Professional Documents
Culture Documents
Lower Respiratory Tract Infections
Uploaded by
Sarah PlunkettOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lower Respiratory Tract Infections
Uploaded by
Sarah PlunkettCopyright:
Available Formats
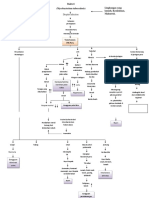
Pneumonia
Transmission Contact droplet 100+ organisms cause
Pathogenesis
Incidence
Symptoms -rattling in chest -shortness of breath -fever -chest pain -wet, thick mucus on coughing -white stuff on X-ray
Other 20% are viral
Mycobacterium tuberculosis Acid fast
Contact, aerosol -Mycolic acid gives exceptionally long stability on surfaces, can be transmitted through air ducts. Airborne precautions
Mycolic Acid: protects from many Abx, drying -Lives in macrophages, slow growing survives phagocytosis and lives in phagosome, dividing only occasionally. Tubercles in lungs = masses of infected macrophages, some of which may die and calcify (obvious in Xray). Tubercles may obstruct airways
1/3 of world! -Was declining, but 2 factors caused the comeback: 1) HIV/AIDS 2) USSR collapseunderfunded Russian prisons were riddled with TB and couldnt afford drugs, so they cut pills in half for prisoners MDR strains
-Bloody cough -trouble breathing -May disseminate to GI, brain, or fetus Asymptomatic: 95% symptoms usually only develop in immunocompromised, but transmission may still occur
TB test: Inject TB Ag just under the skin. If person has antibodies, inflammation will occur within a couple days. Its like an ELISA in the skin! But cant distinguish reliably between past and present infections. Chest X-ray needed for that.
Diseases Community Acquired (CA)- most common: Streptococcus pneumonia (pneumococcus) Atypical pneumonia: walking pneumonia common & less serious Mild, no sputum, caused by obligate intracellular pathogens, hide inside alveolar cells. Chlamydophila pneumonia- survives phagocytosis by alveolar macrophages and replicate in phagosome & Mycoplasma pneumoniae children, lacks a cell wall and is tiny. Lives in bronchial/alveolar epithelia Hospital-Acquired (HA) Pneumonia nosocomial Can be any of the above: pneumococcus, chlamydophila, but often bacteria in wrong place. GI residents and Skin residents Primary TB: initial exposure: bacteria set up tubercles and infection may progress if immunity is weak Secondary TB: reactivation of tubercles due to immune compromise
Vaccine? Yes
Effect of Rx consistent Abx treatment for 6-24 months required to eradicate. Tx very unlikely during treatment. TB vaccine: exists, but low efficacy, and not given because would guarantee positive TB tests. Directly Observed Therapy : (DOT) the gold standard. Required that treatment be administered directly by trained health care workers so as to prevent more MDR.
Transmission Influenza Contact droplet
Pathogenesis Viral receptors: the main recipients of shift, since they are exposed to Abs: 1) Hemagglutinin (HA) 2) Neuramidinase (NA)
Incidence Host range is very broad-many mammals and birds. Key species for human problems= pigs, chickens, humans. Factory farm here and close living quarters in other countries create opportunities for Ag shift.
Symptoms Not vomiting & diarrhea (though that may happen in ~10% of cases) Mainly: -Fever -Achiness -Fatigue -Cough
Other A,B,C Serotypes: A-pandemics B-regional epidemic C-very mild, usually not a problem.
Diseases Pandemics frequent because of high antigenic shift frequency-herd immunity never possible to achieve. 1918- worst by far, but probably wouldnt be as bad today. Transported in it WW1 Avian flu (H5N1)- 50% + mortality in humans, but so far can only spread chickens humans. H1N1 flu (2009)- recent pandemic traced back to pig factory farms, where high population density favors development of virulent disease Hypoxia & retention of CO2 difficulty breathing, death
Vaccine? On Feb 23, 2012 The WHO recommended that the Northern Hemispheres 20122013 seasonal influenza vaccine contain the following 3 vaccine viruses: -an A/California/7/2009 (H1N1)pdm09-like virus -and A/Victoria/361/2011 (H3N2)-like virus -a B/Wisconsin/1/2010like virus
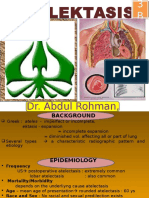
Respiratory Syncytial Virus (RSV)
Contact droplet
Whooping Cough Bortetella pertusis bacterium causes it
Contact droplet
Causes alveolar and bronchial cells to fuse and form syncytia, which results in lower gas exchange abilities, alveolar collapse Pertussis toxin: destroys cilia of respiratory tract. Mucus collects in lungs
SIDS link likely responsible for some cases of SIDS, especially with secondary factors like tobacco smoke exposure Rare, but rising -congestion -sneezing progresses over 1-2 weeks to paroxysmal coughing and apnea (inability to breathe) -exhaustion -death possible Usually only in immunocompromised people. Severe pneumonia with a high fever high mortality rate (15-50% of those with symptoms)
DTaP, Tdap
Legionnaires Disease Legionella pneumophila: lung bacterium
Aerosol Airborne precautions
Obligate intracellular. Very difficult to culture, fastidious . Amoebas in the environment, freeliving, harmless amoebas act as a reservoir. They must be inhaled for infection to occur. You must inhale in spray to become infected. Air conditioning units, showerheads, and produce sprays at groceries have all been implicated
Transmission Hantavirus Pulmonary Syndrome (HPS) Aerosol Specifically, aerosolized urine or feces from infected rodents (reservoir)
Pathogenesis
Incidence Epidemiology tends to arise at newly dispersed suburban edges, especially with those storing food
Symptoms Sudden flu-like symptoms -lungs fill with fluid -high mortality rate
Other
Diseases Sin Nombre Virus- Asia, prior to 1990s, hantaviruses only found in East Asia. Outbreak in Navajo Nation in 1994 led to discovery of new hantavirus, now called Sin Nombre. Cases are sporadic today, mainly in W/SW US.
Vaccine?
Q Fever Coxiella burnetii endospores, so can survive long after remains have decayed Obligate intracellular bacteria hard to culture Inhalation Anthrax Bacillus anthraciscommon in soil, but has high ID50, plus must be inhaled for serious disease. Thus, very rare
Aerosol From aerosolized sheep placenta/fetuses. Causes spontaneous abortion to facilitate its transmission among herd animals Aerosol inhaled endospores. Human to Human transmission not demonstrated, but droplet precautions still recommended Aerosol (at least) Maybe also droplet
Goats, sheep are most common in those with frequent contact with these animals
-chills -cough -fever-like symptoms -abortion can cause fetal death in humans
-mild, until anthrax toxin accumulates sufficiently to kill many alveolar cells cyanosis, death.
Fungal Infections Pneumocystits carinii pneumonia (PCP) very common in AIDS patients
Primarily immunecompromised LRTIs-can see hyphae on X-ray
-mild pneumonitis -dry cough, put progressive inability to breath (dyspnea) and pneumonia. -Hypoxia -Death
Bioterrorism: endospores and nonobvious pathology make it attractive, but would require high degree of training and production facility for significant dispersal. Still, big deal on the NCLEX. HIV-most patients with PCP have HIV. Significant decline now that HAART is available
Prophylactic Abx recommended for possible exposure
Others: -Histoplasmosis -Coccidiomycosis -Aspergillosis
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Health Problems Illnesses Sickness Ailments Injuries Matching Exercise Vocabulary WorksheetDocument2 pagesHealth Problems Illnesses Sickness Ailments Injuries Matching Exercise Vocabulary Worksheetpepac414100% (1)
- Pneumonia Teaching PlanDocument5 pagesPneumonia Teaching PlanFhai Escio71% (7)
- Backup NclexDocument61 pagesBackup NclexSarah PlunkettNo ratings yet
- Rhythm Strips AnalysisDocument107 pagesRhythm Strips AnalysisSarah PlunkettNo ratings yet
- Student Clinical Report SheetDocument2 pagesStudent Clinical Report SheetSarah Plunkett100% (1)
- MRN: - Weight: - KG Age: - : Risk/RestraintDocument2 pagesMRN: - Weight: - KG Age: - : Risk/Restraintrustiejade100% (3)
- Concept Map of Nursing SchoolDocument1 pageConcept Map of Nursing SchoolSarah PlunkettNo ratings yet
- NCLEX Cram SheetDocument2 pagesNCLEX Cram SheetSarah Plunkett100% (1)
- SAMs Pre TestDocument5 pagesSAMs Pre TestSarah PlunkettNo ratings yet
- Drugs Med-SurgTest 3Document6 pagesDrugs Med-SurgTest 3Sarah PlunkettNo ratings yet
- SPA Team Volunteer ApplicationDocument7 pagesSPA Team Volunteer ApplicationSarah PlunkettNo ratings yet
- MedSurg Medication Study Guide Test 1Document12 pagesMedSurg Medication Study Guide Test 1Sarah PlunkettNo ratings yet
- MedSurg Medications & TablesDocument71 pagesMedSurg Medications & TablesSarah PlunkettNo ratings yet
- Transmission Pathogenesis Incidence Symptoms Other Diseases Vaccine? Acute MeningitisDocument4 pagesTransmission Pathogenesis Incidence Symptoms Other Diseases Vaccine? Acute MeningitisSarah PlunkettNo ratings yet
- Micro Final NotesDocument24 pagesMicro Final NotesSarah Plunkett100% (1)
- MedSurg Drug List Test 1Document2 pagesMedSurg Drug List Test 1Sarah PlunkettNo ratings yet
- GI Infections HepatitisDocument4 pagesGI Infections HepatitisSarah PlunkettNo ratings yet
- Upper Respiratory Tract InfectionsDocument1 pageUpper Respiratory Tract InfectionsSarah PlunkettNo ratings yet
- Patho FinalDocument25 pagesPatho FinalSarah PlunkettNo ratings yet
- Soft Tissue InfectionsDocument1 pageSoft Tissue InfectionsSarah PlunkettNo ratings yet
- Surface InfectionsDocument1 pageSurface InfectionsSarah PlunkettNo ratings yet
- Systemic Infections Affecting Skin All ViralDocument2 pagesSystemic Infections Affecting Skin All ViralSarah PlunkettNo ratings yet
- Eye InfectionsDocument1 pageEye InfectionsSarah PlunkettNo ratings yet
- Helicobacter Pylori-A: Transmission Pathogenesis Incidence Symptoms Other Diseases Vaccine? Stomach UlcersDocument4 pagesHelicobacter Pylori-A: Transmission Pathogenesis Incidence Symptoms Other Diseases Vaccine? Stomach UlcersSarah PlunkettNo ratings yet
- Blood InfectionsDocument3 pagesBlood InfectionsSarah PlunkettNo ratings yet
- Reproductive InfectionsDocument2 pagesReproductive InfectionsSarah PlunkettNo ratings yet
- Acute Bronchitis HandoutDocument5 pagesAcute Bronchitis HandoutDianne LegionNo ratings yet
- Pneumothorax: Algorithm: Queen's Dect: KGH BleepDocument2 pagesPneumothorax: Algorithm: Queen's Dect: KGH BleepRachmi Merrina0% (1)
- Droplet Infection: Tuberkulosis (TB) ParuDocument2 pagesDroplet Infection: Tuberkulosis (TB) ParuMiiniieNo ratings yet
- Choking Relief For Adults, Children and Infants Signs of ChokingDocument3 pagesChoking Relief For Adults, Children and Infants Signs of ChokingJeah Bearl AbellarNo ratings yet
- DESIMINATION PPT BaruDocument13 pagesDESIMINATION PPT BaruRian ZulkarnainNo ratings yet
- Fix Entry Des Bu ZumDocument199 pagesFix Entry Des Bu Zumretno kumalasariNo ratings yet
- PatomekanismeDocument18 pagesPatomekanismeEdwin Pasha Jr.No ratings yet
- Who Pneu Im Pgi ProtocolDocument2 pagesWho Pneu Im Pgi ProtocolRoxanneGailBigcasGoleroNo ratings yet
- NURSING CARE PLAN About Ineffective Airway ClearanceDocument6 pagesNURSING CARE PLAN About Ineffective Airway ClearanceJoji BaitNo ratings yet
- Pulmonary InfectionDocument1 pagePulmonary InfectionAzirayah WoshiNo ratings yet
- Bronchitis in ChildrenDocument3 pagesBronchitis in ChildrenVibhaSingh1No ratings yet
- Neonatal Chest X-RayDocument19 pagesNeonatal Chest X-RaydeborapkphnNo ratings yet
- Bronchiectasis: Chapter 284 Harrison's Internal Medicine Jing R. BautistaDocument28 pagesBronchiectasis: Chapter 284 Harrison's Internal Medicine Jing R. BautistaMa. Luisa BuotNo ratings yet
- Weekly Influenza Surveillance Update 2020-2021 From The Rhode Island Department of Health.Document29 pagesWeekly Influenza Surveillance Update 2020-2021 From The Rhode Island Department of Health.Frank MaradiagaNo ratings yet
- 10 Quiz of PneumoniaDocument3 pages10 Quiz of PneumoniaTatyannah Alexa MaristelaNo ratings yet
- High Resolution CT of The Lung Patterns of Disease and Differential DiagnosesDocument30 pagesHigh Resolution CT of The Lung Patterns of Disease and Differential DiagnosesNicolai Babalici100% (1)
- 3 3 1 Medical History Visit 1Document2 pages3 3 1 Medical History Visit 1Amaris HopkinsNo ratings yet
- Jurnal Fisioterapi DadaDocument11 pagesJurnal Fisioterapi DadaRosvita IndriawatiNo ratings yet
- Mendelson Syndrome - StatPearls - NCBI BookshelfDocument8 pagesMendelson Syndrome - StatPearls - NCBI Bookshelfcesar aNo ratings yet
- Diagnosa Banding PneumoniaDocument7 pagesDiagnosa Banding PneumoniaLuphly TaluvtaNo ratings yet
- Corona Virus Pre Departure Screening Questionnaire R2 PDFDocument2 pagesCorona Virus Pre Departure Screening Questionnaire R2 PDFKaryaMaju Comp0% (1)
- Nursing Care PlanDocument4 pagesNursing Care PlanGabrielGitaNo ratings yet
- AtelectasisDocument26 pagesAtelectasisArini NurlelaNo ratings yet
- BronchiectasisDocument61 pagesBronchiectasisRapid MedicineNo ratings yet
- My Oral Proyect: Student: Garcia Ynoñan Jesus EnriqueDocument10 pagesMy Oral Proyect: Student: Garcia Ynoñan Jesus EnriqueJesúsEnriqueGarciaNo ratings yet
- COPD vs. Asthma Symptoms: 6 Differences and 6 SimilaritiesDocument3 pagesCOPD vs. Asthma Symptoms: 6 Differences and 6 Similaritiessd saklineNo ratings yet
- Hongkong Boostrix Diftetkok Boostrix - Polio Engerix - B Hyper-Tet Infanrix-Ipv+Hib MMR Ii VarivaxDocument7 pagesHongkong Boostrix Diftetkok Boostrix - Polio Engerix - B Hyper-Tet Infanrix-Ipv+Hib MMR Ii Varivaxapotik medicareNo ratings yet
- What Are The Similarities Between Flu and CovidDocument1 pageWhat Are The Similarities Between Flu and CovidZakya Oumelbanine KlNo ratings yet