GE BasavaDocument21 pagesGE BasavaAmalin PrãdhãñNo ratings yet
- Addison Disease, Penyakit AddisonDocument11 pagesAddison Disease, Penyakit AddisonKertiasihwayanNo ratings yet
- Case Study 1: Nicole: 1. Discuss The Significance of Nicole's Laboratory FindingsDocument12 pagesCase Study 1: Nicole: 1. Discuss The Significance of Nicole's Laboratory FindingsClint NavarroNo ratings yet
- Abruptio Placenta. Final OutputDocument15 pagesAbruptio Placenta. Final OutputCharles Loriaga Cruz IINo ratings yet
- NCP Poststreptococcal GlomerulonephritisDocument12 pagesNCP Poststreptococcal GlomerulonephritisScarlet ScarletNo ratings yet
- Abortion BSN 0PR-2: Case Study of BelleDocument27 pagesAbortion BSN 0PR-2: Case Study of BellekervinNo ratings yet
- Tuberculosis and Nephrotic Syndrome in A Child: Case ReportDocument34 pagesTuberculosis and Nephrotic Syndrome in A Child: Case ReportAldo YustiantoNo ratings yet
- Clinical Log-5 Tibia #Document5 pagesClinical Log-5 Tibia #Tahani KhalilNo ratings yet
- Case Report Pediatric Von&JepDocument23 pagesCase Report Pediatric Von&JepFarizan NurmushoffaNo ratings yet
- Addison's DiseaseDocument14 pagesAddison's Diseasedivya4nirmalaNo ratings yet
- Guada A. Dumapit RN, ManDocument18 pagesGuada A. Dumapit RN, ManAnne B. BuenvenidaNo ratings yet
- Birth Asphyxia: by Anne E. Odaro MCM/2017/69852Document26 pagesBirth Asphyxia: by Anne E. Odaro MCM/2017/69852ElvisNo ratings yet
- Cystic FibrosisDocument69 pagesCystic FibrosisPadma Sagarika KarriNo ratings yet
- Nursing Pediatric Case StudyDocument9 pagesNursing Pediatric Case StudyKJay Solijon100% (1)
- Premature Rupture of MembraneDocument5 pagesPremature Rupture of MembraneEspiritu, ChriscelNo ratings yet
- Dengue: Dengue Hemorrhagic Fever, Resulting in Bleeding, Low Levels of Blood Platelets andDocument5 pagesDengue: Dengue Hemorrhagic Fever, Resulting in Bleeding, Low Levels of Blood Platelets andFrance John Evangelista TorresNo ratings yet
- Pregnancy HypertensionDocument30 pagesPregnancy HypertensionJon Gab PaquitNo ratings yet
- PPH Introduction 1Document95 pagesPPH Introduction 1regine maeNo ratings yet
- Case StudyDocument84 pagesCase Studyalcojonic0% (1)
- Case Studies - Tetralogy of FallotDocument16 pagesCase Studies - Tetralogy of FallotKunwar Sidharth SaurabhNo ratings yet
- Toaz - Info Case Study Pneumonia PRDocument41 pagesToaz - Info Case Study Pneumonia PRTrixNo ratings yet
- Decompensated Liver DiseaseDocument16 pagesDecompensated Liver Diseasedk.clinicalresearchNo ratings yet
- Case Study - Hyperthermia: Name: Shamira Morrow DateDocument2 pagesCase Study - Hyperthermia: Name: Shamira Morrow Dateapi-419026891No ratings yet
- Spina Bifida, Meningocele MyelomeningoceleDocument1 pageSpina Bifida, Meningocele MyelomeningocelesmilingstarsNo ratings yet
- Case Stude NNJDocument6 pagesCase Stude NNJmuzamirNo ratings yet
- Case Presentation OF Acute Tonsillitis: Nueva Ecija University of Science andDocument38 pagesCase Presentation OF Acute Tonsillitis: Nueva Ecija University of Science andBeverly DatuNo ratings yet
- Client Profile With HypertensionDocument8 pagesClient Profile With HypertensionplokatzNo ratings yet
- Scrub Typhus FeverDocument20 pagesScrub Typhus FeverDimpal ChoudharyNo ratings yet
- Tetralogy of FallotDocument3 pagesTetralogy of FallotJohn Mark PocsidioNo ratings yet
- Respiratory DistressDocument10 pagesRespiratory DistressnilmbbsNo ratings yet
- Ramos-2bn NCP Delivery RoomDocument2 pagesRamos-2bn NCP Delivery RoomLouwella RamosNo ratings yet
- Case Presentation On Copd: By, Thomas Eipe Pharm D InternDocument32 pagesCase Presentation On Copd: By, Thomas Eipe Pharm D InternThomas EipeNo ratings yet
- Background: Viral Mumps InfectionDocument5 pagesBackground: Viral Mumps InfectionAgustin UyNo ratings yet
- AKI CASE NishaDocument64 pagesAKI CASE NishaSurkhali Bipana100% (1)
- Precipitate LaborDocument1 pagePrecipitate LaborJeli AlgasNo ratings yet
- Cirrhosis Case For PrintingDocument12 pagesCirrhosis Case For PrintingSean Mercado100% (1)
- Med Template - NifedipineDocument2 pagesMed Template - NifedipineAshlee KeeferNo ratings yet
- Thalassemiafinal 111212142013 Phpapp02 130321172427 Phpapp01Document35 pagesThalassemiafinal 111212142013 Phpapp02 130321172427 Phpapp01MUHAMMAD WAQAS TARIQNo ratings yet
- Thalassemia Case ReportDocument40 pagesThalassemia Case ReportZarvi Jane MangubatNo ratings yet
- Suitcase Lady Christie Mclaren ThesisDocument7 pagesSuitcase Lady Christie Mclaren ThesisWriteMyPaperForMeCheapNewHaven100% (2)
- Christify LyricsDocument1 pageChristify LyricsJomel GarciaNo ratings yet
- 9709 w06 Ms 6Document6 pages9709 w06 Ms 6michael hengNo ratings yet
- HAPPY CHRISTMAS b2 ActivitiesDocument2 pagesHAPPY CHRISTMAS b2 ActivitiesnereaNo ratings yet
- தசம பின்னம் ஆண்டு 4Document22 pagesதசம பின்னம் ஆண்டு 4Jessica BarnesNo ratings yet
- The Meaning of LifeDocument1 pageThe Meaning of LifeJayas SharmaNo ratings yet
- Synonyms & Antonyms of Mop: Save Word To Save This Word, You'll Need To Log inDocument6 pagesSynonyms & Antonyms of Mop: Save Word To Save This Word, You'll Need To Log inDexterNo ratings yet
- Syntax Made Easy (Roberta D'Alessandro)Document23 pagesSyntax Made Easy (Roberta D'Alessandro)John DoeNo ratings yet
- Cambridge International Advanced Subsidiary LevelDocument12 pagesCambridge International Advanced Subsidiary LevelMayur MandhubNo ratings yet
- Navneet Publications India Limited HardDocument34 pagesNavneet Publications India Limited Harddyumna100% (1)
- Disseminated Tuberculosis in An AIDS/HIV-Infected Patient: AbstractDocument3 pagesDisseminated Tuberculosis in An AIDS/HIV-Infected Patient: AbstractAmelia Fitria DewiNo ratings yet
- Effective Leadership Case Study AssignmentDocument5 pagesEffective Leadership Case Study AssignmentAboubakr Soultan67% (3)
- TIFR Pamphlet On Homological MethodsDocument105 pagesTIFR Pamphlet On Homological MethodsRAMJANNo ratings yet
- Artificial Neural NetworkDocument16 pagesArtificial Neural NetworkSahil ChopraNo ratings yet
- Essay On NumbersDocument1 pageEssay On NumbersTasneem C BalindongNo ratings yet
- The Wall Dramaturgical PacketDocument24 pagesThe Wall Dramaturgical PacketMarilo CostaNo ratings yet
- Application of Schiff Base Ligamd ComplexDocument7 pagesApplication of Schiff Base Ligamd Complexrajbharaths1094No ratings yet
- Chapter-1-Operations and Management: There Are Four Main Reasons Why We Study OM 1)Document3 pagesChapter-1-Operations and Management: There Are Four Main Reasons Why We Study OM 1)Karthik SaiNo ratings yet
- Ass HeniDocument14 pagesAss Henialexsabebe28No ratings yet
- Villaroel Vs EstradaDocument1 pageVillaroel Vs EstradaLylo BesaresNo ratings yet
- Resume Design 2019Document2 pagesResume Design 2019ezke4pq2100% (2)
- Concrete Batching and MixingDocument8 pagesConcrete Batching and MixingIm ChinithNo ratings yet
- 19 March 2018 CcmaDocument4 pages19 March 2018 Ccmabronnaf80No ratings yet