Professional Documents
Culture Documents
TRANS Muscle Disease
Uploaded by
2012Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
TRANS Muscle Disease
Uploaded by
2012Copyright:
Available Formats
OS 211 Dr. Mina N.
Astejada
Muscle Diseases Exam 3
Outline: • a neuromuscular disease in which the muscle fibers
I. Introduction do not function for any one of many reasons, resulting
in muscular weakness
II. Classification of Myopathies
• primary defect is within the muscle (vs. neuropathy)
A. Hereditary
1. Congenital Myopathy
II. Classification of Myopathies (Appendix A)
a. Central Core Disease
b. Centronuclear/Myotubular Myopathy
c. Nemaline Myopathy A. Hereditary Myopathies
d. Congenital Fiber Type Disproportion 1. Congenital Myopathy
2. Muscular Dystrophy A clinically, genetically and pathologically
heterogeneous disorder defined by the presence
a. Congenital Muscular Dystrophy of particular histological features
b. Dystrophinopathies
Onset is often at birth or early childhood (~7
c. Limb Girdle Muscular Dystrophy years old)
3. Myotonia Dystrophica Floppy infant with variable hypotonia
4. Channelopathies Long “myopathic” face is a common feature
a. Sodium Channel Disease CNS and peripheral nerves are not usually
involved
b. Calcium channel Disease
c. Myotonia Congenita
Normal intelligence
5. Mitochondrial Myopathy Generally non-progressive
6. Metabolic Myopathy Diaphragmatic involvement may be
disproportionate to overall muscle weakness
B. Acquired
Inheritance: AR, AD or X-linked
1. Inflammatory Myopathies
CK are usually normal or slightly elevated
a. Idiopathic
b. Infectious Treatment: supportive
2. Toxic Myopathy
*Classification is based on histologic features (muscle biopsy
is therefore needed for diagnosis):
a. Central Core Disease
*Hi 2012! This trans was made from scratch because the 2011
supplementary CD doesn’t have a softcopy of this trans (they have the - Gene: Ryanodine receptor (RyR1)
filename but if u try to open it, different content)! But we are confident
about this trans. Medyo tinoxic namin ‘to! Happy reading! Swerte ng
- associated with malignant hyperthermia
Jolly B’s na magttrans nito! Hehe libre nyo kami. Haha!
I. Introduction b. Centronuclear/Myotubular Myopathy
Skeletal Muscle - Gene: Myotubularin (MTM1) X-linked
75% water Dynamin (DNM2) AR
20% protein
c. Nemaline Myopathy
5% others: high-energy phosphates, urea, lactic acid,
Ca, Mg, P, enzymes, amino acids, lipids and - Gene: ACTA1*, nebulin, α-tropomyosin, β-
carbohydrates
tropomyosin, slow troponin T
Myopathies
d. Congenital Fiber Type Disproportion
November 28, 2008 | Friday Page 1 of 10
D Twilighters
OS 211 Dr. Mina N. Astejada
Muscle Diseases Exam 3
- Gene: ACTA1*
Walker-Warburg Muscle Eye Fukuyam MDC1
* same gene but different location of mutation Brain a C
Agyria Pachygyria/ Agyria Focal Normal
Agyria brain
Figure 2. CNS Involvement in CMD. Take note that CNS involvement
A B is not an absolute characteristic of CMD.
b. Dystrophinopathies
Duchene Muscular Dystrophy (DMD)
C D • Most common
• Sex - linked recessive disorder (Xp21)
Figure 1. Different Types of Congenital Myopathy Based on Histology.
(A. Central Core Disease, B. Centronuclear Myopathy, C. Nemaline
Myopathy, D. Congenital Fiber Type Disproportion) • mutation in the gene coding for dystrophin (400kD)
• Clinical Features:
2. Muscular Dystrophy
1. Early signs - starts at age 3 to 5 years
First described by Nattrass in 1954 - Pelvic girdle weakness (waddling gait,
frequent falls, difficulty climbing stairs, awkward
It is a heterogeneous group of inherited primary running)
diseases of the muscle, clinically characterized
by progressive muscle weakness and wasting. - Pseudohypertrophy of calf muscles
Histologically, it is unified by the presence of - (+) Gowers’ sign
necrotic and regenerating processes, often
associated with an increased amount of 2. Later signs - 10 to 14 yrs old
connective and adipose tissues
- relentless progression & involvement of
TYPES: shoulder girdle muscles
a. Congenital Muscular Dystrophy (CMD) - Scoliosis & thoracic deformity
First described by Batten in 1903 - Inability to ambulate
A group of clinically heterogeneous AR inherited - at 20 to 25 yrs old - respiratory failure usual
muscle diseases endpoint in DMD; but because of advancement
in ventilation technology, cardiac failure is now
Characterized by hypotonia at birth, generalized the common endpoint
muscle weakness, frequently multiple contractures
Muscle Biopsy: necrotic and regenerating
process
• Diagnosis:
The clinical spectrum ranges from a very severe 1. Genetic studies
form, often resulting in early infant death, to
- Multiplex PCR- detect dystrophin gene deletion
relatively mild conditions, where the patient
in 60 % of cases
survives into adulthood
- MLPA- detect deletion and duplication, more
CK could range from normal to marked elevation
sensitive than multiplex PCR
2. Immunohistochemical stain for dystrophin –
negative
• Treatment:
1. NOT YET AVAILABLE
November 28, 2008 | Friday Page 2 of 10
D Twilighters
OS 211 Dr. Mina N. Astejada
Muscle Diseases Exam 3
2. Temporary stabilization with steroids DMD/BMD suspect
3. Gene therapy to date is not possible DNA
Multiplex PCR No gene deletion
Muscle biopsy
Becker Muscular Dystrophy (BMD)
Immunohistochemistry Normal
• Milder form of DMD (milder weakness) for dystrophin dystrophin staining
(+) Dystrophin gene
deletion
• Sex - linked recessive disorder (Xp21), allelic
No dystrophin Reduced dystrophin
staining staining
• 1 in 30,000 male births
DMD/BMD
• Partial deletion of the gene coding for dystrophin Non DMD/BMD
(vs. complete deletion in DMD) DMD BMD
Figure 4. Diagnostic Algorithm between DMD and BMD. Notice that
• Dystrophin is partially present , muscle both DMD and BMD have dystrophin gene deletion but BMD has
partial deletion only (kaya may patches pa of dystrophin sa histo). So
membrane is semi – functional
that’s why you need muscle biopsy to differentiate the two (gets?)
• Clinical Features:
1. Later onset of muscle weakness at slower rate c. Limb Girdle Muscular Dystrophy
2. Ambulatory up to adult life A group of phenotypically and genetically
heterogeneous disorder
3. Cardiac abnormality may be seen but mental
retardation is rare Weakness of the proximal muscles in the upper and
lower extremities
18 different gene locus identified:
Type 1- AD
Type 2- AR
LGMD 2A- Calpainopathy
Normal • fiber size variation
• endomysial fibrosis – increase
CT surrounding muscle cell
• lobulated fibers
LGMD 2B- Dysferlinopathy
DMD
• (-) dysferlin in diseased muscle
cells
* Tyoe 2 is most common. Calpainopathy can only be
diagnosed with genetic screening. Dysferlinopathy can now be
BMD diagnosed immunohistichemically by the absence of dysferlin
in diseased muscle cells
Figure 3. Immunohistochemical stain: important to differentiate DMD * Dysferlin is a protein linked with skeletal muscle repair.
and BMD. BMD has patches of dystrophin in the plasma membrane Absence is characterized with muscle weakness and wasting.
while DMD totally has no outline of dystrophin. Compare both with a
normal plasma membrane which has a clear outline of dystrophin.
3. Myotonia Dystrophica
• multisystem disease (muscle, heart, eye, endocrine
system & CNS)
• sustained muscle contraction; failure of relaxation
• close eyes or hands see if he can open eyes or
hands immediately
November 28, 2008 | Friday Page 3 of 10
D Twilighters
OS 211 Dr. Mina N. Astejada
Muscle Diseases Exam 3
• Histo: lots of nuclei in center indicates immature During attack, areflexia,
fiber (normal: peripheral/subsarcomeral), chained
nuclei, pale peripheral region (ring binden fiber), [K+] > 6mM, signs of hyperkalemia in ECG
type1 fiber hypotrophy (DARKER colored due to
lots of mitochondria) mas maliit size ng fiber Tx: acetazolamide and thiazide diuretics (excrete
excess K)
• Charcteristics:
Weakness
Paramyotonia Congenita:
Myotonia (sustained muscle contraction)
Paradoxical myotonia, increasing muscle stiffness
Cataracts with physical exercise, worsening of myotonia by cold,
weakness after exposure to cold.
Cardiac arrhythmia
Tx: acetazolamide, mexiletine and salbutamol
Frontal balding
Potassium-aggravated myotonia :
TYPES: (based on weakness pattern distribution)
Muscle stiffness without weakness and cold
Type I sensitivity.
• Distal> proximal
• Facial muscle affected b. Calcium Channel Diseases (all are PRIMARY diseases-
genetic)
• CTG trinucleotide repeats in DMPK gene
(chromosome 19) Hypokalemic Periodic Paralysis
• AD Characterized by prolonged (days/ weeks)and severe
bouts of weakness weakness is due to the
decrease in serum K+ (hindi makalabas sa cell)
therefore there is a decrease in action potential
Precipitated by rest after a period of exercise or stress
Type II
• Proximal > distal Tx: oral potassium supplements, acetazolamide
• Facial muscle rarely involved
Malignant Hyperthermia
• CCTG repeat expansion in ZNF9 gene (Chromosome
3)
Dramatic and often fatal condition characterized by
• AD rapid and sustained rise in Temp during generalized
anesthesia associated with generalized muscle
rigidity, tachycardia, tachypnea and cyanosis
4. Channelopathies Severe respiratory and metabolic acidosis
• Mutations in the genes encoding the proteins of the Extensive muscle necrosis with subsequent
ion channels of the sarcolemma, SR and T-tubules myoglobinuria and renal shutdown
disrupt the normal transport of ions, in particular,
Na+, K+, Cl- and Ca2+ CK =/>50,000IU/L with elevated serum K+
• Clinically falls into 2 groups: those with myotonia
and those with paralysis
QUESTION: Why is Hyper- and Hypo-kalemic Periodic
Paralysis under sodium and calcium channel diseases,
• Appendix 1: Ion Channel Disorders of the Skeletal respectively?
Muscle. REMEMBER: Becker Syndrome lang ang
AR! All the rest are AD! ANSWER: Kasi daw K+ can pass through those channels
made up of calcium and sodium. The problem is with calcium
and sodium. Ung K+ ay effect na lang of that disorder (thus,
the name hyper- and hypo-kalemic). According to ma’am din, it
TYPES: is not that well understood pa.
a. Sodium Channel Diseases:
Hyperkalemic Periodic Paralysis c. Myotonia Congenita
Paralytic episodes usually at rest after physical
excercise. • Gene mutation (encoding chloride channel)
November 28, 2008 | Friday Page 4 of 10
D Twilighters
OS 211 Dr. Mina N. Astejada
Muscle Diseases Exam 3
• Characteristics:
- Myotonia
- Muscle stiffness
- warm-up phenomenon- increased muscle
strength with decreased activity
- Muscle hypertrophy
“- herculean” appearance
TYPES:
Thomsen’s disease: AD inheritance, generalized
Becker’s disease: AR inheritance; more of lower ex Figure 5. Modified Trichrome Gomori stain: Ragged red fibers are the
small patches of red stain surrounding and inside the muscle fiber.
Mitochondrial Diseases
6. Metabolic Myopathy
Maternally inherited
Glycogenosis
Clinically heterogenous
breakdown of glycogen is an important source
Onset may vary from birth to adulthood of energy in muscle
Course may be rapidly progressive, static or even defect in any steps in the glycolytic pathway
reversible can cause muscle fatigue, cramps, or
rhabdomyolysis, which is an important
Distribution of weakness may be generalized with indicator of several metabolic problems
respiratory failure or proximal more than distal, and
may involve facial muscles with associated ptosis and
progressive external ophthalmoplegia
Acid Maltase Deficiency
Serum and CSF lactate level may be increased
• 3 main clinical types: severe infantile
(Pompe’s), juvenile and adult onset
5. Mitochondrial Myopathy Pompe’s disease (most common): usually
fatal in infancy affecting the liver, heart,
Mitochondrial myopathy, Lactic acid and stroke-like skeletal muscles, CNS and kidneys
symptoms (MELAS)
Severe hypotonia
- can be a differential diagnosis for stroke
because of the ‘stroke-like’ symptoms: sudden
weakness in 1 side; normal labs Tx: enzyme replacements (Genzyme)
ONLY metabolic disease with treatment!
Myoclonic epilepsy and ragged red fiber (MERRF)
Patho: lots of vacuoles with basophilic
- cereballar atrophy materials
Chronic Progressive External Ophthalmoplegia Tx effect could be toxic myopathy (but don’t
(CPEO) deny Tx) monitor CK level and glycogen
Kearns Sayre Syndrome (KSS): retinitis B. Acquired Myopathies
pigmentosa, PEO and heart block
1. Inflammatory Myopathies
*RAGGED RED FIBER is present in all types of mitochondrial
myopathy! This indicates an abnormal mitochondria TYPES:
a. Idiopathic: (Appendix B)
o Dermatomyositis (DM)
- Gottrons papules; Heliotrope rash in the face
and/or eyelids
November 28, 2008 | Friday Page 5 of 10
D Twilighters
OS 211 Dr. Mina N. Astejada
Muscle Diseases Exam 3
- Perifascicular atrophy: muscle fibers at
periphery of fascicles are atrophied
(secondary to ischemia; blood vessels o Overlap syndromes with CTD
involved); natitira ung nucleus tapos
nakakain ung membrane o Sarcoidosis
- Perivascular inf;ammation: lymphocytes o Behcet’s Syndrome
surround muscle fiber
Severe quadriceps atrophy
o Polymyositis (PM)
b. Infectious Myopathies
- fiber size variation
- atrophy not just peripheral A. Bacterial: Staphylococci, Streptococci, Yersinia,
- marked inflammation Legionella, Borrelia burgdoferi (Lyme’s dse),
Clostridium welchii (gas gangrene), Leprous myositis
o Inclusion Body Myositis (IBM) B. Parasitic: Trichinosis, Cysticercosis,
Trypanosomiasis, Toxoplasmosis
- most common acquired muscle disease >50
y/o C. Fungal: Candida, cyptococcus, sporotrichosis,
actinomycosis, Histoplasmosis
- Prevalence of 5-10/million
D. Viral: Adenovirus, Coxsackie, CMV, Influenza, EBV,
- Affects men > women at 2-3:1 HIV, Parainfluenza, HTLV-1, Hepatitis B & C
- Average time from symptom onset to
diagnosis is ~ 6 yrs
- Scooped out forearm; finger flexor atrophy
2. Toxic Myopathy (Appendix C)
(more distal dominant than polymyositis);
quadriceps atrophy
- DOES NOT RESPOND TO STEROIDS!
END OF TRANS
Appendx A. Classification of Myopathies
Based on age of onset:
November 28, 2008 | Friday Page 6 of 10
D Twilighters
OS 211 Dr. Mina N. Astejada
Muscle Diseases Exam 3
Based on etiology:
Hereditary Acquired
Channelopathies Drug-induced myopathies
Congenital myopathies Endocrine myopathies
Metabolic myopathies Inflammatory myopathies
Mitochondrial myopathies Myopathies associated with
systemic diseases
Muscular myopathies
Toxic myopathies
myotonias
November 28, 2008 | Friday Page 7 of 10
D Twilighters
OS 211 Dr. Mina N. Astejada
Muscle Diseases Exam 3
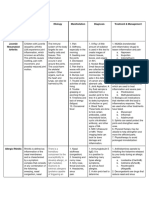
Appendix B. Clinical Features of Major Inflammatory Myopathies
Myopathy Gender Ageof Weakness CK Levels Histologic Response
Onset pattern Findings to Steroids
DM F >M Childto Proximal > 50X↑ Perimysial & Yes
Adult Distal perivasular
inflammation ;
perifascicular
atrophy
PM F >M Adult Proximal > 50X↑ Endomysial Yes
Distal inflammatiion
IBM M>F Elderly Proximal = 10X↑ Endomysial No
(>50yrs) Distal inflammation ;
Rimmed
vacuoles,
tubofilaments
on EM
Edward’s Troop: Nonette’s Gang:
November 28, 2008 | Friday Page 8 of 10
D Twilighters
OS 211 Dr. Mina N. Astejada
Muscle Diseases Exam 3
Nonette’s Mob:
Edward: Merry Christmas Jelly A’s & Jolly B’s!!! Enjoy the break!
Nonette: Hi phinoms, Conquis, & 4play! This trans is dedicated
to my Block B sisses dahil miss ko na kayo! Wag kayong
masyadong ma-toxic. Chillax! After renal, super benign nyo na!
Kami nmn ang toxic. Ultimate bonding soon, girls! Mwah! Hi
mahjong girls! Tanx sa mga pagkain. Kaya ako tumataba dhil sa
inyo! Haha! Go Duquerendribles! To my Singapore groupies,
sana makuha ko tlga on time ang passport ko. Baka hndi ako
makasama! Oh no! Wag nmn!!! Good luck Jelly A’s. Last stretch
for neuro. We can do this!!!
Appendix C. Features of Glycogenoses That Affect Muscles
Drug Clinical features Histology Comments
1. Statins (Cholesterol Myalgia,
Myalgia, weakness or Atrophy, inflammation, Fibrates &niacin also implicated in
loweringmyopath thyor
yor even rhabdomyolysis Occasional necrosis causing
causingCLAM
CLAM) CK elevation – 1%
1%
2. Ste
Steroids Insidious onset after weeks or months of Type II atrophy Regular exercise may redu ce this
reduce
use , Flourinatedform
Flourinatedforms are more myotoxic
Painless proximal weakness &atrophy, (eg.
eg. Dexamethasone,
ethasone, triamcinolon
cinolonee))
Normal CK levels
3. Zidovudine Proximal weakness, myalgia,
yalgia, elevated Mitochondrial proliferation,
CK levels Ragged Red Population
4. Chloroquine Painless proximal weakness, elevated CK Curvelinear bodies on EM Cardiac muscles &PN may be
involved
5. Colchicine Muscle pain &weakness Acid phosphase (+) PN involvement
Vacuoles
6. Amiodarone Muscle pain &weakness Vacuolar myopathyw
yopathywith inclusion
inclusion PN involvement
bodies
7. D- penicillamine
icillam Poximal pain and weakness Inflammation
(Seen in 1%
1%of treated patients)
8. Cyclosporine Muscle pain &weakness, Atrophy, accumulation of
Occasional CK elevation mitochondria, lipid vacuoles
9. Valp
alproic Acid Muscle weakness Mitochondria abnormalities, lipid Can improve with carnitine
accumulation supplementation
PALARONG MED IS THE BEST! CONGRATS 2012 PLAYERS! (Photos by Joanne Lucero )
November 28, 2008 | Friday Page 9 of 10
D Twilighters
OS 211 Dr. Mina N. Astejada
Muscle Diseases Exam 3
November 28, 2008 | Friday Page 10 of 10
D Twilighters
You might also like
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Surgery Shelf Notes 2021 PDFDocument43 pagesSurgery Shelf Notes 2021 PDFBhandari SadikshyaNo ratings yet
- Approach To Myopathy by AnkitDocument83 pagesApproach To Myopathy by AnkitankitNo ratings yet
- ITE Review 1.23.16Document4 pagesITE Review 1.23.16Diana HyltonNo ratings yet
- 5.02 Muscular Disease and Muscular Dystrophies: Mild NoneDocument10 pages5.02 Muscular Disease and Muscular Dystrophies: Mild NonevmdcabanillaNo ratings yet
- Khalish - Myotonic Dystrophy PDFDocument3 pagesKhalish - Myotonic Dystrophy PDFkhalishNo ratings yet
- Clinical and Pathologic Aspects of Congenital Myopathies: Ikuya Nonaka MDDocument8 pagesClinical and Pathologic Aspects of Congenital Myopathies: Ikuya Nonaka MDEvlin KoharNo ratings yet
- CNS Pathology-Degeneration and DementiaDocument7 pagesCNS Pathology-Degeneration and DementiaShunqing ZhangNo ratings yet
- Cancer BulletsDocument3 pagesCancer Bulletsraquel maniegoNo ratings yet
- New Classification and Treatment For Myotonic Disorders: Review ArticleDocument6 pagesNew Classification and Treatment For Myotonic Disorders: Review ArticleDana DumitruNo ratings yet
- BoeEoiATKXmvogGcWqYr1601439144 PDFDocument41 pagesBoeEoiATKXmvogGcWqYr1601439144 PDFsrisabrina christiaNo ratings yet
- Hercules Baby - A Rare Case Presentation of Congenital MyopathyDocument4 pagesHercules Baby - A Rare Case Presentation of Congenital MyopathyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- CNS Pathology SummaryDocument38 pagesCNS Pathology Summaryimeds100% (2)
- Muscular DystrophyDocument4 pagesMuscular DystrophyAbdul FarooqNo ratings yet
- Myotonic Muscle Disorders and Periodic Paralysis SyndromesDocument20 pagesMyotonic Muscle Disorders and Periodic Paralysis SyndromesIzabella MihályNo ratings yet
- Dolwick2012 PDFDocument10 pagesDolwick2012 PDFpaolaNo ratings yet
- Transverse Myelitis AtfDocument3 pagesTransverse Myelitis AtfRishi VermaNo ratings yet
- ArticlesDocument10 pagesArticlespurvaNo ratings yet
- Diseases of The PulpDocument93 pagesDiseases of The PulpIsha MalabedNo ratings yet
- Musculoskeletal ChartsDocument27 pagesMusculoskeletal Chartssurviving nursing school100% (3)
- Peripheral Nerve DiseaseDocument1 pagePeripheral Nerve DiseaseerickNo ratings yet
- Romero 2013Document16 pagesRomero 2013Rizki Nandasari SulbahriNo ratings yet
- A Review of Equine Muscle Disorders 2008 Neuromuscular DisordersDocument11 pagesA Review of Equine Muscle Disorders 2008 Neuromuscular DisordersADRIANA MARCELA HIGUERA MUÑOZNo ratings yet
- حل اسئلة العملي-1Document91 pagesحل اسئلة العملي-1حسام الوجيهNo ratings yet
- Tut1 BioDocument5 pagesTut1 Biodrahmed1028No ratings yet
- (MED) F.22 Polymyositis, Dermatomyositis (Reading Assignment)Document6 pages(MED) F.22 Polymyositis, Dermatomyositis (Reading Assignment)Yves RamosNo ratings yet
- Ii. Pathophysiology Causative Agents:: Alternative Learning Activities Level 3Document6 pagesIi. Pathophysiology Causative Agents:: Alternative Learning Activities Level 3Joyce Ann CumlatNo ratings yet
- CH 7 Genetic and Pediatric Diseases (P. 243-272, Nature of Genetic Abnormalities Contributing To Human DiseaseDocument16 pagesCH 7 Genetic and Pediatric Diseases (P. 243-272, Nature of Genetic Abnormalities Contributing To Human DiseaseJustine HungNo ratings yet
- Neuromuscular DisordersDocument12 pagesNeuromuscular DisordersZed HarrisNo ratings yet
- UMNLand AHCDocument27 pagesUMNLand AHCdrmamodoNo ratings yet
- Primary Mitochondrial Myopathies in Childhood 2021 Neuromuscular DisordersDocument10 pagesPrimary Mitochondrial Myopathies in Childhood 2021 Neuromuscular DisordersSuzie Simone Mardones SilvaNo ratings yet
- Self-Assessment: QuestionsDocument4 pagesSelf-Assessment: QuestionsRohit BharadwajNo ratings yet
- IMSE311 Lec Week-14Document6 pagesIMSE311 Lec Week-14Joanne RemolloNo ratings yet
- Mod 1 Pathophysiologic Effects of Cancer and Treatment ModalitiesDocument2 pagesMod 1 Pathophysiologic Effects of Cancer and Treatment ModalitiesJorese Hannah VictorinoNo ratings yet
- Revenge 3Document2 pagesRevenge 3Descargar scribdNo ratings yet
- Zaman Muscle PathologyDocument14 pagesZaman Muscle PathologyartikslennonNo ratings yet
- Advances in Shock Management and Fluid Resuscitation in ChildrenDocument9 pagesAdvances in Shock Management and Fluid Resuscitation in ChildrenErico Marcel Cieza MoraNo ratings yet
- Weakness (Approach To Diagnosis) - Dr. TulmoDocument2 pagesWeakness (Approach To Diagnosis) - Dr. TulmoMonique BorresNo ratings yet
- Bilateral Thalamic LesionsDocument10 pagesBilateral Thalamic LesionsOralBoardsNo ratings yet
- Met5. Mitochondrial DisordersDocument8 pagesMet5. Mitochondrial DisordersMonica J Ortiz PereiraNo ratings yet
- Out PDFDocument12 pagesOut PDFMaria RenjaanNo ratings yet
- Congenital Myopathies: Clinical Phenotypes and New Diagnostic ToolsDocument16 pagesCongenital Myopathies: Clinical Phenotypes and New Diagnostic ToolsRizki Nandasari SulbahriNo ratings yet
- General Principles of NeurologyDocument8 pagesGeneral Principles of NeurologyCARZ 42No ratings yet
- Neuromuskular: Dr. Ketut Widyastuti, SP.SDocument81 pagesNeuromuskular: Dr. Ketut Widyastuti, SP.SMirae RoseNo ratings yet
- 02.01-04 CNS I - AntiepilepticsDocument10 pages02.01-04 CNS I - AntiepilepticsMiguel C. DolotNo ratings yet
- Understanding Monogenic and Mitochondrial DiseasesDocument7 pagesUnderstanding Monogenic and Mitochondrial DiseasesErvin HoxhaNo ratings yet
- NCMA 219 - Course Task #11 (Dalman, Jhaziel)Document6 pagesNCMA 219 - Course Task #11 (Dalman, Jhaziel)Jhaziel Elizabeth C. Dalman100% (1)
- A Clinical Approach To The Patient With Suspected MyopathyDocument20 pagesA Clinical Approach To The Patient With Suspected Myopathyalvarorm1No ratings yet
- Autoimmune Myasthenia Gravis: Emerging Clinical and Biological HeterogeneityDocument16 pagesAutoimmune Myasthenia Gravis: Emerging Clinical and Biological HeterogeneityGiuseppeNo ratings yet
- Neurologic Disorders: 1 Anatomy & Physiology of The Nervous SystemDocument19 pagesNeurologic Disorders: 1 Anatomy & Physiology of The Nervous SystemJazzy Kathlene DumableNo ratings yet
- Bja MGDocument6 pagesBja MGVignesh VenkatesanNo ratings yet
- Muscle BiopsyDocument22 pagesMuscle BiopsyRoshan ThomasNo ratings yet
- Diseases of Skeletal Muscle FinalDocument30 pagesDiseases of Skeletal Muscle FinalclaudiaNo ratings yet
- Alzheimers DiseaseDocument21 pagesAlzheimers DiseaseBijay SharmaNo ratings yet
- Hematology Lec MidtermDocument10 pagesHematology Lec MidtermLoren EscotoNo ratings yet
- Dolor PlaquetasDocument5 pagesDolor PlaquetasmoisesNo ratings yet
- Systemic and Inflammatory Response To Injury: Dr. Michael Martin BaccayDocument9 pagesSystemic and Inflammatory Response To Injury: Dr. Michael Martin BaccayRamil SalmorinNo ratings yet
- Peripheral Nervous System (PNS) : 1. Anatomical ClassificationDocument4 pagesPeripheral Nervous System (PNS) : 1. Anatomical ClassificationShafiq ZahariNo ratings yet
- Myopathies: Presented By, Dr. Chandan N Intern, Department of Medicine, MIMS, MandyaDocument42 pagesMyopathies: Presented By, Dr. Chandan N Intern, Department of Medicine, MIMS, MandyaShafira WidiaNo ratings yet
- Neurologicemergenciesin Pediatricpatients Includingaccidentaland NonaccidentaltraumaDocument18 pagesNeurologicemergenciesin Pediatricpatients Includingaccidentaland NonaccidentaltraumaAvrilMontNo ratings yet
- Disorders of Neuromuscular TransmissionDocument15 pagesDisorders of Neuromuscular TransmissionShaheyar Ali QureshiNo ratings yet
- BSN 3 NSG Course Outlines TopicsDocument9 pagesBSN 3 NSG Course Outlines TopicsAllene PaderangaNo ratings yet
- Fa Step 1 ScheduleDocument5 pagesFa Step 1 ScheduleDinesh DalviNo ratings yet
- Boards SyllabusDocument14 pagesBoards Syllabus2012No ratings yet
- General Recommendation ImmunizationDocument69 pagesGeneral Recommendation Immunization2012No ratings yet
- PCAP UpdatesDocument60 pagesPCAP Updates2012No ratings yet
- ADA Summary of Guidelines 2011Document7 pagesADA Summary of Guidelines 2011IffatNaeemNo ratings yet
- Boards SyllabusDocument14 pagesBoards Syllabus2012No ratings yet
- Clin Tox Oral Vs IV ActylcysteineDocument19 pagesClin Tox Oral Vs IV Actylcysteine2012No ratings yet
- Diseases of The Anus Rev#1CDocument77 pagesDiseases of The Anus Rev#1C2012No ratings yet
- USMLEboardswhatworked 2008Document32 pagesUSMLEboardswhatworked 20082012No ratings yet
- CEBM Levels of EvidenceDocument2 pagesCEBM Levels of Evidence2012100% (2)
- The Division of Plastic SurgeryDocument36 pagesThe Division of Plastic Surgery2012No ratings yet
- Glomerulonephritis Block A TransDocument7 pagesGlomerulonephritis Block A Trans2012No ratings yet
- Review Lectures Forlu6: Basic Eye Exam Common Opd Complaints Common Er Cases PharmacologyDocument110 pagesReview Lectures Forlu6: Basic Eye Exam Common Opd Complaints Common Er Cases Pharmacologyupmed2012block9No ratings yet
- Review of The Evidence For Herbal Medications and NutraceuticalsDocument5 pagesReview of The Evidence For Herbal Medications and Nutraceuticals2012No ratings yet
- Art of Med Trans Feb 28Document9 pagesArt of Med Trans Feb 282012No ratings yet
- CSAP Full 2002Document125 pagesCSAP Full 20022012No ratings yet
- SCOPING DOCUMENT For WHO Treatment Guidelines On Pain Related ToDocument10 pagesSCOPING DOCUMENT For WHO Treatment Guidelines On Pain Related To2012No ratings yet
- Pharma EvaluationDocument1 pagePharma Evaluation2012No ratings yet
- Test Blueprint For Final Exam 2008-2009 For 75 PtsDocument3 pagesTest Blueprint For Final Exam 2008-2009 For 75 Pts2012No ratings yet
- American Diabetes Association (ADA) gUIDELINESDocument43 pagesAmerican Diabetes Association (ADA) gUIDELINESSamuel Rudolf Maranatha JulioNo ratings yet
- Organ Transplantation, Immunology and RejectionDocument2 pagesOrgan Transplantation, Immunology and Rejection2012No ratings yet
- Patho Lab Trans - ButchDocument6 pagesPatho Lab Trans - Butch2012No ratings yet
- Renal Patho Lab 2 PART 1 ColoredDocument8 pagesRenal Patho Lab 2 PART 1 Colored2012No ratings yet
- Cancer Pain Relief Who 1998Document86 pagesCancer Pain Relief Who 19982012100% (1)
- Trans Pulmopatho ColoredDocument8 pagesTrans Pulmopatho Colored2012No ratings yet
- Trans Glomerularpatho FinalDocument16 pagesTrans Glomerularpatho Final2012100% (1)
- OS 214 - Renal Module - Imaging of The KUBDocument9 pagesOS 214 - Renal Module - Imaging of The KUB2012No ratings yet
- 434 OS 212 PictoTrans - Cutaneous SymptomatologyDocument51 pages434 OS 212 PictoTrans - Cutaneous Symptomatology2012No ratings yet
- Approach To Myopathy (2022)Document72 pagesApproach To Myopathy (2022)Gerald PagalingNo ratings yet
- Miopati - Referensi MiopatiDocument25 pagesMiopati - Referensi MiopatiKelvin Theandro GotamaNo ratings yet
- Kelainan Kongenital Muskuloskeletal UmumDocument148 pagesKelainan Kongenital Muskuloskeletal Umumwafda satriaNo ratings yet
- EMG-NCV Tests Biofeedback: Dr. Vaishali (PT), Sr. Lecturer, AIMS, AhmedabadDocument119 pagesEMG-NCV Tests Biofeedback: Dr. Vaishali (PT), Sr. Lecturer, AIMS, AhmedabadSakshi Gadhvi100% (1)
- Myopathy: Figure 35-1Document14 pagesMyopathy: Figure 35-1Izabella MihályNo ratings yet
- Myotonia Congenita 書Document19 pagesMyotonia Congenita 書Wang Kuan-YingNo ratings yet
- Examination of The Motor System: Approach To Weakness: Key Teaching PointsDocument20 pagesExamination of The Motor System: Approach To Weakness: Key Teaching PointsMiravay ChavezNo ratings yet
- Presentation EMG AplicationDocument87 pagesPresentation EMG AplicationAndreas Arie WidiadiaksaNo ratings yet
- Case Report - MyopathyDocument17 pagesCase Report - MyopathydewaNo ratings yet
- Q & A Periodic ParalysisDocument3 pagesQ & A Periodic ParalysisRiri DaynuriNo ratings yet
- Diseases of The MuscleDocument51 pagesDiseases of The MuscleGianina RafaelNo ratings yet
- ChannelopathiesDocument18 pagesChannelopathiesJackyDanielsNo ratings yet
- A Pattern Recognition Approach To Myopathy.15Document24 pagesA Pattern Recognition Approach To Myopathy.15Maryam NabNo ratings yet
- Normal and Abnormal Spontaneous ActivityDocument23 pagesNormal and Abnormal Spontaneous ActivityLuís PachecoNo ratings yet
- Myopathy: By: Rey MartinoDocument16 pagesMyopathy: By: Rey Martinorey martinoNo ratings yet
- Hereditary Muscular DiseasesDocument18 pagesHereditary Muscular Diseasessafia ahmedNo ratings yet
- Musawi 30Document22 pagesMusawi 30Full MarksNo ratings yet
- Disorders of Skeletal MuscleDocument31 pagesDisorders of Skeletal Muscleapi-19916399No ratings yet
- Diseases of The Nerves and MusclesDocument17 pagesDiseases of The Nerves and MusclesHadil AltilbaniNo ratings yet
- A Pattern Recognition Approach To Myopathy. CONTINUUMDocument24 pagesA Pattern Recognition Approach To Myopathy. CONTINUUMjorgegrodlNo ratings yet
- The Office Evaluation of WeaknessDocument15 pagesThe Office Evaluation of WeaknessGustavo PestanaNo ratings yet
- Neurological Channelopathies: ReviewDocument14 pagesNeurological Channelopathies: ReviewPanduRespatiNo ratings yet
- Approach To MyopathyDocument22 pagesApproach To MyopathySurat Tanprawate100% (2)
- Muscle Channelopathies - The Nondystrophic Myotonias and Periodic ParalysesDocument17 pagesMuscle Channelopathies - The Nondystrophic Myotonias and Periodic ParalysesCarlos RiquelmeNo ratings yet
- Horlings 2008Document12 pagesHorlings 2008VIVEKNo ratings yet
- Differential Diagnosis of Periodic Paralysis and Important Diagnostic TestsDocument46 pagesDifferential Diagnosis of Periodic Paralysis and Important Diagnostic Teststhelegend 2022No ratings yet
- Rogawski 2004Document8 pagesRogawski 2004Dr. Kaushal Kishor SharmaNo ratings yet