Professional Documents
Culture Documents
Anomalies of The Cervical Vertebrae
Uploaded by
Mohammed KorayemOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anomalies of The Cervical Vertebrae
Uploaded by
Mohammed KorayemCopyright:
Available Formats
ONLINE ONLY
Anomalies of the cervical vertebrae in patients with skeletal Class II malocclusion and horizontal maxillary overjet
Liselotte Sonnesena and Inger Kjrb Copenhagen, Denmark Introduction: Cervical column morphology was examined in adult patients with skeletal Class II malocclusion and horizontal maxillary overjet; the ndings were compared with cervical column morphology in an adult control group with neutral occlusion and normal craniofacial morphology. This has not previously been investigated. Methods: The overjet group consisted of 34 patients: 28 women (ages, 18-42 years) and 6 men (ages, 18-38 years). Their horizontal overjets ranged from 5.47 to 15.29 mm. The control group consisted of 21 subjects: 15 women (ages, 23-40 years) and 6 men (ages, 25-44 years). A visual assessment of the cervical column was made, and craniofacial dimensions were measured on each subjects prole radiograph. Results: In the overjet group, 52.9% had fusion of the cervical column, and 5.9% had posterior arch deciency. Fusions occurred signicantly more often in the overjet group compared with the control group (P .01). Associations were found between fusions of the cervical column and mandibular retrognathia (P .05), large cranial base angle (P .05), and large horizontal overjet (P .05). Conclusions: The results could provide a new method to phenotypically subdivide skeletal maxillary overjets. This is important for the diagnosis and the correct treatment of these patients. (Am J Orthod Dentofacial Orthop 2008;133: 189.e15-189.e20)
eviations of cervical column morphology occur in healthy subjects with neutral occlusion and normal craniofacial morphology and in patients with craniofacial syndromes, deviating craniofacial morphology, and severe malocclusion traits. Recently, it was found that fusions between the second and third cervical vertebrae occur in 14.3% of healthy subjects.1 Thus, fusions of the upper cervical column in that range are considered normal. In previous studies, an association was found between malformations of the upper cervical vertebrae and patients with cleft lip or palate.2-4 Recently, an association was also found between malformation of the upper cervical vertebrae not only in patients with condylar hypoplasia1 but also in patients with skeletal deepbite5 and skeletal mandibular overjet.6 These studies showed that cervical column deviations occurred in 72.7% of those in the condylar hypoplasia group, in 41.5% of the deepbite group, and in 61.4% of the
From the Department of Orthodontics, School of Dentistry, Faculty of Health Sciences, University of Copenhagen, Copenhagen, Denmark. a Associate professor. b Professor. Reprint requests to: Liselotte Sonnesen, Department of Orthodontics, School of Dentistry, Faculty of Health Sciences, University of Copenhagen, 20 Nrre All, DK-2200 Copenhagen N, Denmark; e-mail, lls@odont.ku.dk. Submitted, May 09, 2007; revised and accepted, July 20, 2007. 0889-5406/$34.00 Copyright 2008 by the American Association of Orthodontists. doi:10.1016/j.ajodo.2007.07.018
mandibular overjet group. Deviations occurred signicantly more often in all 3 patient groups compared with the control group. This indicates that the morphological deviations of the upper cervical vertebrae are associated not only with malformation of the jaws but also with craniofacial morphology and occlusion. Accordingly, it is relevant to focus on similar associations in patients with skeletal Class II and horizontal maxillary overjet. To our knowledge, no one has studied cervical column morphology in relation to skeletal Class II malocclusion and horizontal maxillary overjet. Our aims in this study were (1) to describe the morphology of the cervical column in adult patients with skeletal horizontal maxillary overjet, (2) to compare the morphology of the cervical column in a group of adult patients with skeletal horizontal maxillary overjet (overjet group) with a control group with neutral occlusion and normal craniofacial morphology (control group), and (3) to analyze associations between the morphology of the cervical column and craniofacial dimensions in the total group (overjet and control groups).
MATERIAL AND METHODS
The overjet group consisted of 34 patients: 28 women (ages, 18-42 years; mean, 25.0) and 6 men (ages, 18-38 years; mean, 24.0). The inclusion criteria for the horizon188.e15
188.e16 Sonnesen and Kjr
American Journal of Orthodontics and Dentofacial Orthopedics February 2008
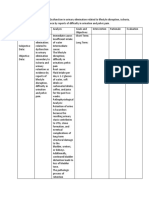
Table I.
Craniofacial dimensions in the horizontal maxillary overjet and the control groups
Overjet (n 34) SD Controls (n Mean 21) SD Group P Sex P
Variable () Sagittal dimensions Ss-N-Pg Ss-N-Sm S-N-Ss S-N-Pg Vertical dimensions NL-ML NSL-NL NSL-ML Cranial base angle N-S-Ba Incisor relationship Overjet (mm) Overbite (mm)
Mean
7.04 7.98 81.14 75.09 30.45 8.49 38.93 132.44 10.03 1.97
2.39 1.83 3.85 4.04 3.46 3.46 9.64 5.52 2.95 3.83
1.58 2.14 81.64 80.12 22.32 7.41 29.71 130.99 2.82 2.30
1.92 1.59 2.97 3.41 3.13 3.02 4.81 4.61 0.73 0.96
* * NS * * NS * NS * NS
NS NS NS NS
NS
NS NS NS
*P .001; unpaired t test. P .05; women larger than men; unpaired t test. NS, not signicant; unpaired t test.
tal maxillary overjet group were (1) 18 to 42 years of age, (2) no history of orthodontic treatment during childhood, (3) skeletal horizontal maxillary overjet (sagittal jaw relationship larger than 1 SD as described by Bjrk7 and assessed by lateral radiographs of each patient), (4) at least 24 permanent teeth, (5) no craniofacial anomalies or systemic muscle or joint disorders, and (6) availability of a prole radiograph before surgical orthodontic treatment with the rst 5 cervical vertebrae visible. Thirty-four prole radiographs were systematically selected according to these inclusion criteria from patients registered since 1975 in the orthodontic surgical patient archive (378 records) at the Department of Orthodontics, School of Dentistry, University of Copenhagen in Denmark. The sagittal jaw relationships were between 4.5 and 12.67 (mean, 7.98), the horizontal overjets were 5.47 to 15.29 mm (mean, 10.03 mm), and the vertical jaw relationships were 15.00 to 43.10 (mean, 30.45) (Table I). The control group consisted of 21 subjects: 15 women (ages, 23-40 years; mean, 29.2) and 6 men (ages, 25-44 years; mean, 32.8). The subjects were students and staff members at the Aarhus School of Dentistry in Aarhus, Denmark. The selection criteria were (1) neutral occlusion or minor malocclusion not requiring orthodontic treatment according to the Danish screening procedure for malocclusion entailing health risks,8,9 (2) no previous history of orthodontic treatment, (3) sagittal and vertical jaw relationship within 1 SD as described by Bjrk7 and assessed by lateral radiographs of each subject, (4) at least 24 permanent teeth, (5) no craniofacial anomalies or systemic muscle
or joint disorders, and (6) availability of a prole radiograph with the rst 5 cervical vertebrae visible. The sagittal jaw relationships ranged from 0.60 and 5.40 (mean, 2.15), the horizontal overjets were 1.50 to 4.70 mm (mean, 2.82 mm), and the vertical jaw relationships were between 18.00 and 28.20 (mean, 22.32) (Table I). The differences in mean values for the craniofacial dimensions between the 2 groups and the sexes are shown in Table I. The morphology of the cervical column was assessed from visual inspection of the rst 5 cervical vertebrae (C1-C5) as they are normally seen on a standardized lateral skull radiograph. Characteristics of the cervical column were classied according to the method of Sandham2 and divided into 2 categories: posterior arch deciency and fusion anomalies. Posterior arch deciency consisted of partial cleft and dehiscence. Fusion anomalies were registered in subjects with fusions of 2 cervical bodies, block fusion when more than 2 bodies were fused, and occipitalization of C1 and the occipital bone. Only anomalies that were veried on the later prole radiographs after surgery were considered anomalies of the cervical column.
Craniofacial dimensions
For the control group, the prole radiographs were taken with the teeth in occlusion and standardized head posturethe mirror positionas described by Siersbk-Nielsen and Solow.10 The radiographs were taken at the Department of Oral Radiology, Aarhus School of
American Journal of Orthodontics and Dentofacial Orthopedics Volume 133, Number 2
Sonnesen and Kjr 188.e17
nial base, and vertical and sagittal craniofacial dimensions was assessed by remeasurement of 20 lateral radiographs selected at random from the previously recorded radiographs. The radiographs were digitized again, and the differences between the 2 sets of recordings were calculated. No signicant differences between the 2 sets of recordings were found by paired t test. The method errors calculated by Dahlbergs formula13 ranged from 0.09 to 0.69, and the Houston reliability coefcients were from 0.99 to 1.00.14 The reliability was within the same range as for traditional lm-based radiographs.15
Statistical analysis
Fig 1. Reference points and lines according to the method of Solow and Tallgren.28
Dentistry, in a Bucky Conds cephalometer (Petersen and Schmidt, Copenhagen, Denmark) with a lm-tofocus distance of 180 cm and a lm-to-median plane distance of 10 cm. No correction was made for the constant linear enlargement of 5.6%. A plumb line was suspended from the ceiling to mark the true vertical line on the radiographs. The digital radiography system was photostimulable phosphor plate, Digora (Soredex, Helsinki, Finland), placed in a traditional 24 30-cm cassette without intensifying screen. The reference points were marked and digitized in PorDias for Windows (version 6; Institute for Orthodontic Computer Science, Middelfart, Denmark) (Fig 1), and 9 variables representing the cranial base angle and the vertical and sagittal craniofacial dimensions were calculated. For the horizontal maxillary overjet group, the 34 prole radiographs were taken in a cephalostat with a lm-to-focus distance of 180 cm and a lm-to-median plane distance of 10 cm. No correction was made for the constant linear enlargement of 5.6%.11 The variables are listed in Table I. The reliability of the visual assessment of the morphological characteristics of the cervical vertebrae was determined by interobserver examinations between the authors. The interobserver examinations showed very good agreement (0.82) as assessed by the kappa coefcient.12 The reliability of the variables describing the cra-
The normality of the distributions was assessed by the parameters of skewness and kurtosis and by the Shapiro-Wilks W test. The cephalometric measurements were normally distributed except for overjet. For the craniofacial dimensions, the effect of age was assessed by linear regression analysis and, for morphological characteristics of the cervical column, by logistic regression analysis. Differences in the means of the craniofacial dimensions between sexes and groups were assessed with the unpaired t test. Differences in the occurrence of morphological characteristics of the cervical column between sexes and groups were assessed with the Fisher exact test. Associations between the morphology of the cervical column and each craniofacial dimension were expressed in terms of Nagalkerke16 logistic regression correlation coefcients (R2) and tested for the possible effects of age and sex by multiple logistic regression analyses. A multiple logistic regression analysis with stepwise backward elimination was then performed to determine the relationship between the morphology of the cervical column as the dependent variable and the variables that were signicantly correlated with the morphology of the cervical column as the independent variables. The multiple correlation coefcients (R2) (R R2) in the logistic regression analysis were calculated according to the method of Nagelkerke.16 In all logistic regression models, the linearity of the effect was tested with the HosmerLemeshow goodness-of-t test. The results were considered signicant at P .05. The statistical analyses were performed with SPSS software (version 13.00; SPSS, Chicago, Ill).
RESULTS
In the overjet group, 52.9% had fusion of the cervical column, and 5.9% had posterior arch deciency (Table II). The fusion always occurred between C2 and C3, and posterior arch deciency always occurred in combination with fusion (Fig 2). No statis-
188.e18 Sonnesen and Kjr
American Journal of Orthodontics and Dentofacial Orthopedics February 2008
Table II.
Prevalence of morphological characteristics of cervical column in patients with horizontal maxillary overjet (overjet group) and subjects with neutral occlusion and normal craniofacial morphology (control group)
Overjet group Control group n 18 3 1 1 % 85.7 14.3 4.8 4.8 P * * NS NS
Table III. Signicant correlations (R) between morphology of cervical column and mandibulary prognathism (S-N-Pg), inclination of the maxilla (NSL-NL), cranial base angle (N-S-Ba) and overjet in the total group (n 55) Fusion S-N-Pg NSL-NL N-S-Ba Overjet .36* NS .36* .35* Posterior arch deciency NS .54* .65* NS More than 1 deviation NS .54* .65* NS
Variable Normal Fusion anomalies Posterior arch deciency More than 1 deviation
n 16 18 2 2
% 47.1 52.9 5.9 5.9
*P 0.1; Fisher exact test. NS, not signicant; Fisher exact text.
*P .05; logistic regression. NS, not signicant; logistic regression.
logical characteristics of the cervical column (women, 13.3%; men, 16.7%). The comparison of the overjet group and the control group showed that the morphological deviations of the cervical column occurred signicantly more often in the overjet group (P .01, Table II).
Craniofacial dimensions related to the cervical column morphology
Fig 2. Morphological characteristics of the cervical column in patients with skeletal horizontal overjet illustrated by radiographs and graphic drawings: 1, fusion of C2 and C3 (fusion anomalies); 2, partial cleft of the posterior portion of the neural arch of atlas (posterior arch deciency).
In the total group, the correlation analysis showed that mandibular retrognathia (S-N-Pg, P .05), large cranial base angle (N-S-Ba, P .05), and large horizontal overjet (P .05) were signicantly correlated with fusion of the cervical column. These associations were not due to the effect of age or sex. Posterior arch deciency was signicantly positively correlated with maxillary inclination (NSL-NL, P .05) and cranial base angle (N-S-Ba, P .05). The signicant regression coefcients (R) were low to moderate, with numerical values from 0.35 to 0.65 (Table III). The multiple logistic regression analysis showed that the most important factors for fusion of the cervical column were cranial base angle (P .05) and horizontal overjet (P .05) (R2 0.22, R 0.47). Multiple logistic regression analysis for posterior arch deciency was not included in the analyses because of its low prevalence.
DISCUSSION
tical sex differences were found in the occurrence of morphological characteristics of the cervical column (women, 46.4%; men, 83.0%) even though the sex difference was large. As previously reported, in the control group, 14.3% had fusion of the cervical column, and 4.8% had fusion and posterior arch deciency (Table II).1 The fusion always occurred between C2 and C3. No statistical sex differences were found in the occurrence of morpho-
The morphological deviations of the cervical column, which have not previously been described on lateral radiographs or by either computed tomography scan or magnetic resonance imaging, occurred signicantly more often in the overjet group (52.9%) compared not only with the control group but also with a group of patients with skeletal deepbite (41.%),5 whereas the prevalences were greater in patients with
American Journal of Orthodontics and Dentofacial Orthopedics Volume 133, Number 2
Sonnesen and Kjr 188.e19
skeletal mandibular overjet (61.4%)6 and patients with condylar hypoplasia (72.7%).1 Because the prevalence of morphological cervical column deviations differs in groups with skeletal craniofacial morphology deviations and malocclusion traits, the pattern of cervical column morphology was the same as seen in the controls and a group of patients with skeletal deepbite.5 In these groups, the fusions always occurred between C2 and C3. The pattern in patients with skeletal mandibular overjet and patients with condylar hypoplasia was different. In the patients with condylar hypoplasia, 9% of the fusions occurred between C3 and C4,1 and, in the mandibular overjet group, 3.5% of the fusions were block fusions.6 As a conclusion from this comparison, the cervical column differs phenotypically in the various skeletal malocclusion traits. Body fusions occurred in the deepbite, control, and horizontal maxillary overjet groups at the same cervical region but with different prevalences, whereas, in patients with mandibular overjet, the malformations are located in the same region, but block fusion occurs. It is not known why these malformations occur in the cervical column and why they occur with different frequencies. Also, the different patterns in groups of patients with varied skeletal craniofacial morphologies and malocclusion traits are inexplicable. In the prenatal period, the vertebral bodies were formed around the notochord, and thus the notochord might be responsible for their location and morphology.17-20 Previous studies also found that different genes act in different regions,21-24 and this might be the focus of future studies on the pathogenesis.
Associations
cervical vertebrae, especially the vertebral bodies, but also the basilar part of the occipital bone, which is the posterior part of the cranial base angle,17-20,25-27 it is understandable, as seen in this study, that the cranial base angle is associated with malformations in the cervical vertebrae. The mesoderm forming the vertebral arches and the remaining parts of the occipital bone is also formed from notochordal inductions. In this study, we found an association between posterior arch deciency as partial cleft of the vertebral arches and the cranial base angle and the maxillary inclination. Because the maxilla is attached to the inferior cranial base,7 it could be presumed that also the inclination of the anterior part of the cranial base deviates in horizontal skeletal overjets. Future molecular genetic studies and prenatal insight into normal and pathologic associations between development in the cranial base, the jaws, and the cervical region might be essential to subdivide maxillary overjets and thereby explain the etiology of skeletal deviations in the craniofacial prole. The clinical application of this phenotypic differentiation of maxillary overjets is a more accurate diagnosis that might help to determine the correct treatment for these patients.
CONCLUSIONS
In this study, mandibular retrognathia, cranial base angle, and horizontal overjet were correlated with fusion of the cervical column. This means that patients with skeletal horizontal overjet are most likely to have fusion anomalies if the horizontal overjet is caused by mandibular retrognathia and a large cranial base angle and not by maxillary prognathia. This agrees with a previous study that found that patients with skeletal mandibular overjet were more likely to have fusion anomalies if the mandibular overjet was caused by maxillary retrognathia and not by mandibular prognathia.6 This could indicate that fusions of the cervical column are more likely to be associated with retrognathia of the jaws in general instead of prognathia of the jaws. We found that the craniofacial parameters most important for the fusions of the cervical vertebral bodies were cranial base angle and horizontal overjet. Because the notochord determines the development of not only the
In the overjet group, 52.9% had fusion of the cervical column, and 5.9% had posterior arch deciency. The morphological deviations of the cervical column occurred signicantly more often in the overjet group than in the control group, whereas the pattern of morphological deviations of the cervical column was the same in both groups. Associations were found between fusions of the cervical column and mandibular retrognathia, large cranial base angle, and large horizontal overjet, and between posterior arch deciency and large maxillary inclination and cranial base angle. The craniofacial parameters most important for the fusions were cranial base angle and horizontal overjet. Our ndings differ from previous studies on prole radiographs of skeletal mandibular overjet and skeletal deepbite and subjects with condylar hypoplasia. Molecular genetic studies and prenatal insight into normal and pathologic associations between development in the cranial base, the jaws, and the cervical region might be necessary to explain the etiology of skeletal deviations in the craniofacial prole. We thank the students and staff at the Aarhus School of Dentistry, Aarhus University; Jan Hesselberg Madsen, specialist in orthodontics, coordinator of the
188.e20 Sonnesen and Kjr
American Journal of Orthodontics and Dentofacial Orthopedics February 2008
treatment of orthodontic surgical patients at the Department of Orthodontics, University of Copenhagen; and Maria Kvetny for linguistic support and manuscript preparation.
REFERENCES 1. Sonnesen L, Pedersen C, Kjr I. Cervical column morphology related to head posture, cranial base angle and condylar malformation. Eur J Orthod 2007;29:1-6. 2. Sandham A. Cervical vertebral anomalies in cleft lip and palate. Cleft Palate J 1986;23:206-14. 3. Horswell BB. The incidence and relationship of cervical spine anomalies in patients with cleft lip and/or palate. J Oral Maxillofac Surg 1991;49:693-7. 4. Ugar DA, Semb G. The prevalence of anomalies of the upper cervical vertebrae in subjects with cleft lip, cleft palate, or both. Cleft Palate Craniofac J 2001;38:498-503. 5. Sonnesen L, Kjr I. Cervical vertebral body fusions in patients with skeletal deep bite. Eur J Orthod Epub ahead of print: August 9, 2007. 6. Sonnesen L, Kjr I. Cervical column morphology in patients with skeletal Class III malocclusion and mandibular overjet. Am J Orthod Dentofacial Orthop 2007;132:427.e7-12. 7. Bjrk A. The face in prole. Svensk Tandlkebladet 1947;40(Suppl 5B):1. 8. Bekendtgrelse om kommunal tandpleje. Danish Ministry of Health Order No. 338; 1990. 9. Solow B. Orthodontic screening and third party nancing. Eur J Orthod 1995;17:79-83. 10. Siersbk-Nielsen S, Solow B. Intra- and interexaminer variability in head posture recorded by dental auxiliaries. Am J Orthod 1982;82:50-7. 11. Bjrk A. Kbernes relation til det vrige kranium. In: Ahlgren J editor. Nordisk lrobok i ortodonti. Stockholm: Sveriges Tandlkarfrbunds Frlagsfrening; 1975. 12. Cohen JA. A coefcient of agreement for nominal scales. J Educ Psychol Meas 1960;20:37-46. 13. Dahlberg G. Statistical methods for medical and biological students. New York: Interscience Publications; 1940.
14. Houston WJB. The analysis of errors in orthodontic measurements. Am J Orthod 1983;83:382-90. 15. Sonnesen L, Bakke M, Solow B. Temporomandibular disorders in relation to craniofacial dimensions, head posture and bite force in children selected for orthodontic treatment. Eur J Orthod 2001;23:179-92. 16. Nagelkerke NJD. A note on a general denition of the coefcient of determination. Biometrika 1991;78:691-2. 17. Kjr I, Keeling JW, Grm N. Midline maxillofacial skeleton in human anencephalic fetuses. Cleft Palate Craniofac J 1994;31: 250-6. 18. Kjr I. Human prenatal craniofacial development related to brain development under normal and pathologic conditions. Acta Odontol Scand 1995;53:135-43. 19. Kjr I. Neuro-osteology. Crit Rev Oral Biol Med 1998;9: 224-44. 20. Kjr I, Hansen BF. The adenohypophysis and the cranial base in early human development. J Craniofac Genet Dev Biol 1995;15: 157-61. 21. Acampora D, DEsposito M, Faiella A, Pannese M, Migliaccio E, Morelli F, et al. The human HOX gene family. Nucleic Acids Res 1989;17:10385-402. 22. Duboule D, Dolle P. The structural and functional organization of the murine HOX gene family resembles that of drosophila homeotic genes. EMBO J 1989;8:1497-505. 23. Krumlauf R. Hox genes in vertebrate development. Cell 1994; 78:191-201. 24. Ruddle FH, Amemiya CT, Carr JL, Kim CB, Ledje C, Shashikant CS, et al. Evolution of chordate hox gene clusters. Ann NY Acad Sci 1999;870:238-48. 25. Mller F, ORahilly R. The early development of the nervous system in staged insectivore and primate embryos. J Comp Neurol 1980;193:741-51. 26. Kjr I, Niebuhr E. Studies of the cranial base in 23 patients with cri-du-chat syndrome suggest a cranial developmental eld involved in the condition. Am J Med Genet 1999;82:6-14. 27. Sadler TW. Embryology of neural tube development. Am J Med Genet C Semin Med Genet 2005;135:2-8. 28. Solow B, Tallgren A. Head posture and craniofacial morphology. Am J Phys Anthropol 1976;44:417-35.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 04 CIN and Cervical Cancer UNEDITEDDocument120 pages04 CIN and Cervical Cancer UNEDITEDRalph JuicoNo ratings yet
- g40 DatasheetDocument10 pagesg40 DatasheetifeanyiukNo ratings yet
- The Medico-Legal Back An Illustrated Guide, 2004 PDFDocument210 pagesThe Medico-Legal Back An Illustrated Guide, 2004 PDFvitaarfianaNo ratings yet
- Community Health NursingDocument9 pagesCommunity Health NursingtheglobalnursingNo ratings yet
- Hefler Et Al., 2009Document4 pagesHefler Et Al., 2009Jonathan LucisNo ratings yet
- CHD Managemen Withot Surgery Cansy JHC (Prof. Mul) PDFDocument39 pagesCHD Managemen Withot Surgery Cansy JHC (Prof. Mul) PDFFery NurjayantoNo ratings yet
- Medical prescription abbreviation guideDocument10 pagesMedical prescription abbreviation guideFemi AlfarishiNo ratings yet
- Acute Coronary SyndromeDocument4 pagesAcute Coronary SyndromeHaryaman JustisiaNo ratings yet
- Shoulder Dystocia - StatPearls - NCBI BookshelfDocument7 pagesShoulder Dystocia - StatPearls - NCBI Bookshelfjennie JeanNo ratings yet
- Kangaroo Joey ManualDocument16 pagesKangaroo Joey ManualCarmen Leiva AsencioNo ratings yet
- Male CircumcisionDocument17 pagesMale Circumcisionkarthime86No ratings yet
- Abnormal Labour: Perceptor: Dr. Nurul Islamy, M. Kes., Sp. OGDocument54 pagesAbnormal Labour: Perceptor: Dr. Nurul Islamy, M. Kes., Sp. OGramadhiena destia100% (1)
- MSU Nursing Roles MatrixDocument2 pagesMSU Nursing Roles MatrixSitty Aizah MangotaraNo ratings yet
- Atlas of Robotic Urologic SurgeryDocument473 pagesAtlas of Robotic Urologic SurgerySarita Moreno SorribasNo ratings yet
- Maquet LyraDocument12 pagesMaquet LyraMiguel YepesNo ratings yet
- Toddler Assessment: A Step-by-Step GuideDocument30 pagesToddler Assessment: A Step-by-Step GuideNEHA PANDEY100% (3)
- Oral Allylestrenol A Pregnancy-Supporting ProgestogenDocument7 pagesOral Allylestrenol A Pregnancy-Supporting Progestogenjefri efendiNo ratings yet
- Introduction of Labour MonitoringDocument29 pagesIntroduction of Labour MonitoringMishti MokarramaNo ratings yet
- Labial AdhesionsDocument2 pagesLabial AdhesionsLydia TsiapleNo ratings yet
- International Conference On Applied Science and HealthDocument6 pagesInternational Conference On Applied Science and HealthDerison MarsinovaNo ratings yet
- Olivia Engle NP ResumeDocument1 pageOlivia Engle NP Resumeapi-654403621No ratings yet
- CAT Clitoral Phimosis FINALDocument14 pagesCAT Clitoral Phimosis FINALadi130584No ratings yet
- Aquilion One 640 LineasDocument8 pagesAquilion One 640 LineasJussef M. ValverdeNo ratings yet
- FINASLIDEMASTERALDocument42 pagesFINASLIDEMASTERALClaudette Carylle IgnacioNo ratings yet
- Do's and Dont's For Ultrasound Clinic (Final)Document4 pagesDo's and Dont's For Ultrasound Clinic (Final)Raviraj TirukeNo ratings yet
- Burn Project ReferencesDocument2 pagesBurn Project Referencesapi-279967709No ratings yet
- Qatar Star Network - As of April 30, 2019Document7 pagesQatar Star Network - As of April 30, 2019Gends DavoNo ratings yet
- Impaired Urinary EliminatonDocument5 pagesImpaired Urinary EliminatonLoriejae Marie DesulocNo ratings yet
- Resume 1Document3 pagesResume 1api-654010039No ratings yet
- A pictorial guide to key images in second trimester ultrasoundsDocument16 pagesA pictorial guide to key images in second trimester ultrasoundsSultan AlexandruNo ratings yet