Professional Documents
Culture Documents
Word Bank: Edward Lee Physiology Test Resp
Uploaded by
Edward LeeOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Word Bank: Edward Lee Physiology Test Resp
Uploaded by
Edward LeeCopyright:
Available Formats
Edward Lee Physiology Test Resp.
WORD BANK
Acidosis / Alkalosis increased/decreased acidity of blood Apnea suspension of external breathing Asthma inflammation of airways, collection of symptoms Compliance tendency of an organ to resist recoil toward its original dimension Hypercapnia too much CO2 Hypocapnia too little CO2 Hypoxia deprivation of O2 Respiration (ventilation of lungs) exchange of gases between air + blood, blood + tissue fluid use of O2 in cellular metabolism
1. flow of air from nose to pulmonary alveoli
General Aspects of Respiratory System Airflow in lungs (bronchi bronchioles alveoli) Conducting division (passages serve only for airflow, nostrils to bronchioles) Respiratory division (alveoli + distal gas-exchange regions) Upper respiratory tract (organs in head + neck, nose through larynx) Lower respiratory tract (organs of the thorax, trachea through lungs)
2. structure and function of components of the respiratory tract including pleural membranes
Nose
Functions to warm, cleanse, humidify inhaled air, detects odors, resonating chamber>modify voice Bony + cartilaginous supports superior half: nasal bones medially + maxillae laterally inferior half: lateral + alar cartilages ala nasi: flared portion shaped by dense CT, forms lateral wall of each nostril Olfactory epithelium lines superior concha + parts of the nasal septum. Bones beneath epithelium are irregular and air is turbulent, causing odorants to contact olfactory epithelium. Epithelial cilia arise from olfactory cells. They lack dynein and dont move. The cilia cell membrane contain olfactory receptors to receive odorants dissolved in the serous epithelium. Axons of the olfactory cells collect in the lamina propria. Olfactory cells and processes receive mechanical, metabolic support from supporting (sustentacular) cells. Basal cells divide, differentiate to those. Paranasal Sinuses These are air-filled, mucosallined cavities which develop in facial + cranial bones. The spaces communicate with the nasal airway. Their function is unknown but has been subject to a great deal of speculation. They could serve to decrease the weight of the skull or to function as resonators for the voice. In lower animals with a more acute sense of smell, the sinuses are largely lined by olfactory
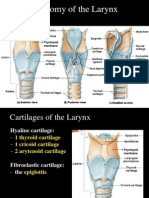
epithelium. Sinuses may have originally developed to increase the available surface area for the sense of smell. Therefore, in humans, with olfaction limited to a much smaller area, sinuses may be vestigial anachronisms. Though their function is obscure, their medical significance is not. Sinuses frequently become infected due to obstruction of normal drainage, + negative pressure in a sinus can cause headache. Pharynx Nasopharynx (pseudostratified epithelium) dorsal to soft palate, receives auditory tubes + contains pharyngeal tonsil air turns 90 downward trapping large particles (>10m) Oropharynx (stratified squamous epithelium) space between soft palate + root of tongue, inferiorly as far as hyoid bone, contains palatine + lingual tonsils Laryngopharynx (stratified squamous epithelium) hyoid bone to cricoid cartilage (inferior end of larynx) Larynx Glottis - superior opening Epiglottis - flap of tissue that guards glottis, directs food + drink to esophagus Infant larynx (by age 2, more muscular tongue forces larynx down) higher in throat, forms a continuous airway from nasal cavity that allows breathing while swallowing 9 cartilages of larynx Epiglottic cartilage Thyroid cartilage - largest, has laryngeal prominence Cricoid cartilage - connects larynx to trachea Arytenoid cartilages (2) - posterior to thyroid cartilage Corniculate cartilages (2) - attached to arytenoid cartilages like a pair of little horns Cuneiform cartilages (2) - support soft tissue between arytenoids + the epiglottis Trachea Rigid tube 4.5 in. long + 2.5 in. in diameter, anterior to esophagus Supported by 16 to 20 C-shaped cartilaginous rings opening in rings faces posteriorly towards esophagus trachealis muscle spans rings openings, adjusts air by expanding/contracting Larynx + trachea lined with ciliated pseudostratified epithelium. mucociliary escalator The trachea is lined by respiratory epithelium. The number of goblet cells is variable + depends on physical or chemical irritation of the epithelium which increase goblet cell number. Prolonged intense irritation of the epithelium may lead to its transformation to a stratified squamous epithelium (squamous metaplasia). In addition to the staple of basal cells, ciliated cells + goblet cells , the respiratory epithelium also contains
brush cells, endocrine cells (or small granule cells, function not clear), surfactant-producing cells (or Clara cells), + serous cells. The trachea is stabilised by 16-20 C-shaped cartilages (hyaline cartilage). The free dorsal ends of the cartilages are connected by bands of smooth muscle (trachealis muscle) + connective tissue fibers. Longitudinal collagenous + elastic connective tissue fibers (annular ligaments) link the individual cartilages + allow both the lengthening + shortening of the trachea for example during swallowing or movements of the neck. They are inseparable from the fibers of the perichondrium. The tracheal cartilages may ossify with age. Bronchial Tree Primary bronchi (C-shaped rings) arise from trachea, after 2-3 cm enter hilum of lungs right bronchus slightly wider + more vertical (aspiration) Secondary (lobar) bronchi (overlapping plates) branches into one secondary bronchus for each lobe Tertiary (segmental) bronchi (overlapping plates) [10 right, 8 left] bronchopulmonary segment: portion of lung supplied by each Bronchioles (lack cartilage) have layer of smooth muscle pulmonary lobule: portion ventilated by one bronchiole divides into 50 - 80 terminal bronchioles terminal bronchioles have cilia , give off 2 or more respiratory bronchioles respiratory bronchioles divide into 2-10 alveolar ducts Alveolar ducts - end in alveolar sacs Alveoli - bud from respiratory bronchioles, alveolar ducts + alveolar sacs Pleura + Pleural Fluid (Visceral + parietal layers, with pleural cavity + fluid) reduction of friction compartmentalization - prevents spread of infection creation of pressure gradient - lower pressure assists in inflation of lungs The pleura + pleural fluid function to reduce friction between the lungs + the inside of the chest wall during breathing. This function of the pleural cavity can be disrupted in several ways: Pneumothorax (collapsed lung): air enters the pleural cavity, either from the outside or from the lungs. This can be the result of a penetrating chest wound, or of an internal injury. Pleural Infusion: fluid accumulates in the pleural space, compressing the lungs. This can result for example from lung cancer, infection or heart failure. Mesothelioma: this is a type of cancer caused by asbestos exposure. The epithelium of the alveoli is formed by two cell types:
Alveolar type I cells (small alveolar cells or type I pneumocytes) are extremely flattened (the cell may be as thin as 0.05 m) + form the bulk (95%) of the surface of the alveolar walls. The shape of the cells is very complex, + they may actually form part of the epithelium on both faces of the alveolar wall. Alveolar type II cells (large alveolar cells or type II pneumocytes) are irregularly (sometimes cuboidal) shaped. They form small bulges on the alveolar walls. Type II alveolar cells contain are large number of granules called cytosomes (or multilamellar bodies), which consist of precursors to pulmonary surfactant (the mixture of phospholipids which keep surface tension in the alveoli low) . There are just about as many type II cells as type I cells. Their small contribution to alveolar area is explained by their shape. Bullae are large dilated airspaces that bulge out from beneath the pleura (in emphysema)
3. the gas laws of respiratory physiology, partial pressures
Mechanics of Ventilation Gas laws - Boyles law: pressure + volume; Charles law: temperature + volume; Daltons law: partial pressure; Henrys law: gases dissolving in liquids Pressure + Flow Atmospheric pressure drives respiration Intrapulmonary pressure + lung volume pressure is inversely proportional to volume (for a given amount of gas, as volume , pressure + as volume , pressure ) Pressure gradients difference between atmospheric + intrapulmonary pressure created by changes in volume of thoracic cavity
4. mechanisms of breathing including anatomy, pressure gradients, air flow
Inspiration Muscles Involved Diaphragm (dome shaped) (contraction flattens diaphragm) Scalenes (fix first pair of ribs) External intercostals (elevate 2 - 12 pairs) Pectoralis minor, sternocleidomastoid + erector spinae muscles - used in deep inspiration Inspiration Pressure Changes intrapleural pressure - as volume of thoracic cavity , visceral pleura clings to parietal pleura intrapulmonary pressure - lungs expand with the visceral pleura Transpulmonary pressure - intrapleural minus intrapulmonary pressure (not all pressure change in the pleural cavity is transferred to the lungs) Inflation of lungs aided by warming of inhaled air A quiet breathe flows 500 ml of air through lungs Passive Expiration During quiet breathing, expiration achieved by elasticity of lungs + thoracic cage As volume of thoracic cavity , intrapulmonary pressure + air is expelled
After inspiration, phrenic nerves continue to stimulate diaphragm, -> braking action, elastic recoil Forced Expiration Internal intercostal muscles - depress the ribs Contract abdominal muscles - intra-abdominal pressure forces diaphragm upward, pressure on thoracic cavity Pneumothorax Presence of air in pleural cavity - negative intrapleural pressure allows lungs to recoil + collapse Collapse of lung (or part of lung) is called atelectasis Resistance to Airflow Pulmonary compliance distensibility of the lungs; the change in lung volume relative to a given change in transpulmonary pressure decreased in diseases with pulmonary fibrosis (TB) Bronchiolar diameter primary control over resistance to airflow bronchoconstriction - triggered by airborne irritants, cold air, histamine bronchodilation (sympathetic nerves, epinephrine) Alveolar Surface Tension Thin film of water necessary for gas exchange Problem created by surface tension resists expansion of alveoli + distal bronchioles law of Laplace: force drawing alveoli in on itself is directly proportional to surface tension + inversely proportional to the radius of the alveolus Pulmonary surfactant (great alveolar cells) disrupts hydrogen bonds, surface tension during expiration contraction, surfactant concentration prevents alveolar collapse Respiratory distress syndrome of premature infants Alveolar Ventilation Dead air - fills conducting division of airway, cannot exchange gases Anatomic dead space - conducting division of airway Physiologic dead space - sum of anatomic dead space + any pathological alveolar dead space Alveolar ventilation rate air that actually ventilates alveoli X respiratory rate directly relevant to bodys ability to exchange gases Nonrespiratory Air Movements Functions other than alveolar ventilation flow of blood + lymph from abdominal to thoracic vessels Variations in ventilation also serve speaking, yawning, sneezing, coughing Valsalva maneuver - take a deep breath, hold it + then contract abdominal muscles; increases pressure in the abdominal cavity. To expel urine, feces + to aid in childbirth
Spirometer (device a subject breathes into that measures ventilation) Respiratory volumes tidal volume: air inhaled or exhaled in one quiet breath inspiratory reserve volume: air in excess of tidal inspiration that can be inhaled with maximum effort expiratory reserve volume: air in excess of tidal expiration that can be exhaled with maximum effort residual volume: air remaining in lungs after maximum expiration, keeps alveoli inflated Respiratory Capacities Vital capacity - amount of air that can be exhaled with maximum effort after maximum inspiration; assess strength of thoracic muscles + pulmonary function Inspiratory capacity - maximum amount of air that can be inhaled after a normal tidal expiration Functional residual capacity - amount of air in lungs after a normal tidal expiration Total lung capacity [maximum amount of air lungs can contain] Effects on Respiratory Volumes + Capacities Age: lungs less compliant, respiratory muscles weaken Exercise: maintains strength of respiratory muscles Body size: proportional, big body has large lungs Restrictive disorders: compliance + vital capacity Obstructive disorders: interfere with airflow, expiration more effort or less complete Forced expiratory volume: % of vital capacity exhaled/ time; healthy adult - 75 to 85% in 1 sec Minute respiratory volume: TV x respiratory rate, at rest 500 x 12 = 6 L/min; maximum: 125 to 170 L/min
6. Neural Control of Ventilation
5. Measurements of Ventilation
Breathing depends on repetitive stimuli from brain Neurons in medulla oblongata + pons control unconscious breathing Voluntary control provided by the motor cortex Inspiratory neurons: fire during inspiration Expiratory neurons: fire during forced expiration Fibers travel down spinal cord to lower motor neurons, fibers of phrenic nerve go to diaphragm + intercostal nerves go to intercostal muscles Respiratory Control Centers Two respiratory nuclei in medulla oblongata inspiratory center (dorsal respiratory group) more frequently they fire, more deeply you inhale longer duration they fire, breath is prolonged, slow rate expiratory center (ventral respiratory group) - involved in forced expiration Pons pneumotaxic center - sends continual inhibitory impulses to inspiratory center, as
impulse frequency rises, breathe faster + shallower apneustic center - sends continual stimulatory impulses to inspiratory center Afferent Connections to Brainstem Input from limbic system + hypothalamus respiratory effects of pain + emotion Input from chemoreceptors brainstem + arteries monitor blood pH, CO2 + O2 levels Input from airways + lungs response to inhaled irritants - stimulate vagal afferents to medulla, results in bronchoconstriction or coughing inflation reflex - excessive inflation triggers this reflex, stops inspiration Voluntary Control Neural pathways motor cortex of frontal lobe of cerebrum sends impulses down corticospinal tracts to respiratory neurons in spinal cord, bypassing brainstem Limitations on voluntary control blood CO2 + O2 limits cause automatic respiration Composition of Air Mixture of gases, each contributes its partial pressure nitrogen constitutes 78.6% of the atmosphere, PN2 = 78.6% x 760 mmHg = 597 mmHg PO2 = 159, PH2O = 3.7, PCO2 = 0.3 mmHg (597 + 159 + 3.7 + 0.3 = 760) Partial pressures determine rate of diffusion of gas + gas exchange between blood + alveolus Alveolar air humidified, exchanges gases with blood, mixes with residual air contains: PN2 = 569, PO2 = 104, PH2O = 47, PCO2 = 40 mmHg
7. gas exchange and transport
Air-Water Interface Gases diffuse down their concentration gradients Henrys law: amount of gas that dissolves in water is determined by its solubility in water + its partial pressure in air Alveolar Gas Exchange Time required for gases to equilibrate = 0.25 sec RBC transit time at rest = 0.75 sec to pass through alveolar capillary RBC transit time with vigorous exercise = 0.3 sec Concentration gradients of gases PO2 = 104 in alveolar air versus 40 in blood PCO2 = 46 in blood arriving versus 40 in alveolar air Gas solubility - CO2 is 20 times as soluble as O2 Membrane thickness - only 0.5 m thick Membrane surface area - 100 ml blood in alveolar capillaries, spread over 70 m2 Ventilation-perfusion coupling - areas of good ventilation need good perfusion (vasodilation)
Oxygen Transport Concentration in arterial blood 20 ml/dl, (98.5% bound to hemoglobin, 1.5% dissolved) Binding to hemoglobin each heme group of 4 globin chains may bind O2 oxyhemoglobin (HbO2 ), deoxyhemoglobin (HHb) Oxyhemoglobin dissociation curve relationship between hemoglobin saturation + PO2 is not a simple linear one after binding with O2, hemoglobin changes shape to facilitate further uptake (positive feedback cycle) Carbon Dioxide Transport As carbonic acid - 90% [CO2 + H2O H2CO3 HCO3- + H+] As carbaminohemoglobin (HbCO2)- 5% binds to amino groups of Hb (and plasma proteins) As dissolved gas - 5% Alveolar exchange of CO2 carbonic acid - 70% , carbaminohemoglobin - 23%, dissolved gas - 7% Systematic Gas Exchange CO2 loading carbonic anhydrase in RBC catalyzes [CO2 + H2O H2CO3 HCO3- + H+] chloride shift keeps reaction proceeding, exchanges HCO3- for Cl(H+ binds to hemoglobin) O2 unloading H+ binding to HbO2 its affinity for O2 Hb arrives 97% saturated, leaves 75% saturated - venous reserve utilization coefficient - amount of oxygen Hb has released 22% Alveolar Gas Exchange [Pt 2] Reactions are reverse of systemic gas exchange CO2 unloading as Hb loads O2 its affinity for H+ decreases, H+ dissociates from Hb + bind with HCO3 CO2 + H2O H2CO3 HCO3- + H+ reverse chloride shift keeps reaction proceeding, exchanges Cl- for HCO3(which diffuses back into RBC), free CO2 generated + diffuses into alveolus to be exhaled Adjustment to Tissues Metabolic Needs Factors affecting O2 unloading (HbO2 releases O2) ambient PO2: active tissue has PO2 , O2 is released temperature: active tissue has increased temp, O2 is released (see next slide) Bohr effect: active tissue has CO2, which raises H+ + lowers pH, O2 is released (see following slide)
8. blood chemistry
bisphosphoglycerate (BPG): RBCs produce this as a metabolic intermediate, BPG binds to Hb + causes HbO2 to release O2 body temp (fever), TH, GH, testosterone, epinephrine raise BPG, O2 unloading Factors affecting CO2 loading Haldane effect: low level of HbO2 (as in active tissue) enables blood to transport more CO2 HbO2 does not bind CO2 as well as deoxyhemoglobin (HHb) HHb binds more H+ than HbO2, shifts the CO2 + H2O HCO3- + H+ reaction to the right
Blood Chemistry + Respiratory Rhythm Chemoreceptors monitor pH, PCO2, PO2 of body fluids peripheral chemoreceptors - aortic bodies signal medulla by vagus nerves, while carotid bodies signal medulla by glossopharyngeal nerves central chemoreceptors (surface of medulla) [primarily monitor pH of CSF] Effects of Hydrogen Ions pH of CSF (most powerful respiratory stimulus) Respiratory acidosis (pH < 7.35) caused by failure of pulmonary ventilation hypercapnia (PCO2) > 43 mmHg CO2 easily crosses blood-brain barrier, in CSF the CO2 reacts with water + releases H+, central chemoreceptors strongly stimulate inspiratory center corrected by hyperventilation, pushes reaction to the left by blowing off CO2 CO2 (expired) + H2O H2CO3 HCO3- + H+ Respiratory alkalosis (pH < 7.35) ( H+, lowers pH to normal) hypocapnia (PCO2) < 37 mmHg corrected by hypoventilation, pushes reaction to the right CO2 + H2O H2CO3 HCO3- + H+ pH imbalances can have metabolic causes - diabetes mellitus: fat oxidation causes ketoacidosis, can be compensated for by Kussmaul respiration, (deep rapid breathing) Effects of Carbon Dioxide Indirect effects (through pH) Direct effects ( CO2 may directly stimulate peripheral chemoreceptors + trigger ventilation more quickly than central chemoreceptors Effects of Oxygen (usually little effect) Chronic hypoxemia, PO < 60 mmHg, can significantly stimulate ventilation emphysema, pneumonia. high altitudes after several days Hypoxia
LABELING
hypoxemic hypoxia - usually due to inadequate pulmonary gas exchange. high altitudes, drowning, aspiration, respiratory arrest, degenerative lung diseases, CO poisoning ischemic hypoxia - inadequate circulation anemic hypoxia - anemia histotoxic hypoxia - metabolic poison (cyanide) cyanosis - blueness of skin primary effect of hypoxia is tissue necrosis, organs with high metabolic demands first Oxygen excess [hyperbaric used to be treatment for premature infants but caused retinal damage] oxygen toxicity: pure O breathed at 2.5 atm or greater generates free radicals + H2O2, destroys enzymes, damages nervous tissue, seizures, coma death Alveoli Nares nostrils Bronchiole Nasal Conchae bones Bronchus Nasopharynx above oropharynx Cricoid cartilage top of larynx Oropharynx above laryngopharynx Epiglottis Thyroid Cartilage Eustachian tube opening hole in cheek Trachea, Palate, Larynx, Laryngopharynx
DISEASES
Lung cancer is the leading cancer killer in both men +
women. An estimated 173,700 new cases of lung cancer + an estimated 160,440 deaths from lung cancer will occur in the United States during 2004. The rate of lung cancer cases appears to be dropping among white + African-American men in the United States, while it continues to rise among both white + African-American women. There are two major types of lung cancer: non-small cell lung cancer + small cell lung cancer. Non-small cell lung cancer is much more common. It usually spreads to different parts of the body more slowly than small cell lung cancer. Squamous cell carcinoma, adenocarcinoma, + large cell carcinoma are three types of non-small cell lung cancer. Small cell lung cancer also called oat cell cancer, accounts for about 20% of all lung cancer. Smoking + Lung Cancer Lung cancer accounts for more deaths than any other form of cancer most important cause is smoking (15 carcinogens) Squamous-cell carcinoma (most common) begins with transformation of bronchial epithelium into stratified squamous
dividing cells invade bronchial wall, cause bleeding lesions dense swirls of keratin replace functional respiratory tissue Smoking is the number one cause of lung cancer. Lung cancer may also be the most tragic cancer because in most cases, it might have been prevented - 87% of lung cancer cases are caused by smoking. Cigarette smoke contains more than 4,000 different chemicals, many of which are proven cancer-causing substances, or carcinogens. Smoking cigars or pipes also increases the risk of lung cancer. The more time + quantity you smoke, the greater your risk of lung cancer. But if you stop smoking, the risk of lung cancer decreases each year as normal cells replace abnormal cells. After ten years, the risk drops to a level that is one-third to one-half of the risk for people who continue to smoke. In addition, quitting smoking greatly reduces the risk of developing other smoking-related diseases, such as heart disease, stroke, emphysema + chronic bronchitis. In its early stages, lung cancer usually does not cause symptoms. When symptoms occur, the cancer is often advanced. Symptoms of lung cancer include chronic cough, hoarseness, coughing up blood, weight loss & loss of appetite, shortness of breath, mysterious fever, wheezing, repeated bouts of bronchitis or pneumonia, chest pain Progression 90% of lung tumors originate in primary bronchi Tumor invades bronchial wall, compresses airway + may cause atelectasis Often first sign is coughing up blood Metastasis is rapid + has usually occurred by time of diagnosis common sites: pericardium, heart, bones, liver, lymph nodes + brain Prognosis poor 7% of patients survive 5 years after diagnosis Chronic Obstructive Pulmonary Disease Asthma - allergen triggers histamine release, intense bronchoconstriction Other COPDs usually associated with smoking chronic bronchitis cilia immobilized + in number, goblet cells enlarge + produce excess mucus, sputum formed (mixture of mucus + cellular debris) which is ideal growth media for bacteria, chronic infection + bronchial inflammation develops emphysema alveolar walls break down, less respiratory membrane for gas exchange, lungs fibrotic, less elastic, air passages collapse, obstruct outflow of air, air stuck in lungs
pulmonary compliance + vital capacity hypoxemia, hypercapnia, respiratory acidosis hypoxemia stimulates erythropoietin release + leads to polycythemia cor pulmonale - hypertrophy + potential failure of right heart due to obstruction of pulmonary circulation Restrictive lung disease is caused by a decrease in the amount of air that your lungs can hold. Your lungs become "stiff," which reduces their ability to expand when you inhale. Restrictive disorders include sarcoidosis + pulmonary fibrosis. Obstructive lung disease is due to a decrease in the amount of air that you can exhale from your lungs. This is caused by narrowing or blockage of the airways. Obstructive disorders include emphysema + asthma. Breathing tests (pulmonary function tests) help diagnose restrictive + obstructive lung diseases. There are a number of restrictive disorders of the respiratory system that cause difficult breathing. Some produce a rigidity of the lungs (pneumoconiosis, collagen disease, pulmonary fibrosis); other involve the interactions of muscles + nerves (myasthenia gravis, Guillain Barre syndrome); + still others prevent the lungs from expanding to full volume (pleural effusion, pneumothorax, hemothorax). A restrictive deficit in pulmonary function can also be caused by pulmonary edema, which usually stems from heart failure or occasionally from toxic inhalants. Difficulty breathing Difficulty breathing (dyspnea) comes after any strenuous activity. Troubled breathing is sometimes experienced in pregnancy, since the uterus expands upward, reducing the possibility of a full inhalation. Severe obesity can also reduce the capacity of the lungs to inhale fully. The primary symptom of bronchitis is a deep cough that brings up yellowish or grayish phlegm from the lungs. With emphysema, the shortness of breath gradually becomes worse over the years. The distinct symptoms of bronchitis + the gradual onset of emphysema will usually prevent these disorders from being misdiagnosed as severe anxiety or panic. Dyspnea may occur in any of the various diseases of the heart + lungs, but it is more prominent in those associated with lung congestion. For example, mitral stenosis occurs when a small valve between the left upper chamber + left lower chamber of the heart (the left atrium + left ventricle) becomes abnormally narrow. As blood is forced through the heart, pressure backs up into the lungs + produces congestion. It is this congestion that causes breathlessness. Other possible cardiovascular problems that can lead to difficulty breathing include left ventricular failure, aortic insufficiency, pericardial effusion, + cardiac arrhythmia. Asthma, or hyperreactive airway disease: Exercise-induced asthma (EIA), or exercise-induced bronchospasm: exercise or vigorous physical activity triggers acute bronchospasm in persons with heightened airway reactivity. It is observed primarily in persons who are
asthmatic but can also be found in patients with atopy, allergic rhinitis, or cystic fibrosis + even in healthy persons The pathophysiology of asthma is complex + involves the following components: (1) airway inflammation, (2) intermittent airflow obstruction, + (3) bronchial hyperresponsiveness. The mechanism of inflammation in asthma may be acute, subacute, or chronic, + the presence of airway edema + mucus secretion also contributes to airflow obstruction + bronchial reactivity. Varying degrees of mononuclear cell + eosinophil infiltration, mucus hypersecretion, desquamation of the epithelium, smooth muscle hyperplasia, + airway remodeling are present. The presence of airway hyperresponsiveness or bronchial hyperreactivity in asthma is an exaggerated response to numerous exogenous + endogenous stimuli. The mechanisms involved include direct stimulation of airway smooth muscle + indirect stimulation by pharmacologically active substances from mediator-secreting cells such as mast cells or nonmyelinated sensory neurons. The degree of airway hyperresponsiveness generally correlates with the clinical severity of asthma. Asthma signs + symptoms can range from mild to severe. Warning signs + symptoms for adults can include: Increased shortness of breath or wheezing Disturbed sleep caused by shortness of breath, coughing or wheezing Chest tightness or pain Increased need to use bronchodilators medications that open up airways by relaxing the surrounding muscles A fall in peak flow rates as measured by a peak flow meter, a simple + inexpensive device that allows you to monitor your own lung function Asthma can develop at any age. If you're younger than 30, your asthma is probably triggered by allergies. Many people older than 30 with asthma are also allergic to airborne particles. For some people with asthma, particularly older adults, respiratory allergies don't seem to play a role. Instead, exposure to any irritant such as a virus, cigarette smoke, cold air, + even emotional stress can trigger wheezing. In most cases though, asthma results from a combination of allergic + nonallergic responses. You may react to one or more of the following triggers: Allergens, such as pollen, cockroaches + molds Air pollutants + irritants Smoking + secondhand smoke. Respiratory infections, including the common cold. Physical exertion, including exercise. Cold air. Certain medications, including beta blockers, aspirin + other nonsteroidal anti-inflammatory drugs. Sulfites (preservatives added to some perishable foods.) Gastroesophageal reflux disease (GERD), a condition in which stomach acids back up into your esophagus. GERD may trigger an asthma attack or make an attack worse. Sinusitis.
Chronic obstructive pulmonary disease COPD; Chronic obstructive airways disease; Chronic obstructive lung disease; Chronic bronchitis; Emphysema; Bronchitis - chronic
Last reviewed: May 1, 2011. Chronic obstructive pulmonary disease (COPD) is one of the most common lung diseases. It makes it difficult to breathe. There are two main forms of COPD: Chronic bronchitis, which involves a longterm cough with mucus Emphysema, which involves destruction of the lungs over time Most people with COPD have a combination of both conditions. Causes, incidence, and risk factors Smoking is the leading cause of COPD. The more a person smokes, the more likely that person will develop COPD. However, some people smoke for years and never get COPD. In rare cases, nonsmokers who lack a protein called alpha-1 antitrypsin can develop emphysema. Other risk factors for COPD are: Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and pollution Frequent use of cooking fire without proper ventilation Symptoms Cough, with or without mucus Fatigue Many respiratory infections Shortness of breath (dyspnea) that gets worse with mild activity Trouble catching one's breath Wheezing Because the symptoms of COPD develop slowly, some people may not know that they are sick. Signs and tests The best test for COPD is a lung function test called spirometry. This involves blowing out as hard as possible into a small machine that tests lung capacity. The results can be checked right away, and the test does not involve exercising, drawing blood, or exposure to radiation. Using a stethoscope to listen to the lungs can also be helpful. However, sometimes the lungs sound normal even when COPD is present. Pictures of the lungs (such as x-rays and CT scans) can be helpful, but sometimes look normal even when a person has COPD (especially chest x-ray). Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood. Treatment There is no cure for COPD. However, there are many things you can do to relieve symptoms and keep the disease from getting worse. Persons with COPD MUST stop smoking. This is the best way to slow down the lung damage. Medications used to treat COPD include: Inhalers (bronchodilators) to open the airways, such as ipratropium (Atrovent),
tiotropium (Spiriva), salmeterol (Serevent), formoterol (Foradil), or albuterol Inhaled steroids to reduce lung inflammation Anti-inflammatory medications such as montelukast (Singulair) and roflimulast are sometimes used In severe cases or during flare-ups, you may need to receive: Steroids by mouth or through a vein (intravenously) Bronchodilators through a nebulizer Oxygen therapy Assistance during breathing from a machine (through a mask, BiPAP, or endotracheal tube) Antibiotics are prescribed during symptom flareups, because infections can make COPD worse. You may need oxygen therapy at home if you have a low level of oxygen in your blood. Pulmonary rehabilitation does not cure the lung disease, but it can teach you to breathe in a different way so you can stay active. Exercise can help maintain muscle strength in the legs. Walk to build up strength. Ask the doctor or therapist how far to walk. Slowly increase how far you walk. Try not to talk when you walk if you get short of breath. Use pursed lip breathing when breathing out (to empty your lungs before the next breath) Things you can do to make it easier for yourself around the home include: Avoiding very cold air Making sure no one smokes in your home Reducing air pollution by getting rid of fireplace smoke and other irritants Eat a healthy diet with fish, poultry, or lean meat, as well as fruits and vegetables. If it is hard to keep your weight up, talk to a doctor or dietitian about eating foods with more calories. Surgery may be used, but only a few patients benefit from these surgical treatments: Surgery to remove parts of the diseased lung can help other areas (not as diseased) work better in some patients with emphysema Lung transplant for severe cases Support Groups People often can help ease the stress of illness by joining a support group in which members share common experiences and problems. See also: Lung disease - support group Expectations (prognosis) COPD is a long-term (chronic) illness. The disease will get worse more quickly if you do not stop smoking.
Patients with severe COPD will be short of breath with most activities and will be admitted to the hospital more often. These patients should talk with their doctor about breathing machines and end-oflife care. Complications Irregular heartbeat (arrhythmia) Need for breathing machine and oxygen therapy Right-sided heart failure or cor pulmonale (heart swelling and heart failure due to chronic lung disease) Pneumonia Pneumothorax Severe weight loss and malnutrition Thinning of the bones (osteoporosis)
Bronchitis
Inflammation - bronchi; Acute bronchitis
Last reviewed: April 27, 2010.
Bronchitis is inflammation of the main air passages to the lungs. Bronchitis may be short-lived (acute) or chronic, meaning that it lasts a long time and often recurs. See also: Chronic obstructive pulmonary disease (COPD)
Causes, incidence, and risk factors
Acute bronchitis generally follows a viral respiratory infection. At first, it affects your nose, sinuses, and throat and then spreads to the lungs. Sometimes, you may get another (secondary) bacterial infection in the airways.This means that bacteria infect the airways, in addition to the virus. People at risk for acute bronchitis include: The elderly, infants, and young children Persons with heart or lung disease Smokers Chronic bronchitis is a long-term condition. People have a cough that produces excessive mucus. To be diagnosed with chronic bronchitis, you must have a cough with mucus most days of the month for at least 3 months. Chronic bronchitis is one type of chronic obstructive pulmonary disease, or COPD for short. (Emphysema is another type of COPD.) The following things can make bronchitis worse: Air pollution Allergies Certain occupations (such as coal mining, textile manufacturing, or grain handling) Infections
Symptoms
The symptoms of either type of bronchitis may include: Chest discomfort Cough that produces mucus; if it's yellow-green, you are more likely to have a bacterial infection Fatigue Fever -- usually low Shortness of breath worsened by exertion or mild activity Wheezing Even after acute bronchitis has cleared, you may have a dry, nagging cough that lingers for several weeks. Additional symptoms of chronic bronchitis include:
Ankle, feet, and leg swelling Blue-colored lips from low levels of oxygen Frequent respiratory infections (such as colds or the flu)
Signs and tests
The health care provider will listen to your lungs with a stethoscope. Abnormal sounds in the lungs called rales or other abnormal breathing sounds may be heard. Tests may include: Chest x-ray Lung function tests provide information that is useful for diagnosis and your outlook. Pulse oximetry helps determine the amount of oxygen in your blood. This quick and painless test uses a device that is placed onto the end of your finger. Arterial blood gas is a more exact measurement of oxygen and carbon dioxide levels, but it requires a needle stick and is more painful. Sputum samples may be taken to check for signs of inflammation or bacterial infection.
You have a low-grade fever for 3 or more days You have thick, greenish mucus, especially if it has a bad smell You feel short of breath or have chest pain You have an underlying chronic illness, like heart or lung disease
Prevention
DO NOT smoke. Get a yearly flu vaccine and a pneumococcal vaccine as directed by your doctor. Reduce your exposure to air pollution. Wash your hands (and your children's hands) frequently to avoid spreading viruses and other infections. Symptoms depend on the type of cancer you have, but may include: Chest pain Cough that doesn't go away Coughing up blood Fatigue Losing weight without trying Loss of appetite Shortness of breath Wheezing Other symptoms that may also occur with lung cancer, often in the late stages: Bone pain or tenderness Eyelid drooping Facial paralysis Hoarseness or changing voice Joint pain Nail problems Shoulder pain Swallowing difficulty Swelling of the face or arms Weakness These symptoms can also be due to other, less serious conditions, so it is important to talk to your health care provider. For more information, see: Non-small cell lung cancer Small cell lung cancer
Treatment
You DO NOT need antibiotics for acute bronchitis caused by a virus. The infection will generally go away on its own within 1 week. Take the following steps for some relief: Do not smoke Drink plenty of fluids Rest Take aspirin or acetaminophen (Tylenol) if you have a fever. DO NOT give aspirin to children Use a humidifier or steam in the bathroom If your symptoms do not improve, your doctor may prescribe an inhaler to open your airways if you are wheezing. If your doctor thinks that you have a secondary bacterial infection, antibiotics may be prescribed. Most of the time, antibiotics are not needed or recommended. For any bronchitis, the most important step you can take is to QUIT smoking. If bronchitis is caught early enough, you can prevent the damage to your lungs.
Expectations (prognosis)
For acute bronchitis, symptoms usually go away within 7 to 10 days if you do not have an underlying lung disorder. However, a dry, hacking cough can linger for a number of months. The chance for recovery is poor for persons with advanced chronic bronchitis. Early recognition and treatment, combined with smoking cessation, significantly improve the chance of a good outcome.
Asthma
Bronchial asthma; Exercise-induced asthma
Last reviewed: May 1, 2011.
Complications
Pneumonia can develop from either acute or chronic bronchitis. If you have chronic bronchitis, you are more likely to develop recurrent respiratory infections. You may also develop: Emphysema Right-sided heart failure or cor pulmonale Pulmonary hypertension
Asthma is a disorder that causes the airways of the lungs to swell and narrow, leading to wheezing, shortness of breath, chest tightness, and coughing. See also: Pediatric asthma Work-related asthma
Causes, incidence, and risk factors
Asthma is caused by inflammation in the airways. When an asthma attack occurs, the muscles surrounding the airways become tight and the lining of the air passages swells. This reduces the amount of air that can pass by. In sensitive people, asthma symptoms can be triggered by breathing in allergy-causing substances (called allergens or triggers).
Calling your health care provider
Call your doctor if: You have a cough most days or you have a cough that returns frequently You are coughing up blood You have a high fever or shaking chills
Common asthma triggers include: Animals (pet hair or dander) Dust Changes in weather (most often cold weather) Chemicals in the air or in food Exercise Mold Pollen Respiratory infections, such as the common cold Strong emotions (stress) Tobacco smoke Aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) provoke asthma in some patients. Many people with asthma have a personal or family history of allergies, such as hay fever (allergic rhinitis) or eczema. Others have no history of allergies.
Symptoms
Most people with asthma have attacks separated by symptomfree periods. Some people have long-term shortness of breath with episodes of increased shortness of breath. Either wheezing or a cough may be the main symptom. Asthma attacks can last for minutes to days, and can become dangerous if the airflow is severely restricted. Symptoms include: Cough with or without sputum (phlegm) production Pulling in of the skin between the ribs when breathing (intercostal retractions) Shortness of breath that gets worse with exercise or activity Wheezing, which: Comes in episodes with symptom-free periods in between May be worse at night or in early morning May go away on its own Gets better when using drugs that open the airways (bronchodilators) Gets worse when breathing in cold air Gets worse with exercise Gets worse with heartburn (reflux) Usually begins suddenly Emergency symptoms: Bluish color to the lips and face Decreased level of alertness, such as severe drowsiness or confusion, during an asthma attack Extreme difficulty breathing Rapid pulse Severe anxiety due to shortness of breath Sweating Other symptoms that may occur with this disease: Abnormal breathing pattern --breathing out takes more than twice as long as breathing in Breathing temporarily stops Chest pain Tightness in the chest
Dust mites Molds Pet dander Pollens Common respiratory irritants include: Fumes from burning wood or gas Pollution Tobacco smoke The doctor will use a stethoscope to listen to the lungs. Asthma-related sounds may be heard. However, lung sounds are usually normal between asthma episodes. Tests may include: Arterial blood gas Blood tests to measure eosinophil count (a type of white blood cell) and IgE (a type of immune system protein called an immunoglobulin) Chest x-ray Lung function tests Peak flow measurements
Treatment
The goal of treatment is to avoid the substances that trigger your symptoms and control airway inflammation. You and your doctor should work together as a team to develop and carry out a plan for eliminating asthma triggers and monitoring symptoms. For information on treating asthma in children, see: Pediatric asthma There are two basic kinds of medication for treating asthma: Control drugs to prevent attacks Quick-relief drugs for use during attacks Control drugs for asthma control your symptoms if you don't have mild asthma. You must take them every day for them to work. Take them even when you feel okay. The most common control drugs are: Inhaled corticosteroids (such as Asmanex, Alvesco, Qvar AeroBid, Flovent, Pulmicort) prevent symptoms by helping to keep your airways from swelling up. Long-acting beta-agonist inhalers also help prevent asthma symptoms. Do not take long-acting betaagonist inhaler drugs alone. These drugs are almost always used together with an inhaled steroid drug. It may be easier to use an inhaler that contains both drugs. Other control drugs that may be used are: Leukotriene inhibitors (such as Singulair and Accolate) Omalizumab (Xolair) Cromolyn sodium (Intal) or nedocromil sodium (Tilade) Aminophylline or theophylline (rarely used anymore) Quick-relief drugs work fast to control asthma symptoms: You take them when you are coughing, wheezing, having trouble breathing, or having an asthma attack. They are also called "rescue" drugs. They also can be used just before exercising to help prevent asthma symptoms that are caused by exercise.
Signs and tests
Allergy testing may be helpful to identify allergens in people with persistent asthma. Common allergens include: Cockroach allergens
Tell your doctor if you are using quick-relief medicines twice a week or more to control your asthma symptoms. Your asthma may not be under control, and your doctor may need to change your dose of daily control drugs. Quick-relief drugs include: Short-acting bronchodilators (inhalers), such as Proventil, Ventolin, and Xopenex Your doctor might prescribe oral steroids (corticosteroids) when you have an asthma attack that is not going away. These are medicines that you take by mouth as pills, capsules, or liquid. Plan ahead. Make sure you do not run out of these medications. A severe asthma attack requires a check-up by a doctor. You may also need a hospital stay, oxygen, breathing assistance, and medications given through a vein (IV). ASTHMA CARE AT HOME Self-care skills that are important in taking care of your asthma are Know the asthma symptoms to watch out for Know how to take your peak flow reading and what it means Keep the phone number of your child's doctor or nurse with you. Know which triggers make your asthma worse and what to do when this happens. Children with asthma need a lot of support at school. They may need help from school staff to keep their asthma under control and to be able to do school activities. Asthma action plans are written documents for anyone with asthma. An asthma action plan should include: A plan for taking asthma medications when your condition is stable A list of asthma triggers and how to avoid them How to recognize when your asthma is getting worse, and when to call your doctor or nurse A peak flow meter is a simple device to measure how quickly you can move air out of your lungs. It can help you see if an attack is coming, sometimes even before any symptoms appear. Peak flow measurements can help show when medication is needed, or other action needs to be taken. Peak flow values of 50% - 80% of a specific person's best results are a sign of a moderate asthma attack, while values below 50% are a sign of a severe attack.
Death Decreased ability to exercise and take part in other activities Lack of sleep due to nighttime symptoms Permanent changes in the function of the lungs Persistent cough Trouble breathing that requires breathing assistance (ventilator)
Calling your health care provider
Call for an appointment with your health care provider if asthma symptoms develop. Call your health care provider or go to the emergency room if: An asthma attack requires more medication than recommended Symptoms get worse or do not improve with treatment You have shortness of breath while talking Your peak flow measurement is 50% - 80% of your personal best Go to the emergency room if the following symptoms occur: Drowsiness or confusion Severe shortness of breath at rest A peak flow measurement is less than 50% of your personal best Severe chest pain Bluish color to the lips and face Extreme difficulty breathing Rapid pulse Severe anxiety due to shortness of breath
Prevention
You can reduce asthma symptoms by avoiding known triggers and substances that irritate the airways. Cover bedding with "allergy-proof" casings to reduce exposure to dust mites. Remove carpets from bedrooms and vacuum regularly. Use only unscented detergents and cleaning materials in the home. Keep humidity levels low and fix leaks to reduce the growth of organisms such as mold. Keep the house clean and keep food in containers and out of bedrooms -- this helps reduce the possibility of cockroaches, which can trigger asthma attacks in some people. If a person is allergic to an animal that cannot be removed from the home, the animal should be kept out of the bedroom. Place filtering material over the heating outlets to trap animal dander. Eliminate tobacco smoke from the home. This is the single most important thing a family can do to help a child with asthma. Smoking outside the house is not enough. Family members and visitors who smoke outside carry smoke residue inside on their clothes and hair -- this can trigger asthma symptoms. Persons with asthma should also avoid air pollution, industrial dusts, and other irritating fumes as much as possible.
Support Groups
You can often ease the stress caused by illness by joining a support group, where members share common experiences and problems. See: Asthma and allergy - support group
Expectations (prognosis)
There is no cure for asthma, although symptoms sometimes improve over time. With proper self management and medical treatment, most people with asthma can lead normal lives.
Complications
The complications of asthma can be severe. Some include:
You might also like
- Fundamentals Workbook ENG RevDocument25 pagesFundamentals Workbook ENG RevottozirgNo ratings yet
- Many Mindfulness Exercises: Patricia Bear, LPCDocument6 pagesMany Mindfulness Exercises: Patricia Bear, LPCAna LeahNo ratings yet
- Respiratory System: Anatomy & PhysiologyDocument111 pagesRespiratory System: Anatomy & PhysiologyJape GarridoNo ratings yet
- The Miracle of Manaforce PowerDocument26 pagesThe Miracle of Manaforce PowerenekosaaneNo ratings yet
- Simple MeditationDocument2 pagesSimple MeditationDr.ManageNo ratings yet
- Respiratory System (Anatomy and Physiology)Document71 pagesRespiratory System (Anatomy and Physiology)Butch Dumdum100% (11)
- Physiotherapy in Respiratory Care 3rd Ed - A. Hough (Nelson Thornes, 2001) WW PDFDocument562 pagesPhysiotherapy in Respiratory Care 3rd Ed - A. Hough (Nelson Thornes, 2001) WW PDFDaria Nectaria100% (1)
- Shen Gong Exercises PDFDocument3 pagesShen Gong Exercises PDFRahimNo ratings yet
- The Human Respiratory SystemDocument15 pagesThe Human Respiratory SystemNandita Halder100% (1)
- MCQ Exam 2011 PDFDocument22 pagesMCQ Exam 2011 PDFBranka Kurtovic80% (10)
- Anatomy of Respiratory SystemDocument57 pagesAnatomy of Respiratory SystemRyan Larsen100% (1)
- OxygenationDocument20 pagesOxygenationKhie-An OcampoNo ratings yet
- HaraShiatsu Self HealingDocument3 pagesHaraShiatsu Self HealingAWEDIOHEADNo ratings yet
- Anaesthesia Breathing CircuitsDocument8 pagesAnaesthesia Breathing CircuitsSuresh KumarNo ratings yet
- Respiratory System Anatomy, Assessment & Diagnostic TestsDocument24 pagesRespiratory System Anatomy, Assessment & Diagnostic TestsPrince Rener Velasco PeraNo ratings yet
- Respiratory SystemDocument32 pagesRespiratory Systemapi-202513022No ratings yet
- NursingBulletin Respiratory SystemDocument35 pagesNursingBulletin Respiratory Systemseigelystic100% (3)
- Pear Cone WaveDocument2 pagesPear Cone WaveMichael Grant White100% (2)
- The Respiratory SystemDocument147 pagesThe Respiratory SystemAya SobhiNo ratings yet
- Alexander Breathing Pain ReliefDocument2 pagesAlexander Breathing Pain ReliefSyedNo ratings yet
- Anatomy and Physiology: The Respiratory SystemDocument82 pagesAnatomy and Physiology: The Respiratory SystemMaria Angelique Ofciar100% (2)
- Anatomy of Respiratory System: Dr. Dwi Rita Anggraini, MkesDocument64 pagesAnatomy of Respiratory System: Dr. Dwi Rita Anggraini, MkesFira TasyaNo ratings yet
- Anatomy and Physiology of The Respiratory SystemDocument5 pagesAnatomy and Physiology of The Respiratory SystemxoxosvwNo ratings yet
- Respiratory Physiology AnswersDocument4 pagesRespiratory Physiology AnswersRamya100% (3)
- Group1 Review of Respiratory SystemDocument41 pagesGroup1 Review of Respiratory Systemjohn obinaNo ratings yet
- Respiratory System s2 2019Document56 pagesRespiratory System s2 2019noviantyramadhani12No ratings yet
- 22 Respiratory SystemDocument99 pages22 Respiratory SystemvanderphysNo ratings yet
- The Respiratory System: ASTIKA NUR ROHMAH, S.Kep., NS., M.BiomedDocument43 pagesThe Respiratory System: ASTIKA NUR ROHMAH, S.Kep., NS., M.BiomedAdek KhazeliaNo ratings yet
- Respiratory NotesDocument6 pagesRespiratory NotesBethany CrawfordNo ratings yet
- Respiratory SystemDocument53 pagesRespiratory SystemRotan CirebonNo ratings yet
- Physiology of The Respiratory System-1Document155 pagesPhysiology of The Respiratory System-1Adil MusaddiqNo ratings yet
- Self Test 3Document6 pagesSelf Test 3202310446No ratings yet
- Week 3 Respiratory SystemDocument10 pagesWeek 3 Respiratory SystemangeliaNo ratings yet
- 1.anatomy of Respiratory SystemDocument73 pages1.anatomy of Respiratory Systemokoti.omutanyi22No ratings yet
- Lecture 5 Respiratory System 1Document61 pagesLecture 5 Respiratory System 1hafiz patahNo ratings yet
- Anatomi Sistem ParuDocument64 pagesAnatomi Sistem ParuMochammad Fariz AmsalNo ratings yet
- Respiratory SystemDocument12 pagesRespiratory Systemab4943409No ratings yet
- Anatomy, Physiology and Pathology of The RespiratoryDocument68 pagesAnatomy, Physiology and Pathology of The Respiratorytheresia_s_k100% (1)
- Anatomy of The Respiratory SystemDocument37 pagesAnatomy of The Respiratory SystemPal SedNo ratings yet
- Respiratory System Anatomy and Physiology: Marianne Belleza, RNDocument18 pagesRespiratory System Anatomy and Physiology: Marianne Belleza, RNTiara GustiwiyanaNo ratings yet
- Respiratory SystemDocument9 pagesRespiratory SystemShivani Sriram100% (1)
- RESPIRATORY DISTURBANCES - HandoutsDocument35 pagesRESPIRATORY DISTURBANCES - Handoutsfebie pachecoNo ratings yet
- NCM 112 LEC Topic 1 Respiratory System Anatomy PhysiologyDocument7 pagesNCM 112 LEC Topic 1 Respiratory System Anatomy PhysiologyViviene Faye FombuenaNo ratings yet
- Respiratory Tract Structure: Alveolus)Document5 pagesRespiratory Tract Structure: Alveolus)MarekGojtowskiNo ratings yet
- UntitledDocument62 pagesUntitledManaye MamuyeNo ratings yet
- Lecture - 5 PDFDocument5 pagesLecture - 5 PDFDavid JokerNo ratings yet
- ANAPHYDocument10 pagesANAPHYcharles babasaNo ratings yet
- Respiratory SystemDocument5 pagesRespiratory SystemPreeti ChouhanNo ratings yet
- Module 4 Respiratory SystemDocument8 pagesModule 4 Respiratory SystemJake Donely C. PaduaNo ratings yet
- Anatomy 2nd-U-3 Respiratory SystemDocument113 pagesAnatomy 2nd-U-3 Respiratory Systemsinte beyuNo ratings yet
- 1-Respiratory MechanicsDocument56 pages1-Respiratory MechanicsDoha JKNo ratings yet
- Respiratory System PDFDocument16 pagesRespiratory System PDFMary Ann SacramentoNo ratings yet
- The Respiratory System PP First - Stage 2021Document27 pagesThe Respiratory System PP First - Stage 2021HHHNo ratings yet
- Respiratory SystemDocument5 pagesRespiratory SystemКрістіна БаландаNo ratings yet
- Respiratory System - Anatomy and PhysiologyDocument6 pagesRespiratory System - Anatomy and PhysiologyJay Crishnan Morales CajandingNo ratings yet
- Functional Anatomy of The Respiratory System NoseDocument5 pagesFunctional Anatomy of The Respiratory System NoseEjie Boy IsagaNo ratings yet
- Respiratory System: Sakina Dept. Anatomi Dan Histologi FK UnairDocument52 pagesRespiratory System: Sakina Dept. Anatomi Dan Histologi FK UnairFhyrha MyuceNo ratings yet
- ScienceDocument14 pagesSciencesheanellerenzsantosNo ratings yet
- Respiratory SystemDocument5 pagesRespiratory SystemrianaNo ratings yet
- Lec:2 Respiratory System DR - HudaDocument4 pagesLec:2 Respiratory System DR - HudaLina AyadNo ratings yet
- Respiratory System 1 Physiology 16-11-2018Document25 pagesRespiratory System 1 Physiology 16-11-2018Kangwa MasekaNo ratings yet
- Anatomy and Physiology of Respiratory SystemDocument4 pagesAnatomy and Physiology of Respiratory Systembilliam123No ratings yet
- Human Biology: Respiratory SystemDocument33 pagesHuman Biology: Respiratory SystemSaikrishna RaoNo ratings yet
- Anatomy & PhysiologyDocument42 pagesAnatomy & PhysiologyArah Lyn ApiagNo ratings yet
- Anatomy of The Larynx: Thyrohyoid MembraneDocument35 pagesAnatomy of The Larynx: Thyrohyoid MembraneVarsha Shende KhobragadeNo ratings yet
- Respiratory & Urinary System 1Document3 pagesRespiratory & Urinary System 1Ishmael DimagibaNo ratings yet
- PAin and Oxygenation HandoutsPRELIMSDocument7 pagesPAin and Oxygenation HandoutsPRELIMSJhoanna de ChavezNo ratings yet
- Functions of The Respiratory SystemDocument10 pagesFunctions of The Respiratory SystemKrisha AvorqueNo ratings yet
- Functional Human Physiology: The Respiratory SystemDocument64 pagesFunctional Human Physiology: The Respiratory SystemnashqonashNo ratings yet
- Respiratory System Semi FinalDocument60 pagesRespiratory System Semi FinalMichelle AnteneroNo ratings yet
- How Do Humans Breathe? Science Book Age 8 | Children's Biology BooksFrom EverandHow Do Humans Breathe? Science Book Age 8 | Children's Biology BooksNo ratings yet
- Apa Itu MengikDocument2 pagesApa Itu MengikAmy Tryabto ArifinNo ratings yet
- Dental Human PhysiologyDocument148 pagesDental Human Physiologypawi18No ratings yet
- 10th Biology Guess 2019Document5 pages10th Biology Guess 2019muhammad zulqarnainNo ratings yet
- CSEC Biology January 2007 042Document8 pagesCSEC Biology January 2007 042Makayla AlexanderNo ratings yet
- Ewquickguide 2 EdDocument188 pagesEwquickguide 2 EdStanley Wu TaiNo ratings yet
- Definisi Dan Terapi - Id.enDocument11 pagesDefinisi Dan Terapi - Id.enCindy Ari SantiNo ratings yet
- 10bja Medsci - Mckenzie CheyneDocument60 pages10bja Medsci - Mckenzie Cheyneapi-284323075No ratings yet
- KA THA RA HEALING STEP ONE - Awakening The MENTOR & 6th & 7th SensesDocument5 pagesKA THA RA HEALING STEP ONE - Awakening The MENTOR & 6th & 7th SensesfarahNo ratings yet
- Patient-Ventilator Dyssynchrony in The Intensive Care Unit A PracticalDocument12 pagesPatient-Ventilator Dyssynchrony in The Intensive Care Unit A PracticalBrenda Serrano LaraNo ratings yet
- RespirationDocument6 pagesRespirationAbu BeastNo ratings yet
- Marieb 2015 11th 0321919009 SampleDocument31 pagesMarieb 2015 11th 0321919009 SampleJoe Chill100% (1)
- Ebook Pulmonary Physiology Tenth Edition PDF Full Chapter PDFDocument67 pagesEbook Pulmonary Physiology Tenth Edition PDF Full Chapter PDFbobby.bianco575100% (25)
- Box Breathing PDFDocument8 pagesBox Breathing PDFScribd AnonNo ratings yet
- Alteration in Respiratory SystemDocument138 pagesAlteration in Respiratory Systemcute_gurljhoanNo ratings yet
- GR-5 ScienceDocument354 pagesGR-5 SciencePrecious RubaNo ratings yet
- BBBBBBNNNDocument6 pagesBBBBBBNNNIrfana EfendiNo ratings yet
- Medtronic PB560 - 10039030M00 - PB560 SYSTEM FINAL TEST PROCEDUREDocument12 pagesMedtronic PB560 - 10039030M00 - PB560 SYSTEM FINAL TEST PROCEDUREDaniel MarquesNo ratings yet
- Forced Smoking Stories I'Ve CollectedDocument241 pagesForced Smoking Stories I'Ve CollectedErnesto PazNo ratings yet