Professional Documents
Culture Documents
Nursing Care Plan For Glaucoma
Uploaded by
Emiey RaraOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing Care Plan For Glaucoma
Uploaded by
Emiey RaraCopyright:
Available Formats
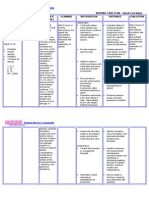
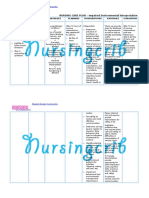
Nursing Care Plan for Glaucoma Nursing Assessment for Glaucoma 1.
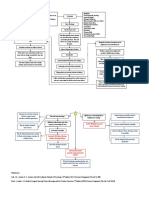
History or presence of risk factors : Positive family history (believed to be associated with primary open angle glaucoma). Tumors of the eye Hemorrhage intraocular Inflammatory intraocular uveiti) Eye contusion from trauma. Physical examination based on those in the general assessment of the eye may indicate: For primary open angle Reported a loss of peripheral vision slow (see tunnel) For primary angle closure : Incidence of sudden severe pain in the eye is often accompanied by headache, nausea and vomiting. Complaints halo light, blurred vision, and decreased light perception. The pupils are being fixed with redness due to inflammation of the sclera and cornea looks cloudy. Diagnostic Examination Tonometri used to measure intra-ocular pressure. Glaucoma is suspected when IOP greater than 22 mmHg. Gonioskopi possible to see directly the anterior chamber angle glaucoma to distinguish between closed and open-angle glaucoma. Optalmoskopi allow inspectors to see directly optic disc and internal eye structure. Assess the patient's understanding about the condition and emotional response to the condition and plan of action. Nursing Diagnosis and Nursing Interventions for Glaucoma Pain related to spasm, intra-ocular pressure, glaucoma acute. Which is characterized by :
o o o o o
2.
o o o
3.
o o o
4.
patients express pain in the eye, protect the side of the pain patients, frowned and whimpered. Goal : reduction of discomfort, said pain is gone / reduced, relaxed facial expression, no moaning. Intervention :
o o o o o
Monitor blood pressure, pulse, and respiration every 4 hours. Monitor the degree of eye pain every 30 minutes during the acute phase. Monitor input and output every 8 hours while receiving intravenous osmotic agent. Monitor visual acuity at any time before hatching ophthalmic agents. Give appropriate instructions optalmic agent for glaucoma. Inform your doctor if : hypotension urinary output of less than 240 ml / hour No loss of pain in the eye within 30 minutes of drug therapy Decrease in constant visual acuity. Prepare patients for surgery Maintain bed rest in semi-Fowler position. Prevent increase in IOP : Instruct to avoid coughing, sneezing, straining, or placing the head below the pelvic Provide quiet environment and avoid light. Give anlgetic prescription and evaluation of its effectiveness.
Complications:
Bacterial sinusitis is nearly always harmless (although uncomfortable and sometimes even very painful). If an episode becomes severe, antibiotics generally eliminate further problems. In rare cases, however, sinusitis can be very serious. Osteomyelitis. Adolescent males with acute frontal sinusitis are at particular risk for severe problems. One important complication is
infection of the bones (osteomyelitis) of the forehead and other facial bones. In such cases, the patient usually experiences headache, fever, and a soft swelling over the bone known as Pott's puffy tumor. Infection of the Eye Socket. Infection of the eye socket, or orbital infection, which causes swelling and subsequent drooping of the eyelid, is a rare but serious complication of ethmoid sinusitis. In these cases, the patient loses movement in the eye, and pressure on the optic nerve can lead to vision loss, which is sometimes permanent. Fever and severe illness are usually present. Blood Clot. Blood clots are another danger, although rare, from ethmoid or frontal sinusitis. If a blood clot forms in the sinus area around the front and top of the face, symptoms are similar to orbital infection. In addition, the pupil may be fixed and dilated. Although symptoms usually begin on one side of the head, the process usually spreads to both sides. Brain Infection. The most dangerous complication of sinusitis, particularly frontal and sphenoid sinusitis, is the spread of infection by anaerobic bacteria to the brain, either through the bones or blood vessels. Abscesses, meningitis, and other life-threatening conditions may result. In such cases, the patient may experience mild personality changes, headache, altered consciousness, visual problems, and, finally, seizures, coma, and death.
inflammation or swelling of the tonsils from frequent or ongoing (chronic) tonsillitis can cause complications such as: Difficulty breathing Disrupted breathing during sleep (obstructive sleep apnea) Infection that spreads deep into surrounding tissue (tonsillar cellulitis) Infection that results in a collection of pus behind a tonsil (tonsillar abscess)
You might also like
- Chapter 31 Immunologic System IntroductionDocument5 pagesChapter 31 Immunologic System IntroductionStacey100% (2)
- 217 RF Peripheral Neurovascular DysfunctionDocument8 pages217 RF Peripheral Neurovascular Dysfunctionapi-271775750No ratings yet
- Chicken-Pox Concept MapDocument4 pagesChicken-Pox Concept MapElle0% (1)
- Nursing Diagnosis For CataractDocument3 pagesNursing Diagnosis For CataractZainul HazwanNo ratings yet
- NCPDocument2 pagesNCPAnne De VeraNo ratings yet
- Ppe4 Reflection AssignmentDocument11 pagesPpe4 Reflection Assignmentapi-318846856100% (1)
- Spinal Cord InjuryDocument3 pagesSpinal Cord InjuryDan Leo UnicoNo ratings yet
- Impaired Physical Mobility...Document3 pagesImpaired Physical Mobility...Christy BerryNo ratings yet
- A Case Study On Mild Compression Deformity L1Document25 pagesA Case Study On Mild Compression Deformity L1JM UncianoNo ratings yet
- NCP (Or) ThyroidectomyDocument3 pagesNCP (Or) ThyroidectomyChiz CorreNo ratings yet
- Surgical NCPDocument6 pagesSurgical NCPAreeya SushmitaNo ratings yet
- Cues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale EvaluationDocument4 pagesCues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale Evaluationjomsportg0% (1)
- Word Ncp.......... TetanusDocument6 pagesWord Ncp.......... TetanusaianrNo ratings yet
- Risk For Peripheral NeurovacularDocument4 pagesRisk For Peripheral NeurovacularRoseben SomidoNo ratings yet
- Retinal DetachmentDocument6 pagesRetinal DetachmentNader Smadi100% (3)
- Nursing Care Plan D-CDocument2 pagesNursing Care Plan D-CGian MonillaNo ratings yet
- NCP Self Care DeficitDocument3 pagesNCP Self Care DeficitLeizel ApolonioNo ratings yet
- Nursing Care Plan For Low SelfDocument3 pagesNursing Care Plan For Low SelfMarissa AsimNo ratings yet
- Diabetic Ketoacidosis Case StudyDocument5 pagesDiabetic Ketoacidosis Case StudyJully GaciasNo ratings yet
- Risk For InfectionDocument1 pageRisk For InfectionEuanne OrellanoNo ratings yet
- Head Injury....Document47 pagesHead Injury....nikowareNo ratings yet
- Compartment Syndrome NCP (PAIN)Document2 pagesCompartment Syndrome NCP (PAIN)eunica16No ratings yet
- Impaired Physical MobilityDocument2 pagesImpaired Physical MobilityJayson OlileNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Risk For ConstipationDocument4 pagesNursing Care Plan: Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Risk For Constipationkenneth_bambaNo ratings yet
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Intervention Rationale EvaluationDocument2 pagesNovilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Intervention Rationale EvaluationCharina AubreyNo ratings yet
- LARYNGITISDocument13 pagesLARYNGITIStherese BNo ratings yet
- Patient With Neutropenia Risk For Infection Related To Inadequate Secondary Defenses (Leukopenia, Neutropenia), Altered Response To MicrobialDocument2 pagesPatient With Neutropenia Risk For Infection Related To Inadequate Secondary Defenses (Leukopenia, Neutropenia), Altered Response To MicrobialICa MarlinaNo ratings yet
- Nursing Care Plan: Nikolai P. Funcion, FSUU-SNDocument5 pagesNursing Care Plan: Nikolai P. Funcion, FSUU-SNNikolai FuncionNo ratings yet
- NCP For Ulnar SurgeryDocument5 pagesNCP For Ulnar SurgeryjiloNo ratings yet
- NCP Ineffective Breathing PatternDocument4 pagesNCP Ineffective Breathing PatternSeika SouiNo ratings yet
- LCPDDocument7 pagesLCPDakoismeNo ratings yet
- Cholecystectomy (: Laparoscopic GallstonesDocument4 pagesCholecystectomy (: Laparoscopic GallstonesAlexia BatungbacalNo ratings yet
- Nursing Care Plan For Impaired Environmental Interpretaion NCPDocument4 pagesNursing Care Plan For Impaired Environmental Interpretaion NCPderic100% (2)
- Burns - Skin Integrity, ImpairedDocument2 pagesBurns - Skin Integrity, Impairedmakyofrancis20No ratings yet
- Doxofylline: D 400 MG TabletsDocument33 pagesDoxofylline: D 400 MG TabletsBibek Singh Mahat100% (2)
- As Needed.: Environmental Stimuli 6Document4 pagesAs Needed.: Environmental Stimuli 6Nicole GumolonNo ratings yet
- Aaa Gastrectomy NCP FinalDocument13 pagesAaa Gastrectomy NCP Finallexzaf100% (1)
- Fistula NCPDocument1 pageFistula NCPHasna LisnaNo ratings yet
- What Is Stroke?: BY: Luis Alberto Sanchez Hernandez Physical TherapistDocument12 pagesWhat Is Stroke?: BY: Luis Alberto Sanchez Hernandez Physical TherapistLidiaAMonroyRNo ratings yet
- Potts Disease NCP .. JustificationDocument8 pagesPotts Disease NCP .. JustificationMicah SalesNo ratings yet
- Assessment Nursing Diagnosis Planning Nursing Intervention Rationale EvaluationDocument3 pagesAssessment Nursing Diagnosis Planning Nursing Intervention Rationale EvaluationMikhaelEarlSantosTacordaNo ratings yet
- FractureDocument4 pagesFractureRaveen mayiNo ratings yet
- NCP CataractDocument3 pagesNCP CataractKate ChavezNo ratings yet
- NCP Icu-CcuDocument6 pagesNCP Icu-CcuJohn CenasNo ratings yet
- NCP Alzheimers DiseaseDocument2 pagesNCP Alzheimers DiseaseShawn TejanoNo ratings yet
- Scribd 020922 Case Study-Oncology A&kDocument2 pagesScribd 020922 Case Study-Oncology A&kKellie DNo ratings yet
- Ineffective Breathing PatternDocument7 pagesIneffective Breathing PatternJanmae JivNo ratings yet
- Case Study Pleural EffusionDocument4 pagesCase Study Pleural EffusionKhristine Anne FabayNo ratings yet
- Pathophysiology of FractureDocument2 pagesPathophysiology of Fracturemyer pasandalanNo ratings yet
- Nursing Care Plan of CataractDocument3 pagesNursing Care Plan of CataractDimzmonyo100% (1)
- Leg 1 A NCM 107-LMRDocument4 pagesLeg 1 A NCM 107-LMRAleli DoNo ratings yet
- NP Motor Vehiculr AccidentDocument16 pagesNP Motor Vehiculr AccidentAngelie Joy100% (1)
- NCPDocument6 pagesNCPBon BonNo ratings yet
- Ineffective Cerebral Tissue Perfusion Related ToDocument7 pagesIneffective Cerebral Tissue Perfusion Related TohannahNo ratings yet
- Activity IntoleranceDocument1 pageActivity IntoleranceAndrea Francesca SantosNo ratings yet
- Case Report PresentationDocument34 pagesCase Report PresentationDwi Permana PutraNo ratings yet
- Presentasi Kasus Glaukoma AkutDocument24 pagesPresentasi Kasus Glaukoma AkutHendrawan Ariwibowo100% (1)
- Angle-Closure Glaucoma - UpToDateDocument9 pagesAngle-Closure Glaucoma - UpToDateElaine June FielNo ratings yet
- Activity7 (Sympathetic Ophthalmia)Document4 pagesActivity7 (Sympathetic Ophthalmia)Gabbii CincoNo ratings yet
- Acute Angle Closure GlaucomaDocument17 pagesAcute Angle Closure GlaucomaOvidiu RusuNo ratings yet
- GlaucomaDocument9 pagesGlaucomat2ybrkm5hwNo ratings yet
- Sleep ParalysisDocument34 pagesSleep ParalysisKholah RizwanNo ratings yet
- 03 Enf. SistemicasDocument12 pages03 Enf. SistemicasAgustin BuryakNo ratings yet
- Catangay Module 1Document3 pagesCatangay Module 1Kristen Althea CatangayNo ratings yet
- State of Lung Cancer 2021Document16 pagesState of Lung Cancer 2021Honolulu Star-AdvertiserNo ratings yet
- Adji Suranto. Khasiat Dan Manfaat Madu Herbal (Jakarta: Agromedia Pustaka, 2004)Document2 pagesAdji Suranto. Khasiat Dan Manfaat Madu Herbal (Jakarta: Agromedia Pustaka, 2004)Dania Shafa AlmasaNo ratings yet
- 06 Case SheetDocument10 pages06 Case Sheetshad mansooriNo ratings yet
- Chapter 10 Interstitial Lung DiseaseDocument10 pagesChapter 10 Interstitial Lung DiseaseAleksandar Tasic100% (1)
- Med Term 3 (1) - 231209 - 003105Document30 pagesMed Term 3 (1) - 231209 - 003105Anushka KarthikeyanNo ratings yet
- Scoliosis, Lordosis, and KyphosisDocument40 pagesScoliosis, Lordosis, and KyphosisRati W. PaneseNo ratings yet
- AlbuminDocument14 pagesAlbuminrahmifitriaNo ratings yet
- Drug Study Form 1 OBDocument1 pageDrug Study Form 1 OBJOSHUA NERZA LACANDOZENo ratings yet
- Vestibular Rehabilitation Exercises Pi 1209Document3 pagesVestibular Rehabilitation Exercises Pi 1209Abner SánchezNo ratings yet
- Med 02 2023Document19 pagesMed 02 2023Nimer Abdelhadi AliNo ratings yet
- NCP Case PresDocument5 pagesNCP Case Pressyd19No ratings yet
- PAINWeek Journal Vol 7, Q1Document78 pagesPAINWeek Journal Vol 7, Q1Apostolos T.No ratings yet
- Mtap - Bacteriology FinalsDocument6 pagesMtap - Bacteriology FinalsMoira Pauline LibroraniaNo ratings yet
- Blood Bank ManualDocument29 pagesBlood Bank ManualMarice Ferrufino SchmidtNo ratings yet
- B) Schistosomes: Alhamdi Bara AspalalDocument5 pagesB) Schistosomes: Alhamdi Bara AspalalKervy Jay AgraviadorNo ratings yet
- List of Medical Triads, Tetrads, and PentadsDocument5 pagesList of Medical Triads, Tetrads, and PentadsHajer BassemNo ratings yet
- Breast Cancer Awareness - 13 October 2019Document4 pagesBreast Cancer Awareness - 13 October 2019Times MediaNo ratings yet
- Pycnogenol For Menstrual DiscomfortDocument5 pagesPycnogenol For Menstrual DiscomfortLubimOffNo ratings yet
- NCP TetanusDocument6 pagesNCP Tetanusjoanna50% (6)
- Acute Adverse Effects of TransfusionDocument64 pagesAcute Adverse Effects of TransfusionArifudin Cipto HusodoNo ratings yet
- Entamoeba Coli: BackgroundDocument4 pagesEntamoeba Coli: BackgroundJam Pelario100% (1)
- Faringitis StreptococcusDocument16 pagesFaringitis StreptococcusnurNo ratings yet
- Vulvar Lesions: CAPT Mike Hughey, MC, USNRDocument31 pagesVulvar Lesions: CAPT Mike Hughey, MC, USNRlalalala50% (2)
- (SLE) and PregnancyDocument39 pages(SLE) and PregnancyRake SardevaNo ratings yet
- Male and Female Pattern Hair LossDocument15 pagesMale and Female Pattern Hair LossRahul SrivastavaNo ratings yet
- Generalized Anxiety Disorder Screener GAD7Document2 pagesGeneralized Anxiety Disorder Screener GAD7Indira Damar PangestuNo ratings yet