Professional Documents
Culture Documents
Drugs in Pediatrics
Uploaded by
Karla SanchezCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Drugs in Pediatrics
Uploaded by
Karla SanchezCopyright:
Available Formats
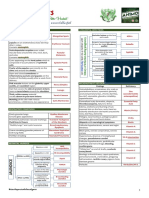
Drugs in Pediatrics NMT11
www.MedadTeam.org 1
Respiratory
TB TB TB TB
Treatment Treatment Treatment Treatment: :: :
Combined drug therapy for Long time: 2 22 2 to to to to 3 33 3 first line drugs for at least 6 66 6- -- -9 99 9 months months months months.
1 11 1- -- - First line drugs are First line drugs are First line drugs are First line drugs are: : : :
Dose Dose Dose Dose Route Route Route Route Side effect Side effect Side effect Side effect
Isoniazid Isoniazid Isoniazid Isoniazid 10-20 mg/kg/day orally Hepatotoxicity
Rifampicin Rifampicin Rifampicin Rifampicin 10-20 mg/kg/day orally Hepatotoxicity
Pyrazinamide Pyrazinamide Pyrazinamide Pyrazinamide 20 20 20 20- -- -40 40 40 40 mg/kg/day orally Hepatotoxicity
2 22 2- -- - Second line drugs are: Second line drugs are: Second line drugs are: Second line drugs are:
Dose Dose Dose Dose Route Route Route Route Side effect Side effect Side effect Side effect
Ethambutol Ethambutol Ethambutol Ethambutol 10-20 mg/kg/day orally
Ethionamide Ethionamide Ethionamide Ethionamide 10-20 mg/kg/day orally
Streptomycin Streptomycin Streptomycin Streptomycin 20 20 20 20- -- -40 40 40 40 mg/kg/day IM IM IM IM Ototoxicity, Nephrotoxicity Ototoxicity, Nephrotoxicity Ototoxicity, Nephrotoxicity Ototoxicity, Nephrotoxicity
Kanamycin Kanamycin Kanamycin Kanamycin
Bronchial Bronchial Bronchial Bronchial asthma asthma asthma asthma
TTT of acute attack: TTT of acute attack: TTT of acute attack: TTT of acute attack:
A AA A- -- -Acute mild to moderate attack Acute mild to moderate attack Acute mild to moderate attack Acute mild to moderate attack: :: :
1 11 1- -- -Bronchodilators Bronchodilators Bronchodilators Bronchodilators:
Dose Dose Dose Dose Route Route Route Route Action Action Action Action
B BB B- -- -agonist: agonist: agonist: agonist:
Salbutamol, Salbutamol, Salbutamol, Salbutamol,
Terbutaline, Terbutaline, Terbutaline, Terbutaline,
Fenoterol Fenoterol Fenoterol Fenoterol
0.1-0.2 mg/kg/d - Orally in mild attack
- Nebulizer for infants and
young children
- Inhalers for older children
Selective B
agonist
Theophylline Theophylline Theophylline Theophylline
(methylxanthine (methylxanthine (methylxanthine (methylxanthine
derivatives) derivatives) derivatives) derivatives)
15-20 mg/kg/d orally or rectally
direct
relaxation of
bronchial
Sm.Ms
Anticholinergic: Anticholinergic: Anticholinergic: Anticholinergic:
Ipratropium Ipratropium Ipratropium Ipratropium
250 microgram/dose,
4times daily
Inhalation Reduce the
intrinsic vagal
tone
2 22 2- -- -Corticosteriods Corticosteriods Corticosteriods Corticosteriods:
In moderate or severe cases orally or parenterally orally or parenterally orally or parenterally orally or parenterally (anti-inflammatory and interfere with
synthesis of LKs& PGs)
N.B: N.B: N.B: N.B: Mild cases>>one or 2 bronchodilators are given, inhaled bronchodilator are the best
Moderate cases>>inhaled bronchodilator and oral corticosteroids can be used
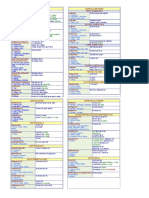
Drugs in Pediatrics NMT11
www.MedadTeam.org 2
B BB B- -- -Acute severe attack (status asthmatics) Acute severe attack (status asthmatics) Acute severe attack (status asthmatics) Acute severe attack (status asthmatics): :: :
-Drugs:
Dose Dose Dose Dose Route Route Route Route
Intermittent B Intermittent B Intermittent B Intermittent B2 22 2 agonist agonist agonist agonist
nebulized Salbutamol nebulized Salbutamol nebulized Salbutamol nebulized Salbutamol
0.25-0.5 ml added to 2-3 ml saline every 1-2 h inhalation
theophylline theophylline theophylline theophylline 5 mg/k/6 hr IV slowly
hydrocortisone hydrocortisone hydrocortisone hydrocortisone 5-10mg/kg/6 hr IV
Preventive TTT in between attacks Preventive TTT in between attacks Preventive TTT in between attacks Preventive TTT in between attacks:
Anti Anti Anti Anti- -- -inflammatory drugs inflammatory drugs inflammatory drugs inflammatory drugs: it is indicated in persistant asthma
1 11 1- -- -Corticosteriods: Corticosteriods: Corticosteriods: Corticosteriods:
Dose Dose Dose Dose Route Route Route Route
beclomethazone beclomethazone beclomethazone beclomethazone 200-800 microgram/d (4 doses/d) inhaled
Budesinide Budesinide Budesinide Budesinide 200-800 microgram/d (2 doses)
Fluticasone Fluticasone Fluticasone Fluticasone 100-500 microgram/d (2 doses)
Prednisone Prednisone Prednisone Prednisone 2mg/kg/d divided doses for 3-10 days oral
2 22 2- -- -Antileukotrines Antileukotrines Antileukotrines Antileukotrines:
Dose Dose Dose Dose Route Route Route Route
Montelukast (Singulair) Montelukast (Singulair) Montelukast (Singulair) Montelukast (Singulair) 5-10mg (once daily) orally
3 33 3- -- -Mast cell stabilizers Mast cell stabilizers Mast cell stabilizers Mast cell stabilizers:
Dose Dose Dose Dose Route Route Route Route
Ketotifen Ketotifen Ketotifen Ketotifen 0.06mg/kg/d orally
Na cromoglycate Na cromoglycate Na cromoglycate Na cromoglycate 5-20mg/dose (3-4 doses/d) inhalation
Cardiology
Rheumatic fever Rheumatic fever Rheumatic fever Rheumatic fever
1 11 1- -- -Prevention Prevention Prevention Prevention: (very imp.)
- Prevention of streptococcal infection e.g. proper ventilation
- Early diagnosis of strept. Pharyngitis , then,
- Adequate TTT by:
Benzathine penicillin Benzathine penicillin Benzathine penicillin Benzathine penicillin 1,200,000 IM single injection
OR
Benzathine penicillin Benzathine penicillin Benzathine penicillin Benzathine penicillin 1,200,000 oral at least 10 d
In Allergic Pt.
- Prevention of rheumatic activity in pts with history if R.F.:
Erythromycine Erythromycine Erythromycine Erythromycine 50mg/kg/d
Drugs in Pediatrics NMT11
www.MedadTeam.org 3
Benzathine penicillin Benzathine penicillin Benzathine penicillin Benzathine penicillin 1,200,000 IM every 2-3 weeks for life
2 22 2- -- -Supportive TTT Supportive TTT Supportive TTT Supportive TTT:
- Rest: pts with carditis should have absolute bed rest for at least 4 weeks,
Daily examination is important to detect carditis that usually present within 2w of onset
3 33 3- -- -Specific TTT Specific TTT Specific TTT Specific TTT:
A AA A- -- -Arthritis only Arthritis only Arthritis only Arthritis only (or carditis without cardiomgaly):
Salicylates Salicylates Salicylates Salicylates 100mg/kg for 2w then 74mg/kg for 4-6 w
B BB B- -- -Carditis with cardiomegaly or failure Carditis with cardiomegaly or failure Carditis with cardiomegaly or failure Carditis with cardiomegaly or failure:
Prednisone Prednisone Prednisone Prednisone 2mg/kg/d for 2-3w then taper
Salicylates Salicylates Salicylates Salicylates 75mg/kg/d during tapering 1m after stopping Prednisone
C CC C- -- -Chorea Chorea Chorea Chorea:
Phenobarbitone Phenobarbitone Phenobarbitone Phenobarbitone 3-5 mg/kg/d
Haloperidol Haloperidol Haloperidol Haloperidol 0.02-0.1 mg/kg/d (in pts over 12 years)
4 44 4- -- -TTT of complications TTT of complications TTT of complications TTT of complications: H.F
- Mild cases: complete bed rest, o2, fluid restrictions and steroids
- Sever cases:
Dose Dose Dose Dose Action Action Action Action
furosemide furosemide furosemide furosemide 2mg/kg/d Preload reducing agents
(diuretics)
digoxin digoxin digoxin digoxin Digitalizing dose : 0.02-0.05 mg/kg Inotropes
maintenance dose: 0.01 mg/kg/d
captopril captopril captopril captopril may be given After load reducing agents
Infective endocarditis Infective endocarditis Infective endocarditis Infective endocarditis
Prevention Prevention Prevention Prevention
Dental procedures and surgery:
Dose Dose Dose Dose Route Route Route Route Timing Timing Timing Timing
Amoxicillin Amoxicillin Amoxicillin Amoxicillin 50mg/kg (single large dose) oral 1 h. before the procedure
Specific Specific Specific Specific: immediate parenteral antibiotic for 6 weeks
Dose Dose Dose Dose Route Route Route Route Duration Duration Duration Duration
Penicillin G Penicillin G Penicillin G Penicillin G 300000 IU/kg/day
parenteral
for 6 weeks
Oxacillin Oxacillin Oxacillin Oxacillin 200mg/kg/day
Gentamicin Gentamicin Gentamicin Gentamicin 2 mg/kg/day
=This treatment is modified according to the results of blood culture
Drugs in Pediatrics NMT11
www.MedadTeam.org 4
Hepatology
Chronic hepatitis Chronic hepatitis Chronic hepatitis Chronic hepatitis
Antiviral drugs Antiviral drugs Antiviral drugs Antiviral drugs in chronic HBV, HCV have limited response (25%)
Immunosuppressive (e.g. corticosteroids Immunosuppressive (e.g. corticosteroids Immunosuppressive (e.g. corticosteroids Immunosuppressive (e.g. corticosteroids- -- -azathioprine azathioprine azathioprine azathioprine) in autoimmune hepatitis
D DD D- -- -penicillamine (copper chelating agent) in Wilson disease. penicillamine (copper chelating agent) in Wilson disease. penicillamine (copper chelating agent) in Wilson disease. penicillamine (copper chelating agent) in Wilson disease. It is the only curable chronic
liver disease and it should be excluded in every case of chronic hepatitis
Liver implantation Liver implantation Liver implantation Liver implantation in end stage liver disease
Cholestasis Cholestasis Cholestasis Cholestasis
1 11 1- -- - Treatment of correctable conditions Treatment of correctable conditions Treatment of correctable conditions Treatment of correctable conditions
Antibiotics for septicemia.
Elimination of lactose from diet in galactosemia
Surgical treatment of Choledochal cyst
2 22 2- -- - Extrahepatic biliary atresia Extrahepatic biliary atresia Extrahepatic biliary atresia Extrahepatic biliary atresia
Correctable lesion (rare): direct drainage.
No correctable lesion: kasia (hepatoportoenterostomy).it should be done before 60 days
to obtain best results.
Liver transplantation for end stage liver disease ( biliary atresia is the commonest
indication )
3 33 3- -- - Sup Sup Sup Supportive treatment portive treatment portive treatment portive treatment
Nutritional support Nutritional support Nutritional support Nutritional support
Fat soluble vitamins defeciency is replaced by synthetic water soluble preparations
(e.g. for vit A and K) active vit D and vit E is given by injection .
Medium chain triglycerides containing formulas.
Calcium, zinc and Phosphorus.
Pruritus Pruritus Pruritus Pruritus
Phenobarbitone
Cholestramine ( bile acid binder )
Portal hypertension Portal hypertension Portal hypertension Portal hypertension
1 11 1- -- - Management of variceal hemorrhage Management of variceal hemorrhage Management of variceal hemorrhage Management of variceal hemorrhage: :: :
Emergency therapy for bleeding varices Emergency therapy for bleeding varices Emergency therapy for bleeding varices Emergency therapy for bleeding varices: :: :
. Anti shock measures: blood transfusion, intravenous fluids.
. Correction of coagulopathy: vitamin k, fresh plasma, platelets transfusion
. Nasogastric tube placement
. Vasopressin infusion if bleeding persist
Emergency endoscopy Emergency endoscopy Emergency endoscopy Emergency endoscopy and either injection sclerotherapy or band ligation
Emergency shunt Emergency shunt Emergency shunt Emergency shunt: : : : protosystemic shunt
2 22 2- -- - Prevention of bleeding from varices Prevention of bleeding from varices Prevention of bleeding from varices Prevention of bleeding from varices: :: :
Prevention of the first attack of bleeding Prevention of the first attack of bleeding Prevention of the first attack of bleeding Prevention of the first attack of bleeding
. Avoid aspirin and non steroid anti inflammatory drugs
. B adrenergic blockers (propranolol) to lower the pressure in portal area
. Prophylactic sclerotherapy or band ligation
Drugs in Pediatrics NMT11
www.MedadTeam.org 5
prevention of re prevention of re prevention of re prevention of re- -- - bleeding bleeding bleeding bleeding: in addition to above measures, the following may needed: : in addition to above measures, the following may needed: : in addition to above measures, the following may needed: : in addition to above measures, the following may needed:
. Surgical protosystemic shunt. .Liver transplantation.
Nephrology
Minimal change nephrotic syndrome Minimal change nephrotic syndrome Minimal change nephrotic syndrome Minimal change nephrotic syndrome
E Home management Home management Home management Home management: : : : for most cases
E Hospitalization Hospitalization Hospitalization Hospitalization: : : : indicated for the first attack or relapses with marked edema
1 11 1- -- - Supportive treatment Supportive treatment Supportive treatment Supportive treatment: :: :
. . . . Diet Diet Diet Diet: : : : rich in protein to compensate for protein loss & salt free
Fluid restriction is indicated only in moderate or severe cases of edema
. . . . Bed rest Bed rest Bed rest Bed rest: : : : is not indicated & children with mild edema can attend school
2 22 2- -- - Specific treatment Specific treatment Specific treatment Specific treatment: :: :
Control of edema Control of edema Control of edema Control of edema: :: :
> Mild edema: > Mild edema: > Mild edema: > Mild edema: salt free diet is sufficient
> Moderate edema: > Moderate edema: > Moderate edema: > Moderate edema: diuretics (Furosemide) 1-2 mg/kg/day
Furosemide Furosemide Furosemide Furosemide 1-2 22 2 mg/kg/day diuretics
> Marked edema: > Marked edema: > Marked edema: > Marked edema: intravenous salt free albumin followed by Furosemide
Steroids Steroids Steroids Steroids: :: :
Induction or remission Induction or remission Induction or remission Induction or remission: Daily therapy : Daily therapy : Daily therapy : Daily therapy
Prednisone Prednisone Prednisone Prednisone 2 22 2 mg/kg/day (60 mg/m
2
/day) divided into 3-4 doses
Respose: urine becomes free of albumin usually occurs after 2 weeks. Therapy is continued
for 1 week after that
No respose after 1 month: Steroid resistant (renal biopsy is indicated)
Minimal Minimal Minimal Minimal lesion lesion lesion lesion type type type type usually usually usually usually gives gives gives gives excellent excellent excellent excellent respose respose respose respose to to to to corticosteroids corticosteroids corticosteroids corticosteroids
Maintenance of remission Maintenance of remission Maintenance of remission Maintenance of remission: Alternate day therapy : Alternate day therapy : Alternate day therapy : Alternate day therapy
For those For those For those For those who responded to prednisone who responded to prednisone who responded to prednisone who responded to prednisone
Prednisone Prednisone Prednisone Prednisone 2 22 2 mg/kg/day single morning dose after breakfast every other day for 3-6 ms
Relapses Relapses Relapses Relapses: :: : Relapse is the recurrence of edema. It is treated as the initial attack but
alternate day therapy is continued for longer period ( (( (6 66 6- -- -12 12 12 12 months) months) months) months)
Cyclophosphamide Cyclophosphamide Cyclophosphamide Cyclophosphamide 2 22 2-3 mg/kg/day single dose for 8 weeks
- in steroid resistant and in cases with frequent relapses
- alternate day therapy with low prednisone is continued during therapy
- Total leucocytic count is monitored every week (stop therapy if count drops below
3000/mm
3
3 33 3- -- - Treatment of complications: treatment of infections Treatment of complications: treatment of infections Treatment of complications: treatment of infections Treatment of complications: treatment of infections
. Antibiotics: . Antibiotics: . Antibiotics: . Antibiotics: Penicillin Penicillin Penicillin Penicillin for urgent treatment of any suspected infections (peritonitis & skin
infections)
Acute poststreptococcal glomerulonephritis Acute poststreptococcal glomerulonephritis Acute poststreptococcal glomerulonephritis Acute poststreptococcal glomerulonephritis
E Home management Home management Home management Home management: :: : for most cases. More than 95 5 of cases will recover completely within
few weeks & even without therapy
Drugs in Pediatrics NMT11
www.MedadTeam.org 6
E Hospitalization Hospitalization Hospitalization Hospitalization: :: : for cases complicated with severe hypertension, marked congestion or severe
renal failure
Supporative treatment: Supporative treatment: Supporative treatment: Supporative treatment:
- Rest Rest Rest Rest: indicated only during the oliguria phase of illness (first week)
- Diet Diet Diet Diet:
High carbohydrate diet High carbohydrate diet High carbohydrate diet High carbohydrate diet
Salt & protein restriction Salt & protein restriction Salt & protein restriction Salt & protein restriction during the oliguria phase and in the presence of
complications e.g: hypertension & marked congestion
Fluid balance: Fluid balance: Fluid balance: Fluid balance: amount of fluids/day = urine output of the previous day + insensible
water loss (400cc/m
2
)
Specific treatment: Specific treatment: Specific treatment: Specific treatment:
- Control of edema Control of edema Control of edema Control of edema:
. In most cases edema subsides spontaneously by the end of the first week. Fluid
restriction & salt restriction during the first week are usually sufficient
. Diuretics e.g: Frusemide Frusemide Frusemide Frusemide, in some cases
- Control of hypertension Control of hypertension Control of hypertension Control of hypertension (when diastolic pressure exceeds 95 mmHg- usually one oral
antihypertensive drugs is sufficient)
Captopril Captopril Captopril Captopril 0.5-1 mg/kg/day divided into 3-4 doses) ACE Inhibitor
B blockers B blockers B blockers B blockers
- For eradication of any streptococcal infection
Penicillin Penicillin Penicillin Penicillin oral 10 days course
Treatment of complications: Treatment of complications: Treatment of complications: Treatment of complications:
Renal failure Renal failure Renal failure Renal failure diuretics, fluid restriction, treatment of acidosis, dialysis)
Heart failure Heart failure Heart failure Heart failure Dopamine not digitalis
Hypertensive Hypertensive Hypertensive Hypertensive
encephalopathy encephalopathy encephalopathy encephalopathy
I.V. Diazoxide
Chronic renal failure Chronic renal failure Chronic renal failure Chronic renal failure
Periodic clinical evaluation Periodic clinical evaluation Periodic clinical evaluation Periodic clinical evaluation: nutritional status, growth, blood pressure, cariac function &
skeletal examination for rachitic changes
Laboratory evaluation Laboratory evaluation Laboratory evaluation Laboratory evaluation: blood urea, creatinine, acid base status-serum electrolytes (Na,K,Ca,P)
hemoglobin level & radiological examination of bones for evidence of rachitic changes
Measurement of glomerular filtration rate Measurement of glomerular filtration rate Measurement of glomerular filtration rate Measurement of glomerular filtration rate: is important to determine the degree of renal
insufficiency:
. Values between 20-30 ml/min/m
2
: manifestations of renal failure appear
. Values below 10 ml/min/m
2
denote severe renal insufficiency
1- Conservative measures Conservative measures Conservative measures Conservative measures: mild to moderate cases of renal insufficieny with GFR above 10
ml/min/m
2
- Diet Diet Diet Diet:
. Carbohydrate & fat: Carbohydrate & fat: Carbohydrate & fat: Carbohydrate & fat: allowed freely to provide sufficient calories
. Protein restriction Protein restriction Protein restriction Protein restriction to dercearse the nitrogenous waste products
. Salt restriction Salt restriction Salt restriction Salt restriction in cases with hypertension
- Drugs Drugs Drugs Drugs:
Drugs in Pediatrics NMT11
www.MedadTeam.org 7
Rickets Rickets Rickets Rickets active form of Vitamin D
Growth failure Growth failure Growth failure Growth failure feeding regimen-growth hormone therapy
H HH Hypertension ypertension ypertension ypertension salt restriction, oral furosemide & anti-hypertensive drugs
H HH Hyperphsphatemia & yperphsphatemia & yperphsphatemia & yperphsphatemia &
h hh hypocalcemia ypocalcemia ypocalcemia ypocalcemia
> Oral calcium supplementation
> Vit D therapy
> Oral aluminium hydroxide
A AA Anaemia naemia naemia naemia erythropoietin & packed RBCs
A AA Acidosis cidosis cidosis cidosis oral NaHco
3
A AA Antibiotics ntibiotics ntibiotics ntibiotics for severe urinary tract infection or severe systemic infections as it
may precipitate an episode of acute renal failure
2- Dialysis Dialysis Dialysis Dialysis: severe renal insufficiency with GFR below 10 ml/min/m
2
or when conservation
measures are no longer effective
- Peritoneal (continous ambulatory or chronic cycling)
- Hemodialysis
3- Renal transplantation Renal transplantation Renal transplantation Renal transplantation:
- It is the ideal therapy for children with severe renal insufficiency
- It can be carried out in children above the age of 5 years
- Problems limiting its application include: graft rejection, finding suitable donor
Urinary tract infection Urinary tract infection Urinary tract infection Urinary tract infection
Proper antibiotics according to culture and sensitivity
1 11 1. .. . Acute cases Acute cases Acute cases Acute cases:
Pyelonephritis Pyelonephritis Pyelonephritis Pyelonephritis:
Drugs Drugs Drugs Drugs Dose Dose Dose Dose Route Route Route Route
Gentamicxin Gentamicxin Gentamicxin Gentamicxin
ampicillin ampicillin ampicillin ampicillin
4 mg/kg/day
100 mg/kg/day
IV initially then shift to oral therapy
after 5 days if the patient is improving
Duration of therapy 10-14 days
Urine should be sterile within 48 hours of adequate therapy
Cystitis Cystitis Cystitis Cystitis:
Drugs Drugs Drugs Drugs Dose Dose Dose Dose Route Route Route Route
Amoxicillin or co Amoxicillin or co Amoxicillin or co Amoxicillin or co- -- -trimoxazol trimoxazol trimoxazol trimoxazol 50 mg/kg/day oral
For 7-10 days
Treatment can be adjusted according to the results of urine culture and sensitivity
2 22 2. .. . Recurrent cases Recurrent cases Recurrent cases Recurrent cases: After eradication of infection the following should be done:
- Suppressive therapy with co-trimoxazol (Trimethoprim-sulfamethoxazole) given in lower
dose (one third of usual therapeutic dose)
- Adequate fluid intake
- Frequent voiding
- Avoid constipation
Nocturnal enuresis Nocturnal enuresis Nocturnal enuresis Nocturnal enuresis
- Identification & treatment of organic causes organic causes organic causes organic causes e.g. urinary tract infection & polyuria
Simple measures in children above Simple measures in children above Simple measures in children above Simple measures in children above 4 44 4 years years years years:
Drugs in Pediatrics NMT11
www.MedadTeam.org 8
- Fluid restriction after dinner
- Let the child urinate before sleep
- Wake the child up by night to urinate
- Rewarding for dry night
- Punishment should be avoided
Drug therapy in children above Drug therapy in children above Drug therapy in children above Drug therapy in children above 6 66 6 years years years years:
Oxybutyrin Oxybutyrin Oxybutyrin Oxybutyrin Anticholinergic drugs increase bladder capacity
Desmopressin Desmopressin Desmopressin Desmopressin vasopressin analog single night dose 0.1-0.2 mg
Alarm device Alarm device Alarm device Alarm device it gives a ring immediately at the beginning of wetting so the child can wake up
for urination
Neurology
Epilepsy Epilepsy Epilepsy Epilepsy
I- Treatment of the ongoing seizures or treatment of status epilepticus Treatment of the ongoing seizures or treatment of status epilepticus Treatment of the ongoing seizures or treatment of status epilepticus Treatment of the ongoing seizures or treatment of status epilepticus.
First aid measures First aid measures First aid measures First aid measures
- Patent airway - O
2
- IV line
Immediate anticonvulsant drugs Immediate anticonvulsant drugs Immediate anticonvulsant drugs Immediate anticonvulsant drugs
Diazepam Diazepam Diazepam Diazepam 0.3-0.5 mg/kg IV or rectal
Phenobarbitone Phenobarbitone Phenobarbitone Phenobarbitone 10-15 mg/kg (loading dose) that can be repeated
5 mg/kg (maintenance dose) after seizure control
If phenobarbitone failed to control the seizures shift to other drugs
Phenytoin Phenytoin Phenytoin Phenytoin 15-20 mg/kg (loading dose)
5 mg/kg/day (maintenance)
Na valproate Na valproate Na valproate Na valproate 20-40 mg rectally
II II II II- -- - Prevention of recurrence by antiepileptic drugs Prevention of recurrence by antiepileptic drugs Prevention of recurrence by antiepileptic drugs Prevention of recurrence by antiepileptic drugs
- Drugs Drugs Drugs Drugs:
Drug Drug Drug Drug Seizure type Seizure type Seizure type Seizure type Dose(mg/kg/day) Dose(mg/kg/day) Dose(mg/kg/day) Dose(mg/kg/day)
1 11 1- -- - Sodium valproate Sodium valproate Sodium valproate Sodium valproate
- Generalized seizures:
Tonic clonic, Absence and myoclonic
- Partial seizures
10-40
2 22 2- -- - Carbamazepine Carbamazepine Carbamazepine Carbamazepine
- Partial seizures: the best in partial seizures
- Generalized tonic clonic
10-30
3 33 3- -- - Phenobarbitone Phenobarbitone Phenobarbitone Phenobarbitone
- Generalized tonic clonic
- Partial seizures
3-5
4 44 4- -- - Phenytoin Phenytoin Phenytoin Phenytoin As phenobarbitone 5-8
5 55 5- -- - Clonazepam Clonazepam Clonazepam Clonazepam
- Myoclonic
- Infantile spasms
0.05-0.1
6 66 6- -- - Ethosuximide Ethosuximide Ethosuximide Ethosuximide
- absence
- Myoclonic
20-40
Drugs in Pediatrics NMT11
www.MedadTeam.org 9
7 77 7- -- - Vigabatrin Vigabatrin Vigabatrin Vigabatrin
- Partial
- Infantile spasms
40-80
8 88 8- -- - Lamotrigine Lamotrigine Lamotrigine Lamotrigine - Atypical absence seizures 5-10
9 99 9- -- - Topiramate Topiramate Topiramate Topiramate - Partial seizures 5-10
10 10 10 10- -- - Corticosterioids Corticosterioids Corticosterioids Corticosterioids
and ACTH and ACTH and ACTH and ACTH
- Infantile spasms, myoclonic seizures
- Symptomatic intractable seizures
- I II Important mportant mportant mportant rules rules rules rules for long term drug therapy for long term drug therapy for long term drug therapy for long term drug therapy
1- Initiation of therapy only after accurate diagnosis.
2- Choice of drugs according to clinical and EEG findings.
3- Number of drugs: start with one drug in small dose (to avoid toxicity and improve
compliance) then increases gradually until seizure control or maximum dose is reached
. Failure of the first drug is an indication to add the second drug.
4- Duration and termination of therapy
At least 2 years after the child is being seizure free termination should be gradually.
5- Patent counseling
Avoid watching TV except in lighted room and far enough from the screen.
Computer games should be done under supervision
Meningitis Meningitis Meningitis Meningitis
1 11 1- -- - Prevention Prevention Prevention Prevention
- -- - Vaccination Vaccination Vaccination Vaccination
Infants in the first year of life:- HIB vaccine HIB vaccine HIB vaccine HIB vaccine 3 33 3 doses doses doses doses (against Hemophilus influenza)
Children:- Meningococcal polysaccharide vaccine (A and C) at Meningococcal polysaccharide vaccine (A and C) at Meningococcal polysaccharide vaccine (A and C) at Meningococcal polysaccharide vaccine (A and C) at 3 33 3 years years years years
- -- - Chemoprophylaxis Chemoprophylaxis Chemoprophylaxis Chemoprophylaxis
Rifampicin Rifampicin Rifampicin Rifampicin used to eradicate meningococci from the nasopharynx of carriers and
minimize the risk of contact infection.
2 22 2- -- - Supportive treatment Supportive treatment Supportive treatment Supportive treatment
- -- - I.V fluid I.V fluid I.V fluid I.V fluid if meningitis is complicated by shock (otherwise it should be restricted to minimize
cerebral edema)
- Blood transfusion for cases with DIC
- Anticonvulsants: diazepam and phenoparbitone diazepam and phenoparbitone diazepam and phenoparbitone diazepam and phenoparbitone
3 33 3- -- - Specific treatment: antibiotics Specific treatment: antibiotics Specific treatment: antibiotics Specific treatment: antibiotics
Neonates 3 weeks Initial antibiotics should be active against
haemophilus influenzae type b, streptococci haemophilus influenzae type b, streptococci haemophilus influenzae type b, streptococci haemophilus influenzae type b, streptococci
and menin and menin and menin and meningococci gococci gococci gococci, then modified according
to the result of culture and sensitivity tests
IV IV IV IV for at least
10 10 10 10- -- - 14 14 14 14 days days days days
Neonates and infants younger
than 2 months
Cefotriaxone Cefotriaxone Cefotriaxone Cefotriaxone 100 100 100 100 mg kg/day mg kg/day mg kg/day mg kg/day,
Chloramphenicol Chloramphenicol Chloramphenicol Chloramphenicol 100 100 100 100 mg kg/day mg kg/day mg kg/day mg kg/day,
Ampicillin Ampicillin Ampicillin Ampicillin 100 100 100 100 mg kg/day mg kg/day mg kg/day mg kg/day,
Infants and children older than
2 months
Third generation cephalosporin and cephalosporin and cephalosporin and cephalosporin and
chloramphenicol chloramphenicol chloramphenicol chloramphenicol
E N.B Corticosteroids for H influenza improve CSF findings and decrease the incidence of
hearing loss
Drugs in Pediatrics NMT11
www.MedadTeam.org 10
4 44 4- -- - Treatment of complications Treatment of complications Treatment of complications Treatment of complications
Assisted ventilation if respiratory failure occurs.
Subdural taps to evacuate extensive subdural effusions
5 55 5- -- - Follow up after treatment Follow up after treatment Follow up after treatment Follow up after treatment
.Children who have meningitis should have a complete neurological evaluation at the time of
discharge (vision, hearing and developmental assessment).
. Periodic follow up for at least 2 years is recommended.
Nutritional disorders
Protein energy malnutrition Protein energy malnutrition Protein energy malnutrition Protein energy malnutrition
Prevention of protein energy malnutrition Prevention of protein energy malnutrition Prevention of protein energy malnutrition Prevention of protein energy malnutrition
1 11 1- -- - Breast feeding Breast feeding Breast feeding Breast feeding promotion (it is the most important)
Enumerate factors important for successful breast feeding
2 22 2- -- - Health education Health education Health education Health education of the mother about infant feeding
3 33 3- -- - Assessment of nutritional status Assessment of nutritional status Assessment of nutritional status Assessment of nutritional status during infancy in every visit for earlier diagnosis of nutritional
deficiency disorders
Management of protein energy malnutrition Management of protein energy malnutrition Management of protein energy malnutrition Management of protein energy malnutrition
1 11 1- -- -Hospital management Hospital management Hospital management Hospital management
Indication
. 3
rd
degree marasmus
. Kwashiorkor or marasmic kwashiorkor (edema)
. Infections e.g. pneumonia, diarrhea
Treatment of life threatening conditions is the initial line of management:-
. Control of infections Control of infections Control of infections Control of infections by proper antibiotics according to culture & sensitivity
. Correction of shock, dehydration & electrolyte imbalance Correction of shock, dehydration & electrolyte imbalance Correction of shock, dehydration & electrolyte imbalance Correction of shock, dehydration & electrolyte imbalance by proper I.V. fluids
. Correction of anemia Correction of anemia Correction of anemia Correction of anemia by blood or packed red cells 10-15cc/kg
. Prevention of hypothermia Prevention of hypothermia Prevention of hypothermia Prevention of hypothermia (adequate clothing & external heat)
2 22 2- -- -Home or hospital: nutritional Home or hospital: nutritional Home or hospital: nutritional Home or hospital: nutritional management: management: management: management:
Marasmus Marasmus Marasmus Marasmus Kwashiorkor Kwashiorkor Kwashiorkor Kwashiorkor
Type Type Type Type . Milk Milk Milk Milk: in young non-weaned
infants
. Other food Other food Other food Other food (balanced diet): in
older weaned infants
. Milk Milk Milk Milk: start with soy based lactose free
formula (lactose intolerance), then gradually
shift to standard formulas
. Other food Other food Other food Other food:
=Animal protein (high biological value):
eggs, chicken, meat & yogurt
=Plant protein: lentils, beans
=Fresh vegetables & fruits are added
Amount Amount Amount Amount . 150-200 Kcal. / kg / day . High protein diet: 4-6 gram protein/kg/day
Drugs in Pediatrics NMT11
www.MedadTeam.org 11
N.B: N.B: N.B: N.B:
calculation according to actual
body weight & gradually increase
(5-10 Kcal/kg/day) every day or
every other day according to the
infant tolerance
Route Route Route Route Orally Orally Orally Orally . Nasogastric tube Nasogastric tube Nasogastric tube Nasogastric tube may be required if there
is marked anorexia
. Parentral feeding Parentral feeding Parentral feeding Parentral feeding may be required in
severe cases
N.B N.B N.B N.B: Kwashiorkor Kwashiorkor Kwashiorkor Kwashiorkor (more difficult to manage because of anorexia)
CMarasmus & kwashiorkor Marasmus & kwashiorkor Marasmus & kwashiorkor Marasmus & kwashiorkor
- Treatment of vitamin & mineral deficiency
Vit Vit Vit Vit. A . A . A . A Single dose Single dose Single dose Single dose
=50 000 IU (age up to 6 months)
=100 000 IU (from 6 months to one year)
=200 000 IU (more than one year)
Folic acid Folic acid Folic acid Folic acid iron iron iron iron (4-6 mg/kg/day) in 3 doses
Others Others Others Others vitamin D, C & B complex minerals as (potassium & zinc)
- Treatment of parasitic infestations if present
Rickets Rickets Rickets Rickets
Preventive treatment Preventive treatment Preventive treatment Preventive treatment:
- Vitamin D orally Vitamin D orally Vitamin D orally Vitamin D orally daily from
the second month of life
=Full term Full term Full term Full term: 400-800 IU
=Preterm Preterm Preterm Preterm: 1000-1500 IU from the age of one month
- Exposure to sun Exposure to sun Exposure to sun Exposure to sun
- Diet rich in vitamin D Diet rich in vitamin D Diet rich in vitamin D Diet rich in vitamin D e.g. egg yolk, liver, oily fish
Specific treatment Specific treatment Specific treatment Specific treatment: :: :
1 11 1- -- -Vitamin D therapy Vitamin D therapy Vitamin D therapy Vitamin D therapy Vitamin D deficiency rickets is sensitive to vitamin D in ordinary doses
Oral treatment Oral treatment Oral treatment Oral treatment I.M injection I.M injection I.M injection I.M injection
Daily for 2-4 weeks Single injection without further therapy
=Vitamin D3 :2000-5000 IU/day
OR OR OR OR
=1.25 dihydroxycholecalciferol 0.5-2 Mg/day
600.000 IU
N.B N.B N.B N.B: If no no no no healing healing healing healing occurs the rickets is probably resistant to vitamin D resistant to vitamin D resistant to vitamin D resistant to vitamin D
Drugs in Pediatrics NMT11
www.MedadTeam.org 12
N.B: N.B: N.B: N.B: Injection treatment may be better than oral treatment because of Injection treatment may be better than oral treatment because of Injection treatment may be better than oral treatment because of Injection treatment may be better than oral treatment because of:
- More rapid healing
- Less dependence on parents for daily administration
- Earlier differential diagnosis from vitamin D resistant rickets
2 22 2- -- -Instructions to the parents Instructions to the parents Instructions to the parents Instructions to the parents:
- Diet rich in vitamin D Diet rich in vitamin D Diet rich in vitamin D Diet rich in vitamin D
- Proper sun exposure Proper sun exposure Proper sun exposure Proper sun exposure
Treatment of complications Treatment of complications Treatment of complications Treatment of complications:
- Tetany Tetany Tetany Tetany: :: : 1ml/kg calcium gluconate 10% I.V slowly to be accompanied by oral calcium
- Treatment of iron deficiency anemia Treatment of iron deficiency anemia Treatment of iron deficiency anemia Treatment of iron deficiency anemia by oral iron therapy 6 mg/kg/day
- Deformities Deformities Deformities Deformities: surgical treatment if sever and persistent
Infections
Rashes Rashes Rashes Rashes
Measles Measles Measles Measles Scarlet fever Scarlet fever Scarlet fever Scarlet fever Chicken box Chicken box Chicken box Chicken box
Prevention Prevention Prevention Prevention Active : measles measles measles measles
vaccine vaccine vaccine vaccine (MMR)
Passive: immune immune immune immune
serum globulin serum globulin serum globulin serum globulin
(0.25ml/kg IM)
within 5 days after
exposure. The dose
increased if delayed
beyond the 5
th
day.
Prevention of droplet droplet droplet droplet
infection infection infection infection.
Live attenuated Live attenuated Live attenuated Live attenuated
varicella vaccine varicella vaccine varicella vaccine varicella vaccine is
being used
Supportive Supportive Supportive Supportive
treatment treatment treatment treatment
Diet : increase fluid fluid fluid fluid
intake
Drugs Drugs Drugs Drugs :
- Cough : sedatives
- Fever : anti-pyretic
- Eye : eye drops
Diet : increase fluid fluid fluid fluid
intake
Drugs Drugs Drugs Drugs : symptomatic
treatment
- Fever : anti-pyretic
- Headache & pain :
analgesics
Itching Itching Itching Itching : local &
systemic anti-pruritic
agents
Fever Fever Fever Fever : antipyretics-not
aspirin-as it increases
the risk of Reye
syndrome in which
there is acute
encephalopathy and
fatty degeneration of
the viscera
Specific Specific Specific Specific
treatment treatment treatment treatment
No specific No specific No specific No specific
treatment treatment treatment treatment
Large doses of
Penicillin : Penicillin : Penicillin : Penicillin : is the
drug of choice : oral
penicillin V 400.000
Antiviral drugs
(Acyclovir) (Acyclovir) (Acyclovir) (Acyclovir) in
immunocompromised
Drugs in Pediatrics NMT11
www.MedadTeam.org 13
gamma globulin gamma globulin gamma globulin gamma globulin in
encephalitis
Oral vitamin A vitamin A vitamin A vitamin A
( 400,000 IU) in
severe cases
I.V vitamin A vitamin A vitamin A vitamin A for
measles affecting
kwashiorkor
IU/dose 3 times/day
for at least 10 days
Erythromycin : Erythromycin : Erythromycin : Erythromycin :
(40 mg/kg/day)
in penicillin sensitive
patients
patients
Treatment of Treatment of Treatment of Treatment of
complications complications complications complications
Otitis media &
bronchopneumonia
are treated by proper
antibiotics
Re-examination after 2-
3 weeks for detection
and management of
remote complications
e.g. Rheumatic fever &
glomerulonephritis.
Skin infections: by proper
antibiotics
CRest of rashes: Rest of rashes: Rest of rashes: Rest of rashes:
1) Rubella Rubella Rubella Rubella : ttt is the same items as in measles
2) Roseola infantum Roseola infantum Roseola infantum Roseola infantum :
Antipyretics
Sedatives to infants susceptible to febrile convulsions
3) Infectious mononucleosis Infectious mononucleosis Infectious mononucleosis Infectious mononucleosis : No specific treatment
Rest of infections Rest of infections Rest of infections Rest of infections
Mumps Mumps Mumps Mumps Tetanus Tetanus Tetanus Tetanus Diphtheria Diphtheria Diphtheria Diphtheria
Prevention Prevention Prevention Prevention Active : Mumps Mumps Mumps Mumps
vaccine or MMR vaccine or MMR vaccine or MMR vaccine or MMR
Passive : hyper hyper hyper hyper
immune mumps immune mumps immune mumps immune mumps
gamma gamma gamma gamma globulins globulins globulins globulins (of
value if given early in
the incubation
period)
DPT DPT DPT DPT
Tetanus toxoid Tetanus toxoid Tetanus toxoid Tetanus toxoid during
pregnancy for
prevention of tetanus
neonatorum
Following injury : if not
immunized, human human human human
antitetanus antitetanus antitetanus antitetanus
immunoglobulin immunoglobulin immunoglobulin immunoglobulin 250-
500 units I.M or tetanus tetanus tetanus tetanus
antitoxin antitoxin antitoxin antitoxin 3000 units
DPT vaccine DPT vaccine DPT vaccine DPT vaccine
Supportive Supportive Supportive Supportive
treatment treatment treatment treatment
M MM Measures to relieve easures to relieve easures to relieve easures to relieve
pain pain pain pain:
1. Analgesics
2. Parotitis : heat to
the glands
3. Orchitis : ice bags
Isolation Isolation Isolation Isolation and nursing in
a dark quiet room
Control of convulsions Control of convulsions Control of convulsions Control of convulsions
(patent airways,
oxygen, diazepam)
Maintenance of fluids Maintenance of fluids Maintenance of fluids Maintenance of fluids
Rest Rest Rest Rest : complete bed
rest if myocarditis is
diagnosed
Proper hydration and Proper hydration and Proper hydration and Proper hydration and
high caloric intake high caloric intake high caloric intake high caloric intake
Tube feeding Tube feeding Tube feeding Tube feeding for
Drugs in Pediatrics NMT11
www.MedadTeam.org 14
support the
testis
M MM Mouth outh outh outh: antiseptic
solutions to keep it
clean
and electrolyte balance and electrolyte balance and electrolyte balance and electrolyte balance palatal or pharyngeal
paralysis pt to avoid
aspiration
Specific Specific Specific Specific
treatment treatment treatment treatment
No specific treatment
Human tetanus Human tetanus Human tetanus Human tetanus
immunoglobulin immunoglobulin immunoglobulin immunoglobulin 5000 5000 5000 5000- -- -
10000 10000 10000 10000 I.M (single dose,
neither allergy nor
anaphylaxis and more
persistent titers)
Tetanus antitoxin Tetanus antitoxin Tetanus antitoxin Tetanus antitoxin
5000 5000 5000 50000-10000 10000 10000 100000U
(1/2I.M and I.V) after
sensitivity test
Antibiotics to eradicate Antibiotics to eradicate Antibiotics to eradicate Antibiotics to eradicate
the organism the organism the organism the organism: :: : penicillin
G 10000 10000 10000 10000U/Kg/day I.V
for 10days
Wound: cleaned, left Wound: cleaned, left Wound: cleaned, left Wound: cleaned, left
opened and deprided opened and deprided opened and deprided opened and deprided
1. Antitoxin Antitoxin Antitoxin Antitoxin to
neutralize the
exotoxin 40000-
100000 units I.M or
I.M and I.V
after sensitivity test
2. Antibiotic Antibiotic Antibiotic Antibiotic to
eradicate the
organism
Procaine penicillin Procaine penicillin Procaine penicillin Procaine penicillin
600000 I.U for 7-
10 days
Erythromycin Erythromycin Erythromycin Erythromycin 40
mg/kg/day for 7-
10 days
(forsensitive pt)
Treatment of Treatment of Treatment of Treatment of
complications complications complications complications
Encephalitis : control
of convulsions and
measures to lower the
increased tension
Respiratory support for
cases with asphyxia
CTTT of Pertussis TTT of Pertussis TTT of Pertussis TTT of Pertussis :
Erythromycin Erythromycin Erythromycin Erythromycin: 50 50 50 50mg/kg/day mg/kg/day mg/kg/day mg/kg/day for 14 days may abort or eliminate the disease if given early.
GIT
Vomiting & Persistent diarrhea Vomiting & Persistent diarrhea Vomiting & Persistent diarrhea Vomiting & Persistent diarrhea
Vomiting Vomiting Vomiting Vomiting Persistent diarrhea Persistent diarrhea Persistent diarrhea Persistent diarrhea
- Treatment of the cause
- Antiemetic :
- Metoclopramide : 0.5mg / kg /day
in in in in 3 33 3 divided doses divided doses divided doses divided doses
- Dompridone : 1mg / kg /day in in in in 3 33 3
divided doses divided doses divided doses divided doses
Removal of the offending agent from diet Removal of the offending agent from diet Removal of the offending agent from diet Removal of the offending agent from diet e.g.
- lactose : give instead lactose free formula
(Isomil)
- Cows milk: give instead soy bean based
formula.
Fat Fat Fat Fat given as medium chain triglycerides to
facilitate absorption.
Vitamins Vitamins Vitamins Vitamins especially vitamin vitamin vitamin vitamin A AA A and trace elements
Drugs in Pediatrics NMT11
www.MedadTeam.org 15
Gastroenteritis Gastroenteritis Gastroenteritis Gastroenteritis
1 11 1- -- - Home management : mild to moderate cases Home management : mild to moderate cases Home management : mild to moderate cases Home management : mild to moderate cases
Rehydration solutions Rehydration solutions Rehydration solutions Rehydration solutions: most imp. Item in management.
o Principle: Glucose- facilitated Na absorption mechanism.
o Composition:
NaCl: NaCl: NaCl: NaCl: 3.5 3.5 3.5 3.5 gm gm gm gm To be To be To be To be
dissolved dissolved dissolved dissolved
in one in one in one in one
liter liter liter liter
Na: Na: Na: Na: 90 90 90 90mEq/L mEq/L mEq/L mEq/L
NaHCO NaHCO NaHCO NaHCO3 33 3: : : : 2.5 2.5 2.5 2.5gm gm gm gm Cl : Cl : Cl : Cl : 80 80 80 80mEq/L mEq/L mEq/L mEq/L
KCl : KCl : KCl : KCl : 1.5 1.5 1.5 1.5 gm gm gm gm K: K: K: K: 20 20 20 20mEq/L mEq/L mEq/L mEq/L
Glucose : Glucose : Glucose : Glucose : 20 20 20 20 gm gm gm gm Glucose: Glucose: Glucose: Glucose:111 111 111 111mmol/L mmol/L mmol/L mmol/L
o Indications
- All cases with mild and moderate dehydration
o Dose
- 50-100 ml/kg according to the degree of dehydration to be given over 4-6 hours.
- Thirst mechanism is effective in regulating the amount giving to the child.
o Method
- Usually given by spoon or cup. spoon or cup. spoon or cup. spoon or cup.
- Nasogastric tube Nasogastric tube Nasogastric tube Nasogastric tube may be used in case of:
a- Refusal of ORS
b- Newborn in an incubator
c- Uncooperative mother
o Advantages:
- Suitable for all age groups all age groups all age groups all age groups
- All types of All types of All types of All types of diarrhea diarrhea diarrhea diarrhea
- All types of All types of All types of All types of dehydration dehydration dehydration dehydration provided that Na level is between 115-165 mEq/L
Feeding Feeding Feeding Feeding:
Should not be delayed Should not be delayed Should not be delayed Should not be delayed Delay repair of intestinal cells Persistant diarrhea
Shortly after starting rehydration therapy
o In breast fed infants: breast breast breast breast milk milk milk milk is given in small amounts and gradually increased
according to child's tolerance.
o In formula fed infants: start with diluted formula diluted formula diluted formula diluted formula (1/4 strength) and increase the
conc. gradually.
o In older children: gradual introduction of solid food solid food solid food solid food beginning with vegetables
fruits and jellies.
Treatment of infection Treatment of infection Treatment of infection Treatment of infection:
Self Self Self Self- -- -limited limited limited limited
Antibiotics may kill normal flora Antibiotics may kill normal flora Antibiotics may kill normal flora Antibiotics may kill normal flora persistant diarrhea
o Antibiotics are indicated in:
a- Cholera
b- Giardia, entameba,: Metronidazole 25 25 25 25mg/kg/day mg/kg/day mg/kg/day mg/kg/day( Giardia) and 50 50 50 50mg/kg/day mg/kg/day mg/kg/day mg/kg/day
(Entameba)
c- Shigella
Symptomatic treatment Symptomatic treatment Symptomatic treatment Symptomatic treatment
Drugs in Pediatrics NMT11
www.MedadTeam.org 16
2 22 2- -- - Hospital management for severe complicated cases Hospital management for severe complicated cases Hospital management for severe complicated cases Hospital management for severe complicated cases
Indications Indications Indications Indications
o Deterioration Deterioration Deterioration Deterioration of the patient during home management
o Severe dehydration dehydration dehydration dehydration or shock
o Severe vomiting vomiting vomiting vomiting
o The presence of serious complications complications complications complications: septicemia, metabolic acidosis or bleeding.
A AA A- -- - Intravenous rehydration Intravenous rehydration Intravenous rehydration Intravenous rehydration
Shock therapy Shock therapy Shock therapy Shock therapy Deficit therapy Deficit therapy Deficit therapy Deficit therapy Maintenance therapy Maintenance therapy Maintenance therapy Maintenance therapy
( over 1 11 1 hour) (over 8 88 8 hrs) ( over 24 24 24 24 hrs)
Lactated ringer Lactated ringer Lactated ringer Lactated ringer
sol. sol. sol. sol. ( (( (20 20 20 20 ml/ ml/ ml/ ml/kg) kg) kg) kg)
Glucose Glucose Glucose Glucose 5% 5% 5% 5% and saline in ratio and saline in ratio and saline in ratio and saline in ratio 1:1 1:1 1:1 1:1
a aa a- -- - 40 40 40 40ml/kg in mild mild mild mild dehydration
b bb b- -- - 80 80 80 80ml/kg in moderate moderate moderate moderate cases
c cc c- -- - 120 120 120 120ml/kg in severe severe severe severe dehydration
Glucose Glucose Glucose Glucose 5% 5% 5% 5% and saline in a ratio and saline in a ratio and saline in a ratio and saline in a ratio 4:1 4:1 4:1 4:1
a aa a- -- - 100 100 100 100ml/kg for the first first first first 10 10 10 10 kg kg kg kg
b bb b- -- - 50 50 50 50ml/kg for each kg from from from from 11 11 11 11- -- -20 20 20 20 kg kg kg kg
c cc c- -- - 20 20 20 20ml/kg for each kg above above above above 20 20 20 20 kg kg kg kg
E Deficit therapy Deficit therapy Deficit therapy Deficit therapy in hypernatremic dehydration is made with only 70% of the
calculated amount and should be given slowly to prevent brain edema.
E Potassium Potassium Potassium Potassium therapy therapy therapy therapy: potassium chloride solution (15%) is added to deficit and
maintenance therapy: 1 11 1ml ml ml ml for each for each for each for each 100 100 100 100 ml ml ml ml solution to correct hypokalemia.
B BB B- -- - Treatment Treatment Treatment Treatment of complications of complications of complications of complications
Painful oral lesion Painful oral lesion Painful oral lesion Painful oral lesion
Monilial stomatitis Monilial stomatitis Monilial stomatitis Monilial stomatitis Herpetic gingivostomatitis Herpetic gingivostomatitis Herpetic gingivostomatitis Herpetic gingivostomatitis H HH Herpangina erpangina erpangina erpangina
Antifungal oral nystatin
(mucostatin) or oral
miconazol (daktarin oral gel)
for 10 days
Symptomatic Symptomatic Symptomatic Symptomatic oral analgesics
&antipyretics.
. Antiviral agents are not
indicated
Symptomatic Symptomatic Symptomatic Symptomatic
Hematology
Thalathemia major Thalathemia major Thalathemia major Thalathemia major
1 11 1- -- -Correction of anemia Correction of anemia Correction of anemia Correction of anemia 2 22 2- -- -Removal & prevention of iron ov Removal & prevention of iron ov Removal & prevention of iron ov Removal & prevention of iron overload by erload by erload by erload by
iron chelating agents iron chelating agents iron chelating agents iron chelating agents
Packed RBCs transfusion Packed RBCs transfusion Packed RBCs transfusion Packed RBCs transfusion
-10-15 ml/ kg/ every 4-5 weeks to maintain
Hb level above 10 gm% (hypertransfusion)
Folic acid Folic acid Folic acid Folic acid
To prevent megaloplastic changes in the
bone marrow
Dyferoxamine Dyferoxamine Dyferoxamine Dyferoxamine: :: : SC by a pump over 10
hours 5-6 nights/ week
Deferiprone Deferiprone Deferiprone Deferiprone: :: : oral chelating drug used
when complications of dyferoxamine occur
Drugs in Pediatrics NMT11
www.MedadTeam.org 17
3 33 3- -- - Splenectomy Splenectomy Splenectomy Splenectomy
Indications Indications Indications Indications -Hypersplenism
-Huge spleen causing pressure symptoms
Timing Timing Timing Timing Should not be done before 4 years to avoid sepsis
Care after Care after Care after Care after
splenectomy splenectomy splenectomy splenectomy
-Vaccination against pneumococci, meningiococci & haemophilus
influenza b
-Long acting penicillin
4 44 4- -- - Recent treatment Recent treatment Recent treatment Recent treatment : :: :
Bone marrow transplantation using marrow cells or peripheral stem cells
Induction of fetal Hb production by drugs e.g. L-carnitine
Gene therapy is under trial
Iron deficiency anemia Iron deficiency anemia Iron deficiency anemia Iron deficiency anemia
Prevention Prevention Prevention Prevention: :: :
- Adequate supply of iron to iron to iron to iron to mother mother mother mother during pregnancy
- Proper weaning: iron containing food iron containing food iron containing food iron containing food (green vegetables or meat products) should be given
to infant from age 6
th
month
- Ear Ear Ear Early ly ly ly diagnosis and treatment of the cause diagnosis and treatment of the cause diagnosis and treatment of the cause diagnosis and treatment of the cause e.g. Parasitic infestation-bleeding
Specific treatment Specific treatment Specific treatment Specific treatment: :: : C Iron therapy Iron therapy Iron therapy Iron therapy C
Oral Oral Oral Oral Intramuscular Intramuscular Intramuscular Intramuscular
Indications Indications Indications Indications the usual route failure of oral route
Preparations Preparations Preparations Preparations ferrous sulfate-ferrous gluconate iron dextran
Dose Dose Dose Dose 6 66 6mg/kg/day mg/kg/day mg/kg/day mg/kg/day 3 doses between meals 1 11 1ml( ml( ml( ml(50 50 50 50mg) mg) mg) mg) in infant-2ml(100mg) in
young children
Course Course Course Course 4 44 4- -- -6 66 6 weaks weaks weaks weaks after normalization of all
blood values to replete stores
3 33 3 to to to to5 55 5 days days days days
Supportive treatment Supportive treatment Supportive treatment Supportive treatment: :: :
Blood transfusion (packed red cells: 10 10 10 10 ml/kg slowly ml/kg slowly ml/kg slowly ml/kg slowly) in impending heart failure or when there
is serious infection
Immune thrombocytopenic purpura (ITP) Immune thrombocytopenic purpura (ITP) Immune thrombocytopenic purpura (ITP) Immune thrombocytopenic purpura (ITP)
Moderate and severe Moderate and severe Moderate and severe Moderate and severe Number below below below below 20 20 20 20, ,, ,000 000 000 000 or mucous membrane bleeding
1 11 1- -- - Steroids Steroids Steroids Steroids 2 22 2- -- - IV Ig or anti D: IV Ig or anti D: IV Ig or anti D: IV Ig or anti D:
Action Action Action Action inhibit Ab synthesis & reduce capillary
fragility
bind antibodies before attacking
platelets
Dose Dose Dose Dose 1-2 mg / kg /day 400 /kg over 4-8 hours
Drugs in Pediatrics NMT11
www.MedadTeam.org 18
Duration Duration Duration Duration until platelet count is normal or for 3
weeks which ever comes first
5 consecutive days , booster doses very
2-4 weeks may be needed
Excellent Excellent Excellent Excellent
response response response response
Rapid control of serious bleeding
especially postoperative in steroid
resistant cases. platelet count increase in
7-14 days after therapy
3 33 3- -- - Transfusion therapy Transfusion therapy Transfusion therapy Transfusion therapy
4 44 4- -- - Splenectomy Splenectomy Splenectomy Splenectomy in chronic cases who are steroid resistant
5 55 5- -- - Immunosuppressive Immunosuppressive Immunosuppressive Immunosuppressive e.g. azathioprine or cyclosporine in resistant cases who failed to respond
to splenectomy or relapse postoperatively
6 66 6- -- - Plasmapharesis Plasmapharesis Plasmapharesis Plasmapharesis transient effect if all measures failed
You might also like
- Preventive Pediatrics 2016Document48 pagesPreventive Pediatrics 2016riz04_fortitudessa5178100% (9)
- Pediatric Drugs MKDDocument3 pagesPediatric Drugs MKDquixoticdreamer100% (7)
- Pedia TicklerDocument8 pagesPedia TicklerMargi Gale Nanale50% (6)
- Common Pediatric Cases in OpdDocument90 pagesCommon Pediatric Cases in OpdJamie Sebastian100% (3)
- Pediatrics II Neonatal Resuscitation AlgorithmDocument6 pagesPediatrics II Neonatal Resuscitation AlgorithmYndhira Xheyenn Laylo100% (1)
- Pedia Notes: Anthropometric FluidsDocument9 pagesPedia Notes: Anthropometric FluidsIxc Nxc50% (2)
- Pediatrics: Compilation of Tables From Topnotch Pedia HandoutDocument6 pagesPediatrics: Compilation of Tables From Topnotch Pedia HandoutCielo Lomibao0% (1)
- Pedia Small Notebook EditedDocument17 pagesPedia Small Notebook EditedStarlet Rhonadez Bito-onon Oriel100% (12)
- Pedia TicklerDocument71 pagesPedia TicklermikayNo ratings yet
- PEDIATRIC EOR EXAM: EENT, DERM, HEENTDocument28 pagesPEDIATRIC EOR EXAM: EENT, DERM, HEENTKylie Elaine100% (3)
- Drugs and DosagesDocument4 pagesDrugs and DosagesDin-Din Que33% (3)
- FLUIDS and ELECTROLYTES: NEWBORN GUIDELINESDocument6 pagesFLUIDS and ELECTROLYTES: NEWBORN GUIDELINESDre Valdez100% (5)
- The Seven Habits of Highly Effective PeopleDocument60 pagesThe Seven Habits of Highly Effective PeopleBBCherriNo ratings yet
- Beta-Lactams Cephalosporins: Phenoxymethyl PenicillinDocument3 pagesBeta-Lactams Cephalosporins: Phenoxymethyl PenicillinBobet ReñaNo ratings yet
- Pedia Handy NotesDocument18 pagesPedia Handy NotesCarl Donaire100% (2)
- Pediatrics MnemonicsDocument5 pagesPediatrics Mnemonicsarturschander3614100% (3)
- PPS Core PediatricsDocument53 pagesPPS Core PediatricsDenise Castro100% (3)
- Pediatric Respiratory Distress: Causes and ManagementDocument323 pagesPediatric Respiratory Distress: Causes and Managementmefav7778520100% (1)
- Summer Internship Project-NishantDocument80 pagesSummer Internship Project-Nishantnishant singhNo ratings yet
- Notes On The Life and Works of Jose Rizal - IncompleteDocument15 pagesNotes On The Life and Works of Jose Rizal - Incompleteblock_me_please50% (2)
- Pediatrics Pediatrics Pediatrics Pediatrics Pediatrics: Pediatrics Pediatrics Pediatrics Pediatrics PediatricsDocument2 pagesPediatrics Pediatrics Pediatrics Pediatrics Pediatrics: Pediatrics Pediatrics Pediatrics Pediatrics PediatricsBobet Reña100% (2)
- PediaidiotnotesDocument13 pagesPediaidiotnotesLeiza Tabora96% (23)
- Pedia Notes Compiled PDFDocument133 pagesPedia Notes Compiled PDFAljeirou AlcachupasNo ratings yet
- Pocket PediaDocument15 pagesPocket PediaChai Gabayeron100% (1)
- Pediatric Drug Dosing and Fluid Therapy CalculationsDocument7 pagesPediatric Drug Dosing and Fluid Therapy Calculationseyakoy100% (4)
- Pedia TicklerDocument9 pagesPedia TicklerDianeAbonita100% (2)
- Expanded Program on ImmunizationDocument9 pagesExpanded Program on ImmunizationArianne AshleyNo ratings yet
- Tickler Final PDFDocument29 pagesTickler Final PDFSerious LeoNo ratings yet
- Ob Supplement Handout by DR - Chris SorianoDocument33 pagesOb Supplement Handout by DR - Chris SorianoHedley Chua75% (4)
- Blood Gas Analysis and Interpretation Guide for Neonates, Children and AdultsDocument7 pagesBlood Gas Analysis and Interpretation Guide for Neonates, Children and AdultsClav RamosNo ratings yet
- 10 Warning Signs of ImmunodeficiencyDocument24 pages10 Warning Signs of Immunodeficiencyacque100% (2)
- Opd Meds JgejDocument4 pagesOpd Meds JgejDinen Dot100% (5)
- History and PEDocument3 pagesHistory and PEBom TnaNo ratings yet
- Philippine Pediatric Society, IncDocument19 pagesPhilippine Pediatric Society, IncAsmphLibrary OrtigasNo ratings yet
- Board Review: PediatricsDocument215 pagesBoard Review: Pediatricsokurimkuri94% (16)
- With Notes From The Lecture. If Anything, Just Refer To The Book.Document8 pagesWith Notes From The Lecture. If Anything, Just Refer To The Book.Mao Gallardo100% (2)
- Pediatrics MnemonicsDocument11 pagesPediatrics MnemonicsIndrajit Rana95% (21)
- PEDIATRIC NotesDocument79 pagesPEDIATRIC NotesM A83% (6)
- Pediatric Clinical H&PDocument7 pagesPediatric Clinical H&PJay Vee100% (1)
- Moonlighting 101Document20 pagesMoonlighting 101Dayanara Gener100% (1)
- TICKLER-PRINT Pedia PDFDocument8 pagesTICKLER-PRINT Pedia PDFCarlos H. AcuñaNo ratings yet
- Pediatrics Notes PDFDocument80 pagesPediatrics Notes PDFTG Meadow100% (1)
- Notes For Pedia HandoutDocument2 pagesNotes For Pedia HandoutAiszel Angeli Pepito Ligo100% (2)
- CPG On Hypertension in PregnancyDocument91 pagesCPG On Hypertension in PregnancyRumelle Reyes100% (3)
- NICU Survival GuideDocument14 pagesNICU Survival Guidesedaka26No ratings yet
- Moonlight Medicine Targets Infectious DiseasesDocument282 pagesMoonlight Medicine Targets Infectious DiseasesMeg Mateo100% (1)
- SGOP2019 Cervical Cancer GuidelinesDocument8 pagesSGOP2019 Cervical Cancer GuidelinesNico Angelo CopoNo ratings yet
- Pedia Idiot NotesDocument18 pagesPedia Idiot Noteswiljamesclim100% (8)
- Medad TeamDocument18 pagesMedad TeamAxmed MaxamedNo ratings yet
- Cardiology and endocrine dosesDocument3 pagesCardiology and endocrine dosesSelim TarekNo ratings yet
- Drugs and Renal DiseasesDocument31 pagesDrugs and Renal DiseasesStanley Tatenda MukonoNo ratings yet
- Antimicrobial Dosage Adjustments in Renal Impairment For FormularyDocument20 pagesAntimicrobial Dosage Adjustments in Renal Impairment For Formularyangkatanjuli2019No ratings yet
- Mi FinalDocument29 pagesMi Finalmuthu gowthamNo ratings yet
- Management of MI 2Document24 pagesManagement of MI 2muthu gowthamNo ratings yet
- May 2021 .Document22 pagesMay 2021 .Innocent DimpleNo ratings yet
- Drugs Acting On The Respiratory SystemDocument55 pagesDrugs Acting On The Respiratory SystemDereje DZNo ratings yet
- Classdrugtherapyofshock 160310043509Document55 pagesClassdrugtherapyofshock 160310043509febr1sNo ratings yet
- Drugs in The Neonatal Unit: 1 Julia PettyDocument5 pagesDrugs in The Neonatal Unit: 1 Julia PettyMarjoNo ratings yet
- AnticoagulantsDocument19 pagesAnticoagulantsOsama ZbedaNo ratings yet
- Drug Dosage Adjustment in Renal FailureDocument52 pagesDrug Dosage Adjustment in Renal FailureHernita FerliyaniNo ratings yet
- Streptomycin use and monitoring in MDR-TBDocument3 pagesStreptomycin use and monitoring in MDR-TBfayrouz fathiNo ratings yet
- PHARMACOKINETICS-Not ProtectedDocument35 pagesPHARMACOKINETICS-Not ProtectedAbir HerabNo ratings yet
- Where On Earth Can Go Next?: AppleDocument100 pagesWhere On Earth Can Go Next?: Applepetrushevski_designeNo ratings yet
- Electronic Harassment Strahlenfolter - A Short History of Sound Weapons Pt2 - InfrasoundDocument10 pagesElectronic Harassment Strahlenfolter - A Short History of Sound Weapons Pt2 - InfrasoundFrank-BoenischNo ratings yet
- Compare and Contrast High School and College EssayDocument6 pagesCompare and Contrast High School and College Essayafibkyielxfbab100% (1)
- LLoyd's Register Marine - Global Marine Safety TrendsDocument23 pagesLLoyd's Register Marine - Global Marine Safety Trendssuvabrata_das01100% (1)
- The Emperor Jones: What's Inside in ContextDocument27 pagesThe Emperor Jones: What's Inside in ContextHarshvardhan RaiNo ratings yet
- Analysis of VariancesDocument40 pagesAnalysis of VariancesSameer MalhotraNo ratings yet
- Product Catalog 2016Document84 pagesProduct Catalog 2016Sauro GordiniNo ratings yet
- A Woman's Talent Is To Listen, Says The Vatican - Advanced PDFDocument6 pagesA Woman's Talent Is To Listen, Says The Vatican - Advanced PDFhahahapsuNo ratings yet
- JR Hydraulic Eng. Waterways Bed Protection Incomat BelfastDocument2 pagesJR Hydraulic Eng. Waterways Bed Protection Incomat Belfastpablopadawan1No ratings yet
- PGP TutorialDocument21 pagesPGP TutorialSabri AllaniNo ratings yet
- MVJUSTINIANI - BAFACR16 - INTERIM ASSESSMENT 1 - 3T - AY2022 23 With Answer KeysDocument4 pagesMVJUSTINIANI - BAFACR16 - INTERIM ASSESSMENT 1 - 3T - AY2022 23 With Answer KeysDe Gala ShailynNo ratings yet
- Chemical Cleaning Products Are Destroying The Ecosystem and Your Septic Tank - Organica BiotechDocument14 pagesChemical Cleaning Products Are Destroying The Ecosystem and Your Septic Tank - Organica BiotechKrispin FongNo ratings yet
- Denodo Job RoleDocument2 pagesDenodo Job Role059 Monisha BaskarNo ratings yet
- Wika Type 111.11Document2 pagesWika Type 111.11warehouse cikalongNo ratings yet
- CH - 3Document3 pagesCH - 3Phantom GamingNo ratings yet
- The Invisible Hero Final TNDocument8 pagesThe Invisible Hero Final TNKatherine ShenNo ratings yet
- Chapter 1 - IntroductionDocument42 pagesChapter 1 - IntroductionShola ayipNo ratings yet
- Interna Medicine RheumatologyDocument15 pagesInterna Medicine RheumatologyHidayah13No ratings yet
- R4 User GuideDocument48 pagesR4 User GuideAaron SmithNo ratings yet
- Vintage Style Indonesian Geography Lesson For High School by SlidesgoDocument56 pagesVintage Style Indonesian Geography Lesson For High School by Slidesgoohd InstalasicontrolNo ratings yet
- Ilham Bahasa InggrisDocument12 pagesIlham Bahasa Inggrisilhamwicaksono835No ratings yet
- BMXNRPDocument60 pagesBMXNRPSivaprasad KcNo ratings yet
- Keberhasilan Aklimatisasi Dan Pembesaran Bibit Kompot Anggrek Bulan (Phalaenopsis) Pada Beberapa Kombinasi Media TanamDocument6 pagesKeberhasilan Aklimatisasi Dan Pembesaran Bibit Kompot Anggrek Bulan (Phalaenopsis) Pada Beberapa Kombinasi Media TanamSihonoNo ratings yet
- Electrophoresis and Fractionation of Wheat GlutenDocument14 pagesElectrophoresis and Fractionation of Wheat GlutensecucaNo ratings yet
- Voltaire's Candide and the Role of Free WillDocument3 pagesVoltaire's Candide and the Role of Free WillAngy ShoogzNo ratings yet
- Research Paper Theory of Mind 2Document15 pagesResearch Paper Theory of Mind 2api-529331295No ratings yet
- OROLO & W. D. GannDocument56 pagesOROLO & W. D. GannGaurav Garg100% (1)
- Application Programming InterfaceDocument12 pagesApplication Programming InterfacesorinproiecteNo ratings yet