Professional Documents
Culture Documents
Circadian Rhythm Sleep Disorders: Gilbert E. D'Alonzo, Do Samuel L. Krachman, Do
Uploaded by
Azrina BlackOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Circadian Rhythm Sleep Disorders: Gilbert E. D'Alonzo, Do Samuel L. Krachman, Do
Uploaded by
Azrina BlackCopyright:
Available Formats
Circadian rhythm sleep disorders
GILBERT E. DALONZO, DO SAMUEL L. KRACHMAN, DO
Night owls and morning larks are descriptive terms used to characterize individuals who go to sleep or awaken differently than most individuals. Many of these individuals have a primary circadian sleep dysrhythmia. Identification and proper treatment of a specific condition can markedly improve their quality of life. Secondary circadian dysrhythmias are very common. Nearly everyone at some time in his or her life experiences jet lag or shift work sleep disorder, two conditions in which we ignore our biologic rhythms. The impact of these conditions on performance and judgment can be tempered by certain pharmacologic and nonpharmacologic strategies. A better understanding of both primary and secondary circadian rhythm sleep disorders will be valuable to the primary care physician, leading to earlier diagnosis and improved treatment of patients with these conditions. (Key words: dyssomnias, intrinsic sleep disorders, extrinsic sleep disorders, circadian rhythm sleep disorders, jet lag, shift work)
yssomnias are a variety of disorders that produce difficulty either initiating or maintaining sleep or cause excessive sleepiness. Dyssomnias are generally categorized into three groups of disorders: the intrinsic sleep disorders, the extrinsic sleep disorders, and the circadian rhythm sleep disorders (Figure 1). Intrinsic sleep disorders either originate or develop in the body. A variety of sleep disorders are caused by psychological or medical disorders. The term intrinsic implies that the primary cause of the disorder is an abnormality in the
Dr DAlonzo is a professor of medicine, Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Temple University Medical School and Hospital, Philadelphia, Pa. Dr Krachman is an associate professor of medicine, and Director, Temple University Sleep Disorders Center. Correspondence to Gilbert E. DAlonzo, DO, Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Temple University Medical School and Hospital, 3401 N Broad St, Rm 920, Philadelphia, PA 19140. E-mail: gdalonzo@nimbus.ocis.temple.edu
physiologic process in the body. Examples of intrinsic sleep disorders include narcolepsy, obstructive sleep apnea, and periodic limb movement disorder. Extrinsic sleep disorders either originate or develop from causes outside the body. When the external factors that lead to the sleep disorder are removed, the disorder resolves and the patient begins to sleep better. Examples of extrinsic sleep disorders include alcohol-dependent sleep disorder, hypnotic-dependent sleep disorder, food allergy insomnia, and high-altitude insomnia, to name a few. In teenagers, for example, a form of extrinsic sleep disorder, inadequate sleep hygiene, often develops. Inadequate sleep hygiene is caused by the performance of activities that are inconsistent with the maintenance of good quality sleep and full daytime alertness, such as vigorous exercise close to bedtime, party going in the evening, and intense work late in the evening. Circadian rhythm sleep disorders are related to the timing of sleep within the
24-hour day. The staging of circadian rhythms supports day-night patterns and energy expenditure and conservation associated with the different requirements of activity and sleep. Although the temporal alteration of activity and rest during each 24-hour day does not cause circadian rhythms, the clock-time during which a person sleeps and is active does determine their staging. Thus, persons who consistently work day shifts and sleep nights exhibit a staging of their circadian rhythms nearly opposite to that of those who constantly work night shifts and sleep during the day. The sleep-wake routine during the 24 hours of a day is a powerful synchronizer of circadian clocks and rhythmic processes. The resetting of biologic clocks following an abrupt change in this sleep-activity schedule is not immediate. Four to 10 days may be required to complete the resetting of biologic clocks and rhythms. This is especially apparent in travelers who are rapidly transported by aircrafts across several time zones, or in individuals who rotate shifts while working and their normal nocturnal sleep period is disrupted when working on the night shift. This disorganization of the phase relationships between rhythms produces the psychological and physiologic effects referred to by air travelers as jet lag. These disorders affect alertness, concentration, and performance, all of which may be crucial for safety in certain situations. Primary circadian dysrhythmias include delayed sleep phase syndrome, advanced sleep phase syndrome, non24hour sleep-wake syndrome, and irregular sleep-wake pattern. Certain conditions are classified as secondary circadian dysrhythmias and include time zone change syndrome (jet lag), and shift work sleep disorder.
Primary circadian dysrhythmias Delayed sleep phase syndrome
Nearly everyone has heard the term night owls. Such individuals are those who delay going to sleep and find it difficult to wake up at a desired time; however, they do wake up in the morning without getting enough rest, often func-
DAlonzo and Krachman Circadian rhythm sleep disorders
JAOA Vol 100 No 8 Supplement to August 2000 S15
tioning in a daze if not overtly sleepy. Delayed sleep phase syndrome is characterized by1: sleep-onset and wake times that are intractably later than desired; actual sleep-onset times at nearly the same daily clock hour; little or no reported difficulty in maintaining sleep once asleep; extreme difficulty awakening at a desired time; and an inability to advance the sleep phase to an earlier hour by enforcing conventional sleep and wake times. During weekends or vacations, the patient sleeps normally, but at a delayed phase relative to local time. Therefore, these patients do not have a problem with sleeping; they are just out of synchronization with the expected norm. The consequences of such a problem depend on the tolerance of the patients environment. Some individuals may have serious problems during school or work. Contrarily, an individual with a flexible schedule may have no problems with delayed sleep phase syndrome. However, a more rigid work or school schedule may create a major problem for such a patient. This particular syndrome can dramatically disrupt families. Individuals with delayed sleep phase syndrome may resort to the use of alcohol or sedativehypnotic agents in an attempt to induce sleep earlier, at times leading to alcohol or drug dependence. Adolescence appears to be a particularly vulnerable life stage for the development of this syndrome.2 The differential diagnosis includes irregular sleep-wake pattern, sleep apnea syndromes, narcolepsy, periodic limb movement disorder, and a large number of psychiatric disorders, including depression and obsessive-compulsive behavior. An association appears to exist between delayed sleep phase syndrome and depression.3 Twenty-four-hour polysomnographic recording or continuous temperature monitoring can be used to diagnose the condition.4 Often, however, diagnosis is made on the basis of a strong clinical suspicion and sleep diaries (Figure 2). Therapy for delayed sleep phase syndrome involves chronotherapy. 5
Checklist
The use of bright light early in the morning and avoidance of light in the evening can advance a phase, thus being useful in the treatment of delayed sleep phase syndrome. 6
Intrinsic sleep disorders
Intrinsic sleep disorders narcolepsy obstructive sleep apnea periodic limb movement disorder Extrinsic sleep disorders Alcohol-dependent sleep disorder Hypnotic-dependent sleep disorder Food allergy insomnia High-altitude insomnia Inadequate sleep hygiene (in teenagers) Circadian rhythm sleep disorders Primary circadian dysrhythmias delayed sleep phase syndrome advanced sleep phase syndrome (larkishness) non24-hour sleep-wake syndrome (hypernicthermal syndrome) irregular sleep-wake pattern Secondary circadian dysrhythmias time zone change syndrome (jet lag) shift work sleep disorder.
Advanced sleep phase syndrome
Larkishness is another term that is used to describe the advanced sleep phase syndrome.1 Individuals with advanced sleep phase syndrome demonstrate a morning lark pattern, that is, they fall asleep early in the evening and awaken early in the morning. Their daily principal sleep episode is far advanced in relation to the desired clock time. This syndrome results in compelling evening sleepiness, with very early onset of sleep, and awakening earlier in the morning than desired, having had a normal amount of undisturbed sleep. Often, evening social activities are disrupted. Typically, sleep begins between 6 PM and 8 PM, but no later than 9 PM. Patients usually awaken between 1 AM and 3 AM, but no later than 5 AM. Trouble extending their sleep into the morning makes it difficult for these individuals to recover from sleep loss. Because this pattern often occurs in older individuals, fatigue and problems with cognition can occur.7 These individuals avoid evening activities, which often enhance the depression that can coexist. Driving and operating machinery in the evening can be dangerous. The differential diagnosis includes a variety of psychiatric disorders with sleep disturbance. Because individuals with this syndrome fall asleep early in the evening, narcolepsy or sleep apnea syndromes are considered. The advanced sleep phase syndrome is treated by bright-light therapy, which is administered in the late afternoon or early evening, helping to delay the onset of sleep. The technique of bright-light therapy is similar to that used in patients with the delayed sleep phase syndrome, except for the timing of exposure.8
Figure 1. Categories of dyssomnias and selected examples of each. Chronotherapy is a behavioral technique in which the bedtime is systematically delayed. Bedtime is delayed by 3-hour increments each day. The procedure is maintained until the desired bedtime is reached (that is, 11 PM or 12 AM), when the conventional 24-hour day is then established. Another treatment intervention includes bright-light therapy. The therapeutic application of bright light demands total control of exposure to light and dark throughout the day.
Non24-hour sleep-wake syndrome
The hypernicthermal, or non24-hour sleep-wake, syndrome consists of a longterm pattern comprising daily delays of
S16 JAOA Vol 100 No 8 Supplement to August 2000
DAlonzo and Krachman Circadian rhythm sleep disorders
1 to 2 hours in onset of sleep and wake times. Individuals with this syndrome cannot maintain a regular bedtime and find their onset of sleep wandering around the clock, almost as if they were isolated from all environmental time cues. Most humans have an intrinsic circadian rhythm of slightly more than 24 hours. Very rarely, patients have a gradually increasing advance in the onset of sleep. Individuals with the non24-hour sleep-wake syndrome lack the ability to synchronize by the usual time cues such as sunlight, work, or social activity. Retinal blindness is one of the more common causes of this disorder. Individuals with this disorder literally sleep around the clock. When individuals with non24-hour sleep-wake syndrome are in phase with environmental time cues, they seem to have no problem, but when they are out of phase, they complain of difficulties in either falling asleep or awakening too early or too late. Therefore, patients with this syndrome have both symptomatic and asymptomatic periods. Because most patients with this syndrome attempt to sleep and awaken at conventional times, they have progressive sleep loss, which induces daytime hypersomnolence and interferes with work or school performance. They are unable to work at conventional jobs and are even accused of being mentally retarded. Structural lesions of the brain have been associated with the non24-hour sleep-wake syndrome, and magnetic resonance imaging may be necessary.1This particular syndrome has been associated with blindness9; otherwise, it is considered to be rare. In blindness, this syndrome is probably due to the inability of light to influence or synchronize the central circadian pacemaker to the 24-hour day. Like other primary circadian dysrhythmias, the environment of patients with the non24-hour sleep-wake syndrome plays an important role in determining the degree of functional disruption. Those individuals who have this syndrome and a flexible work schedule may have little disruption. Those individuals who must follow a daily schedule, however, often have their lives dramati-
cally disrupted. It is difficult for patients with this syndrome to be successful at school or work because of poor performance related to excessive daytime sleepiness, tardiness, or even absences. The differential diagnosis includes not only all the primary circadian dysrhythmias and a variety of psychiatric disorders, but also narcolepsy and sleep apnea. Treatment of this condition includes reinforcement of daily time cues. It is helpful for individuals with this syndrome to live with a relative who keeps them on a strict schedule. The use of phototherapy may be of some value.10
irregular sleep-wake syndrome can be recognized in residents in extended-care facilities or other institutionalized patients. Reinforcement of time cues may be helpful for some patients with this syndrome. Exposure to bright light during the daytime may be helpful as many individuals with this condition are underexposed to daylight when living in institutions.14,15
Secondary circadian dysrhythmias
Secondary circadian dysrhythmias occur because the biologic clock is working properly but is functioning out of phase to the imposed geophysical environment. Jet planes and electric lights have allowed humans to ignore their biologic rhythms. Obviously, vast numbers of individuals take jet flights across multiple time zones or perform shift work, so these two conditions must be understood. Impairment of performance and judgment often occurs when individuals ignore their biologic clocks. Changes associated with rapid travel across time zones are transient and self-limited, but the changes associated with shift work persist as long as an individual is engaged in shift work.1
Irregular sleep-wake pattern
The irregular sleep-wake pattern consists of temporarily disorganized and variable episodes of sleep and wakefulness.1 Although the total 24-hour average sleep time is within normal limits for age, no single sleep period is of normal length and the likelihood of being asleep at a given time during the day is unpredictable. No recognizable circadian pattern of onset of sleep or of wakefulness can be determined. Sleep is broken up into multiple short blocks of time during each 24-hour period, and marked day-to-day variability exists in the onset of sleep and wakefulness. Polysomnographic recordings over 24 hours reveal multiple short sleep periods that show no unusual features except their brevity.11In fact, this pattern is consistent with what neonates demonstrate, except that there is a smaller fraction of sleep during each 24-hour day. A sleep log can be helpful in identifying this particular syndrome. To diagnose this condition, the sleep disturbance must be present for at least 3 months. Also, patients should not have a medical or psychiatric disorder that would account for their symptoms, and they should not meet the criteria for any other sleep disorder causing insomnia or excessive daytime sleepiness. Irregular sleep-wake syndrome may occur in individuals with central nervous system disorders such as head injury and Alzheimers dementia.12,13 Also, this syndrome can be found in a variety of developmental disabilities. Therefore,
Jet lag
Time zone change syndrome, or jet lag, consists of problems initiating or maintaining sleep, excessive daytime sleepiness, uncomfortable daytime alertness, and poor performance after very rapid travel across multiple time zones.16-18 In addition, a variety of somatic symptoms can be seen, including gastrointestinal distress, anorexia, headache, irritability, depression, fatigue, and disorientation. The severity and duration of these symptoms vary, depending on the number of time zones crossed, the directioneither east or westof travel, the timing of takeoff and arrival, and a variety of individual patient factors. Even athletic performance seems to be disturbed.19 Symptoms typically last longer after eastbound flights. Sleep-wake disturbances generally abate after 2 to 3 days, but other physiologic functions may take 8 or more days to normalize. Those individuals who routinely travel back and forth
DAlonzo and Krachman Circadian rhythm sleep disorders
JAOA Vol 100 No 8 Supplement to August 2000 S17
across time zones, such as airline personnel, diplomats, and corporate executives, may have chronic symptoms of sleep disturbance, irritability, performance impairment, and other complaints. Also, a variety of conditions can occur secondary to repetitive exposure to airplane cabin conditions. Symptoms of such conditions include irritated eyes and nasal passages, dependent edema, and muscle cramps. After rapid air travel across several time zones, endogenous circadian rhythmicities remain aligned to the home environment. Adjustment processes of various circadian rhythms are often slow, averaging approximately 1 hour of phase alignment per day after eastbound flights, and 1.5 hours per day on westbound flights. Therefore, symptoms can last several days, depending on the direction of the flight. Reducing the impact of jet lag is a popular subject, because this phenomenon affects a large number of individuals. Morning people, or larks, report less jet lag than evening types, or night owls, when traveling east. Owls do better than larks when traveling west. Younger travelers suffer less jet lag than older travelers, and individuals who exercise regularly generally do better than those who are sedentary. Successful treatment of the symptoms of jet lag include both behavioral interventions and pharmacotherapy.20 A direct approach for dealing with jet lag includes controlling sleeping and napping to optimize sleep to the appropriate time in the new location. This strategy is particularly important when traveling eastward. A structured sleep schedule can be helpful in minimizing insomnia on arrival. When traveling eastward, many travelers on an overnight flight go to bed immediately on arriving at their destination. They fall asleep quickly, sleep relatively briefly, and awaken, but they have difficulty initiating or maintaining sleep that night. If one could arrive at the destination and avoid sleep or perhaps take only a very short nap, then sleep that night and subsequent nights would likely be more complete. It may be helpful to start
adapting to the new location when still at home, before flying. A week or so before this trip, the traveler going east should start going to bed and getting up earlier. The westbound traveler should go to bed and get up later. At the same time, small shifts can be made in mealtimes, exercise, and medications that are taken on a daily basis. Before, and while on the plane, travelers should eat lightly and avoid alcohol. When on the plane, they should make themselves as comfortable as possible, stay well hydrated, and, on boarding, set their watch with the time at their destination. Using medications to enhance sleep on the plane, when traveling eastward, or after arriving at the new location is a popular countermeasure that travelers use to better adapt. If medication to enhance sleep is used, then short-acting medications can be most helpful. Shortacting benzodiazepines or melatonin21 can be useful. It is prudent to use such hypnotics in small doses when critical activities must be performed during the first day or two after arrival in the new time zone.
Figure 2. Sample sleep log. May be photocopied to give to patients to aid in diagnosis of sleep disorder.
Shift work sleep disorder
Shift work sleep disorder consists of symptoms of insomnia or excessive daytime sleepiness that occur as transient phenomenon in relation to variable work schedules.1 Physicians, particularly those in the emergency department, are familiar with the demands of shift work.22 In shift work sleep disorder, the work is usually scheduled during the typical hours of sleep. The shift work may be rotating or permanent. Affected individuals complain of an inability to maintain a normal duration of sleep when sleep is initiated in the morning, after a night of work. The reduction in sleep time generally ranges from 1 to 4 hours and often affects rapid eye movement sleep. Patients awake and feel unsatisfied with their sleep, not feeling refreshed. While working, excessive sleepiness occurs, and there is often a need for napping, and patients feel that their mental capacity and degree of alertness are impaired. A high rate of serious injury
and gastrointestinal illness is associated with shift work.23 Obviously, these problems are most frequent in workers who are rotating shifts, but they also occur in permanent night workers who usually shift their day/night schedules to more conventional times on their days off, such as weekends. Unlike environmental cues in jet lag, environmental cues in shift work sleep disorder remain opposed to the shifted sleep-wake schedule. This difference is important as light seems to be critical for synchronization of circadian rhythm. The symptoms associated with shift work sleep disorder generally improve after the first week of a new shift, but these symptoms often persist to some degree until a conventional daytime shift is reestablished. After rotation to the day shift from the night shift, sleep onset becomes a problem rather than sleep maintenance for at least several days. Certain individuals may be more adapted to working a shift schedule. Night owls adapt better than morning larks. Younger workers rather than older ones tolerate shift work better. Individuals who inherently require less sleep have an advantage, as do physically fit workers. Disruptions of social and family life are frequent. Shift workers are more predisposed to cardiovascular disease. Women may have problems with menstrual cycle irregularities and difficulty becoming pregnant. Finally, drug and alcohol dependence may result from attempts to improve disturbances in sleep and wakefulness induced by shift work. There may be possible strategies that can be used to improve sleep and performance in shift workers.24,25 Employers have an obligation to select the optimal shift system for their workforce. Educational programs at the workplace can help workers understand appropriate practice of sleep hygiene (Figure 3), and employers can provide family coun-
S18 JAOA Vol 100 No 8 Supplement to August 2000
DAlonzo and Krachman Circadian rhythm sleep disorders
Name: ______________________________________________________________
INSTRUCTIONS: (Please bring thse logs in for your appointment or mail them to the clinic.) 4. ARROW UPWARD when you awaken (include naps). 5. M for meals, S for snacks, a D for drinks with alcohol. 6. Include notes below each week or on the back.
1. Leave the times you are awake BLANK.
2. SHADE or crosshatch, or color the times when you sleep.
3. ARROW DOWN whenever you lie down to sleep.
EXAMPLE: Date
6 AM
8 AM
10 AM
Noon
2 PM
4 PM
6 PM
8 PM
10 PM
MN
2 AM
4 AM
6AM
S M
DS
8/31/2000
FIRST WEEK 8 AM 10 AM Noon 2 PM 4 PM 6 PM 8 PM 10 PM MN 2 AM 4 PM 6AM
DAlonzo and Krachman Circadian rhythm sleep disorders
Date
6 AM
SECOND WEEK 8 AM 10 AM Noon 2 PM 4 PM 6 PM 8 PM 10 PM MN 2 AM 4 AM 6AM
JAOA Vol 100 No 8 Supplement to August 2000 S19
Date
6 AM
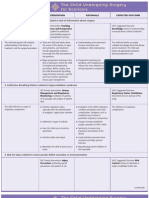
Figure 3. Common treatment modalities in circadian rhythm disorders.
Sleep hygiene
Addressing behaviors that may interfere with sleep and sleep continuity is most helpful in shift workers and those with irregular sleep patterns.
seling for the many social and domestic problems that occur as the result of shift work. It is essential for employees to understand the various strategies for improved sleep and napping. The installation of appropriate lighting at the workplace can be crucial. The speed of shift rotation is important. Two chronotherapeutic principles, delaying sleep periods and slowing shift rotations, have been used successfully to ameliorate the effects of shift work.26 The principle of sleep period delay refers to the direction of the shift work rotation, and hence, the possible timing of the sleep period. It is important to shift from days, to evenings, to nights because this rotation follows the natural tendency of circadian biology to delay the sleep period. Also, slowing the rotation implies that each shift should be maintained for more than 1 week, a minimal time necessary for circadian adaptation. Short-acting benzodiazepines can improve daytime sleep and consequently improve alertness during the night work period.27 The role of pharmacotherapy for insomnia associated with shift work, however, is highly controversial. The controversy focuses on the potential for medication abuse. However, the short-term use of medication can be helpful during those transient periods in which shift work timing is changing. The use of bright light as a synchronizer in shift work may be helpful. The judicious use of caffeine may be helpful. Finally, it is important to make sure that the shift workers medication schedule is altered for the change in shift work that occurs.
Melatonin
This hormone is created in the brain and is related to sleep induction. Ingestion of melatonin may be mildly effective in entraining the circadian cycle in jet lag, shift workers, and individuals with a non24-hour rhythm disorder.
Light therapy
Typically, bright-light (2500 to 10,000 lux) exposure for 30 to 120 minutes each day facilitates the entrainment or realignment of the circadian cycle. If used in the morning, it arouses the individual, and, if used late in the day, it delays sleep onset.
Zeitgebers
A term meaning time givers, these primarily include the initial exposure to light in the morning, common times for personal interactions, and the times we eat. Shifting these activities to synchronize with our time zone aids in changing our internal rhythms.
Phase shifting
This modality is a gradual process of changing the time of going to bed or the time of arousing in small (15 to 60 minutes) increments in order to change the circadian rhythm to match the local pattern.
Environmental modifications
This modality involves modifying our environment to entrain the circadian rhythms to times other than the lightdark cycle of the locality. This is most commonly done in shift workers.
Sleep logs
Sleep diaries or sleep logs provide information on the patients sleep-wake pattern. This information may be used to diagnose disorders or to give the patient insight into their patterns. As part of the treatment, sleep logs may be used to show a patients progress.
Comment
This article reviews a variety of circadian rhythm sleep disturbances. Shift work sleep disorder and time zone change syndrome are common conditions encountered in everyday medical practice. It is important for the primary care physician to have an understanding not only
of these secondary dysrhythmias but also of the primary dysrhythmias associated with circadian rhythm sleep disorders.
2. Thorpy MJ, Korman E, Speilman AJ, Glovinsky PB. Delayed sleep phase syndrome in adolescents. J Adolesc Health Care 1988;9:22-27. 3. Regestein QR, Monk TH. Delayed sleep phase syndrome: a review of its clinical aspects. Am J Psychiatry 1995;152:602-608. 4. Weitzman ED, Czeisler CA, Coleman RM, Spielman AJ, Zimmerman JC, Dement W, et al. Delayed sleep phase syndrome. A chronobiological disorder with sleep-onset insomnia. Arch Gen Psychiatry 1981;38:737-746.
References
1. American Sleep Disorders Association. International Classification of Sleep Disorders, revised: Diagnostic and Coding Manual. Rochester, Minn: American Sleep Disorders Association; 1997.
S20 JAOA Vol 100 No 8 Supplement to August 2000
DAlonzo and Krachman Circadian rhythm sleep disorders
5. Czeisler CA, Richardson GS, Coleman RM, Zimmerman JC, Moore-Ede MC, Dement WC, et al. Chronotherapy: resetting the circadian clocks of patients with delayed sleep phase insomnia. Sleep 1981;4:1-21. 6. Rosenthal NE, Joseph Vanderpool JR, Levendosky AA, Johnston SH, Allen R, Kelly KA, et al. Phase-shifting effects of bright morning light as treatment for delayed sleep phase syndrome. Sleep 1990;13:354361. 7. Miles LE, Dement WC. Sleep and aging. Sleep 1980;3:1-220. 8. Moldofsky H, Musisa S, Phillipson EA. Treatment of a case of advanced sleep phase syndrome by phase advance chronotherapy. Sleep 1986;9:61-65. 9. Sack RL, Lewy AJ, Blood ML, Keith LD, Nakagawa H. Circadian rhythm abnormalities in totally blind people: incidence and clinic significance. J Clin Endocrinol Metab 1992;75:127-134. 10. Hoban TM, Sack RL, Lewy AJ, Miller LS, Singer CM. Entrainment of a free-running human with bright light? Chronobiol Int 1989;6:347-353. 11. Effects of irregular versus regular sleep schedules on permance, mood and body temperature. Biol Physiol 1982;14:287-296. 12. Okawa M, Takahashi K, Sasaki H. Disturbance of circadian rhythms in severly brain-damaged patients correlated with CT findings. J Neurol 1986;233:274282.
13. Bliwise DL. Sleep in normal aging and dementia. Sleep 1993;16:40-81. 14. Ancoli-Israel S, Kripke D, Williams-Jones D, et al. Light exposure and sleep in nursing home patients. Soc Light Treat Biol Rhythms Abs 1991;3:18. 15. Saitlin A. Volicer L, Ross V, Herz L, Campbell S. Bright light treatment of behavioral and sleep disturbances in patients with Alzheimers disease. Am J Psychiatry 1992;149:1028-1032. 16. Loat CE, Rhodes EC. Jet-lag and human performance. Sports Med 1989;8:226-238. 17. Nicholson AN, Pascoe PA, Spencer MB, Stone BM, Roehrs T, Roth T. Lancet 1986;2:1205-1208. 18. Waterhouse J. Jet-lag and shift work: (1). Circadian rhythms. J R Soc Med 1999;92:398-401. 19. Manfredini R, Manfredini F, Fersini C, Conconi F. Circadian rhythms, athletic performance, and jet lag. Br J Sports Med 1998;32:101-106. 20. Graeber RC, Dement WC, Nicholson AN, Sasaki M, Wegmann HM. Aviat Space Environ Med 1986;57:B10B13. 21. Samel A. Melatonin and jet-lag. Eur J Med Res 1999;4:385-388.
22. Whitehead DC, Thomas H Jr, Slapper DR. A rational approach to shift work in emergency medicine. Ann Emerg Med 1992;21:1250-1258. 23. Harrington JM. Shift work and healtha critical review of the literature on working hours. Ann Acad Med Singapore 1994;23:699-705. 24. Knauth P. Changing schedules: shiftwork. Chonobiol Int 1997;14:159-171. 25. Goh VH, Tong TY, Lee LK. Sleep/wake cycle and circadian disturbances in shift work: strategies for their managementa review. Ann Acad Med Singapore 2000;29:90-96. 26. Czeisler CA, Moore-Ede MC, Coleman RH. Rotating shift work schedules that disrupt sleep are improved by applying circadian principles. Science 1982;217:460463. 27. Walsh JK, Muehlbach MJ, Schweitzer PK. Acute administration of triazolam for the daytime sleep of rotating shift workers. Sleep 1984;7:223-229.
DAlonzo and Krachman Circadian rhythm sleep disorders
JAOA Vol 100 No 8 Supplement to August 2000 S21
You might also like
- Major Depression GuideDocument8 pagesMajor Depression GuideLoren SangalangNo ratings yet
- Paranoia Is A Disturbed Thought Process Characterized by Excessive Anxiety or FearDocument11 pagesParanoia Is A Disturbed Thought Process Characterized by Excessive Anxiety or FearNaresh MaliNo ratings yet
- Hallucination PDFDocument10 pagesHallucination PDFfebriantinurulwNo ratings yet
- Basic Anatomy and Physiology of Brain and Spinal CordDocument59 pagesBasic Anatomy and Physiology of Brain and Spinal CorddrmalikarifNo ratings yet
- Psych EthicsDocument150 pagesPsych EthicsGonzalo LopezNo ratings yet
- Chapter 11 Skill Development Exercise Handling GrievancesDocument10 pagesChapter 11 Skill Development Exercise Handling GrievancesMushira AnsariNo ratings yet
- Facts and Myths About EpilepsyDocument10 pagesFacts and Myths About EpilepsyAarkayChandruNo ratings yet
- Interpreting Sleep StudyDocument55 pagesInterpreting Sleep StudySundar RamanathanNo ratings yet
- The Psychiatric Dimensions of Sleep Medicine2008, Vol.3, Issues 2, PDFDocument168 pagesThe Psychiatric Dimensions of Sleep Medicine2008, Vol.3, Issues 2, PDFRamon Alberto Portillo MedinaNo ratings yet
- Eeg, PSG, Sleep DisordersDocument48 pagesEeg, PSG, Sleep DisordersIoana MunteanuNo ratings yet
- Organisational Study Report - Mariyan DivyakarunyalayamDocument5 pagesOrganisational Study Report - Mariyan DivyakarunyalayamBimal AntonyNo ratings yet
- CRSDDocument4 pagesCRSDtaqinosNo ratings yet
- Diagnóstico dos transtornos do sono devido ao ritmo circadianoDocument8 pagesDiagnóstico dos transtornos do sono devido ao ritmo circadianosilveira_manuelNo ratings yet
- Circadian Rhythm: Effect of Circadian DisruptionDocument9 pagesCircadian Rhythm: Effect of Circadian DisruptionJoshua MarkosNo ratings yet
- Effects of Age On Circadian RhythmDocument4 pagesEffects of Age On Circadian RhythmJulie AmalaNo ratings yet
- Body Mind PsychtedliDocument7 pagesBody Mind Psychtedliapi-302965222No ratings yet
- Sleep DeprivationDocument15 pagesSleep DeprivationRengeline LucasNo ratings yet
- 7.sleep DisordersDocument41 pages7.sleep DisordersGERSON RYANTONo ratings yet
- Final Sleep 12Document27 pagesFinal Sleep 12AndresPimentelAlvarezNo ratings yet
- Parasomnias: Cleveland Clinic Sleep Disorders CenterDocument2 pagesParasomnias: Cleveland Clinic Sleep Disorders Centersavvy_as_98No ratings yet
- Sleep Disorders in the Elderly: Diagnosis and ImpactDocument22 pagesSleep Disorders in the Elderly: Diagnosis and ImpactJalajarani SelvaNo ratings yet
- Adult Sleep Disorders TreatmentDocument9 pagesAdult Sleep Disorders TreatmentCharmaine LowNo ratings yet
- 2 11 30 126Document5 pages2 11 30 126Desy SyahfitrianiNo ratings yet
- Sleep Disorders: Its Causes and TreatmentsDocument20 pagesSleep Disorders: Its Causes and TreatmentsBasari OdalNo ratings yet
- Insomnia: What Is Insomnia? What Causes It?Document4 pagesInsomnia: What Is Insomnia? What Causes It?Orive Ralina SegentaNo ratings yet
- Evaluationofthesleepy Patient:: Differential DiagnosisDocument12 pagesEvaluationofthesleepy Patient:: Differential DiagnosisDoina DoniciNo ratings yet
- Sleep Disorders Term PaperDocument4 pagesSleep Disorders Term Paperafdtorpqk100% (1)
- Insomnia and Alcohol and Substance Abuse: George E. Pataki, Gove Rnor Jean Some Rs Miller, CommissionerDocument6 pagesInsomnia and Alcohol and Substance Abuse: George E. Pataki, Gove Rnor Jean Some Rs Miller, Commissionerkim_peyoteNo ratings yet
- The Different Types of Sleeping DisordersDocument5 pagesThe Different Types of Sleeping DisordersRadee King CorpuzNo ratings yet
- Miss Sameera Shafiq: BS (Hons) Psychology 6th SemDocument12 pagesMiss Sameera Shafiq: BS (Hons) Psychology 6th SemMuzamilNo ratings yet
- Eating At Night Time: Sleep Disorders, Health and Hunger Pangs: Tips On What You Can Do About It: Eating DisordersFrom EverandEating At Night Time: Sleep Disorders, Health and Hunger Pangs: Tips On What You Can Do About It: Eating DisordersNo ratings yet
- SLEEP DISORDER GUIDEDocument2 pagesSLEEP DISORDER GUIDEIMANBADARNo ratings yet
- Lewis: Medical-Surgical Nursing, 10 Edition: Sleep and Sleep Disorders Key Points SleepDocument4 pagesLewis: Medical-Surgical Nursing, 10 Edition: Sleep and Sleep Disorders Key Points Sleepsophia onu100% (2)
- sleep paralysis and sleep walkingDocument23 pagessleep paralysis and sleep walkingGunjan NautiyalNo ratings yet
- What are circadian rhythms and how do they affect our healthDocument15 pagesWhat are circadian rhythms and how do they affect our healthGopika SNo ratings yet
- Preface Xi Nancy A. Collop: Number 3 JULY 2008Document4 pagesPreface Xi Nancy A. Collop: Number 3 JULY 2008Herbert Baquerizo VargasNo ratings yet
- Sleep Disorders: PathophysiologyDocument5 pagesSleep Disorders: PathophysiologyRodrigo Ehécatl Torres NevárezNo ratings yet
- Narcolepsy in ChildhoodDocument3 pagesNarcolepsy in ChildhoodNeo GoraNo ratings yet
- Unusual Behaviors During Sleep: The Parasomnias: Enuresis (Or Bed Wetting)Document2 pagesUnusual Behaviors During Sleep: The Parasomnias: Enuresis (Or Bed Wetting)savvy_as_98No ratings yet
- Sleep hygiene education efficacyDocument12 pagesSleep hygiene education efficacynilaahanifahNo ratings yet
- Sleep: Important Considerations in Management of PainDocument8 pagesSleep: Important Considerations in Management of PainMáximo Wladimir Viedma OlivaNo ratings yet
- Sleep: The secret to sleeping well and waking refreshedFrom EverandSleep: The secret to sleeping well and waking refreshedNo ratings yet
- Treatment of Primary InsomniaDocument8 pagesTreatment of Primary Insomniadanny17phNo ratings yet
- Guided Meditations for Anxiety, Insomnia and Sleep: Have a Full Night's Rest with Sleeping Techniques and Deep Relaxation, Which Can Help Adults and Kids Wake up More Happier and Become More Energized!From EverandGuided Meditations for Anxiety, Insomnia and Sleep: Have a Full Night's Rest with Sleeping Techniques and Deep Relaxation, Which Can Help Adults and Kids Wake up More Happier and Become More Energized!No ratings yet
- Iapp Naskar Sleep 2022Document45 pagesIapp Naskar Sleep 2022Dr. Subrata NaskarNo ratings yet
- Insomnia and Circadian Rhythm DisordersDocument50 pagesInsomnia and Circadian Rhythm DisordersRiyaSinghNo ratings yet
- Sleep: Regulation of Health Apps for Sleep Tracking (Guided Visualizations and Sleep Affirmations for Calm and Abundance in Anxious Artists)From EverandSleep: Regulation of Health Apps for Sleep Tracking (Guided Visualizations and Sleep Affirmations for Calm and Abundance in Anxious Artists)No ratings yet
- DSM IV Primary Sleep DisordersDocument3 pagesDSM IV Primary Sleep DisordersMada LinaNo ratings yet
- Sleep Disorders Treatment GuideDocument16 pagesSleep Disorders Treatment GuideNestor BalboaNo ratings yet
- Sleep Deprivation: What It Is and Why It Can Ruin Your LifeFrom EverandSleep Deprivation: What It Is and Why It Can Ruin Your LifeNo ratings yet
- Sleep Disorders: Review Neurology Series Editor, William J. Mullally, MDDocument8 pagesSleep Disorders: Review Neurology Series Editor, William J. Mullally, MDniNo ratings yet
- The Sleep Hack Handbook: Unlocking Secrets to Transform Your Nights for insomnia help: Unlocking Sweet Dreams: The Sleep Hack Handbook and Beyond, #1From EverandThe Sleep Hack Handbook: Unlocking Secrets to Transform Your Nights for insomnia help: Unlocking Sweet Dreams: The Sleep Hack Handbook and Beyond, #1No ratings yet
- Disturbed Sleep PatternDocument4 pagesDisturbed Sleep PatternTsaabitah AnwarNo ratings yet
- RESTORE YOUR SLEEP Practical techniques and exercises to sleep better and heal insomnia.From EverandRESTORE YOUR SLEEP Practical techniques and exercises to sleep better and heal insomnia.No ratings yet
- The Visually ImpairedDocument21 pagesThe Visually ImpairedAnanthi balaNo ratings yet
- Feder 2021Document16 pagesFeder 2021Kerstine Anne AndradeNo ratings yet
- Unit 6 Sleep DisorderDocument57 pagesUnit 6 Sleep DisorderadhikarisujataNo ratings yet
- Biology PDFDocument1,447 pagesBiology PDFPrincess Ethel Atillo100% (2)
- Nutritional Management of High Output Enterocutaneous FistulaDocument2 pagesNutritional Management of High Output Enterocutaneous FistulaAfra AmiraNo ratings yet
- Effects of Electromagnetic Forces of Earth On HumansDocument6 pagesEffects of Electromagnetic Forces of Earth On HumansArtist MetuNo ratings yet
- The Relativistic Brain by Ronald Cicurel and Miguel L. Nicolelis (2015)Document5 pagesThe Relativistic Brain by Ronald Cicurel and Miguel L. Nicolelis (2015)Sinem SerapNo ratings yet
- Assignment Lec 4Document3 pagesAssignment Lec 4morriganNo ratings yet
- Photosynthesis Question Booklet: Name . .Document16 pagesPhotosynthesis Question Booklet: Name . .ajithaNo ratings yet
- FORENSIC SEROLOGY AND BLOOD ANALYSISDocument16 pagesFORENSIC SEROLOGY AND BLOOD ANALYSISBARCELON, CHRISTOPHER JAMESNo ratings yet
- January 2016 (IAL) QP - Unit 1 Edexcel Biology A-LevelDocument24 pagesJanuary 2016 (IAL) QP - Unit 1 Edexcel Biology A-LevelkirthikaNo ratings yet
- CSIR UGC JRF Subjetive Model Test PaperDocument17 pagesCSIR UGC JRF Subjetive Model Test PaperManu Mallahalli ShanthappaNo ratings yet
- ReadingsDocument246 pagesReadingsFul WgNo ratings yet
- 8 Science NCERT Solutions Chapter 10Document7 pages8 Science NCERT Solutions Chapter 10Raj Anand100% (1)
- Science: Quarter 1 - Module 1Document10 pagesScience: Quarter 1 - Module 1RUTH PIANGNo ratings yet
- NURSING CARE PLAN The Child Undergoing Surgery For ScoliosisDocument3 pagesNURSING CARE PLAN The Child Undergoing Surgery For ScoliosisscrewdriverNo ratings yet
- Anesthesiology Resident Survival Guide 2014-2015Document32 pagesAnesthesiology Resident Survival Guide 2014-2015Karla Matos100% (1)
- 3 PBDocument12 pages3 PBDumitruNo ratings yet
- BioSignature Review - Are Hormones The Key To Weight LossDocument19 pagesBioSignature Review - Are Hormones The Key To Weight LossVladimir OlefirenkoNo ratings yet
- Comparative Study The Effect of Induction of General Anesthesia With Propofol Versus Thiopentone in Pediatric Age Group On Cardiovascular SystemDocument8 pagesComparative Study The Effect of Induction of General Anesthesia With Propofol Versus Thiopentone in Pediatric Age Group On Cardiovascular SystemCentral Asian StudiesNo ratings yet
- IlizarovDocument62 pagesIlizarovAsh Moaveni100% (2)
- Center For Prehospital Care: Benjamin E. EsparzaDocument10 pagesCenter For Prehospital Care: Benjamin E. EsparzasenjahipgabiNo ratings yet
- Fuel Metabolism in StarvationDocument27 pagesFuel Metabolism in Starvationilluminel100% (2)
- Tetralogy of Fallot Everything You Wanted To Know But Were Afraid To AskDocument8 pagesTetralogy of Fallot Everything You Wanted To Know But Were Afraid To AsksofiaNo ratings yet
- Circulatory System: Heart, Blood Vessels & Their FunctionsDocument17 pagesCirculatory System: Heart, Blood Vessels & Their FunctionskangaanushkaNo ratings yet
- Posture and AlignmentDocument1 pagePosture and AlignmentNell KeeneNo ratings yet
- SP FinalDocument18 pagesSP Finalapi-344954734No ratings yet
- The Normal Anterior Inferior Cerebellar ArteryDocument19 pagesThe Normal Anterior Inferior Cerebellar Artery16fernandoNo ratings yet
- Management of Clients With Disturbances in OxygenationDocument13 pagesManagement of Clients With Disturbances in OxygenationClyde CapadnganNo ratings yet
- Nutrition in Plants and AnimalsDocument3 pagesNutrition in Plants and AnimalsHaris Ur RehmanNo ratings yet
- 12 SexualQigongDocument6 pages12 SexualQigongAnonymous r84IzwCNo ratings yet
- Anatomy and Physiology-REVIEWER-Practical ExamDocument12 pagesAnatomy and Physiology-REVIEWER-Practical ExamDeity Ann ReuterezNo ratings yet
- Basic Anatomical Terms PPTDocument30 pagesBasic Anatomical Terms PPTInsatiable Clee100% (1)