Professional Documents
Culture Documents
Patient Awareness Hospital Acquired Infection
Uploaded by
Mervin SulistyoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Patient Awareness Hospital Acquired Infection
Uploaded by
Mervin SulistyoCopyright:
Available Formats
Ann R Coll Surg Engl 2003; 85: 123125
Medical audit
Patient perceptions of MRSA
Sally MA Hamour, Austin OBichere, John L Peters, Peter J McDonald
Department of Surgery, Northwick Park Hospital, Harrow, Middlesex, UK
Drug-resistant nosocomial infections are an increasing problem. This issue has received considerable media coverage. To our knowledge there have been no studies investigating patient awareness and perceptions of nosocomial infections. A total of 113 surgical out-patients completed a questionnaire stating whether they had heard of either superbugs or MRSA. A series of questions were asked about the source of any information; methods of transmission and prevention; the consequences of infection and their emotional response if they were to acquire MRSA. Fifty patients (44%) had heard of superbugs or MRSA mainly via the media (58%) or from hospital staff (44%). The majority would feel either angry or afraid if they acquired MRSA in hospital, but there was good awareness of both methods of infection control and the consequences of infection. From our study, we conclude that the media is at least as important as health professionals in providing information. Concerns regarding nosocomial infection may need to be addressed prior to admission. Key words: Methicillin resistance Drug resistance, bacterial Hospital infections Infection control
n the 3 months prior to the study, 103 new cases of MRSA were recorded in our hospital. This study aimed to determine the proportion of patients who were aware of this issue and their understanding of its implications and possible means of prevention. The World Health Organizations report on infectious diseases warned that the level of resistance to drugs used to treat common infectious diseases is reaching crisis point.1 At any one time, more than 1 in 10 acute hospital patients has a hospital-acquired infection.2 Resistant and multiresistant organisms are particularly important as a cause of nosocomial infection,3 and are often difficult and expensive to treat, particularly methicillin-resistant Staphylococcus aureus (MRSA).4 This has been the subject of considerable comment and debate in the popular press. A search of the British Newspaper Index January 1998 to December 1999 using the search terms MRSA, superbug,
hospital-acquired infection and antibiotic resistance revealed 28 articles of which 25 used the term superbug. Much of this coverage has been of a sensationalist nature (Table 1). In contrast, a Medline search 1966 to May 2000 using the search terms MRSA, surgery, superbug, public awareness, antibiotic resistance and drug resistance revealed no studies investigating public awareness of the problems of antibiotic resistance in hospitals. Patients and Methods Between April and June 2000, 116 surgical out-patients attending for pre-admission clinics or flexible cystoscopy completed a questionnaire enquiring whether they had heard of either superbugs or MRSA in hospitals. Those who responded positively went on to answer a series of
Correspondence to: Dr S Hamour MRCP, c/o Liverpool School of Tropical Medicine, Pembroke Place, Liverpool L3 5QA, UK E-mail: sallyhamour@hotmail.com
Ann R Coll Surg Engl 2003; 85
123
HAMOUR
PATIENT PERCEPTIONS OF MRSA
Table 1 Newspaper headlines associated with superbugs Superbug Wars Antibiotic fails to save US Superbug Patient Marching on, Superbug that knows no fear Doctors Losing Superbug Battle Superbug defies Antibiotics Superbug Attacks 17 Superbug is on rampage in hospitals says expert Hospitals on Alert over Superbug that defies Drugs Drug-Resistant Superbug Kills 4 March of the Superbug The Financial Times, 4 September 1998, p 17 The Daily Telegraph, 18 February 1999, p 15 The Daily Mail, 3 August 1998, p 29 The Times, 24 June 1998, p 5 The Times, 23 April 1998, p 1 The Daily Telegraph, 1 August 1998, p 8 The Mail on Sunday, 29 August 1999, p 37 The Daily Mail, 7 September 1999, p 19 The Independent on Sunday, 29 August 1999, p 1 The Daily Mail, 18 June 1999, p 29
questions regarding their source of information; their understanding of preventative measures and the consequences of infection. In addition, their emotional responses to the possibility of MRSA infection in hospital were sought. After completing the questionnaire, patients were offered an information sheet about MRSA. Results A total of 113 patients with a median age of 67 years (range, 2189 years) participated in this study of whom 97 (86%) were male. Fifty patients (44%) had heard of either superbugs or MRSA. Of these, 14 (28%) had acquired information from hospital staff, 21 (42%) from the media and 8 (16%) had heard of it from both sources. Eleven (22%) had acquired information from friends and family as either the sole source of information or in addition to other sources and one patient had heard about it from another patient. Thirty-four patients (68%) correctly identified MRSA or superbug as a multiresistant bacterium and 35 (70%) believed that it could be acquired from the hospital environment. Seventeen (34%) thought that it could be contracted from operations or other procedures and 4 (8%) from hospital staff. Nine patients (18%) were unsure how it could be acquired but 22 (44%) knew that antibiotic-resistant organisms existed in the community as well as in hospitals. Patients reaction to the possibility of acquiring MRSA revealed that 26 (52%) would feel afraid and 19 (38%) would feel angry. Only five (10%) patients would not be concerned and none would feel ashamed. The reasons for feeling angry or afraid were interesting and varied (Table 2). In assessing the perceived effectiveness of infection control measures, 27 (54%) thought hand washing was important. A similar number of patients, 22 (44%) and 21 (42%) believed gloves/aprons and isolation rooms, respectively, helped to prevent transmission. A single patient (2%) thought there was no known method of controlling spread while 12 (24%) were unsure. 124
Table 2 Some responses to the possibility of acquiring MRSA There is no known way to treat it I would hope that a hospital ward would protect me I would be afraid of spreading it to others I would not be responsible for getting it It can kill you It cannot be treated I think it could be prevented I wouldnt expect to acquire MRSA after a routine operation Lack of hygiene
A large number of patients felt the possible consequences of MRSA infection to be significant with 23 (46%) identifying wound infection, 19 (38%) major illness and 11 (22%) delayed discharge as potential problems. Only 4 (8%) thought there were no consequences of infection. Discussion Despite considerable and often sensationalist media coverage, less than half of patients (44%) had prior knowledge of superbugs or MRSA. Of these, the media was, perhaps unsurprisingly, the most frequent source of information. However, it is re-assuring, although not entirely satisfactory, that 44% had gained information from hospital staff. The number of patients gaining information from within the hospital may be high in our sample because many were regular attenders for flexible cystoscopy. In spite of the nature of the media coverage often devoted to antibiotic resistance and hospital-acquired infection, patients were generally well informed about methods of transmission and consequences of infection. However, it was clear that the possibility of infection generated a wide range of strong emotions. Patients in general felt that their health could be threatened and that hospitals failed to protect them adequately. Some were even angry that it implied a lack of hygiene in hospitals. Greater access to accurate information and open channels
Ann R Coll Surg Engl 2003; 85
PATIENT PERCEPTIONS OF MRSA
HAMOUR
of communication between patients and hospital staff are required in order to address these issues. Conclusions Better surveillance, early diagnosis and education of patients and hospital staff are all required to prevent transmission of MRSA.5 Perhaps the most important finding from this study is the high level of anxiety that MRSA infection would provoke amongst patients. These emotions need to be recognized so that patient concerns about nosocomial infection can be addressed in future health initiatives.
References
1. World Health Organization. WHO Report on Infectious Diseases 2000. Overcoming Antimicrobial Resistance. Geneva: WHO, 2000 <www.who.int>. 2. Plowman R, Graves N, Griffin M, Roberts JA, Swan A, Cookson R et al. The Socio-economic Burden of Hospital Acquired Infection. London: PHLS, 2000 <www.doh.gov.uk/haicosts.htm>. 3. Tackling antimicrobial resistance. Drug Ther Bull 1999; 37: 915. 4. Carbon C. Costs of treating infections caused by methicillin-resistant staphylococci and vancomycin resistant enterococci. J Antimicrob Chemother 1999; 44: 316. 5. Humphreys H, Duckworth G. Methicillin-resistant Staphylococcus aureus (MRSA) a re-appraisal of control measures in the light of changing circumstances. J Hosp Infect 1997; 36: 16770.
Ann R Coll Surg Engl 2003; 85
125
You might also like
- 1 - Name of The Candidate and AddressDocument19 pages1 - Name of The Candidate and AddressRini ThomasNo ratings yet
- Risk Factor For MRSA in Skin, Soft Tissue and Bone Infection in The Foot and Leg in California Community HospitalDocument11 pagesRisk Factor For MRSA in Skin, Soft Tissue and Bone Infection in The Foot and Leg in California Community HospitalReza Suryapandu NugrohoNo ratings yet
- 1-7 ThesisDocument62 pages1-7 ThesisShobhit GoswamiNo ratings yet
- 98668Document6 pages98668SyedFaridAliNo ratings yet
- Epidemiology Roun1Document10 pagesEpidemiology Roun1FebniNo ratings yet
- Effectiveness of Contact Isolation During A Hospital Outbreak of Methicillin-Resistant Staphylococcus AureusDocument9 pagesEffectiveness of Contact Isolation During A Hospital Outbreak of Methicillin-Resistant Staphylococcus Aureusmoniart2587No ratings yet
- Chapter One 1.0 Background of The StudyDocument6 pagesChapter One 1.0 Background of The StudyKojo AduNo ratings yet
- Methicillin-Resistant Staphylococcus Tuberculosis: Part 1: Aureus and Multidrug ResistantDocument3 pagesMethicillin-Resistant Staphylococcus Tuberculosis: Part 1: Aureus and Multidrug ResistantSukma EffendyNo ratings yet
- Fauci and Marston - NEJM 2015Document3 pagesFauci and Marston - NEJM 2015Fernanda PachecoNo ratings yet
- Medicine American Journal of Hospice and PalliativeDocument6 pagesMedicine American Journal of Hospice and Palliativem1k0eNo ratings yet
- Infection Control in The ICU EnvironmentDocument273 pagesInfection Control in The ICU EnvironmentJOSEPH APPIAHNo ratings yet
- DR - GulsivDocument5 pagesDR - GulsivPravin SurendranNo ratings yet
- Epidemiology RoundDocument13 pagesEpidemiology RoundFebniNo ratings yet
- BUGS TO SUPER BUGS Emerging Challenges in Health CareDocument2 pagesBUGS TO SUPER BUGS Emerging Challenges in Health Caretummalapalli venkateswara raoNo ratings yet
- 2009guzman BlancoDocument5 pages2009guzman BlancoLuís Flávio Cozza VazNo ratings yet
- Lancet - Septic Shock (Seminars)Document16 pagesLancet - Septic Shock (Seminars)williamsbarriosNo ratings yet
- MRSA-Why and How MRSA Moved Into CommunityDocument14 pagesMRSA-Why and How MRSA Moved Into CommunityDr Kadiyali M SrivatsaNo ratings yet
- 1 s2.0 S1198743X16303639 Main PDFDocument7 pages1 s2.0 S1198743X16303639 Main PDFMuhammad Addinul HudaNo ratings yet
- Pediatrics 2013 Iwamoto E817 24Document10 pagesPediatrics 2013 Iwamoto E817 24phobicmdNo ratings yet
- Hospital-Acquired Pneumonia: Pathophysiology, Diagnosis, and TreatmentDocument23 pagesHospital-Acquired Pneumonia: Pathophysiology, Diagnosis, and Treatmentdarmarianto100% (1)
- Problem Statement Chapter-1&2Document33 pagesProblem Statement Chapter-1&2Anonymous 22GBLsme171% (7)
- 5.4 Risk Factors For MRSA ColonizationDocument8 pages5.4 Risk Factors For MRSA ColonizationQworldNo ratings yet
- Mrsa Research Paper TopicsDocument8 pagesMrsa Research Paper Topicsfvdddmxt100% (1)
- Healthcare Practitioner Awareness of Hospital InfectionsDocument4 pagesHealthcare Practitioner Awareness of Hospital InfectionslulukzNo ratings yet
- 05 N312 18329Document9 pages05 N312 18329GinshaNo ratings yet
- Mrsa101 508Document45 pagesMrsa101 508Sam TullyNo ratings yet
- Case 2. Severe Infection Due To Bacterial Water ContaminationDocument7 pagesCase 2. Severe Infection Due To Bacterial Water Contaminationumaya220% (1)
- Risk Factores For An Outbreak of Multi-Drug-Resistant Acinetobacter - Chest-1999-Husni-1378-82Document7 pagesRisk Factores For An Outbreak of Multi-Drug-Resistant Acinetobacter - Chest-1999-Husni-1378-82Che CruzNo ratings yet
- Running Head: Prevention of Mrsa Infection 1Document10 pagesRunning Head: Prevention of Mrsa Infection 1api-354021178No ratings yet
- Communicable Disease PaperDocument4 pagesCommunicable Disease PaperCorrine BlucherNo ratings yet
- Infections in The Neutropenic Patient-2001Document27 pagesInfections in The Neutropenic Patient-2001Raisa_90No ratings yet
- Parotiditis Viral Art 2Document7 pagesParotiditis Viral Art 2Monse CárdenasNo ratings yet
- Vaccines: Making the Right Choice for Your ChildFrom EverandVaccines: Making the Right Choice for Your ChildRating: 5 out of 5 stars5/5 (2)
- حنينDocument12 pagesحنينHanen sayar AlmarshedyةNo ratings yet
- Sas Hes032 8Document8 pagesSas Hes032 8Jose Melmar Autida AutenticoNo ratings yet
- Research Paper On MrsaDocument4 pagesResearch Paper On Mrsam0d1p1fuwub2100% (1)
- LitEffectiveness of Hand Hygiene Practices in Prevention of Methicillin Resistant Staphylococcusaureusinfection Acquisition in Hospitalized PatientsDocument3 pagesLitEffectiveness of Hand Hygiene Practices in Prevention of Methicillin Resistant Staphylococcusaureusinfection Acquisition in Hospitalized PatientsdreamdreamgarlNo ratings yet
- Judicious Use of Antibiotics: A Guide For Oregon CliniciansDocument32 pagesJudicious Use of Antibiotics: A Guide For Oregon CliniciansRiyan SaputraNo ratings yet
- Epidemiology Surveillance of Fungal InfectionsDocument10 pagesEpidemiology Surveillance of Fungal Infectionsabznaim420No ratings yet
- Society's failure to protect antibioticsDocument3 pagesSociety's failure to protect antibioticsgabyvaleNo ratings yet
- Measles Outbreak NejmoaDocument12 pagesMeasles Outbreak NejmoaVlad ManoleNo ratings yet
- Antibiotic Prescribing and Resistance:: Views From Low-And Middle-Income Prescribing and Dispensing ProfessionalsDocument42 pagesAntibiotic Prescribing and Resistance:: Views From Low-And Middle-Income Prescribing and Dispensing ProfessionalsFaozan FikriNo ratings yet
- Lancet 2023Document17 pagesLancet 2023Julia Urquiza LandaluceNo ratings yet
- Emerging Infections Outbreak ReportingDocument42 pagesEmerging Infections Outbreak ReportingJean SurigaoNo ratings yet
- Yiu Et Al 2016 Risk of Serious Infections in Patients With Psoriasis On Biologic Therapis Metas-AnalysisDocument8 pagesYiu Et Al 2016 Risk of Serious Infections in Patients With Psoriasis On Biologic Therapis Metas-AnalysisMarcel JinihNo ratings yet
- Nucci 2013Document7 pagesNucci 2013Good OneNo ratings yet
- Drug Interactions in Infectious Diseases: Mechanisms and Models of Drug InteractionsFrom EverandDrug Interactions in Infectious Diseases: Mechanisms and Models of Drug InteractionsManjunath P. PaiNo ratings yet
- Advanced Therapeutics - 2020 - BaranyaiDocument22 pagesAdvanced Therapeutics - 2020 - BaranyaiADVOCATE ASHUTOSH SHARMANo ratings yet
- Classification of Drug-Resistant Tuberculosis in An Epidemic AreaDocument4 pagesClassification of Drug-Resistant Tuberculosis in An Epidemic AreaTika Dwi TamaNo ratings yet
- Recommendations and Reports OI - HIVDocument323 pagesRecommendations and Reports OI - HIVJevie KairupanNo ratings yet
- Articulo Evaluacion Final Antimicrobianos 1 2020Document9 pagesArticulo Evaluacion Final Antimicrobianos 1 2020Juan BojacaNo ratings yet
- 2022 Book InfectionPreventionDocument398 pages2022 Book InfectionPreventionAnna Murni Nasution100% (2)
- Acinetobacter BaumanniiDocument12 pagesAcinetobacter BaumanniiKenneth Smith IINo ratings yet
- Finalroughmed 2Document14 pagesFinalroughmed 2api-667132918No ratings yet
- WHO Antimicrobial ResistanceDocument4 pagesWHO Antimicrobial ResistanceDesalegnNo ratings yet
- A Measles Outbreak in An Underimmunized Amish Community in OhioDocument12 pagesA Measles Outbreak in An Underimmunized Amish Community in Ohiomuhammad maadaNo ratings yet
- Infection Is Acommonproblem ForDocument11 pagesInfection Is Acommonproblem ForDitaMayasariNo ratings yet
- Icu Journal. FinalDocument6 pagesIcu Journal. FinalJoehoney BarreraNo ratings yet
- Parasitic Infections and the Immune SystemFrom EverandParasitic Infections and the Immune SystemFelipe KierzenbaumNo ratings yet
- How Does The Coronavirus Test Work? 5 Questions AnsweredDocument10 pagesHow Does The Coronavirus Test Work? 5 Questions AnsweredAdalberto Caldeira Brant FilhoNo ratings yet
- Malaria in Children: Department of Paediatrics and Child Health, Mbarara UniversityDocument13 pagesMalaria in Children: Department of Paediatrics and Child Health, Mbarara UniversityMwanja MosesNo ratings yet
- Report On Global Sexually Transmitted Infection SurveillanceDocument74 pagesReport On Global Sexually Transmitted Infection SurveillanceSafaNo ratings yet
- ASHA Physical & Financial Reporting FormatDocument23 pagesASHA Physical & Financial Reporting FormatBijuMadambil50% (2)
- Inverting The Pyramid - Enhancing Systems For Protecting Children PDFDocument294 pagesInverting The Pyramid - Enhancing Systems For Protecting Children PDFadorandraNo ratings yet
- Different Types of VaccinesDocument4 pagesDifferent Types of VaccinesTenisha KnowlesNo ratings yet
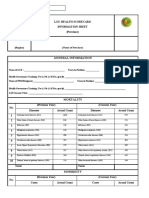
- LGU health scorecard info sheetDocument2 pagesLGU health scorecard info sheetToni Quitalig GamezNo ratings yet
- Iligan Medical Center College College of Nursing and Midwifery Mid 104 (Final Long Quiz)Document1 pageIligan Medical Center College College of Nursing and Midwifery Mid 104 (Final Long Quiz)Rohanisah AdapNo ratings yet
- DOH Manual of Operations-PhilPENDocument60 pagesDOH Manual of Operations-PhilPENKarlo Quezon100% (2)
- Improving School ToiletsDocument5 pagesImproving School Toiletszin GuevarraNo ratings yet
- COVID-19 Pandemic in IndonesiaDocument27 pagesCOVID-19 Pandemic in IndonesiaYugendra RNo ratings yet
- Edit1 - Laporan Aksi Cegah Stunting Dr. Damayanti-1 PDFDocument53 pagesEdit1 - Laporan Aksi Cegah Stunting Dr. Damayanti-1 PDFkeslingkesker situbondoNo ratings yet
- Causative Agents: Leon) (Flaviviruses) (Common in The Phil.) P. OvaleDocument12 pagesCausative Agents: Leon) (Flaviviruses) (Common in The Phil.) P. OvaleJUANJOSEFOXNo ratings yet
- Ovarian Insufficiency: Causes, Symptoms, and TreatmentDocument4 pagesOvarian Insufficiency: Causes, Symptoms, and Treatmentagility dreamsNo ratings yet
- The Real Anthony Fauci PDFDocument14 pagesThe Real Anthony Fauci PDFRocco Lampone100% (1)
- Earth Science: Air Pollution in Tomas CabiliDocument6 pagesEarth Science: Air Pollution in Tomas CabiliAshy LeeNo ratings yet
- Susunan AcaraDocument2 pagesSusunan Acaraniko4eyesNo ratings yet
- Poliomyelitis: Poliomyelitis /poʊlioʊmaɪəlaɪtɪs/, Often Called Polio or Infantile Paralysis, Is An Acute, ViralDocument2 pagesPoliomyelitis: Poliomyelitis /poʊlioʊmaɪəlaɪtɪs/, Often Called Polio or Infantile Paralysis, Is An Acute, Viralbala1307No ratings yet
- Global Handwashing Day 2020: Hagbay Elementary SchoolDocument9 pagesGlobal Handwashing Day 2020: Hagbay Elementary SchoolShalee Carpio BalanquitNo ratings yet
- Definition:: Pertussis (Whooping Cough)Document9 pagesDefinition:: Pertussis (Whooping Cough)Zhyzhy CordovaNo ratings yet
- Free Annual Medical ReportDocument2 pagesFree Annual Medical ReportPravin Nikhade0% (1)
- Health For Life Kenya by Cecilia JakobssonDocument4 pagesHealth For Life Kenya by Cecilia Jakobssonnina_senNo ratings yet
- SC CHN Imci Post Test 50items Mr. JV GasminDocument4 pagesSC CHN Imci Post Test 50items Mr. JV Gasmincianm1143No ratings yet
- Coronavirus Disease (COVID-19) : Case Investigation FormDocument2 pagesCoronavirus Disease (COVID-19) : Case Investigation FormcharleneNo ratings yet
- Pap SmearsDocument28 pagesPap Smearskhadzx100% (2)
- Prenatal Genetic CounselingDocument2 pagesPrenatal Genetic CounselingJanani ParameswaranNo ratings yet
- Health Services Officers Best Kept SecretsDocument5 pagesHealth Services Officers Best Kept SecretsUSPHSNo ratings yet
- COVID-19 Preparedness and Response Plan Template - Updated 6.8.20 - 202006081252049904Document8 pagesCOVID-19 Preparedness and Response Plan Template - Updated 6.8.20 - 202006081252049904Sujit ShahNo ratings yet
- Toguz CV Fall 2019Document6 pagesToguz CV Fall 2019api-270694484No ratings yet
- SRF ID 2746600629803 COVID-19 Test ReportDocument1 pageSRF ID 2746600629803 COVID-19 Test ReportShivshankar HondeNo ratings yet
- Global Initiative For Asthma (2021) Guidelines: Peter Miranda 3 Year IM ResidentDocument32 pagesGlobal Initiative For Asthma (2021) Guidelines: Peter Miranda 3 Year IM ResidentPeter MirandaNo ratings yet