Professional Documents
Culture Documents
The Process of Labor
Uploaded by
Roselyn Baguilet PadilanOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Process of Labor
Uploaded by
Roselyn Baguilet PadilanCopyright:
Available Formats
The Process of Labor It is most important that you trust your body when you go into labor.
Remember, your body was built to carry, nourish, and safely deliver your baby. Some of the factors that affect the course of labor include your health, nutrition, size and shape of your pelvis, size and presentation of the baby, your educational preparation for labor and birth, and the practice of exercises, relaxation and breathing techniques. During labor, the emotional support you receive, along with medical interventions, may also affects the course of labor. How Do I Know When Labor Will Begin? Each labor is unique. No one can predict exactly what your individual labor will be like, or when it may begin. However, prior to the onset of labor, you will notice some signs that are nature's way of telling you that labor is approaching. If you are not sure, call your physician or midwife to discuss your labor signs. In the event you are evaluated at the hospital as being in very early labor and sent home, it is common to feel disappointed, maybe even embarrassed. It is common for first-time mothers to make more than one trip to the hospital. If you are in early labor and sent home, the following may be helpful: walking, showering, resting, drinking fluids, renting a video, listening to music, etc. The most common signs that labor may soon begin include: The baby "drops" or engages into the pelvis, which is called lightening. Lightening may occur two to four weeks prior to labor in first-time mothers and often not until labor begins if you have previously had children. Your abdomen usually appears lower and more protruding. You may experience a greater ease in breathing, relief from heartburn and an ability to eat larger portions. However, the lower position of the baby together with its greater size, can lead to: Increased backache and sacroiliac discomfort Increased awkwardness in walking Increased frequency of urination Frequent bowel movements may be experienced within 48 hours of labor, cleansing the lower bowel in preparation for birth. Diarrhea or flu like symptoms without fever. Indigestion, nausea, or vomiting are common a day or so before labor begins. Increased vaginal discharge during the last few weeks of pregnancy as the body prepares for the passage of the baby through the birth canal. Increased Braxton-Hicks contractions during the last weeks of pregnancy, which are "practice" contractions that prepare the uterus for labor and may cause some effacement and dilation (thinning and opening) of the cervix. These contractions do not ordinarily cause pain but may be sufficiently strong and regular to be confused with true labor. This is referred to as false labor. Possible "bloody show" or the release of slightly brown, pink or blood-tinged mucus from effacement and dilation (the thinning and opening) of the cervix, causing the mucus plug to be released from the cervix. Some women notice a sudden burst of energy, sometimes called a "nesting instinct" approximately 24-48 hours before the start of labor. You may feel a strong desire to clean the house and prepare for the baby. Try not to tire
yourself as nature gives you this extra energy to help you during labor. If you must be active, be careful not to overexert yourself! A loss or leveling off in weight may be noticed in the last few days before labor begins. It is common to lose 1-3 pounds of fluid before labor begins as a result of hormonal shifts. Mother just feels "different," not quite herself.The bag of water may break. Depending on the location of the break in the amniotic sac, the break can feel like a gush, or an uncontrolled trickle of fluid coming from the vagina. Anxiety and disappointment are very common feelings for mothers as the "due date" approaches or passes without labor beginning. Try to keep occupied and active, but do not wear yourself out! Pre Labor vs. True Labor
If you have never experienced labor before, you may find it difficult to know if you are in labor. Before heading to the hospital, call your physician or midwife to discuss your labor symptoms.
It is common for first time mothers to make more than one trip to the hospital. If you are in early labor and sent home, the following activities may be helpful: walking, showering, resting, drinking fluids, listening to music, etc. Pre-labor vs. True Labor Onset of Labor When to go to the hospital Pre-labor vs. True Labor "How Do I know if I'm Really in Labor?" Pre-labor can only be differentiated from true labor by an internal examination of the cervix. True labor contractions become stronger, difficult to talk through, last longer, and are closer together as labor progresses. These will effect changes in the cervix, causing it to thin out and open while encouraging the descent of the baby through the pelvis. True Labor Contractions
May be irregular at first Usually become regular Get longer, stronger, and closer together as time progresses Walking usually makes them stronger Lying down does not make them go away Often begin in your back and move to the front Cervix Changes by becoming thinner and starts to open (dilates)
False (or "Practice") Labor Contractions Usually are irregular and short Do not get longer, stronger, or closer together Can last several minutes in length Walking does not make them stronger, may even cause them to stop Lying down may make them go away May be felt more in the front area and in the groin area Beneficial in preparation for true labor Cervix Very little change or no change; does not thin or open Prodromal Labor Contractions May begin irregular and become regular Usually stay five or greater minutes apart May feel strong, but usually do not get closer together Lying down does not usually make them go away May last 24-36 hours without significant cervical changes Resting and sleeping may be challenging It is common proactice to be sent home to rest or to await stronger labor Cervix May thin out but not dilate more than Onset of Labor Several theories exist as to why labor begins:
The physical aging of the placenta may cause insufficient nutrients to reach the fetus. The uterus reaches a crucial point of distension, which may cause tension on muscle fibers and stimulate their activity. Nerve impulses from the uterus to the posterior pituitary gland may bring about release of oxytocin (a hormone which causes the uterus to contract). Decrease in the level of the hormone pregesterone, may cause uterine changes.
Adrenal glands of the fetus, when mature, may release a substance to stimulate labor. The release of prostaglandin from the wall of the uterus may initiate labor. When to go to the hospital Most physicians and midwives suggest contacting them when your contractions are five minutes apart and lasting 60 seconds and you have had this activity for about an hour. When you reach your doctor or midwife, be prepared to tell him/her: How far apart the contractions are, their length and intensity, and if you are using breathing techniques Whether or not the bag of waters has broken, the time it broke, and the color of the fluid If a bloody show is present. Your physician or midwife will instruct you when to leave for the hospital. If you are a first-time mother and are able to manage the contractions at home, new research is suggesting that first-time mothers should continue to stay at home until it is difficult to breathe through the contractions. However, if you live a great distance from the hospital, are concerned about not getting there on time or have other special concerns, plan on leaving sooner. What to Expect when you arrive at the Hospital When you arrive in labor and delivery, a nurse will check your blood pressure, temperature, may obtain both blood and urine samples, and place devices on your abdomen that monitor the baby's heart rate and your contractions. The nurse, your on-call physician, or midwife will then perform a vaginal exam to evaluate the dilation and effacement of your cervix. It is best to be admitted when active labor begins, especially if you are a first-time mother. In active labor, the contractions are less than five minutes apart, lasting 45-60 seconds and the cervix is dilated three centimeters or more. Depending on your stage of labor, contraction pattern, how far dilated you are and fetal heart tracing, your physician or midwife may admit you to the hospital, or suggest returning home until the contractions are closer together. In the event you are in early labor and sent home, it is common to feel disappointed, maybe even embarrassed. Activities such as walking, showering, resting, drinking fluids, renting a video, or listening to music, can be very helpful in early labor. If you are admitted and have had a positive culture for Group B Beta Strep during your pregnancy, or have any risk factors, you will receive antibiotics prior to delivery. Stages of Labor The four stages of the childbirth process are based on changes in the uterus and cervix as labor progresses. The beginning and end of each stage are described below: First Stage of Labor Begins at the onset of labor and ends when the cervix is 100 percent effaced and completely dilated to 10 centimeters. Average length ranges for a first-time mother is from ten-to-fourteen hours and shorter for subsequent births. The first stage of labor Cerival Effacement and Dilation
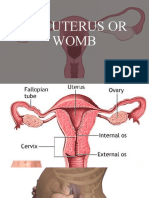
Illustration of Cervical Effacement Second Stage of Labor Begins when the cervix is completely effaced and dilated and ends with the birth of the baby. Average length for a first time mother ranges from 1 to-2 hours and shorter for subsequent births. Read more in our Health Library The second stage of labor Third Stage of Labor Begins with the birth of the baby and ends with the delivery of the placenta. Average length for all vaginal deliveries ranges from five-to-fifteen minutes. Fourth Stage of Labor Begins with delivery of the placenta and ends one-to-two hours after delivery. How Will I know if I am Making Progress? The progress of labor and the baby's position is determined by an internal vaginal exam. These exams are not done frequently and may be done during a contraction. Internal vaginal exams assess: Cervical effacement (thinning measured as 0 to 100 percent) Cervical dilation (opening measured as 0 to 10 centimeters) Baby's presentation (the part of the baby to move to the pelvis first, e.g. head, buttocks, feet) Position of the baby's presenting part (described as anterior, facing your back, or posterior, facing your front) Station (baby's progress down through the pelvis or birth canal. Measured in minus to plus numbers) Labor Contractions Labor contractions are the periodic tightening and relaxing of the uterine muscle, the largest muscle in a woman's body. Something triggers the pituitary gland to release a hormone called oxytocin that stimulates the uterine tightening. It is difficult to predict when true labor contractions will begin. Contractions are often described as a cramping or tightening sensation that starts in the back and moves around to the front in a wave-like manner. Others say the contraction feels like pressure in the back. During a contraction, the abdomen becomes hard to the touch. In the childbirth process, the work of labor is done through a series of contractions. These contractions cause the upper part of the uterus (fundus) to tighten and thicken while the cervix and lower portion of the uterus stretch and relax, helping the baby pass from inside the uterus and into the birth canal for delivery. How Contractions are Timed Contractions are intermittent, with a valuable rest period for you, your baby, and your uterus following each one. When timing contractions, start counting from the beginning of one contraction to the beginning of the next. The easiest way to time contractions is to write down on paper the time each contraction starts and its duration, or count the seconds the actual contraction lasts, as shown in the example below. Writing down the time
and length of the contraction is extremely helpful for describing your contraction pattern to your physician, midwife or hospital labor and delivery personnel. TIME CONTRACTION STARTS 10:00 45 seconds 10:10 45 seconds 10:15 60 seconds 10:20 55 seconds What Contractions Feel Like Many mothers describe contractions that occur in early labor as similar to menstrual cramps, or as severe gas pains, which may be confused with flu symptoms or intestinal disorders. Imagine your contractions as looking like a wave. Each contraction will gradually gain in intensity until the contraction peaks, then slowly subside and go away. As your body does the work of labor, it is likely that the time in between contractions will become shorter. As the strength of each contraction increases, the peaks will come sooner and last longer. There should be some regularity or pattern when timed. Persistent contractions that have no rhythm but are five-to-seven minutes apart or less should be reported to your physician or midwife. Try to visualize contractions as positive Think of each contraction as something positiveit is bringing you that much closer to the birth of your baby. Visualize what the contractions are accomplishing, the thinning and opening of the cervix and the pushing of the baby downward. Try to work with your body rather than against it by staying as relaxed as possible during the contractions. Typical Length or Duration A typical labor for a first time mother is eight-to-fourteen hours, and is usually shorter for a second or subsequent birth. For many women, rocking in a chair or swaying during a contraction assists them with this relaxation. Pushing: The Second Stage of Labor The pushing stage occurs after the cervix is completely dilated and no longer in front of the baby's head. A smooth passageway now exists through which you can push your baby from the uterus and down through the birth canal to delivery. Your contractions may decrease just prior to getting the urge to push. You should take this time to rest prior to pushing. The length of this stage varies with the position and size of the baby and your ability to push with the contractions. For first-time mothers the average length of pushing is one-to-two hours. In some instances, pushing can last longer than two hours if mother and baby are tolerating it. Normally, the baby is born with his face looking toward mother's back (referred to as an anterior position). However, some babies are facing the mother's abdomen (referred to as a posterior position). Posterior babies may have a more difficult time passing through the pelvis, which may cause pushing to be more difficult or require more than two hours of pushing. Contractions during the Pushing Stage DURATION OF CONTRATION
During the second stage of labor, the uterus continues to contract about every five minutes and each contraction lasts 45-to-90 seconds. The contractions are usually strong and forceful and may or may not be accompanied by an urge to push. This can make this phase somewhat more enjoyable since you are now working with each contraction. A renewed sense of energy may occur as you feel the closeness of your baby's birth! However, sometimes after a long or difficult labor, the pushing stage can be exhausting and uncomfortable. Most women will feel increased pressure in their perineum, rectum, and low back at this stage. For many women, the rectal pressure feels the same as having a bowel movement. As the baby's head begins to appear, you may feel a stretching or burning sensation. You may want a mirror positioned so that you can see your progress. Delayed Pushing Pushing is most effective when the mother feels the urge to push. Women who receive epidural anesthesia may have the sensation to bear down numbed by the anesthetic. The practice of "delayed pushing" (waiting for the baby to passively come through the birth canal) has been studied as an alternative to start pushing at 10 centimeters. If you and your baby are doing well, a one-to-two hour period of "passive descent" is safe and may make your pushing more effective. Positions for Pushing There are many different positions that may be used for pushing. In all positions, keep your chin down and use a rounded back to help your abdominal muscles assist your uterus in pushing your baby. The following suggestions of various positions for pushing and advantages of each one. You may be able to speed the progress of the labor if you try positions where gravity assists you (i.e. sitting, or squatting). However, if the baby is delivering quickly, you may be able to slow the stretching of the perineum by trying positions where gravity is neutral (i.e. lying on your side, or getting on your hands and knees). It is important for your comfort to experiment with pushing in different positions. Many women find pulling a towel or sheet held by a partner or tied on the squat bar to be very effective during a pushing contraction. Positions for pushing and their respective advantages Stopping your Pushing There may come a time when you may be asked not to push with a contraction. This is for reasons such as the cervix is not fully dilated or the baby is crowning and the perineum needs to stretch gradually. Usually these situations require you to stop pushing for a short time. During this time, relax your neck, shoulders and legs and pant or blow out during the contraction. Visualize blowing out candles. Your partner may need to hold your face, look directly in your eyes, and pant or blow with you to keep you from pushing. Pushing, for many mothers, is a powerful reflex that requires considerable effort to breathe through rather than to push through. Breathing Techniques for Pushing The breathing techniques used for pushing are varied and depend upon which works best for you. Your health care provider and labor nurse(s) will offer suggestions and are your most valuable resources in evaluating your progress as you push your baby through the birth canal. Work with your contractions to enable yourself to maximize your efforts at the peak of the contraction. Grunting or groaning may be helpful while pushing. Allow yourself the freedom to make the sounds that come naturally. It is unnatural and possibly damaging to you and your baby to hold your breath for a long time. Holding your breath while pushing is fine to do if you feel it assists with bearing down.
Breathing Techniques Breathing often reflects our state of relaxation or excitation. When at rest, breathing is usually slow and rhythmic, (such as when asleep). When tense, breathing may be erratic, or we may hold our breath. Controlling breathing may help you become aware of your state so you can stay relaxed. Breathing techniques are helpful to many women in labor. The theory behind childbirth breathing patterns is based on the concentration required to focus on your breathing. During a contraction, your thought process is redirected from a pain response such as tension and breath holding to a learned relaxed breathing response. The successful development of a relaxed response to painful stimuli is most effective through a lot of practice. Allow your body to relax as completely as possible and work with the contractions while using the breathing and relaxation techniques. There is no right or wrong way to breathe. The breathing techniques are only guidelines and should be adapted to your individual preference and comfort. Guidelines for Breathing Techniques Begin focusing on your breathing when you feel you need help relaxing or can no longer walk or talk through a contraction. For many women, this may be hours into labor. Your breathing should be at a comfortable rate and not cause you to feel short of breath or light-headed. Your breathing style should be your own. The breath may be taken in and out of your nose or mouth, or in your nose and out your mouth. The key is to have the breathing feel natural, relaxed and even. Each of the breathing techniques has two common features: a cleansing breath and a focal point. Cleansing Breath The use of a cleansing breath before and after every contraction is important. It is an exaggerated, deep breath, usually done by breathing in through the nose and out through the mouth. The purposes of this breath are to: Allow for increased oxygen to the baby Internally signal you that a contraction is beginning and to remind you to begin concentrating on breathing, focusing, and relaxing. Externally signal your partner and anyone else assisting with the labor that a contraction is beginning. They can then offer assistance, such as a back massage or verbal encouragement. Allow for blowing off residual tension after a contraction is over. Give your baby a boost of oxygen at the end of the contraction. Focal Point The use of a focal point will help enhance your relaxation and increase your concentration during a contraction. An internal focal point, such as a peaceful scene or serene setting may work well for some; others may find that they need to concentrate on an object in the room or the partner's eyes. This focus may change during labor, as contractions gain strength. Practice using different focal points that enhance your contraction and help eliminate distractions. (Note: a clock is not used as a focal point.
Allow the breathing to continue on its own quietly, easily, and evenly. Concentrate on letting yourself completely relax and let your body go limp with each exhale. Picture a rag doll. Your body may begin to feel warm and heavy. When ready to rouse yourself, breathe in deeply, stretching arms and legs, as you exhale. Slow Paced Breathing Take a "cleansing" breath at the beginning of a contraction Continue to breathe evenly in and out with slow,easy abdominal breathing. Pace is approximately half your normal respiratory rate. You may use Attention Focusing strategies such as: Inhalation/exhalation through nose Inhalation/exhalation through mouth Counting rhythms, imagery, affirming phrases, etc.Movement, stroking, massage, tapping, etc. A visual focal point As contraction ends, take a "cleansing" breath, breathing out slowly, and relaxing completely. Modified Paced Breathing Easy, rhythmical breathing with a frequency of approximately twice your normal respiratory rate. Relaxed movement in chest and abdomen with more use of intercostal (chest) muscle. Use as needed for more challenging contractions Use same steady rate throughout contraction or use attention focusing strategies as needed. Patterned Paced Breathing Even, rhymthmical breathing approximately twice your normal respiratory rate. Breathing pattern does not change rate or volume of air exchange. Pattern 3 breath/1 "blow" Use Attention Focusing strategies as needed. Variations of Patterned Paced Breathing Pattern can be from 1 breath/1 blow to 6 breaths/1 blow. Can use Patterned Paced breathing in 1 breath/1 blow (He/Who) Try pattern of 5/1, 4/1, 3/1, 2/1, 1/1, 2/1, 3/1, 4/1, 5/1 Combine paced breathing techniques in one contraction. Use attention focusing strategies as needed.
You might also like
- Holistic Pregnancy Manual: Maternal Health Manuals, #1From EverandHolistic Pregnancy Manual: Maternal Health Manuals, #1No ratings yet
- Latent Phase of LabourDocument10 pagesLatent Phase of LabourFELIX CLINENo ratings yet
- Pregnancy, Birth and Beyond: A Spiritual and Practical GuideFrom EverandPregnancy, Birth and Beyond: A Spiritual and Practical GuideNo ratings yet
- Pre Labor VsDocument6 pagesPre Labor VsMarffy Llamas100% (1)
- Holistic Postpartum Manual: Maternal Health Manuals, #3From EverandHolistic Postpartum Manual: Maternal Health Manuals, #3No ratings yet
- All About PragnancyDocument29 pagesAll About PragnancyBaalu KathirveluNo ratings yet
- Antenatal Info Booklet Intuitive BirthDocument32 pagesAntenatal Info Booklet Intuitive Birthapi-223713414No ratings yet
- The Earliest Weeks of PregnancyDocument23 pagesThe Earliest Weeks of PregnancyAnaleah MalayaoNo ratings yet
- Labor Delivery TipsDocument32 pagesLabor Delivery TipsAivvee DraculanNo ratings yet
- 9th Month of PregnancyDocument2 pages9th Month of PregnancyVicky OZNo ratings yet
- Birth Course Companion Ebook-3Document97 pagesBirth Course Companion Ebook-3shivanibatraNo ratings yet
- Lending LibraryDocument1 pageLending Libraryapi-247440750No ratings yet
- Welcoming The Maiden Archetype: When Can I Do The Meditation?Document3 pagesWelcoming The Maiden Archetype: When Can I Do The Meditation?Gabrijela TominacNo ratings yet
- The Motherly Guide To Becoming MamaDocument10 pagesThe Motherly Guide To Becoming Mamaamstelbryan39No ratings yet
- Amounts of Foods To OfferDocument1 pageAmounts of Foods To OfferMadalin PlastoiNo ratings yet
- FPQC Positions For LaborDocument3 pagesFPQC Positions For LaborAukia HyuugaNo ratings yet
- Pregnancy Options Book A5 Website 1Document33 pagesPregnancy Options Book A5 Website 1api-252780946No ratings yet
- HandoutmassageDocument1 pageHandoutmassageapi-244719696No ratings yet
- Why Home Birth Is NecessaryDocument3 pagesWhy Home Birth Is NecessaryMutiara Ummu SumayyahNo ratings yet
- L&D Worksheet Student SampleDocument3 pagesL&D Worksheet Student Sampleth233No ratings yet
- Month by MonthDocument28 pagesMonth by MonthChoi Han KimNo ratings yet
- Pregnancy OptionsDocument116 pagesPregnancy OptionsBharti CartesNo ratings yet
- 21 Day Detox RecipesDocument41 pages21 Day Detox Recipesphilippe28790No ratings yet
- Handout 5 PDFDocument4 pagesHandout 5 PDFApRil Anne BalanonNo ratings yet
- Ceremony - Candle Lighting PDFDocument2 pagesCeremony - Candle Lighting PDFrafaelgsccNo ratings yet
- Doulas and Labor SupportDocument2 pagesDoulas and Labor SupportbatlixieNo ratings yet
- Pregnancy Stages GuideDocument15 pagesPregnancy Stages Guidefarhan_ansNo ratings yet
- PHD Student: Thierry Claudien Uhawenimana Supervisors: Prof. Alison Mcfadden, Dr. Nicola Gray, Dr. Heather WhitfordDocument1 pagePHD Student: Thierry Claudien Uhawenimana Supervisors: Prof. Alison Mcfadden, Dr. Nicola Gray, Dr. Heather WhitfordThierry UhawenimanaNo ratings yet
- Natural FertilityDocument148 pagesNatural FertilityAish LakshNo ratings yet
- Labor and Birth HandoutDocument9 pagesLabor and Birth Handoutapi-240665032No ratings yet
- Lamaze 6healthybirthpractices Infographic FinalDocument1 pageLamaze 6healthybirthpractices Infographic Finalapi-264859193No ratings yet
- BCC Session3 LinksextrasDocument13 pagesBCC Session3 Linksextrasapi-222516709No ratings yet
- Chakra Balancing GuideDocument4 pagesChakra Balancing Guidesvp3761No ratings yet
- Easy Steps To A Safer PregnancyDocument53 pagesEasy Steps To A Safer PregnancySummer Time100% (1)
- Leopolds Manuever Final 21aDocument27 pagesLeopolds Manuever Final 21aArun Roa DanielNo ratings yet
- Clinical Week 3 - Teaching Plan - BreastfeedingDocument2 pagesClinical Week 3 - Teaching Plan - Breastfeedingapi-273168705No ratings yet
- The Uterus or WombDocument38 pagesThe Uterus or WombmuwahNo ratings yet
- Labor and Delivery TopicsDocument44 pagesLabor and Delivery TopicsAngela Joy AmparadoNo ratings yet
- Fetal MalpresentationDocument33 pagesFetal MalpresentationMichael Angelo Seña100% (1)
- Lunar Chart GuideDocument9 pagesLunar Chart GuideElena M100% (1)
- Antenatal Care Schedule Handout - GP Low Risk May 2018Document4 pagesAntenatal Care Schedule Handout - GP Low Risk May 2018maddy100% (1)
- Meditation Har Trust in GodDocument3 pagesMeditation Har Trust in GodNicole HawkinsNo ratings yet
- Lotus BirthDocument4 pagesLotus BirthindahNo ratings yet
- Pregnancy Yoga Postures For LabourDocument29 pagesPregnancy Yoga Postures For LabourAjay IyerNo ratings yet
- BCC Session2 LinksextrasDocument6 pagesBCC Session2 Linksextrasapi-222516709No ratings yet
- The Postpartum TraditionDocument24 pagesThe Postpartum TraditionAzher Hameed QamarNo ratings yet
- Module 6 IntrapartumDocument33 pagesModule 6 IntrapartumTiangco Fatima AlfaNo ratings yet
- FAKE FAKE Document - Please Don't Use This: Associated Body PartsDocument18 pagesFAKE FAKE Document - Please Don't Use This: Associated Body Partsgnk1975No ratings yet
- Nursing Mothers GuideDocument11 pagesNursing Mothers GuidepbanerjeeNo ratings yet
- Relaxation Techniques for Labor Pain ReliefDocument23 pagesRelaxation Techniques for Labor Pain ReliefEdderlyn LamarcaNo ratings yet
- The Menstrual Cycle WorksheetDocument2 pagesThe Menstrual Cycle Worksheetapi-383924075% (4)
- Anatomical and Physiological Changes During PregnancyDocument25 pagesAnatomical and Physiological Changes During Pregnancyqaleeq100% (1)
- NWHRC - Pregnancyplanner Your GuideDocument16 pagesNWHRC - Pregnancyplanner Your GuideRiyan WahyudoNo ratings yet
- Birth Partners' Affirmations Script..Document6 pagesBirth Partners' Affirmations Script..nadyaNo ratings yet
- Impact of Doulas Delivery and BFDocument10 pagesImpact of Doulas Delivery and BFFabiola AndreaNo ratings yet
- Ebook Vaginal SteamingDocument14 pagesEbook Vaginal SteamingDana DragomirescuNo ratings yet
- Managing Pain During Childbirth With Massage, Reflexology and Other Manual MethodsDocument11 pagesManaging Pain During Childbirth With Massage, Reflexology and Other Manual MethodsFiraNo ratings yet
- Essential Perinatal Exercises for Strength and FlexibilityDocument12 pagesEssential Perinatal Exercises for Strength and FlexibilityJeane Rose PurazoNo ratings yet
- Pelvic Girdle Pain Fact SheetDocument5 pagesPelvic Girdle Pain Fact SheetagniosaiNo ratings yet
- Formulation and Evaluation of Antiseptic Polyherbal OintmentDocument11 pagesFormulation and Evaluation of Antiseptic Polyherbal OintmentandrapradeshsseNo ratings yet
- MedicalDocument3 pagesMedicalmumtazkauser74No ratings yet
- Case Report in Psychiatry051.03Document4 pagesCase Report in Psychiatry051.03Christian Tan Getana100% (1)
- Med Surge 2 Mod 3 Study GuideDocument19 pagesMed Surge 2 Mod 3 Study GuideDirk Buckner100% (4)
- Mycoplasma Genitalium A4Document1 pageMycoplasma Genitalium A4Nauli NasirNo ratings yet
- Current Status of NTD PhilippinesDocument28 pagesCurrent Status of NTD PhilippinesMelody PardilloNo ratings yet
- Brand Name Generic Name Disease Group Consumer Medicine Information More InfoDocument9 pagesBrand Name Generic Name Disease Group Consumer Medicine Information More InfoBairavi RathakrishnanNo ratings yet
- The Nursing Process: Dr. Abdalkarim RadwanDocument62 pagesThe Nursing Process: Dr. Abdalkarim RadwanAngelique Ramos PascuaNo ratings yet
- Nursing Care of Clients with Physiologic and Psychosocial AlterationsDocument14 pagesNursing Care of Clients with Physiologic and Psychosocial AlterationsBrianMarBeltran100% (1)
- Stress Management in StudentsDocument25 pagesStress Management in StudentsJangNo ratings yet
- Measuring Lung Capacity PDFDocument5 pagesMeasuring Lung Capacity PDFSip BioNo ratings yet
- Leptin HormoneDocument21 pagesLeptin Hormonemarah almahameed100% (2)
- Varicose Vein SurgeryDocument11 pagesVaricose Vein SurgeryDaud YudhistiraNo ratings yet
- NCP Pancreatic MassDocument4 pagesNCP Pancreatic MassJan Lianne BernalesNo ratings yet
- CROSSBITE According To GraberDocument29 pagesCROSSBITE According To GraberAslamCv100% (1)
- Nerve Cell - Cell ProjectDocument23 pagesNerve Cell - Cell Projectapi-327766139No ratings yet
- Unstable Angina Case ReportDocument24 pagesUnstable Angina Case ReportaybatariNo ratings yet
- Thoughts Thoughts: 'Universe, Please Help Me Maintain An Effective Meditative-State. Thank You.'Document4 pagesThoughts Thoughts: 'Universe, Please Help Me Maintain An Effective Meditative-State. Thank You.'Mincheol KangNo ratings yet
- Nurs 205 Concept MapDocument1 pageNurs 205 Concept MapJami SpearsNo ratings yet
- Twins Bootcamp StudyDocument5 pagesTwins Bootcamp Studyandi dirhanNo ratings yet
- Nucleus DropDocument1 pageNucleus DropYovinus DenyNo ratings yet
- Varicella in Pregnancy GuidelineDocument5 pagesVaricella in Pregnancy GuidelineYwagar YwagarNo ratings yet
- Review On Surge Drug Delivery TechnologyDocument8 pagesReview On Surge Drug Delivery TechnologyNayeli MercadoNo ratings yet
- 13 Implant Supported Fixed ProsthesesDocument52 pages13 Implant Supported Fixed ProsthesesJúliaJulieNo ratings yet
- Practicing The A, B, C'S: Albert Ellis and REBTDocument24 pagesPracticing The A, B, C'S: Albert Ellis and REBTShareenjitKaurNo ratings yet
- A Critical Examination of The Homeopathic Treatment of Chronic Fatigue SyndromeDocument18 pagesA Critical Examination of The Homeopathic Treatment of Chronic Fatigue SyndromeceliastNo ratings yet
- Shiatsu Helps Treat AsthmaDocument9 pagesShiatsu Helps Treat Asthmaडा. सत्यदेव त्यागी आर्यNo ratings yet
- WREBDocument94 pagesWREBJessica Bahga100% (1)
- Topical and Structurated Syllabus Corrected.1Document10 pagesTopical and Structurated Syllabus Corrected.1Kikis Dom100% (1)
- Guidelines Antibiotic Step-Down TherapyDocument1 pageGuidelines Antibiotic Step-Down TherapyGayle GreyNo ratings yet
- Chakras and Yoga: Finding Inner Harmony Through Practice, Awaken the Energy Centers for Optimal Physical and Spiritual Health.From EverandChakras and Yoga: Finding Inner Harmony Through Practice, Awaken the Energy Centers for Optimal Physical and Spiritual Health.Rating: 4 out of 5 stars4/5 (2)
- Boundless: Upgrade Your Brain, Optimize Your Body & Defy AgingFrom EverandBoundless: Upgrade Your Brain, Optimize Your Body & Defy AgingRating: 4.5 out of 5 stars4.5/5 (66)
- Hero Maker: 12 Weeks to Superhero Fit: A Hollywood Trainer's REAL Guide to Getting the Body You've Always WantedFrom EverandHero Maker: 12 Weeks to Superhero Fit: A Hollywood Trainer's REAL Guide to Getting the Body You've Always WantedRating: 4 out of 5 stars4/5 (1)
- The Yogi Code: Seven Universal Laws of Infinite SuccessFrom EverandThe Yogi Code: Seven Universal Laws of Infinite SuccessRating: 4.5 out of 5 stars4.5/5 (104)
- Calisthenics: Guide for Bodyweight Exercise, Build your Dream Body in 30 MinutesFrom EverandCalisthenics: Guide for Bodyweight Exercise, Build your Dream Body in 30 MinutesRating: 3 out of 5 stars3/5 (5)
- Relentless: From Good to Great to UnstoppableFrom EverandRelentless: From Good to Great to UnstoppableRating: 5 out of 5 stars5/5 (780)
- Functional Training and Beyond: Building the Ultimate Superfunctional Body and MindFrom EverandFunctional Training and Beyond: Building the Ultimate Superfunctional Body and MindRating: 4.5 out of 5 stars4.5/5 (1)
- Strong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerFrom EverandStrong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerRating: 4 out of 5 stars4/5 (5)
- Muscle for Life: Get Lean, Strong, and Healthy at Any Age!From EverandMuscle for Life: Get Lean, Strong, and Healthy at Any Age!Rating: 4.5 out of 5 stars4.5/5 (22)
- Peak: The New Science of Athletic Performance That is Revolutionizing SportsFrom EverandPeak: The New Science of Athletic Performance That is Revolutionizing SportsRating: 5 out of 5 stars5/5 (95)
- Wall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesFrom EverandWall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesNo ratings yet
- 7 Weeks to 10 Pounds of Muscle: The Complete Day-by-Day Program to Pack on Lean, Healthy Muscle MassFrom Everand7 Weeks to 10 Pounds of Muscle: The Complete Day-by-Day Program to Pack on Lean, Healthy Muscle MassRating: 4 out of 5 stars4/5 (2)
- If You Like Exercise … Chances Are You’Re Doing It Wrong: Proper Strength Training for Maximum ResultsFrom EverandIf You Like Exercise … Chances Are You’Re Doing It Wrong: Proper Strength Training for Maximum ResultsRating: 4.5 out of 5 stars4.5/5 (7)
- SAS Training Manual: How to get fit enough to pass a special forces selection courseFrom EverandSAS Training Manual: How to get fit enough to pass a special forces selection courseRating: 4 out of 5 stars4/5 (3)
- Meat Is for Pussies: A How-To Guide for Dudes Who Want to Get Fit, Kick Ass, and Take NamesFrom EverandMeat Is for Pussies: A How-To Guide for Dudes Who Want to Get Fit, Kick Ass, and Take NamesRating: 3.5 out of 5 stars3.5/5 (8)
- Body by Science: A Research Based Program for Strength Training, Body building, and Complete Fitness in 12 Minutes a WeekFrom EverandBody by Science: A Research Based Program for Strength Training, Body building, and Complete Fitness in 12 Minutes a WeekRating: 4.5 out of 5 stars4.5/5 (84)
- Yamas & Niyamas: Exploring Yoga's Ethical PracticeFrom EverandYamas & Niyamas: Exploring Yoga's Ethical PracticeRating: 4.5 out of 5 stars4.5/5 (110)
- Slow Burn: Burn Fat Faster By Exercising SlowerFrom EverandSlow Burn: Burn Fat Faster By Exercising SlowerRating: 4.5 out of 5 stars4.5/5 (6)
- ROAR: How to Match Your Food and Fitness to Your Unique Female Physiology for Optimum Performance, Great Health, and a Strong, Lean Body for LifeFrom EverandROAR: How to Match Your Food and Fitness to Your Unique Female Physiology for Optimum Performance, Great Health, and a Strong, Lean Body for LifeRating: 4.5 out of 5 stars4.5/5 (44)
- Applied Polyvagal Theory in Yoga: Therapeutic Practices for Emotional HealthFrom EverandApplied Polyvagal Theory in Yoga: Therapeutic Practices for Emotional HealthNo ratings yet
- Beastmode Calisthenics: A Simple and Effective Guide to Get Ripped with Bodyweight TrainingFrom EverandBeastmode Calisthenics: A Simple and Effective Guide to Get Ripped with Bodyweight TrainingNo ratings yet
- Light on Yoga: The Definitive Guide to Yoga PracticeFrom EverandLight on Yoga: The Definitive Guide to Yoga PracticeRating: 5 out of 5 stars5/5 (1)
- Calisthenics: 12 Effective Exercises to Build Calisthenics Body in 14 DaysFrom EverandCalisthenics: 12 Effective Exercises to Build Calisthenics Body in 14 DaysRating: 3 out of 5 stars3/5 (5)
- The Calisthenics Codex: Fifty Exercises for Functional FitnessFrom EverandThe Calisthenics Codex: Fifty Exercises for Functional FitnessRating: 4 out of 5 stars4/5 (9)
- 7 Weeks to 50 Pull-Ups: Strengthen and Sculpt Your Arms, Shoulders, Back, and Abs by Training to Do 50 Consecutive Pull-UpsFrom Everand7 Weeks to 50 Pull-Ups: Strengthen and Sculpt Your Arms, Shoulders, Back, and Abs by Training to Do 50 Consecutive Pull-UpsRating: 3.5 out of 5 stars3.5/5 (2)
- Roxane Gay & Everand Originals: Built for This: The Quiet Strength of PowerliftingFrom EverandRoxane Gay & Everand Originals: Built for This: The Quiet Strength of PowerliftingRating: 4.5 out of 5 stars4.5/5 (19)
- The Professional Yoga Teacher's Handbook: The Ultimate Guide for Current and Aspiring Instructors?Set Your Intention, Develop Your Voice, and Build Your CareerFrom EverandThe Professional Yoga Teacher's Handbook: The Ultimate Guide for Current and Aspiring Instructors?Set Your Intention, Develop Your Voice, and Build Your CareerRating: 5 out of 5 stars5/5 (2)