Professional Documents
Culture Documents
Integrating Play in Neurodevelopmental Treatment
Uploaded by
shafiqpeerOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Integrating Play in Neurodevelopmental Treatment
Uploaded by
shafiqpeerCopyright:
Available Formats
Integrating Play in
Neurodevelopmental
Treatment
Jill Anderson, Jim Hinojosa,
Carrie Strauch
Key Words: activity analysis.
neurodevelopment. play therapy
This article presents one perspective on the integra-
tion ofplay activities within a neurodevelopmental
frame of reference. Based on the premise that activ-
ities are characteristic of occupational therapy in-
tervention, issues related to combining play activi-
ties with neurodevelopmental prinCIples are
discussed. Clinical examples are also prOVided to il-
lustrate the value of integrating play activities
within the occupational therapy treatment of the
child with cerebral palsy.
Jill Anderson, MS, OTR, is Assistant Professor of Occupa-
tional Therapy, State University of New York, Health
Science Center at Brooklyn, 450 Clarkson Avenue, Brook-
lyn, New York 11203. She is NDT-certified in pediatrics.
Jim Hinojosa, MA, OTR, FAOTA, is Associate Professor of
Occupational Therapy, State University of New York,
Health Science Center at Brooklyn, Brooklyn, New York.
Carrie Strauch, OTR, is a private practitioner in New York.
She is NDT-certified in pediatrics.
T
he integration of play activities with neurode-
velopmental treatment (NDT) can be a chal-
lenge even for the experienced occupational
therapist. A primary goal of occupational therapy in
treating children with cerebral palsy is to promote
normal patterns of movement and prevent abnormal
postural reactions while the child is engaged in func-
tional, purposeful actiVities.
Treating a child with cerebral palsy often in-
volves a variety of treatment techniques and method-
ologies from several theoretical frames of reference.
Occupational therapists in pediatrics commonly use
the neurodevelopmental therapy frame of reference,
which involves the use of specific handling tech-
niques to facilitate normal muscle tone, patterns of
movement, and automatic responses. When NDT
principles are integrated into occupational therapy
intervention, the therapist must have a basic under-
standing of the tonal and movement characteristics of
each type of cerebral palsy, specific handling tech-
niques, and the performance components of develop-
mentally appropriate actiVities.
Integrating play activities with NDT can be diffi-
cult. It is a complex task to try to elicit specific re-
sponses through handling while simultaneously en-
gaging the child in purposeful play activities. Unsuc-
cessful attempts to integrate play with NDT may be
frustrating and may result in a limited use of activities
during occupational therapy intervention.
This article discusses some of the issues involved
in combining play with NDT and offers selected activ-
ity solutions. The authors believe that play interaction
with children with cerebral palsy is generally compat-
ible with the application of NDT principles. However,
we recognize that the integration of activities involv-
ing specific play materials, objects, and manipulative
or motor skills may not always be possible.
Review of the Literature
The occupational therapist'S unique use of playas a
therapeutiC activity involves the reconceptualization
of playas a purposeful activity (Hinojosa, Sabari, &
Rosenfeld, 1983). Play is an action on human and
nonhuman objects that is engaged in for its own sake.
Florey (1981) has identified six principles of play
common to many theories: Play is a complex set of
behaviors characterized by fun and spontaneity; play
is sensory, neuromuscular, mental, or a combination
of these three; play involves repetition of experience,
exploration, experimentation, and imitation of one's
surroundings; play integrates the child's internal and
external world; play permits the child to rehearse his
or her interpretation of reality and fantasy; and play
follows a sequential, developmental progression.
Thus, play activities develop the skills that will allow
The American journal of Occupational Therapy 421
the child to interact with the demands of his or her
environment.
There is agreement in the psycboanalyticallitera-
ture on two play has a central role in a
child's development ancl that tbe inhibition of play in
childhood has severe pathological implications (Er-
ikson, 1950; Pellar, 1954, Winnicott, 1971) When the
natural drive to play is thwarted during therapy, the
young child may become distressed. Older children
may lose concentration and repeatedly ask when ther-
apy will be finished or may become less cooperative,
more resistant, and manipulative.
From a psychoanalytic perspective, play helps
children achieve instinctual satisfaction by creating
substitutes that permit emotional expression (Plaut,
1979). A bright, socially interactive, 15-month-old in-
fant with spastic diplegia appeared to have a "psycho-
logical need" to constantly manipulate objects and
exercise control over play materials during therapy.
This upper extremity play may be a substitute for
gross motor exploration and independent ambula-
tion. The play also provided her with control over her
environment and possibly fulfilled her needs for au-
that are characteristic of the separa-
tion-individuation process.
Play facilitates mastery over anxiety by active
rather than passive means. When this same 15-month-
old child was first positioned in a supported standing
position in inhibitory casts, she appeared distressed
and fearful. She tolerated the lower extremity weight
bearing and calmed when her favorite play materials
were presented.
Handicapped children follow a developmental
play sequence similar to the sequence followed by
normal children, but sometimes at a delayed rate
(Field, Roseman, De-Stefano, & Koewler, 1982). An
8-year-old developmentally delayed child reqUired
the use of dramatic, interactive play typical of the pre-
school period to meet her developmental play needs
during therapy. Imaginative play progressed from
symbolic play with animals to role play with human
figures during the course of 1 year. The primary goal
for this child was to facilitate normal motor develop-
ment and the acquisition of fine motor skills.
The NDT frame of reference, an interdisciplinary
therapy approach, focuses on the normalization of
tone and the integration of primitive postural patterns
into the development of normal postural responses
and movement patterns (Smith, 1984). Therapists
evaluate the quality of the child's movement, devel-
opmental milestones, skills, movement sequences,
and postures (Stengel, Attermeier, Bly, & Heriza,
1984). To establish an appropriate goal for the child,
occupational therapists identify movement compo-
nents reqUired to achieve a functional goal (Boehme,
1985). Through handling and movement, appropriate
automatic reactions are elicited to achieve functional
goals (Scherzer & Tscharnuter, 1982)
One goal of NDT is to produce automatic move-
ment patterns without placing conscious attention on
tbe process. Historically, occupational therapists have
selected, used, adapted, and synthesized activities in
their treatment. A child absorbed in play is not fo-
cused on the motor demands inherent in the activity.
Through motor analysis, activity (play) integration,
problem solving, and facilitation of normal tone and
movement, occupational therapists address the spe-
cific developmental needs of the child (Smith, 1984).
Issues in Play and NOT
A primary objective of the NDT certification course is
to refine observation skills while developing han-
dling techniques through facilitation labs and hands-
on clinical practice. The course does not tend to focus
on play activity integration, possibly because of time
constraints. Participants are expected to synthesize
NDT concepts in their particular domain of concern
and into future clinical practice. Because the empha-
sis in the NDT course is on handling and normal
motor development, potential conflicts may arise
when occupational therapists try to integrate purpose-
ful goal-directed activities into NDT.
Traditionally, occupational therapists are ex-
pected to effectively use activities in treatment. Many
therapists who complete the NDT certification course
may experience role conflict if they perceive NDT
strategies as inconsistent with occupational therapy
treatment approaches. Aside from perfecting han-
dling skills, occupational therapists may feel that they
must also master the integration of activities with
NDT. To develop and perfect handling methods with
a specific child while proViding relevant play experi-
ences may create additional challenges. These com-
plex practice issues may be resolved in a variety of
ways. Therapists who specialize in NDT may disre-
gard the notion of combining play activities as a "per-
sonal philosophy of practice" and concentrate pri-
marily on handling techniques. Others may limit han-
dling and focus more on positioning while facilitating
the development of specific skills through activities.
Therapists may also alter the activity and NDT empha-
sis with different children or during treatment ses-
sions depending on the child's specific needs.
Occasionally therapists have difficulty integrating
play activities and may feel they have compromised
their occupational therapy roles. However, because of
the sophistication of skills reqUired to integrate play
with NDT, certain difficulties may be inherent in the
treatment process. Positioning the play activity while
simultaneously handling the child can be a difficult,
almost impossible, task with some children. Handling
July 1987, Volume 41, Number 7 422
techniques are modified according to the child's re-
sponses during movement sequences, and therapists
constantly analyze the child's reactions to determine
the effectiveness of handling methods. The addition
of a play activity creates another component for the
occupational therapist to plan, integrate, and monitor
in an already demanding treatment situation.
During the child's treatment, the therapist may
need periods of time to select, organize, and change
activities. Unfortunately, the child's attention or nor-
malized muscle tone and posture may be lost during
these periods. The efforts of a child with cerebral
palsy to participate in activities may also cause asso-
ciated reactions and abnormal postures that conflict
with the NDT approach. Thus, highly developed ob-
servation and handling skills are essential to coordi-
nate all aspects of treatment. The sophistication and
complexity of this intervention process is often not
recognized by occupational therapists and other pro-
fessionals.
Intervention
Because of their motor impairment, most children
with cerebral palsy cannot fully participate in many
play activities. Incorporating play within NDT has
many benefits and can fulfill a variety of therapeutic
goals (a) to develop specific cognitive and percep-
tual skills, (b) to provide appropriate activity experi-
ences as stimuli for normal movement patterns, and
(c) to mOtivate the child for intervention that suPPOrtS
normal developmental needs Play activities may sat-
isfy both the goal of the child to participate with his or
her world and the therapeutic goals of the therapist.
There are a number of ways of adapting and integrat-
ing activities with NDT
Activity Adaptation
Activity adaptation is inherent in the effective use of
play activities and involves (a) adapting the size,
shape, or consistency of the equipment or materials
used, (b) mOdifying the rules and procedures, (c)
adjusting the pOSition of the child, materials, and/or
environment, and (d) controlling the nature and de-
gree of interpersonal interaction. Thus, play activities
are continually modified to meet the changing needs
of the child. Using play activities while handling a
child involves continuous analysis and adaptation of
the activity. If the motor demands placed on the child
are high, the cognitive demands of the activity may
have to be lowered accordingly. Behavioral changes
and the child's emotional responses to activities and
treatment influence activity choice, adaptation, and
integration. Activities must be meaningful and pur-
posefully incorporated into treatment sessions.
The Americanjournal 0/ Occupational Therapy
The occupational therapist draws from the
knowledge of activity analysis and grading to adapt
activities. By using activity analysis, the therapist
identifies the critical aspects of the activity re lated to
the individual child and NDT goals. The two pro-
cesses involved in this analysis are an assessment of
the motor, cognitive, perceptual, and psychosocial
needs of the child and an evaluation of the compo-
nents of the activity. The specific NDT equipment
needs of the child are also considered A mobile
(therapist Jap, ball, or roll) or nonmobile surface is
selected to meet the therapeutic goals. Having ana-
lyzed both aspects, the therapist is challenged to pro-
vide the appropriate play activity while incorporating
NDT techniques. Each element or characteristiC (size,
shape, etc) of the activity and the type of play (dra-
matic, games with rules, etc) may be modified to
meet the specific needs of the particular child. For
example, if a 5-year-old girl with severe spasticity in
both her upper and lower extremities and normal in
telligence and language wants to play with the doll
house, the therapist first needs to analyze the various
components involved in playing with the doll house
In this case, the activity analysis may lead to adapting
the aCtivity by changing the location of the doll house,
the child's postural demands, or the manner in which
the child wi II manipulate the objects
Issues in Intervention
The successful integration of activities depends on an
appropriately structured physical environment with
the activity at the correct height and distance. Lack of
equipment or environmental restriCtions (e.g., home
and school settings) can complicate integrating play
activities in treatment.
Two factors that influence activity choices are the
neurodevelopmental goals (ie., techniques and se-
quences used with the specific child) and the thera-
pist's own body mechanics and coordination. During
treatment, the therapist must be prepared to move
with the child in a dynamic interplay. Therapists must
be mobile in their positioning and, therefore, use
postures that facilitate their own movement as well as
that of the child Assisting a child onto a roll may be
difficult for a therapist who is in a tailor sitting posi-
tion. During dynamic movement sequences, less
complicated play activities may be indicated.
Therapists adapt the degree of movement within
a given activity and also the sequence of movements.
Therapists may select static or dynamiC positioning.
For example, the child with severely involved, left
hemiplegia may need to sit on a stable surface to per-
form a puzzle or other perceptual motor activity.
When Side-Sitting and reaching with the affected arm
this child experiences movement in a different way
423
(i.e., subtle weight shifts and postural reactions).
When using static positioning and weight shifting,
elongation and the active use of these components
may be facilitated through subtle handling or by
adapting the activity. Thus, NDT principles are incor
porated in a treatment session without the use of ther
apy tools (balls, rolls).
In a dynamic movement sequence, movement
through space occurs with assisting the child from
one position to another. For example, the therapist
helps the child with mild, left hemiplegia down to the
floor to grasp puzzle pieces, step over a roll, and then
place pieces in the puzzle held in a high easel Dy
namic versus static positioning and movement se
quences (i.e., child on floor, roll, ball, or activity on
table, wall, or floor) are determined by the therapist.
Children with severe or complex physical limita
tions often require more handson treatment. Inter
vention demands by the therapist may increase with
the child's motor, psychological, cognitive, and per-
ceptual needs. It may at times be necessary during
treatment for the therapist to find a balance between
the child's ability to participate concurrently in move
ment sequences and play activities. Efforts to promote
one aspect may lead to loss of control of another
aspect.
Skill Development
Developing specific cognitive and perceptual skills in
a child while actively handling the child can be a
complex process. The child with delays in both motor
and perceptual spheres may be unable to participate
in treatment sequences that demand a combination of
these skills. The therapist must prioritize goals both
in treatment planning and during the treatment ses
sion. A preViously planned activity may be abandoned
or modified when the child is unable to successfully
participate or when the treatment objectives cannot
be achieved with the activity.
Occupational therapists may use a variety of theo
retical frames of reference with the same child. For
example, the child may benefit from the NDT frame
of reference with regard to motor deficits but also
require treatment for cognitive or perceptual deficits.
A therapist may even use more than one frame of
reference during a treatment session either simulta
neously or sequentially. For example, the treatment
of an 8-year-old child with mild spastic athetosis and
visual perceptual deficits involved selected visual
motor tasks during upper extremity activities to pro-
mote proximal shoulder girdle control. Because ef-
forts to combine higher level visual motor tasks dur-
ing movement caused excessive distress, this se-
quence was followed with a more sophisticated visual
motor task on the table.
Motivational Use of Play
Creative and innovative use of play materials, the en
vironment, and use of the self as a play agent are the
critical aspects in the effective integration of motiva-
tional play with NDT. The child's play interests and
capabilities have an extremely important role in activ-
ity selection. Although other disciplines use activities
for motivation during NDT, occupational therapists'
educational background and clinical expertise with
play provide a solid foundation for play intervention.
One of the unique contributions of occupational ther-
apy is the adaptation of developmentally appropriate
activities to meet the specific neuromuscular needs of
the child.
The use of current play materials and activities
may have an impact on the success of play during
therapy. Popular and contemporary activities and the
broad spectrum of play interests (i.e., games, televi-
sion shows, computers, technology, and humor) are
important both in activity selection and in interaction
with the child. Battery-operated toys may be adapted
with various kinds of on/off switches for the severely
impaired child with cerebral palsy. Less impaired
children may respond to electronic toys and techno-
logical devices, including toys that speak, respond to
touch, light up, or move, as well as academic learning
toys and computers.
Movement is an important aspect of the child's
developmental process and play repertoire from in-
fancy onward; for example, the 8-month-old rocks on
all four extremities in the quadruped position, the
I8-month-old climbs on and off chairs, or the 8-year-
old rolls down a hill Developmentally appropriate
movements may be considered play activities. Play
can be used to encourage normal movement patterns
when NDT is applied. By varying upper extremity ac-
tions on objects or toys (reaching, throWing, or plac-
ing objects), or the posture (Sitting, quadruped or
high kneeling), and/or the size of the objects, treat-
ment objectives can be met. Upper extremity elonga-
tion, trunk rotation, head and trunk positioning, ap-
propriate grasp, or a combination of these motor com-
ponents may be developed by using play activities as
stimuli for movement.
Activities which are simple, organized, and lim-
ited in scope allow the therapist to more effectively
handle the child while involVing the child in play
activities. Less complicated activities with fewer posi-
tioning requirements are effective and interfere less
with handling. With the young infant (birth to 3
months), the therapist's face and voice can be effec-
tive play objects to stimulate visual fixation and track-
ing, thereby facilitating side-to-side rolling while the
child lies supine. With the preschool child, simple
play materials can stimulate dramatic or imaginary
July 1987, Volume 41, Number 7 424
play. For example, a variety of hats (baseball, fireman,
or space helmet) were used with a 5-year-old boywith
spastic diplegia. First he was seated on a therapy ball
with his shoulders positioned behind his pelvis to
develop abdominal control. Lateral weight shifting
and rotation were encouraged when he reached out [0
grasp and switch hats with the therapist.
The repetitive use of an activity with variations
during a treatment session can also simplify the activ-
ity component. A 2-year-old girl with spastic diplegia
had graduated rings placed over her feet as she lay
supine. She reached for and stacked the rings while
side-sitting and wore them as bracelets when laterally
shifting her weight on the roll. For a 5-year-old child
with athetosis and normal intelligence, a pretend
game of gardening using colored cubes was used
throughout the therapy session. While sitting on a
roll, the child planted the garden (colored cubes),
emphasizing her trunk rotation and upper extremity
weight bearing. Kneeling, she harvested the vegeta-
ble garden by placing the vegetables on a small table.
Moving to stand, she prepared a vegetable soup, mix-
ing the blocks while holding on [0 a large spoon with
both hands.
Age-appropriate toys and activities are used [0
encourage participation in treatment. For example,
when an 18-month-old [Oddler straddled a bolster to
facilitate rotation and lateral weight shifting, three
large dolls were strategically placed on each side of
the roll. The child was encouraged to reach out and
identify the doll's facial features. Stuffed animals, an
effective alternative to bolsters and wedges for posi-
tioning, can also be used as a stimulating material for
dramatic play. With a 5-year-old child, small stuffed
animals were used to encourage pretend games while
the child was standing. Animals were placed appropri-
ately under the feet to facilitate weight shifting in the
step position.
School-age children often create games involVing
rules and competition; the number of seconds a child
can stand on the roll while laterally shifting weight
can prompt interest and motivation Playing baseball
for a 6-year-old boy with spastic diplegia, while he
was sitting on a therapeutic ball to promote lower
extremity weight bearing, prOVided the opportunity to
integrate basic motor skills in a developmentally ap-
propriate manner. The ultimate long-term goal for
children is to develop skills that will allow them [0
fulfill their life roles.
Summary
Occupational therapists' educational background in
normal growth and development, therapeutic use of
activities, and neurophysiological theory proVide the
basis for play intervention. Combining clinical experi-
ence with NDT and play activities with a Willingness
Tbe Ame,-iean loumat of Oee upationat Tberap)'
to experiment and learn from the child's responses
may result in more creative and appropriate actiVities.
Similar movements, actions, and thought processes
during play may facilitate participation in activities of
daily living; thus, play activities may support acqUir-
ing skills in other areas
Although this paper has focused on the integra
tion of NDT with play, the issues discussed may arise
with other neurophysiological treatment approaches.
Activities analysis and adaptation, pOSitioning of the
child, and handling methods are all equally important
aspects of therapeutic intervention. While consider-
ing the realistic physical limitations of the child,
therapists encourage the child's involvement in play
activity [0 develop the child's physical, cognitive, and
psychosocial abilities. Play involves the active partici-
pation of the child with his or her environment in a
manner that is enjoyable, rewarding, and satisfying.
Through play the child with cerebral palsy may ex-
plore and discover the world-learn, practice, and
become an interactive human heing.
References
Boehme R. (1985, November 1). Self-care assessment
and treatment from an NDT perspective. Neuro-Develop-
mental Treatment Association Newsletter, pp. 1, 5.
Erikson, E. H. (1950). Childhood and society. New
York: Norton.
Field, T M., Roseman, S., De-Stefano, L.]., & Koewler,
J (1982) The play of handicapped preschool children with
handicapped and non-handicapped peers in integrated and
non-integrated situations. TopiCS in Early Childhood Special
Education, 2, 28-38.
Florey, L. L. (1981) Studies of play: Implications for
growth, development and for clinical practice. American
journal of Occupational Therapy, 35, 519-528.
Hinojosa,]., Sabari,]., & Rosenfeld, M S. (1983) Pur-
poseful activities Americanjournal of Occupational Ther-
apy, 37, 805-806
Peller, L. E (1954) Libidin;li phases, ego develop-
ment, and play. Psychoanalytic Study of the Child, 9,
178-198
Plaut, E. A. (1979) Play and adaptation Ps)'choanaly-
he Study of the Child, 34, 217-232
Scherzer, A. L., & Tscbarnuter, I (1982) Early diag-
nosis and therapy in cerehral palsy. New York: Marcel
Dekker
Smith, M. M 0984, December). Applying the neuro-
developmental treatment approach to OT Deuelopmental
Disabilities Special interest Section Newsletter, pp. 1-2.
Stengel, T.]., Attermeier, S. M., Bly, L.. & Heriza, C. B
(1984) Evaluation of sensorimotor dysfunction. In S. K
Campbell (Ed.), PediatriC Neurological Physical Therapy
Cpp 13-87) New York: Churchill Livingstone.
Winnicott, D W. (1971) Playing and reality. New
York: Basic Books.
Related Readings
deRenne-Stephan, C. (1980) Imitation: A mechanism
of play behavior American journal of Occupational Ther-
apy, 34, 95-102.
425
Gunn, S. L. (1975). Playas occupation: Implications for
the handicapped. American journal of Occupational Ther-
apy, 29, 222-225.
Hindmarsh, W. A. (1979). Play diagnosis and play ther
apy. American journal of Occupational Therapy, 33,
770-775.
McEnvoy,]., & McConkey, R. (1983). Play activities of
mentally handicapped children at home and mothers' per
ception of play. International journal ofRehabilitation Re
search, 6, 143-151.
Reilly, M. (Ed.) (974) Playas exploratory learning.
Beverly Hills, CA: Sage Publications.
Sparling,]. W., Walker, D. F., & Singdahlsen,]. (1984).
Play techniques with neurologically impaired preschoolers.
Americanjournal of Occupational Therapy, 38, 603-612.
Vanderburg, B., & Kielhofner, G. K. (1985). Play in
evolution, culture, and individual adaptation: Implications
for therapy. American journal of Occupational Therapy,
36,20-28.
July 1987, Volume 41, Number 7 426
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 745 NullDocument5 pages745 Nullhoney arguellesNo ratings yet
- Research Management - Leadership & Management SkillsDocument13 pagesResearch Management - Leadership & Management Skillspuiying80No ratings yet
- Ela Print Concepts Lesson PlanDocument7 pagesEla Print Concepts Lesson Planapi-139062141No ratings yet
- Hallinger Murphy 1985Document33 pagesHallinger Murphy 1985Ivy marie SollerNo ratings yet
- Sentence StemsDocument2 pagesSentence Stemss3pkoNo ratings yet
- Rhetorical AnalysisDocument4 pagesRhetorical Analysisapi-554453220No ratings yet
- City Stars 4 PDFDocument153 pagesCity Stars 4 PDFVera0% (1)
- Northern Mindanao Colleges, Inc.: Self-Learning Module For Principles of Marketing Quarter 1, Week 4Document6 pagesNorthern Mindanao Colleges, Inc.: Self-Learning Module For Principles of Marketing Quarter 1, Week 4Christopher Nanz Lagura CustanNo ratings yet
- Action-Plan in English A.Y 2022-2023Document2 pagesAction-Plan in English A.Y 2022-2023Jessica Zipagan100% (1)
- Workload Management: An Implementation GuideDocument25 pagesWorkload Management: An Implementation Guidetahu walik mas brewokNo ratings yet
- A Project On PoojaDocument6 pagesA Project On PoojaJoel WaghchoureNo ratings yet
- Koretz, Daniel. Measuring UpDocument4 pagesKoretz, Daniel. Measuring UprafadrimarquesNo ratings yet
- Eric Berne Define Transactional Analysis AsDocument3 pagesEric Berne Define Transactional Analysis Aspragyanmishra19No ratings yet
- Module 1.1Document4 pagesModule 1.1Jen Kerly100% (2)
- The Common Mistakes of Undergraduate Efl Students in Writing Argumentative EssaysDocument10 pagesThe Common Mistakes of Undergraduate Efl Students in Writing Argumentative EssaysKenny BayudanNo ratings yet
- EI VAC Lecture 01Document21 pagesEI VAC Lecture 01FREE FIRE GAMERNo ratings yet
- Alfie Meiling - Unit 1 2 - Media Methods Skills and Production TechniquDocument5 pagesAlfie Meiling - Unit 1 2 - Media Methods Skills and Production Techniquapi-370719927No ratings yet
- Test Question TypesDocument5 pagesTest Question TypesiattilasterNo ratings yet
- School of Arts, Sciences and Education: Divine Word College of Bangued Bangued, AbraDocument8 pagesSchool of Arts, Sciences and Education: Divine Word College of Bangued Bangued, AbraAna Madel TorresNo ratings yet
- How To Pass Principal's TestDocument34 pagesHow To Pass Principal's TestHero-name-mo?No ratings yet
- Gioi Thieu SachDocument6 pagesGioi Thieu SachUnknownNo ratings yet
- Class A Operator Management Quiz Jan. 2017: Lanning Analyze Only The Internal Environment of The OrganizationDocument11 pagesClass A Operator Management Quiz Jan. 2017: Lanning Analyze Only The Internal Environment of The OrganizationCyril Grace BoocNo ratings yet
- The Priest of BeautyDocument16 pagesThe Priest of Beautyrhuticarr100% (1)
- MGT502 OnlineQuiz5 - 750MCQs - Solved PDFDocument176 pagesMGT502 OnlineQuiz5 - 750MCQs - Solved PDFZuha RaniNo ratings yet
- OU-ExchangePrograms 2022 A4Document20 pagesOU-ExchangePrograms 2022 A4killer Arun pubgNo ratings yet
- PTSD F What Is PTSD? (DMS-IV)Document8 pagesPTSD F What Is PTSD? (DMS-IV)Abigail VosNo ratings yet
- Action PlanDocument2 pagesAction PlanPhebelyn BaloranNo ratings yet
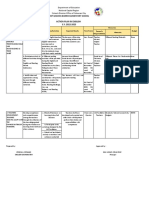
- RPMS Tool For Teacher I-III (Proficient Teachers) : Position and Competency ProfileDocument2 pagesRPMS Tool For Teacher I-III (Proficient Teachers) : Position and Competency ProfileLee ZielNo ratings yet
- LDM2 Study NotebookDocument72 pagesLDM2 Study NotebookThelma Ruiz SacsacNo ratings yet
- Module 4 Lesson 4.1Document17 pagesModule 4 Lesson 4.1mrasonable1027No ratings yet