Professional Documents
Culture Documents
A Review of Evidence Guiding The Use of Corticosteroids in The Treatment of Intraocular Inflammation Paul A. Gaudio
Uploaded by
John SmithOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Review of Evidence Guiding The Use of Corticosteroids in The Treatment of Intraocular Inflammation Paul A. Gaudio
Uploaded by
John SmithCopyright:
Available Formats
Review article A review of evidence guiding the use of corticosteroids in the treatment of intraocular inammation Paul A.
Gaudio
Department of Ophthalmology, Mettapracharak Hospital, Nakhorn Pathom, Thailand
Ocular Immunology and Inammation 0927-3948/04/US$ 22.00 Ocular Immunology and Inammation 2004, Vol. 12, No. 3, pp. 169192 2004 Taylor & Francis Ltd. DOI: 10.1080/092739490500192 Accepted 29 June 2003
Abstract Purpose: To review the published laboratory and clinical studies pertaining to the efcacy of corticosteroids in the treatment of intraocular inammation. Methods: A Pubmed computer search was conducted of all publications focusing on the efcacy of corticosteroids in treating ocular inammation, with an additional search of pertinent citations culled from these articles. Results: Experimental evidence has established the efcacy of corticosteroid eyedrops in treating intraocular inammation. The effectiveness of periocular corticosteroid injections as well as of systemic corticosteroids is supported by extensive clinical experience, although placebo-controlled trials are lacking. Few studies have documented differences in efcacy between the common corticosteroid agents or between the different routes of administration. Subconjunctival injection appears to achieve higher intraocular corticosteroid levels than do other routes of periocular injection or systemic therapy. Clinical experience with intravitreous corticosteroid injection is insufcient to rmly attest to its efcacy or safety. Conclusion: The efcacy of corticosteroids in treating intraocular inammation is based on limited experimental evidence and considerable clinical experience. Key words Corticosteroids; cystoid macular edema; uveitis Introduction This paper is a focused review of publications on the efcacy and practical utility of corticosteroid therapy for treating intraocular inammation. The aim is to evaluate the extent to which common methods of corticosteroid administration are derived from experimental evidence versus clinical impressions and experience. The pharmacology and side effects of corticosteroids have been previously addressed elsewhere; no attempt is made to duplicate those efforts in this review.118 available corticosteroid formulations The most commonly used corticosteroids in ophthalmic practice are listed in Tables 1 and 2. The pharmacology of the currently available agents employed Evidence based corticosteroid use
Correspondence and reprint requests to: Paul A. Gaudio, M.D. Department of Ophthalmology Mettapracharak Hospital Tambon Rai King, Amphur Sampran Nakhorn Pathom 73210 Thailand Acknowledgement: This study was supported in part by a grant from the Heed Foundation.
169
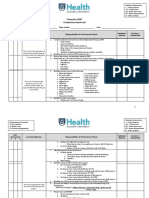
tab l e 1. Topical corticosteroid formulations. Drug name (generic available unless indicated) Dexamethasone sodium phosphate Dexamethasone alcohol Fluorometholone acetate Fluorometholone alchohol Concentration Formulation Common trade name*
Loteprednol (no generic) Medrysone (no generic) Prednisolone acetate
0.1% 0.1% 0.1% 0.1% 0.125% 0.1% 0.5% 0.2% 1% 0.12%0.125% 1%
Solution Suspension Suspension Suspension Suspension Ointment Suspension Suspension Suspension Suspension Suspension Solution Solution Suspension
Prednisolone sodium phosphate
0.125% 1%
Rimexolone (no generic)
1%
Decadron (MSD), (Akorn) Maxidex (Alcon) Flarex, Eone FML (Alcon), Fluor-Op FML Forte (Alcon) FML S.O.P. (Alcon) Lotemax (Bausch & Lomb) Alrex (Bausch & Lomb) HMS (Allergan) Pred Mild (Allergan) Econopred (Alcon) Pred Forte (Allergan), Econopred plus (Alcon) Inammase (CIBA), AK-Pred (Akorn) Inammase forte (CIBA), AK-Pred (Akorn) Vexol (Alcon)
*Trade names used in the United States and Canada. Trade names may vary in other countries.
tab l e 2. Injectable corticosteroid formulations commonly used in treating ocular inammation. Drug Concentration Common trade name* Potency (cortisone equivalents) 20 4 4 20 20 4 Duration of action (approximate) 13 days 36 weeks or more 36 weeks or more 13 days 10 days 612 weeks or more
Dexamethasone sodium phosphate Triamcinolone acetonide diacetate Betamethasone phosphate acetate/phosphate mix Methylprednisolone acetate
4, 10, 24 mg/ml solution 10, 40 mg/ml suspension 40 mg/ml suspension 3 mg/ml solution 3, 6 mg/ml suspension 80, 160 mg/ml depot suspension
Decadron (MSD) Kenalog, Kenalog-40 (Bristol Myers Squibb) Aristocort (Fujisawa) Celestone (Schering) Celestone soluspan (Schering) Depo-Medrol (Upjohn)
*Trade names used in the United States and Canada. Trade names may vary in other countries.
in the treatment of intraocular inammatory disease has been exhaustively reviewed in other publications.1921 limitations to interpreting published studies of corticosteroid efficacy Many laboratory studies of corticosteroids and the eye are difcult to interpret for clinical practice because the studies are limited to animal models and based on laboratory tech170 P.A. Gaudio
niques that are now partially superceded. Considerable experimental data regarding corticosteroids in the eye are derived from studies in rabbits, and may not be directly applicable to human eyes. There are numerous anatomical and physiological differences between rabbit and human eyes, including corneal thickness, tear turnover, aqueous pH, and aqueous protein concentration;18,2225 applying ndings from ocular pharmacokinetic studies in rabbit eyes to the treatment of human eyes, therefore, is problematic. The prevailing understanding of the ocular pharmacokinetics of corticosteroids is in part derived from studies based on techniques which have been supplanted, as the technology used to detect corticosteroids in biological uids has improved considerably in recent years. Early studies used radioisotope labeling to detect corticosteroids in bodily tissue and uids,2629 a technique that does not distinguish between the drug and its metabolites.30,31 The introduction of high performance liquid chromatography (HPLC) has enabled a specic and more sensitive detection of corticosteroid compounds in biological uids than is possible using radioisotope labeling.31,32 Where experimental questions have been re-addressed using HPLC technology, the results frequently conict with earlier ndings from radiolabeling studies. Nevertheless, for some questions, data from updated experimentation is lacking. Methods An online Pubmed search was conducted for all articles published between 1964 and 2002 for which the title, abstract, or key words included corticosteroids and uveitis. Articles for which the title and abstract were not available in English were excluded. The author selected articles for which the title suggested a focus on the efcacy of corticosteroids for treating uveitis. Relevant citations from this initial set were then sought out and reviewed, and the process of culling pertinent citations from pertinent articles was continued until all publications pertinent to this focused review appeared to have been included. Results and discussion topical corticosteroids Corticosteroid eyedrops have been in use since the 1950s for controlling ocular inammation. Extensive clinical experience attests to the efcacy of prednisolone and dexamethasone compounds for treating anterior segment inammation. Prednisolone acetate 1%, prednisolone phosphate 1%, and dexamethasone phosphate 0.1% are commonly employed to treat anterior uveitis.19,33,34 The use of one agent over the others is based on individual preference, since objective data from laboratory studies are conicting as to which of these agents is superior and there have been no controlled clinical trials comparing them. Evidence from animal studies The question of which corticosteroid eyedrop most effectively reduces intraocular inammation arises periodically among ophthalmologists, often with lively debate. Studies in rabbits have attempted to compare the relative anti-inammatory efcacies of prednisolone acetate, prednisolone phosphate, and dexamethasone phosphate, with conicting results. Prednisolone acetate and Evidence based corticosteroid use 171
prednisolone phosphate are pharmacologically inactive esters of prednisolone that serve to increase its solubility.These compounds are enzymatically de-esteried to prednisolone the pharmacologically active agent by esterases in the cornea and aqueous humor. Dexamethasone phosphate is similarly de-esteried. Traditional thinking has held that, since the corneal epithelium is lipophilic and the stroma hydrophilic, biphasic compounds (those with lipophilic and hydrophilic moieties, such as acetates or alcohols) penetrate the cornea to a greater degree than hydrophilic compounds (such as phosphate solutions).27 It has been further assumed that drug solutions rapidly wash out of the eye, while suspensions form a reservoir of continuously dissolving drug abutting the ocular surface. These presuppositions have given rise to the promulgation that prednisolone acetate suspension should achieve greater intraocular penetration hence greater efcacy than prednisolone phosphate solution. Studies performed in the early 1970s using radioisotope labeling in rabbit eyes supported the assumption that prednisolone acetate suspension penetrates the eye better than prednisolone phosphate or dexamethasone phosphate solutions.26,3539 The radioisotope-labeled acetate formulation of both topical dexamethasone and topical prednisolone was found to result in greater anterior chamber radioactivity (presumed to directly correlate with drug concentration) than phosphate formulations when the corneal epithelium was intact. Removal of the epithelium favored the penetration of the phosphates.27 These laboratory experiments have fostered the preferential use of prednisolone acetate in many clinical practice settings. The question of which prednisolone ester formulation better penetrates the eye was re-examined in the early 1990s, and the results differed from those of earlier studies. Using HPLC technology, no difference was found in the amount of prednisolone delivered across rabbit corneas whether prednisolone acetate 1% suspension or prednisolone phosphate 1% solution was placed on the eye.30,32,40 These ndings were noted both in vivo in rabbits and in vitro, using mounted rabbit corneas. HPLC techniques are more specic and more sensitive than radioisotope labeling,31 so one may conclude from these studies that the acetate and phosphate formulations of prednisolone penetrate the rabbit eye equally well. Fluorometholone (FML) was introduced after prednisolone and dexamethasone, and is nearly uniformly noted to be a weaker antiinammatory agent than prednisolone and dexamethasone. When studied in rabbits using radioisotope labeling, the commercially available 0.1% concentration of FML acetate resulted in less intraocular penetration than commercially available prednisolone 1% and dexamethasone 0.1% preparations.41,42 However in another study, when like formulations and concentrations were compared, the ocular penetrations of FML acetate 0.1%, dexamethasone acetate 0.1%, and prednisolone acetate 0.1%, determined by radioisotope labeling, did not differ substantially.43 The latter study suggests that drug concentration and/or ester formulation is more important than the corticosteroid moiety itself for determining ocular penetration.
172
P.A. Gaudio
The potencies of ophthalmic corticosteroids in treating intraocular inammation have not been compared in animal models. Claims that prednisolone acetate is the most potent ophthalmic corticosteroid have been based on a rabbit model of intracorneal inammation, a methodology that is questioned as to its validity.44 The corneal inammation was induced by injecting clove oil into the corneal stroma, and the partially lipophilic compounds prednisolone acetate and dexamethasone alcohol had greater anti-inammatory effects than the hydrophilic prednisolone phosphate or dexamethasone phosphate.27,45,46 Fluorometholone acetate showed anti-inammatory efcacy nearly approximating prednisolone acetate in this model;42 such a nding contrasts with the clinical experience of most practitioners. Other authors have since pointed out that clove oil would naturally favor the penetration of lipophilic moieties and repel hydrophilic compounds.44 This experiment has not been repeated using a different model of inammation. In the absence of convincing evidence regarding the relative efcacies of corticosteroid eyedrops for intraocular inammation, the question remains unanswered as to which should be the drug of choice clinically. Another study showed that increasing the concentration of prednisolone eyedrops from 0.125% to 1% resulted in greater drug delivery into the eye, with the degree of increase varying substantially. Studies in rabbits with radiolabeled prednisolone acetate and phosphate formulations found that, with the epithelium intact, substituting 1% for 0.125% formulations resulted in aqueous humor radioactivity increases of three- to fourfold for both compounds. When the epithelium was removed, this increase was nearly 12-fold.37,39 In a separate experiment, doubling the concentration of radiolabeled topical prednisolone acetate from 1% to 2% yielded less than a 1.5-fold change in aqueous humor radioactivity, but in the clove oil model of corneal stromal inammation even the 3% formulation did not result in substantially greater anti-inammatory efcacy than the 1% formulation.46 Studies exploring the utility of non-drop corticosteroid formulations suggest that dexamethasone phosphate ointment delivers about 25% less drug into the rabbit cornea and aqueous humor than an equivalent concentration and amount of drug solution.27,35 The authors speculate that the petrolatum vehicle binds the corticosteroid and does not release it fast enough to allow rapid ocular penetration. A gel formulation of prednisolone acetate appeared promising for achieving more sustained drug delivery than did the eyedrop suspension; however, it is not available commercially.47,48 Practitioners occasionally note particle size as a factor explaining variable clinical reponses to different brands of prednisolone acetate suspensions. A frequent explanation implicated generic formulations as being less nely milled, having larger particles that are less easily absorbed. A comparison of the absorption of prednisolone acetate suspensions composed of particle sizes between 5 and 22 microns found that the smaller particle size resulted in greater absorption in rabbit eyes.49 No difference in absorption was detected by other investigators comparing particles slightly larger versus smaller than 5 microns.50
Evidence based corticosteroid use
173
Studies in rabbits support the practice of increasing the frequency of topical corticosteroid administration to increase the anti-inammatory effect. Prednisolone acetate every fteen minutes was found to inhibit neutrophil migration into inamed corneas signicantly more than an hourly administration.51 Interestingly, this study also found that an hourly corticosteroid burst one prednisolone drop every minute for ve consecutive minutes each hour had the same neutrophilsuppressive effect as one drop every fteen minutes. It is generally held that corticosteroid eyedrops are ineffective for treating posterior segment inammation. However, the actual degree of penetration of topically applied corticosteroids into the posterior segment has not been quantitated in animals or humans. Data from humans: non-experimental observations Addressing the issue of generic versus brand name prednisolone acetate formulations and whether particle size plays a role, a 1998 study noted problems with generic formulations not maintaining a homogeneous suspension and plugging the bottle tip, thus interfering with drug delivery.52 Econopred (Alcon, Ft Worth, Texas) and Pred-Forte (Allergan, Irvine, CA) are brand name formulations of prednisolone acetate 1% suspension. The manufacturers of Econo-Pred and a generic prednisolone acetate formulation claim that since 1999, the particle size in Pred Forte, Econo-Pred, and generic prednisolone acetate (Falcon) has been less than 1 micron, and that the drug formulations themselves are identical (personal communication from Alcon Laboratories). This has not been evaluated independently. Patients occasionally report other differences between generic and brand name formulations, such as the shape of the bottle tip and ease of squeezing drops out. It may be that these differences, not the drug formulations themselves, are the source of occasional dissatisfaction with generic prednisolone acetate preparations. Uncontrolled studies have found that topical corticosteroids undergo systemic absorption. One study in healthy volunteers receiving dexamethasone 0.01% (one tenth the concentration commonly used in practice) in both eyes every two hours for one week showed marked decreases in urinary cortisol excretion.53 In healthy volunteers receiving dexamethasone 0.1% in both eyes eight times daily for six weeks, plasma cortisol levels were decreased although the hypothalamicadrenal axis was not suppressed.54 In clinical practice, the systemic absorption of corticosteroid eyedrops is probably most relevant for children because the drop volume is the same while a childs body mass is signicantly less. There are noteworthy case reports of systemic side effects of corticosteroid eyedrops. One case report describes an infant who became grossly cushingoid with adrenal gland atrophy, involution of the thymus, and hypertensive encephalopathy after receiving dexamethasone eyedrops bilaterally for four months and three sub-Tenons corticosteroid injections to each eye.55 The chronic cushingoid changes in this child appeared related to the prolonged use of dexamethasone eyedrops. Another case report describes an 11-year-old boy who became grossly cushingoid after receiving six months of prednisolone acetate drops.56 174 P.A. Gaudio
Data from humans: laboratory-based experimental studies A series of studies in post-cataract surgery patients has addressed the issue of the ocular penetration of corticosteroid eyedrops. Prednisolone acetate 1% was compared with prednisolone phosphate 0.5% (a concentration not commercially available in the US or Britain). The former delivered 20 times more prednisolone into the aqueous humor.5760 The authors of that study suggest that the 20-fold difference in ocular penetration cannot be explained entirely by the two-fold difference in drug concentration. An alternative explanation, noted by one of the study authors in a subsequent review,5 is the possibility that corticosteroid ocular penetration may follow nonlinear kinetics, such that very small differences in drug concentration may indeed result in marked differences in absorption.20 More detailed pharmacokinetic studies of corticosteroid ocular penetration have not been performed using chromatography techniques, making it difcult to interpret these authors results. At the very least, a valid comparison of these two drugs ocular penetration requires using like concentrations and these studies cannot be considered conclusive regarding the penetration of different prednisolone esters. In these studies in cataract patients, the aqueous penetration of dexamethasone alcohol 0.1%, betamethasone phosphate 0.1%, and uorometholone alcohol 0.1% (these are the commercially available concentrations of each drug, none of which are widely used to treat intraocular inammation in centers in the US) was substantially less than that of prednisolone acetate 1%,5760 a nding which may simply reect the 10-fold concentration difference in the drugs used. These drugs have different potencies when administered systemically, and when the data were mathematically adjusted to account for the relative potencies of each drug and for the different concentrations studied, prednisolone acetate appeared to deliver the most corticosteroid equivalence into the eye, suggesting that it may be more useful than the others for treating severe intraocular inammation. The problems interpreting data on ocular penetration for clinical relevance have been well recognized.18 The optimal intraocular corticosteroid concentration for treating inammation, where efcacy is maximum and side effects are minimum, is not known, nor are the actual relative anti-inammatory efcacies in the eye of the various clinically available agents.18 Dexamethasone and betamethasone, for example, are 45 times as potent as prednisolone in terms of pharmacologic activity at the molecular level,21 but whether this ratio changes in the microenvironment of the eye, where protein, mineral, carbohydrate, and other concentrations differ from peripheral blood, remains to be determined.18,27 Data from humans: placebo-controlled studies Placebo-controlled studies have shown that topical corticosteroids are efcacious in controlling uveal inammation, if used sufciently frequently. A 1972 study found no difference between dexamethasone (3 times daily) and placebo in treating inammation following cataract surgery,61 while another study found a small difference in anti-inammatory efcacy between once daily and three times daily dosing in a similar populaEvidence based corticosteroid use 175
tion.62 An earlier study63 found that topical betamethasone (an agent currently not marketed in the US), administered every three hours for two weeks, was also more effective than placebo in controlling inammation following intracapsular cataract surgery. A randomized, doublemasked study found topical betamethasone, administered every two hours for three weeks, more effective than clobetasone butyrate (also not marketed in the US or Canada, but previously available as Cloburate in the UK) in controlling signs of inammation in acute unilateral nongranulomatous anterior uveitis, and that either agent was better than placebo.64 A double-blind study published in 1980 evaluated clobetasone butyrate and failed to show a difference between it and prednisolone acetate in controlling anterior segment inammation after cataract surgery, while either drug administered four times per day was more effective than placebo.65 Clinical trials were recently conducted to evaluate loteprednol 0.5% and rimexolone 1%, marketed as anti-inammatory drugs inducing less intraocular pressure (IOP) elevation than traditional agents. In one trial, loteprednol 0.5% was found superior to placebo in treating inammation after cataract surgery when used four times daily postoperatively.66 Two other very carefully structured clinical trials, one studying rimexolone and one evaluating loteprednol, found them only slightly less effective in controlling mild to moderate intraocular inammation than prednisolone acetate 1%.67,68 While both study authors noted that prednisolone induced more IOP elevation than the newer drugs, the clinical signicance of this nding is uncertain because 1) the number of patients with signicant (10 mmg Hg) IOP rise was quite small in all studies and 2) the pre- and post-treatment IOPs are not given, so it is not known whether the IOP rises in the study patients were sufcient to cause glaucomatous damage.69 It appears therefore that loteprednol and rimexolone are both safe drugs with an antiinammatory potency slightly less than prednisolone acetate for mild to moderate ocular inammation. Rimexolone and loteprednol cost considerably more than generic prednisolone formulations (about twice the price in most pharmacies). In interpreting the results of placebo-controlled clinical trials, it should be noted that the patients in these studies frequently had postoperative inammation or unilateral non-granulomatous uveitis, both of which are conditions that are relatively mild and frequently resolve without intervention if given enough time. Therefore, results nding no difference between agents in treating relatively mild inammation require further study, because differences that appear subtle between various agents when treating mild anterior segment inammation may be more evident when treating severe inammation; studies to date have not included such patients. Conclusions regarding corticosteroid eyedrops Corticosteroid eyedrops have been convincingly shown to be more effective than placebo in treating anterior segment inammation. While it is the nearly overwhelming impression of experienced practitioners that prednisolone acetate, prednisolone phosphate, and dexamethasone phosphate are the most potent agents for treating severe anterior segment inamma176 P.A. Gaudio
tion, published data from rabbits and humans are conicting and inadequate to support recommending one agent over the other two. Clinical trials have shown that rimexolone and loteprednol are slightly weaker eyedrops than prednisolone acetate. The controversy regarding particle size affecting the potency of prednisolone acetate preparations is probably not relevant considering the agents currently available. It seems clear from rabbit studies that higher concentrations of corticosteroid eyedrops deliver more drug than do lower concentrations, although a curve of drug concentration versus absorption has not been made experimentally. Dosage frequency also needs clarication: rabbit studies have found that more frequent drops clearly deliver more drug, but the optimal frequency of administration, at which maximal absorption relative to the amount of drug applied to the eye, is not known. periocular injection It has long been common practice to inject corticosteroids directly adjacent to the globe to achieve more consistent intraocular delivery70 and to get the highest possible amount of steroid into the eye and the least amount into the rest of the body.71 Periocular injections are given in the subconjunctival space, beneath Tenons capsule either anteriorly or posteriorly,71 or transcutaneously through the temporal third of the lower eyelid using a short needle to place the drug alongside the globe, which some ophthalmologists term an orbital oor approach. Some practitioners administer corticosteroids by standard retrobulbar injection. Subconjunctival injection Studies involving subconjunctival administration tend not to distinguish injection into the space between the conjunctiva and Tenons capsule from the sub-Tenons space over the anterior globe. A 1969 paper entitled . . . subconjunctival administration . . . in fact unequivocally describes sub-Tenons injection in the description of methods,72 and it seems quite likely that, in other studies and in clinical practice, these two anatomically distinct spaces external to the anterior sclera are frequently not distinguished, and thus will not be distinguished in the ensuing discussion. Data from studies in human volunteers show that subconjunctival injection is a very efcient way to deliver corticosteroids to the vitreous and aqueous, allowing the greatest amount into the eye and the least systemically (as determined by drug levels in peripheral blood) when compared to other modes of administration.7375 Subconjunctival injection (directly over the anterior sclera) has been compared to transcutaneous periocular injection (through the temporal third of the lower eyelid to be delivered along the orbital oor) and to oral administration of dexamethasone in patients undergoing vitrectomy surgery. The subconjunctival injection of 2.5 mg dexamethasone resulted in high vitreous and aqueous humor dexamethasone levels, while a periocular administration of 5 mg yielded about one third as much and levels obtained by the oral administration of 7.5 mg were approximately one twelfth the concentration achieved by the subconjunctival route (the oral dose used in these studies approximates 35 mg prednisone, which is less than is typically started therapeutically for adult uveitis patients). The authors also assayed the subretinal uid, obtained from patients Evidence based corticosteroid use 177
with retinal detachment, for dexamethasone administered by these three techniques; subconjunctival injection again yielded the highest drug levels.76 These studies also showed that subconjunctival injection allows one to deliver less corticosteroid systemically than the other routes of administration. Subconjunctival injection of 2.5 mg dexamethasone resulted in serum levels about one half as high as those after a peribulbar 5 mg injection or a 7.5 mg oral dose.7375 Serum dexamethasone levels following subconjunctival injection were lower than the intraocular drug concentrations, while serum drug levels after periocular injection and oral administration exceeded the intraocular drug levels. These studies suggest that subconjunctival injection is a more efcient way of delivering dexamethasone into the vitreous than transcutaneous periocular injection. However, this nding may not be entirely applicable in the setting of uveitis, because 1) the patients studied underwent vitreoretinal surgery for a variety of diagnoses, some of which presumably involved blood-ocular barrier breakdown, but not all of which were inammatory conditions; 2) it remains to be determined how well subconjunctival injection compares to other routes of administration for delivering corticosteroids to the choroid and retina (Vitreous drug levels would seem a logical surrogate for levels throughout the posterior segment. However, in a recent study of an intraocular corticosteroid implant, drug levels in the vitreous decreased steadily over four weeks following implant placement, while the amount of drug detected in the retina/choroid remained stable. This suggests that corticosteroid concentrations in the vitreous may, in fact, not reect levels in the retina/choroid.);77 and 3) the applicability of these ndings remains unknown with regard to corticosteroid formulations other than dexamethasone. Three theories, based on animal studies, have been offered to explain how subconjunctivally injected corticosteroids enter the eye: 1) directly through the sclera; 2) via the tear lm through the cornea; or 3) via the blood stream. In support of the rst theory, a radiolabeling-based study on rabbits in the 1960s found that the drug directly penetrates the sclera following injection, and that drug concentrations drop off proportionally to distance from the injection sites.78 A study supporting the second theory showed that a subconjunctival injection serves as a depot from which the drug can diffuse and leak anteriorly into the tear lm, from where it can penetrate the cornea to enter the eye, much like a steady stream of eyedrops.79 In support of the third theory, a more recent HPLC-based study in rabbits showed that the ocular penetration of drugs injected beneath the conjunctiva is via the bloodstream.29 Following a subconjunctival dexamethasone injection, intraocular drug levels peaked earliest in the highly vascular choroid, and drug levels in the contralateral eye nearly equaled those in the injected eye after four hours.29 Others have suggested that some component of either transcleral or transcorneal absorption takes place following subconjunctival injection, since in their studies, ocular levels far exceeded blood levels of corticosteroid.74 Although the ultimate question of how subconjunctival corticosteroids enter the eye remains unresolved, the usefulness of this tech178 P.A. Gaudio
nique for intraocular corticosteroid drug delivery has been convincingly established. From a practical standpoint, it may be worth noting that subconjunctival injection can be cosmetically disguring, a side effect that some patients occasionally nd disturbing. Posterior injection A number of authors have stated that the treatment of posterior segment inammation with corticosteroids is best achieved by injecting the drug adjacent to the globe posteriorly in the retrobulbar or posterior sub-Tenons spaces, or along the orbital oor.71,75,8089 Although this practice is supported by very extensive clinical experience dating back nearly 50 years, like many well established medical therapies, it has never undergone placebo-controlled evaluation. Triamcinolone acetonide, triamcinolone diacetate, and methylprednisolone acetate are frequently administered via posterior injection when long-acting effect, sometimes as long as 12 weeks, is needed, and betamethasone is used for an effect of 12 weeks duration. In fact, the duration of action of these agents is impossible to gauge precisely in the setting of uctuating disease activity, and varies extensively between patients. According to manufacturers claims, when injected in joints to treat articular inammation, the duration of action of commercially available triamcinolone acetonide or diacetate and methylprednisolone acetate can last several weeks, and a betamethasone acetate/phosphate mixture may require reinjection every 12 weeks. The duration of action of any of these drugs when injected periocularly has not been studied, although there is one report of pharmacologically active triamcinolone being detected up to 13 months after periocular injection in some patients.90 A mixture of corticosteroids such as dexamethasone and triamcinolone has been advocated, as has the addition of lidocaine with or without epinephrine to betamethasone (many patients nd this drug painful on injection) when injecting these drugs around the eye. An experiment to determine whether particle sizes in various injectable corticosteroids change when mixed with each other showed that no change occurred. When mixed with lidocaine, however, betamethasone particle size did not increase, while particle sizes of triamcinolone and methylprednisolone did.91 Data from human and animal studies have shown that transcutaneous periocular injection is more efcient than oral administration, though less efcient than subconjunctival administration, for delivering corticosteroids to the eye. As noted above, in human studies, periocular injection delivered drug into the eye more effectively than did oral administration, although subconjunctival injection delivered still higher intraocular levels. Systemic absorption after either periocular or oral administration was high, with serum levels exceeding intraocular dexamethasone levels.73,75 Studies in monkeys92 and rabbits93 also found peribulbar injection more efcient than systemic administration for intraocular delivery. Posterior sub-Tenons (PST) depot injections are frequently administered to treat posterior segment inammation and cystoid macular edema (CME) in patients with uveitis.34,86,88 In one study, CME, documented by uorescein angiogram (FA), frequently improved after PST Evidence based corticosteroid use 179
injection, although visual function followed a more variable course and did not always correlate with improved angiographic ndings.94 A retrospective comparison of PST versus retrobulbar corticosteroid injection for the treatment of CME did not show a difference between a single retrobulbar injection and three sub-Tenons injections of triamcinolone (given at two-week intervals) for treating post-cataract CME in 48 patients.95 This study had no control group and statistical power calculations are not shown, so the nding of no difference between groups may not be conclusive. Other direct comparisons between sites of posterior corticosteroid injection have not been performed, and preference for one route of posterior injection over others remains a matter of clinical experience. The means by which corticosteroids injected near the posterior globe enter the eye have not been demonstrated conclusively. One study found that, four hours following retrobulbar dexamethasone injection in rabbits, the injected and contralateral eyes had signicant and nearly equal dexamethasone levels, suggesting largely hematogenous absorption by this route.29 Whether contralateral drug delivery occurs in other forms of posterior injection is unknown, but analyses of the therapeutic efcacy of posterior sub-Tenons injections have found this to be limited to the ipsilateral eye.86,88 PST injection by the superotemporal approach appears to allow the most accurate placement of the subTenons depot adjacent to the sclera behind the macula,96 and some practitioners believe that this proximity is advantageous for treating CME, supposing that the drug can diffuse directly through the sclera to the inner tissues. Human scleral permeability to dexamethasone has been demonstrated in vitro: this permeability was not altered by age, laser, or cryotherapy, but was greater in sclera which had been surgically thinned.97 Surgical thinning is a questionable surrogate for anatomical variation in scleral thickness which this study did not evaluate but this nding nevertheless suggests that scleral permeability to corticosteroids is inversely proportional to anatomical scleral thickness. Whether the scleral permeability to dexamethasone also applies to triamcinolone and other depot corticosteroids is not established, nor is it known whether these compounds, when injected outside the sclera adjacent to the macula, access the macula primarily via direct diffusion, despite the maximum thickness of the posterior sclera, or by hematogenous transport. Disastrous immediate complications of posterior injections may occur. Globe penetration, intravascular injection resulting in arterial occlusion, injection of the optic nerve or beneath the optic nerve sheath, and retrobulbar hemorrhage have been reported.98 Long-term complications of repeated injections include orbital fat atrophy and ptosis, and while it is not known how many uncomplicated injections a patient may safely undergo, there is a report of one patient receiving nearly 60 injections per eye before receiving an intraocular corticosteroid implant that was in development.99 Intraocular pressure (IOP) rise occurs to the same degree and frequency as with corticosteroid eyedrops.100 IOP rise following PST injection was found to be signicantly more likely in patients who had demonstrated a propensity for IOP elevation with corticosteroid eyedrops.88,101,102 180 P.A. Gaudio
Conclusions regarding periocular injection Studies in humans have shown that subconjunctival injection delivers more drug into the eye and relatively less into the bloodstream than does transcutaneous periocular (orbital oor) injection and oral administration, establishing it as a more efcient form of corticosteroid administration. Transcutaneous periocular injection in turn appears to be a more efcient form of administration than oral therapy. Although rigorous comparative studies are lacking, periocular, posterior sub-Tenons, and retrobulbar corticosteroid injections all appear equally effective for treating posterior segment inammation and cystoid macular edema. The mechanism by which corticosteroids injected around the eye enter the eye have not been conclusively demonstrated and may involve a number of different pathways. intravitreous injection Injection of corticosteroid directly into the vitreous is gaining popularity as a therapeutic approach to intraocular inammation and secondary macular edema. The use of this technique in the treatment of infectious endophthalmitis was originally reported in 1974,103 and its application to noninfectious uveitis is more recent. Intravitreous dexamethasone is given fairly commonly along with antibiotics following vitrectomy for the treatment of bacterial endophthalmitis. While animal model experiments have suggested some utility to this therapy,104,105 published clinical studies have not shown it to be benecial to visual outcome. A recent randomized, non-blinded trial in India compared vitrectomy and intravitreous antiobiotics with versus without 400 mg dexamethasone injection in patients with presumed bacterial endophthalmitis.106 The addition of dexamethasone to the treatment appeared safe and effective in reducing short-term inammation, but visual acuity results were not different between the two groups after three months. Retrospective analyses of the utility of intravitreous corticosteroids in postoperative107 and fungal108 endophthalmitis have also failed to show any visual benet. The endophthalmitis vitrectomy study (EVS) did not evaluate intravitreous corticosteroids.109 A report from Spain noted that intravitreous injection of triamcinolone suspension in 10 patients with severe non-infectious uveitis was markedly benecial in reducing inammation.110 While unpublished reports and case presentations corroborating this observation are increasingly frequent at ophthalmological society meetings and in other forums, the safety prole and precise role of this therapy remain to be claried in clinical trials. Corticosteroid implants are an effective mode of delivery into the eye for a sustained period, and early studies in humans have shown promising results for treating inammation. A pilot study of ve patients with severe recalcitrant uveitis evaluated sustained-release implants delivering uocinolone acetonide into the vitreous and showed this therapy helpful in reducing the inammation.111 A sustained-release 60 mg dexamethasone implant (Surodex, Oculex Pharmaceuticals, Sunnyvale, CA) has been evaluated in a few clinical trials and appears safe and approximately as effective as dexamethasone eyedrops for treating inammation after cataract surgery (its primary intended Evidence based corticosteroid use 181
purpose).112114 There is a report of one patient with uveitis whose condition responded well to a dexamethasone implant until the device became depleted.115 A sustained-release betamethasone phosphate implant that has the shape of a nail or tack has been designed to be inserted through the pars plana with the head remaining external, and to release the drug from the pointed tip.77 This implant, which appeared safe when tested in rabbits, is unusual in its conguration as well as in delivering intraocular betamethasone, a drug for which the commercially available injectable formulation is not suitable for intraocular use, due to the preservative vehicle.116 In addition to treating active inammation, intravitreous triamcinolone also appears to be effective in reducing CME, as evidenced by angiography117 and optical coherence tomography (OCT).118,119 Three studies involving a total of 14 patients have been reported in which authors injected between 2 and 4 mg commercially available triamcinolone acetonide; the drug was drawn directly from the bottle and included preservative. CME improvement after several weeks was documented by OCT and FA. Visual function improved in many cases, although less frequently than the anatomical appearance. Both CME and visual function that had improved occasionally returned to preinjection levels by three months. Six of the 14 reported patients developed sustained marked intraocular pressure (IOP) elevation requiring surgical or prolonged medical treatment.117119 The duration of action of intravitreous corticosteroids varies considerably. Intravitreous triamcinolone remained detectable in the vitreous for approximately 41 days following a 0.5 mg injection in rabbit eyes. This duration dropped to almost seven days in eyes that had undergone vitrectomy. The disappearance of the visible white triamcinolone depot correlated with the colorimetrically determined decrease in drug levels.120 Dexamethasone solution remains in the eye for a much shorter time than triamcinolone suspension. In rabbit eyes, the half-life of 400 mg of the drug, determined by radioisotope labeling, was about three hours. In another study with rabbits, HPLC was used to detect the drug and found none present after 72 hours.121 When studied in rabbits, standard treatment doses of dexamethasone were not toxic to the retina. No deleterious effects from the intravitreous injection of 4402000 mg dexamethasone were noted on ophthalmoscopy, and retinal examination was unremarkable following doses up to 2000 mg. However, after a 4000 mg injection, edema and serous retinal detachment developed, but resolved ophthalmoscopically after two weeks. Histopathologic study of the retina showed dose-dependent changes ranging from transient Mueller cell staining at 440 mg to vacuolization between the outer plexiform and outer nuclear layers at intermediate doses, with extensive photoreceptor degeneration and necrosis at 4000 mg.121 A 1985 study showed that the vehicles used in commercially available formulations of triamcinolone acetonide and diacetate (Kenalog and Aristocort, respectively in that study), as well as dexamethasone sodium phosphate (Decadron) and dexamethasone acetate (Decadron LA) appear to be safe and non-toxic after intravitreous injection of standard treatment doses.116 The injection of standard doses of preser182 P.A. Gaudio
vatives (benzyl alcohol, EDTA, methylparaben, propylparaben, sodium carboxymethylcellulose, and polyethylene glycol) into rabbit eyes resulted in no toxicity. The vehicles used in commercially available injectable formulations of methylprednisolone acetate (Depo-Medrol) and betamethasone sodium phosphate (Celestone soluspan), containing the preservatives myristyl gammapicolinium chloride and benzalkalonium chloride, respectively, induced cataract and the latter also caused marked distortion of the retinal cytoarchitecture within hours following injection in rabbit eyes, making these agents unsuitable for intravitreous injection. Conclusions regarding intravitreous corticosteroid injection Intravitreous dexamethasone injection is widely practiced as an adjunct therapy in the treatment of infectious endophthalmitis, although clinical evaluations to date have failed to demonstrate a visual benet. Intravitreous corticosteroid therapy via injection or implants is being increasingly used in the treatment of non-infectious uveitis and CME. While these approaches also lack rigorous clinical evaluation, early impressions have been positive and the therapy appears generally safe, although some patients have sustained IOP elevations. Dexamethasone has not shown toxic effects on the rabbit retina in the dosages typically injected into the vitreous. The vehicles in commercially available injectable formulations of dexamethasone phosphate, triamcinolone acetate, and triamcinolone acetonide appear safe in the amounts typically injected, while the vehicles in commercially available betamethasone and methylprednisolone are deleterious. systemic administration Many practitioners believe that systemic corticosteroids represent the most appropriate rst-line therapy for severe, bilateral, sight-threatening uveitis, particularly inammation involving the posterior segment.19,34,85,122124 Oral therapy with prednisone or prednisolone is used most commonly, although some practitioners advocate intravenous pulse methylprednisolone for an immediate antiphlogistic effect in uveitis125 as well as scleritis,126 Moorens ulcer,125 and corneal graft rejection.127 Oral prednisone or prednisolone are typically started at 1 mg/kg body weight daily, and pulse methylprednisolone doses range from a 500 mg single dose to 1 g three times daily for three consecutive days. These doses are the same as those used in treating systemic inammatory conditions, and no systematic assessment of the efcacy of various doses for treating ocular inammation has, to the authors knowledge, been published. The rationale for pulse therapy is that even very large single doses of corticosteroids are generally safe21 and avoid the side effects of longterm therapy, while having rapid and marked anti-inammatory benets that persist longer than the effects of smaller single doses. It is a common and perhaps prevailing assumption that for corticosteroids to be effective in treating intraocular inammation, these compounds must enter the eye in sufciently high levels. Since uveitis may, however, be the manifestation of systemic immune pathology recognized or not , controlling inammatory activity outside the eye might itself lessen the ocular disease. For this reason, the efcacy of systemic Evidence based corticosteroid use 183
corticosteroids in controlling intraocular inammation does not necessarily correlate with intraocular drug levels. The paucity of evidence supporting either of these notions points at the overall dearth of understanding surrounding the pathobiology of uveitis at the present time. Systemically administered corticosteroids achieve a signicant concentration in the vitreous within hours, even in the absence of inammation. The intraocular dexamethasone concentration has been shown to reach a peak between four and ten hours after a 7.5 mg oral dose.73 Methylprednisolone concentrations in the vitreous peaked approximately six hours following a 500 mg IV pulse in non-inamed eyes, and only two hours in eyes with retinal detachment.128 The precise ocular bioavailability of oral or intravenous corticosteroids at various doses is not known. As a mode of intraocular drug delivery, systemic administration is inefcient for delivering corticosteroids intraocularly; more drug is delivered to the rest of the body than to the eye. The intravitreous dexamethasone concentration following 7.5 mg orally was signicantly less than serum levels when studied in humans.73 Another report described serum drug levels to be greater than vitreous levels by 10-fold or more following systemic administration.128 A 1960 study in rabbits found that aqueous prednisolone levels were lower after IV administration than after topical delivery.129 Further proof of this nding using HPLC technology would be of great clinical value. The principal reservation to corticosteroid use by any route, and particularly by systemic administration, is systemic toxicity. Osteopenia, diabetes mellitus, cushingoid body habitus, adrenal suppression, hypertension, cutaneous tissue atrophy, gastrointestinal irritation, and emotional changes are only a few of the very numerous and well-described toxic effects of corticosteroid use. The risk of adverse effects increases with the duration of therapy as well as the corticosteroid dose, and these effects are occasionally difcult to reverse.21 The toxicity of systemic corticosteroid therapy has been extensively described, including in the ophthalmologic literature.130 When ocular inammation is a manifestation of an overt systemic process, systemic corticosteroids play a major therapeutic role in inammatory diseases of the eye and constitute an important component of the ophthalmologists armamentarium. For patients whose ocular inammation does not appear related to systemic disease, modes of administration that minimize systemic delivery and hence systemic side effects while maximizing ocular delivery are probably most desirable, assuming that such local therapy controls the ocular inammation. Bilateral periocular injection is an alternative to systemic administration in these cases, although the potential hazards and riskbenet ratio need be considered and addressed with patients. Conclusions regarding systemic corticosteroid therapy Oral and intravenous corticosteroid therapy is used by many practitioners to treat severe and bilateral intraocular inammation. This mode of administration results in signicant intraocular corticosteroid levels within hours, but also delivers relatively less drug to the eye and more to the rest of the body than does local therapy. It is not known to what extent 184 P.A. Gaudio
systemically administered corticosteroids must enter the eye to be effective in controlling intraocular inammation. Systemic toxicity is a serious concern in all patients receiving this therapy. It is not known whether systemic administration is safer or more effective than periocular corticosteroid injections in patients whose ocular inammation is associated with an overt systemic inammatory process. summary Corticosteroids used to treat intraocular inammation can be administered as eyedrops, by periocular injection, by intravitreous injection, and systemically by mouth or intravenously. The most potent and commonly used corticosteroid eyedrops are prednisolone and dexamethasone formulations, with preferences for any particular formulation being largely a matter of convention and experience; clinicians impressions are conicting and published data do not support using any one preparation over the others. Periocular injections can be given in the subconjunctival space, beneath Tenons capsule via the superotemporal approach, alongside the globe inferiorly via a transcutaneous (orbital oor) injection, or in the retrobulbar space. Studies in humans suggest that subconjunctival dexamethasone injections deliver more drug into the vitreous and less to the rest of the body than inferior transcutaneous or systemic delivery, but the relative efcacies of each approach for treating intraocular inammation have not been evaluated. The precise mechanism by which locally injected corticosteroids enter the eye are not known. Intravitreous corticosteroid delivery via injection or implants is a relatively new therapy that has not been systematically evaluated and, although preliminary clinical impressions are encouraging, long-term follow-up relating to its use is lacking. Systemic corticosteroid therapy is most commonly used for severe and bilateral intraocular inammation, as well as for inammation occurring concomitantly with a systemic inammatory process. Side effects of corticosteroids by any route are a problem requiring close monitoring, especially when systemic administration is used on a chronic basis.
References
1 Bailey JM. Biochemistry and pharmacology of cyclooxygenase inhibitors. Bull NY Acad Med. 1989; 65:515. 2 Talar-Williams C, Sneller MC. Complications of corticosteroid therapy. Eur Arch Otorhinolaryngol. 1994;251:131136. 3 Carnahan MC, Goldstein DA. Ocular complications of topical, peri-ocular, and systemic corticosteroids. Curr Opin Ophthalmol. 2000;11:478483. 4 Hugues FC, Le Jeunne C. Systemic and local tolerability of ophthalmic drug formulations. An update. Drug Saf. 1993;8:365380.
5 McGhee CN, Dean S, DaneshMeyer H. Locally administered ocular corticosteroids: benets and risks. Drug Saf. 2002;25:3355. 6 Kara-Jose N, Lorenzetti DW, McAuliffe R, Conti T. Time response effects of corticosteroids on corneal wound healing. Can J Ophthalmol. 1972;7:4851. 7 McCarey BE, Napalkov JA, Pippen PA, Koester JM, al Reaves T. Corneal wound healing strength with topical antiinammatory drugs. Cornea. 1995;14:290294. 8 Ho PC, Elliott JH. Kinetics of corneal epithelial regeneration. II. Epidermal growth factor and topical corticosteroids.
Evidence based corticosteroid use
185
10
11
12
13
14
15
16
17
18
19
20
Invest Ophthalmol. 1975;14:630 633. Petroutsos G, Guimaraes R, Giraud JP, Pouliquen Y. Corticosteroids and corneal epithelial wound healing. Br J Ophthalmol. 1982;66:705708. Singh G. Corticosteroids in corneal endothelial wound healing. Ann Ophthalmol. 1985;17:238243. Wakakura M, Ishikawa S. Central serous chorioretinopathy complicating systemic corticosteroid treatment. Br J Ophthalmol. 1984;68:329331. Martins JC, Wilensky JT, Asseff CF, Obstbaum SA, Buerk KM. Corticosteroid-induced uveitis. Am J Ophthalmol. 1974;77:433437. Krupin T, LeBlanc RP, Becker B, Kolker AE, Podos SM. Uveitis in association with topically administered corticosteroid. Am J Ophthalmol. 1970;70:883885 Newsome DA, Wong VG, Cameron TP, Anderson RR. Steroid-induced mydriasis and ptosis. Invest Ophthalmol. 1971;10:424429. Armaly MF. Dexamethasone ocular hypertension in the clinically normal eye. II. The untreated eye, outow facility, and concentration. Arch Ophthalmol. 1966;75:776782. Armaly MF, Becker B. Intraocular pressure response to topical corticosteroids. Fed Proc. 1965;24: 12741278. Donshik PC, Cavanaugh HD, Boruchoff SA, Dohlman CH. Posterior subcapsular cataracts induced by topical corticosteroids following keratoplasty for keratoconus. Ann Ophthalmol. 1981;13:2932. McGhee CN. Pharmacokinetics of ophthalmic corticosteroids. Br J Ophthalmol. 1992;76:681684. Vitale AM, Foster CS. Corticosteroids. In: Foster CS, Vitale AM, editors. Diagnosis and treatment of uveitis. Philadelphia: Harcourt, 2002; 142158. Benet LZ, Mitchell JR, Sheiner LB. Pharmacokinetics: the dynamics of drug absorption, distribution and elimination. In: Goodman Gilman
21
22
23
24
25
26
27
28
A, Rall TW, Nies AS, Taylor P, editors. Goodman Gilmans The pharmacological basis of therapeutics. 3rd ed. New York: Pergamon Press, 1990; 332. Haynes Jr RC. Adrenocorticotropic hormone; adrenocortical steroids and their synthetic analogs; inhibitors of their synthesis and actions of adrenocortical hormones. In: Goodman Gilman A, Rall TW, Nies AS, Taylor P, editors. Goodman Gilmans The pharmacological basis of therapeutics. 3rd ed. New York: Pergamon Press, 1990; 14311462. Worakul N, Unlu N, Robinson JR. Ocular pharmacokinetics. In: Abelson MB, Neufeld AH, Albert DM, Jakobiec FA, Azar DT, Gragoudas ES, editors. Principles and practice of ophthalmology. 2nd ed. Philadelphia: W.B. Saunders, 2000; 202211. Reddy IK, Ganesan MG. Ocular therapeutics and drug delivery: an overview. In: Reddy IK, editor. Ocular therapeutics and drug delivery: a multi-disciplinary approach. Lancaster, PA: Technomic, 1996; 329. Lee V-HL, Robinso JR. Topical ocular drug delivery: recent developments and future challenges. J Ocular Pharmacol. 1986;2:67108. Watsky MA, Jablonski M, Edelhauser HG. Comparison of conjunctival and corneal surface areas in rabbit and human. Curr Eye Res. 1988;7:483486. Cox WV, Kupferman A, Leibowitz HM. Topically applied steroids in corneal disease. I. The role of inammation in stromal absorption of dexamethasone. Arch Ophthalmol. 1972;88:308313. Leibowitz HM, Kupferman A. Bioavailability and therapeutic effectiveness of topically administered corticosteroids. Trans Am Acad Ophthalmol Otolaryngol. 1974;79:7880. Krupin T, Waltman ST, Becker B. Ocular penetration in rabbits of topically applied dexamethasone.
186
P.A. Gaudio
29
30
31
32
33
34
35
36
37
38
Arch Ophthalmol. 1974;92:312 314. Bodker FS, Ticho BH, Feist RM, Lam TT. Intraocular dexamethasone penetration via subconjunctival or retrobulbar injections in rabbits. Ophthalmic Surg. 1993;24:453457. Musson DG, Bidgood AM, Olejnik O. Assay methodology for prednisolone, prednisolone acetate and prednisolone sodium phosphate in rabbit aqueous humor and ocular physiological solutions. J Chromatogr. 1991;565:89102. Frey BM, Frey FJ. Clinical pharmacokinetics of prednisone and prednisolone. Clin Pharmacokinet. 1990;19:126146. Musson DG, Bidgood AM, Olejnik O. An in vitro comparison of the permeability of prednisolone, prednisolone sodium phosphate, and prednisolone acetate across the NZW rabbit cornea. J Ocular Pharmacol. 1992;8:139150. Smith RE, Nozik RA. Uveitis: a clinical approach to diagnosis and management. 2nd ed. Baltimore: Williams and Wilkins, 1989. Nussenblatt RB, Whitcup SM, Palestine AG. Uveitis: fundamentals and clinical practice. 2nd ed. St. Louis: Mosby, 1996. Cox WV, Kupferman A, Leibowitz HM. Topically applied steroids in corneal disease. II. The role of drug vehicle in stromal absorption of dexamethasone. Arch Ophthalmol. 1972;88:549552. Kupferman A, Pratt MV, Suckewer K, Leibowitz HM. Topically applied steroids in corneal disease. 3. The role of drug derivative in stromal absorption of dexamethasone. Arch Ophthalmol. 1974;91:373376. Kupferman A, Leibowitz HM. Topically applied steroids in corneal disease. IV. The role of drug concentration in stromal absorption of prednisolone acetate. Arch Ophthalmol. 1974;91:377380. Kupferman A, Leibowitz HM. Topically applied steroids in corneal disease. V. Dexamethasone alcohol.
39
40
41
42
43
44
45
46
47
48
Arch Ophthalmol. 1974;92:329 330. Kupferman A, Leibowitz HM. Topically applied steroids in corneal disease. VI. Kinetics of prednisolone sodium phosphate. Arch Ophthalmol. 1974;92:331334. Musson DG, Bidgood AM, Olejnik O. Comparative corneal penetration of prednisolone sodium phosphate and prednisolone acetate in NZW rabbits. J Ocular Pharmacol. 1991;7: 175182. Kupferman A, Leibowitz HM. Penetration of uorometholone into the cornea and aqueous humor. Arch Ophthalmol. 1975;93: 425427. Kupferman A, Berrospi AR, Leibowitz HM. Fluorometholone acetate. A new ophthalmic derivative of uorometholone. Arch Ophthalmol. 1982;100:640641. Yamauchi H, Kito H. Studies on intraocular penetration and metabolism of uorometholone in rabbits: a comparison between dexamethasone and prednisolone acetate. Jpn J Ophthalmol. 1975;19: 339347. Olejnik O, Weisbecker CA. Ocular bioavailability of topical prednisolone preparations. Clin Ther. 1990;12:211. Leibowitz HM, Kupferman A. Antiinammatory effectiveness in the cornea of topically administered prednisolone. Invest Ophthalmol. 1974;13:757763. Leibowitz HM, Kupferman A. Kinetics of topically administered prednisolone acetate. Optimal concentration for treatment of inammatory keratitis. Arch Ophthalmol. 1976;94:13871389. Schoenwald RD, Boltralik JJ. A bioavailability comparison in rabbits of two steroids formulated as high-viscosity gels and reference aqueous preparations. Invest Ophthalmol Vis Sci. 1979;18:6166. Kupferman A, Ryan WJ, Leibowitz HM. Prolongation of antiinammatory effect of prednisolone acetate. Inuence of formulation in
Evidence based corticosteroid use
187
49
50
51
52
53
54
55
56
57
58
59
high-viscosity gel. Arch Ophthalmol. 1981;99:20282029. Schoenwald RD, Steward P. Effect of particle size on ophthalmic bioavailability of dexamethasone suspensions in rabbits. J Pharm Sci. 1980;69:391394. Bisrat M, Glazer M. Effect of particle size on ocular permeability of prednisolone acetate in rabbits. Acta Pharmacol Nord. 1992;4:5. Leibowitz HM, Kupferman A. Optimal frequency of topical prednisolone administration. Arch Ophthalmol. 1979;97:2154 2156. Fiscella RG, Jensen M, Van Dyck G. Generic prednisolone suspension substitution. Arch Ophthalmol. 1998;116:703. Burch PG, Migeon CJ. Systemic absorption of topical steroids. Arch Ophthalmol. 1968;79:174176. Krupin T, Mandell AI, Podos SM, Becker B. Topical corticosteroid therapy and pituitary-adrenal function. Arch Ophthalmol. 1976;94: 919920. Romano PE, Traisman HS, Green OC. Fluorinated corticosteroid toxicity in infants. Am J Ophthalmol. 1977;84:247250. Ozerdem U, Levi L, Cheng L, Song MK, Scher C, Freeman WR. Systemic toxicity of topical and periocular corticosteroid therapy in an 11-year-old male with posterior uveitis. Am J Ophthalmol. 2000;130: 240241. McGhee CN, Noble MJ, Watson DG, Dutton GN, Fern AI, Healey TM, Midgley JM. Penetration of topically applied prednisolone sodium phosphate into human aqueous humour. Eye. 1989;3:463 467. McGhee CN, Watson DG, Midgley JM, Noble MJ, Dutton GN, Fern AI. Penetration of synthetic corticosteroids into human aqueous humour. Eye. 1990;4:526530. Watson DG, McGhee CN, Midgley JM, Dutton GN, Noble MJ. Penetration of topically applied betamethasone sodium phosphate
60
61
62
63
64
65
66
67
68
into human aqueous humour. Eye. 1990;4:603606. Watson DG, Midgley JM, McGhee CN. The analysis of corticosteroid acetates by gas chromatography/ negative ion chemical ionization mass spectrometry. Rapid Commun Mass Spectrom. 1989;3:810. Burde RM, Waltman SR. Topical corticosteroids after cataract surgery. Ann Ophthalmol. 1972;4: 290293. Mustakallio A, Kaufman HE, Johnston G, Wilson RS, Roberts MD, Harter JC. Corticosteroid efcacy in postoperative uveitis. Ann Ophthalmol. 1973;5:719730. Corboy JM. Corticosteroid therapy for the reduction of postoperative inammation after cataract extraction. Am J Ophthalmol. 1976; 82:923927. Dunne JA, Travers JP. Double-blind clinical trial of topical steroids in anterior uveitis. Br J Ophthalmol. 1979;63:762767. Ramsell TG, Bartholomew RS, Walker SR. Clinical evaluation of clobetasone butyrate: a comparative study of its effects in postoperative inammation and on intraocular pressure. Br J Ophthalmol. 1980;64: 4345. Stewart R, Horwitz B, Howes J, Novack GD, Hart K. Doublemasked, placebo-controlled evaluation of loteprednol etabonate 0.5% for postoperative inammation. Loteprednol Etabonate Post-operative Inammation Study Group 1. J Cataract Refract Surg. 1998;24: 14801489. Anonymous. Controlled evaluation of loteprednol etabonate and prednisolone acetate in the treatment of acute anterior uveitis. Loteprednol Etabonate US Uveitis Study Group. Am J Ophthalmol. 1999;127:537544. Foster CS, Alter G, DeBarge LR, Raizman MB, Crabb JL, Santos CI, Feiler LS, Friedlaender MH. Efcacy and safety of rimexolone 1% ophthalmic suspension vs 1%
188
P.A. Gaudio
69
70
71
72
73
74
75
76
77
prednisolone acetate in the treatment of uveitis. Am J Ophthalmol. 1996;122:171182. Whitcup SM, Ferris 3rd FL. New corticosteroids for the treatment of ocular inammation. Am J Ophthalmol. 1999;127:597599. Elliot AJ. Recurrent intraocular hemorrhage in young adults (Eales disease). Arch Ophthalmol. 1959;61: 745754. Nozik RA. Periocular injection of steroids. Trans Am Acad Ophthalmol Otolaryngol. 1972;76: 694703. Hyndiuk RA. Radioactive depotcorticosteroid penetration into monkey ocular tissue. II. Subconjunctival administration. Arch Ophthalmol. 1969;82:259 263. Weijtens O, Schoemaker RC, Cohen AF, Romijn FP, Lentjes EG, van Rooij J, van Meurs JC. Dexamethasone concentration in vitreous and serum after oral administration. Am J Ophthalmol. 1998;125:673679. Weijtens O, Feron EJ, Schoemaker RC, Cohen AF, Lentjes EG, Romijn FP, van Meurs JC. High concentration of dexamethasone in aqueous and vitreous after subconjunctival injection. Am J Ophthalmol. 1999;128:192197. Weijtens O, van der Sluijs FA, Schoemaker RC, Lentjes EG, Cohen AF, Romijn FP, van Meurs JC. Peribulbar corticosteroid injection: vitreal and serum concentrations after dexamethasone disodium phosphate injection. Am J Ophthalmol. 1997;123:358363. Weijtens O, Schoemaker RC, Lentjes EG, Romijn FP, Cohen AF, van Meurs JC. Dexamethasone concentration in the subretinal uid after a subconjunctival injection, a peribulbar injection, or an oral dose. Ophthalmology. 2000;107: 19321938. Kunou N, Ogura Y, Honda Y, Hyon SH, Ikada Y. Biodegradable scleral implant for controlled intraocular delivery of betamethasone
78
79
80
81
82
83
84
85
86
87
88
phosphate. J Biomed Mater Res. 2000;51:635641. McCartney HJ, Drysdale IO, Gornall AG, Basu PK. An autoradiographic study of the penetration of subconjunctivally injected hydrocortisone into the normal and inamed rabbit eye. Invest Ophthalmol. 1965;76:297302. Wine NA, Gornall AG, Basu PK. The ocular uptake of subconjunctivally injected C14 hydrocortisone. Am J Ophthalmol. 1964;58:362366. Hakin KN, Ham J, Lightman SL. Use of orbital oor steroids in the management of patients with uniocular non-necrotising scleritis. Br J Ophthalmol. 1991;75:337339. Gebertt S. Depotmethylprednisolone for subconjunctival and retrobulbar injection. Lancet. 1961;2:344345. Rodger FC. Repository corticotherapy in ophthalmic theory and practice. Br J Ophthalmol. 1965;49:298306. Schlaegel Jr TF, Weber JC. Treatment of pars planitis. II. Corticosteroids. Surv Ophthalmol. 1977;22:120,125130. Riordan-Eva P, Lightman S. Orbital oor steroid injections in the treatment of uveitis. Eye. 1994;8: 6669. Lightman S. Use of steroids and immunosuppressive drugs in the management of posterior uveitis. Eye. 1991;5:294298. Tanner V, Kanski JJ, Frith PA. Posterior sub-Tenons triamcinolone injections in the treatment of uveitis. Eye. 1998;12:679685. Walton RC, Vick VL, Greenwald MA. Sub-tenons corticosteroids for the treatment of macular edema in bone marrow transplant retinopathy. Retina. 1999;19: 171173. Helm CJ, Holland GN. The effects of posterior subtenon injection of triamcinolone acetonide in patients with intermediate uveitis. Am J Ophthalmol. 1995;120:55 64.
Evidence based corticosteroid use
189
89 Sajnani D. Posterior sub-Tenons triamcinolone injections in the treatment of uveitis. Eye. 1999;13: 703704. 90 Kalina PH, Erie JC, Rosenbaum L. Biochemical quantication of triamcinolone in subconjunctival depots. Arch Ophthalmol. 1995;113: 867869. 91 Francis BA, Chang EL, Haik BG. Particle size and drug interactions of injectable corticosteroids used in ophthalmic practice. Ophthalmology. 1996;103:1884 1888. 92 Hyndiuk RA, Reagan MG. Radioactive depot-corticosteroid penetration into monkey ocular tissue. I. Retrobulbar and systemic administration. Arch Ophthalmol. 1968;80:499503. 93 Levine ND, Aronson SB. Orbital infusion of steroids in the rabbit. Arch Ophthalmol. 1970;83:599607. 94 Jennings T, Rusin MM, Tessler HH, Cunha-vaz JG. Posterior subtenons injections of corticosteroids in uveitis patients with cystoid macular edema. Jpn J Ophthalmol. 1988;32:385391. 95 Thach AB, Dugel PU, Flindall RJ, Sipperley JO, Sneed SR. A comparison of retrobulbar versus sub-tenons corticosteroid therapy for cystoid macular edema refractory to topical medications. Ophthalmology. 1997;104:2003 2008. 96 Freeman WR, Green RI, Smith RE. Echographic localization of corticosteroids after periocular injection. Am J Ophthalmol. 1987; 103:281288. 97 Olsen TW, Edelhauser HF, Lim JI, Geroski DH. Human scleral permeability: effects of age, cryotherapy, transscleral diode laser, and surgical thinning. Invest Ophthalmol Vis Sci. 1995;36:1893 1903. 98 Morgan CM, Schatz H, Vine AK, Cantrill HL, Davidorf FH, Gitter KA, Rudich R. Ocular complications associated with retrobulbar injections.
99
100
101
102
103
104
105
106
107
Ophthalmology. 1988;95:660 665. Jaffe GJ, Yang CH, Guo H, Denny JP, Lima C, Ashton P. Safety and pharmacokinetics of an intraocular uocinolone acetonide sustained delivery device. Invest Ophthalmol Vis Sci. 2000;41:35693575. Herschler J. Increased intraocular pressure induced by repository corticosteroids. Am J Ophthalmol. 1976;82:9093. Levin DS, Han DP, Dev S, Wirostko WJ, Mieler WF, Connor TB, George V, Eastwood D. Subtenons depot corticosteroid injections in patients with a history of corticosteroidinduced intraocular pressure elevation. Am J Ophthalmol. 2002; 133:196202. Mueller AJ, Jian G, Banker AS, Rahhal FM, Capparelli E, Freeman WR. The effect of deep posterior subtenon injection of corticosteroids on intraocular pressure. Am J Ophthalmol. 1998; 125:158163. Peyman GA, Herbst R. Bacterial endophthalmitis. Treatment with intraocular injection of gentamicin and dexamethasone. Arch Ophthalmol. 1974;91:416418. Graham RO, Peyman GA. Intravitreal injection of dexamethasone. Treatment of experimentally induced endophthalmitis. Arch Ophthalmol. 1974;92:149154. Maxwell Jr DP, Brent BD, Diamond JG, Wu L. Effect of intravitreal dexamethasone on ocular histopathology in a rabbit model of endophthalmitis [see comments]. Ophthalmology. 1991;98:13701375. Das T, Jalali S, Gothwal VK, Sharma S, Naduvilath TJ. Intravitreal dexamethasone in exogenous bacterial endophthalmitis: results of a prospective randomised study. Br J Ophthalmol. 1999;82:10501055. Shah GK, Stein JD, Sharma S, Sivalingam A, Benson WE, Regillo CD, Brown GC, Tasman W. Visual outcomes following the use of
190
P.A. Gaudio
108
109
110
111
112
113
114
115
intravitreal steroids in the treatment of postoperative endophthalmitis. Ophthalmology. 2000;107:486489. Majji AB, Jalali S, Das T, Gopinathan U. Role of intravitreal dexamethasone in exogenous fungal endophthalmitis. Eye. 1999;13:660 665. Anonymous. Results of the Endophthalmitis Vitrectomy Study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Endophthalmitis Vitrectomy Study Group [see comments]. Arch Ophthalmol. 1995; 113:14791496. Benitez Del Castillo Sanchez JM, Garcia Sanchez J. [Intravitreal injection of triamcinolone acetonide in non infectious uveitis]. Arch Soc Esp Oftalmol. 2001;76:661664. Jaffe GJ, Ben-Nun J, Guo H, Dunn JP, Ashton P. Fluocinolone acetonide sustained drug delivery device to treat severe uveitis. Ophthalmology. 2000;107:2024 2033. Tan DT, Chee SP, Lim L, Theng J, Van Ede M. Randomized clinical trial of Surodex steroid drug delivery system for cataract surgery: anterior versus posterior placement of two Surodex in the eye. Ophthalmology. 2001;108:2172 2181. Tan DT, Chee SP, Lim L, Lim AS. Randomized clinical trial of a new dexamethasone delivery system (Surodex) for treatment of postcataract surgery inammation. Ophthalmology. 1999;106:223231. Chang DF, Wong V. Two clinical trials of an intraocular steroid delivery system for cataract surgery. Trans Am Ophthalmol Soc. 1999;97:261274 discussion 274279. Jaffe GJ, Pearson PA, Ashton P. Dexamethasone sustained drug delivery implant for the treatment of severe uveitis. Retina. 2000;20: 402403.
116 Hida T, Chandler D, Arena JE, Machemer R. Experimental and clinical observations of the intraocular toxicity of commercial corticosteroid preparations. Am J Ophthalmol. 1986;101:190195. 117 Young S, Larkin G, Branley M, Lightman S. Safety and efcacy of intravitreal triamcinolone for cystoid macular oedema in uveitis. Clin Exp Ophthalmol. 2001;29: 26. 118 Antcliff RJ, Spalton DJ, Stanford MR, Graham EM, ffytche TJ, Marshall J. Intravitreal triamcinolone for uveitic cystoid macular edema: an optical coherence tomography study. Ophthalmology. 2001;108:765772. 119 Martidis A, Duker JS, Puliato CA. Intravitreal triamcinolone for refractory cystoid macular edema secondary to birdshot retinochoroidopathy. Arch Ophthalmol. 2001;119:13801383. 120 Schindler RH, Chandler D, Thresher R, Machemer R. The clearance of intravitreal triamcinolone acetonide. Am J Ophthalmol. 1982;93:415417. 121 Kwak HW, DAmico DJ. Evaluation of the retinal toxicity and pharmacokinetics of dexamethasone after intravitreal injection [see comments]. Arch Ophthalmol. 1992;110:259266. 122 Woods AC. Clinical and experimental observations on the use of ACTH and cortisone in ocular inammatory disease. Am J Ophthalmol. 1950;33:13251149. 123 Gordon DM. Prednisone and prednisolone in ocular disease. Am J Ophthalmol. 1956;41:593600. 124 Solomon SD, Cunningham ET Jr. Use of corticosteroids and noncorticosteroid immunosuppressive agents in patients with uveitis. Compr Ophthalmol Update. 2000;1: 273286. 125 Wakeeld D, McCluskey P, Penny R. Intravenous pulse methylprednisolone therapy in severe inammatory eye disease.
Evidence based corticosteroid use
191
Arch Ophthalmol. 1986;104:847 851. 126 McCluskey P, Wakeeld D. Intravenous pulse methylprednisolone in scleritis. Arch Ophthalmol. 1987;105: 793797. 127 Hill JC, Maske R, Watson PG. The use of a single pulse of intravenous methylprednisolone in the treatment of corneal graft rejection: a preliminary report. Eye. 1991;5: 420424. 128 Behar-Cohen FF, Gauthier S, El Aouni A, Chapon P, Parel JM,
Renard G, Chauvaud D. Methylprednisolone concentrations in the vitreous and the serum after pulse therapy. Retina. 2001;21: 4853. 129 Kroman HS, Leopold IL. Studies upon methyl- and uorosubstituted prednisolones in the aqueous humor of rabbit. Am J Ophthalmol. 1960;52:7781. 130 Stanbury R, Graham E. Systemic corticosteroid therapy: side effects and their management. Br J Ophthalmol. 1998;82:704 708.
192
P.A. Gaudio
You might also like
- Ravi KananiDocument15 pagesRavi Kananikanani raviNo ratings yet
- Ricinoleic Acid PLO Gel for Eyelid DeliveryDocument4 pagesRicinoleic Acid PLO Gel for Eyelid DeliverySai HS BodduNo ratings yet
- International Journal of Innovative Pharmaceutical Research: Ophthalmic Delivery System For Dexamethasone: An OverviewDocument5 pagesInternational Journal of Innovative Pharmaceutical Research: Ophthalmic Delivery System For Dexamethasone: An OverviewGufron MustofaNo ratings yet
- Jurnal Tetes MataDocument6 pagesJurnal Tetes MataSyafiraNo ratings yet
- Solubility of Budesonide, Hydrocortisone, and Prednisolone in Ethanol + Water Mixtures at 298.2 KDocument90 pagesSolubility of Budesonide, Hydrocortisone, and Prednisolone in Ethanol + Water Mixtures at 298.2 KsekahaNo ratings yet
- 21 Doxofylline PDFDocument10 pages21 Doxofylline PDFBaru Chandrasekhar RaoNo ratings yet
- DWDWQDocument10 pagesDWDWQprinceamitNo ratings yet
- 2014 Article 21Document10 pages2014 Article 21SusPa NarahaNo ratings yet
- Vol 2 - Cont. J. Pharm SciDocument48 pagesVol 2 - Cont. J. Pharm Sciwilolud9822No ratings yet
- Formulation and Evaluation of New Long Acting Metoprolol Tartrate Ophthalmic GelsDocument9 pagesFormulation and Evaluation of New Long Acting Metoprolol Tartrate Ophthalmic GelsmelyNo ratings yet
- Injeksi KonjungtivaDocument24 pagesInjeksi KonjungtivataufikNo ratings yet
- AtenololDocument21 pagesAtenololAbdul QadirNo ratings yet
- Development and in Vitro Characterization of Nanoemulsion Embedded Thermosensitive In-Situ Ocular Gel of Diclofenac Sodium For Sustained DeliveryDocument14 pagesDevelopment and in Vitro Characterization of Nanoemulsion Embedded Thermosensitive In-Situ Ocular Gel of Diclofenac Sodium For Sustained DeliveryVeaux NouNo ratings yet
- Pharmacokinetics: of OphthalmicDocument4 pagesPharmacokinetics: of OphthalmicWina Siska Purnama BurmanNo ratings yet
- 8 CF 3Document10 pages8 CF 3nelisaNo ratings yet
- 1438 PDFDocument8 pages1438 PDFEndungNo ratings yet
- Myarticle IRJP DSRTDocument13 pagesMyarticle IRJP DSRTWendy FernandezNo ratings yet
- Dissolution Enhancement and Formulation of Film CoDocument12 pagesDissolution Enhancement and Formulation of Film CobimaNo ratings yet
- (216 235) V10N5CTDocument20 pages(216 235) V10N5CTgritty gallantNo ratings yet
- Naproxen Patch TransdermalDocument9 pagesNaproxen Patch Transdermalnurhayati novitaNo ratings yet
- Formulation and Evaluation of Itraconazole Opthalmic in Situ GelsDocument8 pagesFormulation and Evaluation of Itraconazole Opthalmic in Situ GelsiajpsNo ratings yet
- Journal of Pharmaceutical Sciences: Pharmaceutics, Drug Delivery and Pharmaceutical TechnologyDocument8 pagesJournal of Pharmaceutical Sciences: Pharmaceutics, Drug Delivery and Pharmaceutical TechnologyDwiPutriAuliyaRachmanNo ratings yet
- Jurnal Pefloxacin2Document15 pagesJurnal Pefloxacin2Novitra DewiNo ratings yet
- Sajp2 (4) 315 318Document4 pagesSajp2 (4) 315 318Habibur RahmanNo ratings yet
- Intravitreal Dexamethasone Reduces Inflammation in Bacterial EndophthalmitisDocument7 pagesIntravitreal Dexamethasone Reduces Inflammation in Bacterial EndophthalmitisxoxotheNo ratings yet
- 35065-Article Text-168446-1-10-20191115Document8 pages35065-Article Text-168446-1-10-20191115Muhammad Iqbal AlgifariNo ratings yet
- The Effect of An Artificial Tear Combining Hyaluronic Acid and Tamarind Seeds Polysaccharide in Patients With Moderate Dry Eye Syndrome: A New Treatment For Dry EyeDocument6 pagesThe Effect of An Artificial Tear Combining Hyaluronic Acid and Tamarind Seeds Polysaccharide in Patients With Moderate Dry Eye Syndrome: A New Treatment For Dry EyeMathieu VigneauNo ratings yet
- 10 1002@ddr 21677Document12 pages10 1002@ddr 21677MuhammadRomadonSyolehhudinNo ratings yet
- Ashraf 2018Document50 pagesAshraf 2018Alyna AlynaNo ratings yet
- Review: Intravitreal Corticosteroids in Diabetic Macular Edema Pharmacokinetic ConsiderationsDocument10 pagesReview: Intravitreal Corticosteroids in Diabetic Macular Edema Pharmacokinetic ConsiderationsNindhya PutriNo ratings yet
- Formulation and Evaluation of Nanoemulsion For Solubility Enhancement of KetoconazoleDocument14 pagesFormulation and Evaluation of Nanoemulsion For Solubility Enhancement of KetoconazoledgdNo ratings yet
- Update On Steroid-Induced Glaucoma: A Review of The Literature and Tips On Managing PatientsDocument3 pagesUpdate On Steroid-Induced Glaucoma: A Review of The Literature and Tips On Managing PatientsagungNo ratings yet
- Formulation and Evaluation of Transdermal Patch of AceclofenacDocument11 pagesFormulation and Evaluation of Transdermal Patch of AceclofenacMuhammad ArmandsyahgzNo ratings yet
- Published ArticleDocument15 pagesPublished ArticleOktavia Rahayu ANo ratings yet
- Na DastinibDocument20 pagesNa DastinibPradheep SNo ratings yet
- Formulation Development and Evaluation of Mouth Dissolving Tablet of ThiocolchicosideDocument18 pagesFormulation Development and Evaluation of Mouth Dissolving Tablet of ThiocolchicosideEditor IJTSRDNo ratings yet
- Research Paper On Nasal Drug Delivery SystemDocument7 pagesResearch Paper On Nasal Drug Delivery Systemgosuzinifet2100% (1)
- 2007 Article 9024Document7 pages2007 Article 9024Theva CharaanNo ratings yet
- Quatittauf EtoricoxidDocument9 pagesQuatittauf EtoricoxidSulistia Nur UtamiNo ratings yet
- Buccal Films ThesisDocument8 pagesBuccal Films Thesistsfublhld100% (2)
- Ocular Ketoconazole Loaded Proniosomal Gels Formulation Ex Vivo Corneal Permeation and in Vivo StudiesDocument12 pagesOcular Ketoconazole Loaded Proniosomal Gels Formulation Ex Vivo Corneal Permeation and in Vivo StudiesManik RahayuniNo ratings yet
- In Vitro and in Vivo Evaluation of Ketotifen Fumarate-Loaded Silicone Hydrogel Contact Lenses For Ocular Drug DeliveryDocument10 pagesIn Vitro and in Vivo Evaluation of Ketotifen Fumarate-Loaded Silicone Hydrogel Contact Lenses For Ocular Drug DeliveryArif_iiucNo ratings yet
- Development of Fast Dissolving Oral Film ContaininDocument14 pagesDevelopment of Fast Dissolving Oral Film ContaininLina WinartiNo ratings yet
- Formulation and Evaluation of Vanishing Herbal Cream of Crude DrugsDocument14 pagesFormulation and Evaluation of Vanishing Herbal Cream of Crude DrugsiajpsNo ratings yet
- Formulation and Evaluation of Sustained Release Matrix Tablets ThesisDocument7 pagesFormulation and Evaluation of Sustained Release Matrix Tablets Thesisnicoledixonmobile100% (1)
- Konstas AG Et Al 24-Hour Efficacy of Travoprost - Timolol BAK-free Versus Latanoprost - TimololDocument13 pagesKonstas AG Et Al 24-Hour Efficacy of Travoprost - Timolol BAK-free Versus Latanoprost - TimololAdriana FallaNo ratings yet
- Buccal Film Thesis PDFDocument7 pagesBuccal Film Thesis PDFafiwiafoc100% (2)
- Latanoprostpaper 2014Document13 pagesLatanoprostpaper 2014ahmed.bouchenakNo ratings yet
- FirstarticleDocument10 pagesFirstarticleAdhi PermanaNo ratings yet
- Potential Use of Niosomal Hydrogel As An Ocular Delivery System For AtenololDocument11 pagesPotential Use of Niosomal Hydrogel As An Ocular Delivery System For AtenololDrAmit VermaNo ratings yet
- 10.1515 - Nanofab 2020 0105Document9 pages10.1515 - Nanofab 2020 0105SHAHIQNo ratings yet
- Wang 2014Document9 pagesWang 2014Fer RodriguezNo ratings yet
- Available Online Through: ISSN: 0975-766XDocument20 pagesAvailable Online Through: ISSN: 0975-766XnurulNo ratings yet
- Design, Development and in Vitro Evaluation of Transdermal Patches Containing Domperidone MaleateDocument8 pagesDesign, Development and in Vitro Evaluation of Transdermal Patches Containing Domperidone MaleateIrfan N KhanNo ratings yet
- Formulation and in Vitro Evaluation of Fesoterodine Fumarate Sustained Release TabletsDocument13 pagesFormulation and in Vitro Evaluation of Fesoterodine Fumarate Sustained Release TabletsBaru Chandrasekhar RaoNo ratings yet
- 51 Vol. 5 Issue 5 May 2014IJPSR RA 3450 Paper 51Document12 pages51 Vol. 5 Issue 5 May 2014IJPSR RA 3450 Paper 51yurlinzha ChyntiaTandipareNo ratings yet
- 16363797731583832601formulation and Evaluation of Ophthalmic Antibacterial Gels and Comparison of Different Polymers Using Factorial DesignDocument7 pages16363797731583832601formulation and Evaluation of Ophthalmic Antibacterial Gels and Comparison of Different Polymers Using Factorial Designazita nezamiNo ratings yet
- Formulation and Evaluation of Floating Tablet of Metoprolol SuccinateDocument13 pagesFormulation and Evaluation of Floating Tablet of Metoprolol SuccinateEditor IJTSRDNo ratings yet
- 6 Vol. 8 Issue 1 January 2017 IJPSR RA 6983Document10 pages6 Vol. 8 Issue 1 January 2017 IJPSR RA 6983vinayNo ratings yet
- Parenteral Products: The Preparation and Quality Control of Products for InjectionFrom EverandParenteral Products: The Preparation and Quality Control of Products for InjectionNo ratings yet
- Gastric and Duodenal Disorders - Test 4Document21 pagesGastric and Duodenal Disorders - Test 4Vickie BuckerNo ratings yet
- Tabel Interaksi Kolom BetonDocument10 pagesTabel Interaksi Kolom BetonEndoGutierrezNo ratings yet
- Managing The Myths of Health Care PDFDocument5 pagesManaging The Myths of Health Care PDFkaremNo ratings yet
- How To Lower Blood Pressure QuicklyDocument38 pagesHow To Lower Blood Pressure QuicklyKay OlokoNo ratings yet
- Sirenomelia: A Case Report of A Rare Congenital Anamaly and Review of LiteratureDocument3 pagesSirenomelia: A Case Report of A Rare Congenital Anamaly and Review of LiteratureInt Journal of Recent Surgical and Medical SciNo ratings yet
- Perbandingan Pengenceran Larutan Giemsa 3% Dan 5% Terhadap Pemeriksaan Morfologi PlasmodiumDocument9 pagesPerbandingan Pengenceran Larutan Giemsa 3% Dan 5% Terhadap Pemeriksaan Morfologi PlasmodiumMuti WahyuNo ratings yet
- The Clinical Toxicology of Sulfur Mustard: Review ArticleDocument18 pagesThe Clinical Toxicology of Sulfur Mustard: Review ArticleGiany GausNo ratings yet
- Public Notice Dated 16.11.2018-Disability-AppendixHDocument4 pagesPublic Notice Dated 16.11.2018-Disability-AppendixHDisability Rights AllianceNo ratings yet
- A Study of Demographic Variables of Violent Asphyxial Death: JPAFMAT, 2003, Vol.: 3 ISSN - 0972 - 5687Document4 pagesA Study of Demographic Variables of Violent Asphyxial Death: JPAFMAT, 2003, Vol.: 3 ISSN - 0972 - 5687Reza ArgoNo ratings yet
- Wound Management ProcedureDocument51 pagesWound Management ProcedureSisca Dwi AgustinaNo ratings yet
- Enriched Air Diver Knowledge ReviewDocument2 pagesEnriched Air Diver Knowledge Reviewgabriele belmonte100% (1)
- Recurrent Gingival Cyst of Adult: A Rare Case Report With Review of LiteratureDocument5 pagesRecurrent Gingival Cyst of Adult: A Rare Case Report With Review of Literaturesayantan karmakarNo ratings yet
- Understanding the Immunogenic Properties of VirusesDocument41 pagesUnderstanding the Immunogenic Properties of VirusesMaruf Raza DarubagiNo ratings yet
- Managing dental patients with cardiovascular diseasesDocument54 pagesManaging dental patients with cardiovascular diseasesSafiraMaulidaNo ratings yet
- John Paul PeraltaDocument5 pagesJohn Paul PeraltaAndrea Joyce AngelesNo ratings yet
- OB Meds WorksheetDocument18 pagesOB Meds WorksheetrickyandsheenaNo ratings yet
- B.A.,D.D.S.,M.S.D. : Herbert Werdlow, Bethesda, MDDocument7 pagesB.A.,D.D.S.,M.S.D. : Herbert Werdlow, Bethesda, MDMuchlis Fauzi ENo ratings yet
- Klinefelter SyndromeDocument6 pagesKlinefelter Syndromemeeeenon100% (1)
- Effectiveness of Planned Teaching Programme On The Knowledge of Endotracheal Suctioning Among Staff Nurses Working in IcuDocument6 pagesEffectiveness of Planned Teaching Programme On The Knowledge of Endotracheal Suctioning Among Staff Nurses Working in IcuRizwan KhanNo ratings yet
- Maharashtra Government PGM Admissions 2015-2016 Round 2 Selection ListDocument30 pagesMaharashtra Government PGM Admissions 2015-2016 Round 2 Selection ListAbhinav BhardwajNo ratings yet
- The Bite Stage. The Try-In Stage. The Fitting StageDocument4 pagesThe Bite Stage. The Try-In Stage. The Fitting StageStanislavNemtanuNo ratings yet
- Pearls in The Management of ExotropiaDocument4 pagesPearls in The Management of ExotropiaGuy BarnettNo ratings yet
- PHMB-Silver Sulfadiazine - HCDT-20-019Document7 pagesPHMB-Silver Sulfadiazine - HCDT-20-019gloriaNo ratings yet
- Cirugia BariatricaDocument9 pagesCirugia BariatricaedwardmenesesNo ratings yet
- How To Lower Your TriglyceridesDocument4 pagesHow To Lower Your TriglyceridesNoli CanlasNo ratings yet
- Tfios Mediastudyguide v4Document7 pagesTfios Mediastudyguide v4api-308995770No ratings yet
- Prismaflex CRRT Competency Based Tool PDFDocument5 pagesPrismaflex CRRT Competency Based Tool PDFalex100% (1)
- PHC Conference Agenda 6-13Document5 pagesPHC Conference Agenda 6-13OSUMCNo ratings yet
- Eosinophin in Infectious DiseaseDocument29 pagesEosinophin in Infectious DiseasentnquynhproNo ratings yet
- Significant Prognostic Impact of Improvement in VeDocument10 pagesSignificant Prognostic Impact of Improvement in VeFIA SlotNo ratings yet