Professional Documents
Culture Documents
Medical Emergencies in Dental Practice: 1. The Drug Box, Equipment and General Approach
Uploaded by
Rodelix San Juan DacanayOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medical Emergencies in Dental Practice: 1. The Drug Box, Equipment and General Approach
Uploaded by
Rodelix San Juan DacanayCopyright:
Available Formats
MedicalEmergencies
This article counts towards one of the five core subjects introduced in 2007 by the GDC.
Mark Greenwood
Medical Emergencies in Dental Practice: 1. The Drug Box, Equipment and General Approach
Abstract: Every dental practitioner needs a knowledge of the diagnosis and management of medical emergencies. This first paper, in a series of two, deals with the general aspects of emergency treatment, including basic principles applicable to all emergencies and a consideration of the management of cardiac arrest. The second paper deals with more specific aspects of medical emergency management. Clinical Relevance: All dental practitioners require a knowledge of medical emergency management. Dent Update 2009; 36: 202211
Medical emergencies in dental practice are uncommon but could occur at any time. It is important, however, that dental practitioners are proficient in recognizing them and carrying out initial management of such emergencies. The commonest emergencies seen include the following: Faints; Hypoglycaemia; Asthma attacks; Anaphylaxis; Angina; and Seizures. Examples of such events have been reported to occur on average once every 34 years per dentist.1 All members of the dental team need to be aware of what their role would be in the event of a medical emergency and should be trained appropriately with regular practise sessions. Successful patient management
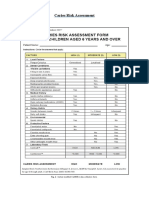
Drug Oxygen Glyceryl trinitrate (GTN) spray (400 micrograms per actuation) Dispersible aspirin (300 mg) Salbutamol aerosol inhaler (100 micrograms per actuation) Adrenaline injection (1:1000, 1 mg/ml) Glucagon injection (1 mg) Oral glucose solution/gel (GlucoGel)* Midazolam 10 mg or 5 mg/ml (buccal or intranasal)
Route of Administration Inhalation Sublingual
Oral (chewed) Inhalation
Intramuscular Intramuscular/subcutaneous Oral Infiltration/inhalation
Mark Greenwood, PhD, MDS, FDS, FRCS, FRCS(OMFS), FHEA, Consultant, Honorary Clinical Professor, Oral and Maxillofacial Surgery, School of Dental Sciences, Newcastle University, Framlington Place, Newcastle upon Tyne NE2 4BW, UK.
*Alternatives: 2 teaspoons of sugar/3 sugar lumps 200 ml milk Non-diet Lucozade 50 ml Coca-cola non-diet 90 ml If necessary this can be repeated at 10-15 minute intervals.
Table 1. Contents of the emergency drug box and routes of administration.
begins with anticipation of the more likely potential medical emergencies that
could arise by taking a thorough medical history. If a medical condition is identified May 2009
202 DentalUpdate
MedicalEmergencies
Portable oxygen cylinder (D size) with a flowmeter and pressure reduction valve Oxygen face mask with tubing Oropharyngeal airways sizes 1, 2, 3 and 4 (Figure 2) Pocket mask with port for oxygen Figure 3 Bag and mask apparatus (1 litre bag capacity) with oxygen reservoir Well-fitting face masks Portable suction Single-use sterile syringes and needles Spacer device for inhaled bronchodilators Blood glucose measurement device Automated External Defibrillator (AED) Figure 5
Figure 1. A Glucagon kit with water for dilution already drawn up and powder for reconstitution. Kits such as these can save valuable time in managing emergencies, in this case hypoglycaemia. Table 2. Suggested minimum equipment for medical emergency management (adapted from Resuscitation Council (UK)).
Figure 2. An oropharyngeal airway.
and medication is normally taken, a check should always be made to ensure that the medication has been taken as usual. The management of specific medical emergencies is considered in the second paper. This paper considers more general aspects with regard to management, together with the management of cardiac arrest.
Kingdom.2 Wherever possible, drugs in solution should be carried in a pre-filled syringe or kit (Figure 1). All drugs should be stored together, ideally in a purposedesigned container. The optimum route for delivery of emergency drugs is usually the intravenous route but dentists are often inexperienced with this route of delivery. Formulations have now been developed that allow for other routes to be used which are much quicker and user-friendly and the intravenous route for emergency drugs is no longer recommended for dental practitioners. Oxygen should always be available, deliverable at adequate flow rates (10 litres per minute).
equipment listed in Table 2 will be discussed in the second paper. It is a public expectation that Automated External Defibrillators (AEDs) should be available in the healthcare environment and dentistry is not considered an exception.2 All emergency medical equipment should be latex-free and single use wherever possible.
Staff training
Staff should be trained in the management of medical emergencies to a degree which is appropriate to their level of clinical responsibility. Skills should be updated on an annual basis. It is important that new members of staff have medical emergency training incorporated into their induction programme. A full record should be kept of training. Staff should know who to contact in the event of help being required and designated emergency phone numbers (usually 999) should be readily available.
Equipment for use in medical emergencies
The Resuscitation Council (UK) have recommended as a minimum the equipment shown in Table 2.2 Named individuals should be nominated to check equipment. This should be carried out at least weekly and the process should be audited. The use of the items of
Contents of the emergency drug box
Medical emergencies may require equipment, drugs or both in order to manage them effectively. If these are unavailable, patients should not be treated. It is also important to check that the drugs are within their expiry date. Drugs to be included in the emergency drug box are summarized in Table 1. The list is based on that given in the Resuscitation Council (UK) document on Medical Emergencies and Resuscitation in Dentistry.2 The Resuscitation Council (UK) recommends that such kits should be standardized throughout the United May 2009
The ABCDE approach to an emergency patient
Medical emergencies can
A B C D E
Airway Breathing Circulation Disability (or neurological status) Exposure (in dental practice, to facilitate placement of AED paddles) or appropriately exposing parts to be examined
Table 3. The ABCDE approach to an emergency patient.
DentalUpdate 203
MedicalEmergencies
Figure 3. Pocket mask with a port for oxygen.
Inability to complete sentences or speak Paradoxical movement of chest and abdomen (see-saw respiration) Use of accessory muscles of respiration Blue lips and tongue (central cyanosis) No breathing sounds (complete airway obstruction) Stridor (inspiratory) obstruction of larynx or above Wheeze (expiratory) obstruction of lower airways, eg asthma or chronic obstructive pulmonary disease Gurgling suggests liquid or semi-solid material in the upper airway Snoring the pharynx is partly occluded by the soft palate or tongue
Table 4. Signs of airway obstruction.
often be prevented by early recognition. An abnormal patient colour, pulse rate or breathing can signal some impending emergencies. It is important to have a systematic approach to an acutely ill patient and to remain calm. The principles are summarized in the ABCDE approach (Table 3). These aspects will be considered in turn but it is useful to start with a brief discussion of some general points. Ensure that the environment is safe. It is important to call for help at a very early stage this includes anything from other members of the dental team to calling for an ambulance. Continuous reappraisal of the patients condition should be carried out and the airway must always be the starting point for this. Without appropriate oxygen delivery, all other management steps will be ultimately futile. It is important to assess the success or otherwise of manoeuvres or treatments given, bearing in mind that treatments may take time to work. If the patient is conscious, ask him/her how they are. This may give important information about the problem (for example, the patient who cannot speak or tells you that they have chest pain). If the patient is unresponsive, the patient should be shaken and asked Are you alright?. If they do not respond at all, have no pulse and show no signs of life they have had a cardiac arrest and should be managed as described later. Signs of life refers to breathing and circulation (see later). They may respond in a breathless manner and should be asked Are you choking?.3
Airway (A)
Usually, a simple method of clearing the airway is all that is needed. A head tilt, chin lift or jaw thrust will open the airway. Patients who are unable to speak are in need of urgent attention and establishing a patent airway is vital. It is important to remove any visible foreign bodies, blood or debris and the use of suction may be beneficial. Clearing the mouth should be done with great care using a finger sweep in adults to avoid pushing material further into the upper airway. Simple airway adjuncts, such as an oropharyngeal airway (Figure 2), may be used. An impaired airway may be recognized by some of the signs and symptoms summarized in Table 4. It is important to administer oxygen at high concentration (10 litres per minute) via a well-fitting face mask with a port for oxygen (Figure 3). Even patients with chronic obstructive pulmonary disease who retain carbon dioxide should be given a high concentration of oxygen. Such patients may depend on hypoxic drive to stimulate respiration but, in the short-term, a high concentration of oxygen will do no harm, so its avoidance in an acute situation is unnecessary.
Breathing (B) and Circulation (C)
If there is any doubt as to whether breathing is normal, action should be as if it is not normal, ie commence cardiopulmonary resuscitation (CPR). A victim may be barely breathing or gasping in the first few minutes after cardiac arrest and this should not be mistaken for normal breathing. Agonal gasps refer to abnormal breathing present in up to 40% of victims of cardiac arrest. CPR should therefore be carried out if the victim is unconscious (unresponsive) and not breathing normally. Agonal gasps should not delay the start of CPR as they are not normal breathing.
If the collapsed patient is breathing normally
He/she should be turned into the recovery position (essentially on his/her side best learnt as a practical exercise); Send for help or call for an ambulance; Ensure that breathing continues.
If the patient is not breathing normally
Airway obstruction is a medical emergency and must be managed quickly.
A clinician should look, listen and feel for signs of respiratory distress. This should be done whilst keeping the airway open and the clinician should: Look for chest movement; Listen for breath sounds at the victims mouth; Feel for air on the rescuers cheek with the rescuers head turned against the patients mouth; This should be done for no more than 10 seconds to determine normal breathing;
Ensure an ambulance is summoned (may necessitate leaving the victim) but, in a dental setting, the practitioner should not be working alone; Start chest compressions: kneel at the side of the victim; place the heel of one hand in the centre of the victims chest and the other hand on top of the first hand it will usually be possible to do this without removing the victims clothes. If there is any doubt, outer clothing should be undone/removed; interlock the fingers of both hands do not apply pressure over the ribs, upper abdomen or the lower end of the sternum; the rescuer should be positioned vertically above the victims chest. With May 2009
204 DentalUpdate
MedicalEmergencies
Signs Are the patients hands blue or pink, cool or warm? What is the capillary refill time?* Pulse rate (carotid or radial artery), rhythm and strength. Symptoms Is there a history of chest pain/does the patient report chest pain? *If pressure is applied to the finger nail to produce blanching, the colour should return in less than 2 seconds in a normal patient. Remember that local causes such as a cold environment could also delay the response.
Table 5. Simple methods of circulatory assessment.
hands should be returned to the sternum without delay to continue the chest compressions in a ratio of 30:2. Only stop to recheck the patient if normal breathing starts, otherwise resuscitation should be continuous until: qualified help takes over; the rescuer becomes exhausted.
If rescue breaths do not make the chest rise Figure 4. Algorithm for Basic Life Support in an adult patient (from Resuscitation Council UK).
straight arms the sternum should be depressed 45 cm; after each compression all the pressure should be released so that the rib cage recoils to its rest position but the hands should be maintained in contact with the sternum; the rate should be approximately 100 times per minute (a little less than 2 compressions per second). After 30 compressions, the airway should be opened using head tilt and chin lift and 2 rescue breaths should be given. This may be carried out using a bag and mask or mouth-to-mouth (with the nostrils closed between thumb and index finger) or mouth-to-mask. Practical skills are best learnt on a resuscitation course but certain principles are given below: inflations should make the chest rise. About 1 second should be taken to do this; the chest should be allowed to fall whilst maintaining the airway. Two rescue breaths should be given; May 2009
Check for visible obstruction in the mouth and remove if possible; Make sure that the head tilt and chin lift are adequate; Do not waste time attempting more than two breaths each time before continuing chest compressions. Carrying out these manoeuvres is tiring and, if there is more than one rescuer, CPR should be alternated between them every 2 minutes. The algorithm for adult basic life support is given in Figure 4.
Factors to consider in assessing circulation (C)
when attempted by some healthcare professionals.4 Checking the carotid pulse should only be carried out by those proficient in doing this. The latest guidelines highlight the need to identify agonal gasps (as well as the absence of breathing) as a sign to commence CPR and lay no particular emphasis on checking the carotid pulse. Once A, B and C are secured, persisting problems should be considered by an appraisal of D and E, below, particularly if the patient is still compromised.
Disability (D)
Circulatory assessment should never delay the start of CPR. Simple observations to make a gross assessment of circulatory efficiency are given in Table 5. By far the most common cause of a collapse that is circulatory in origin is the simple faint (vaso-vagal syncope). A rapid recovery can be expected in these cases if the patient is laid flat and the legs raised. Prompt management is required, however, as cerebral hypoxia has devastating consequences if prolonged. Other causes than a faint must be considered if recovery does not happen promptly. It has been found that checking the carotid pulse to diagnose cardiac arrest can be unreliable, even sometimes
Disability is the term which refers to an assessment of the neurological status of the patient. In this context, primarily, it refers to the level of consciousness (in trauma patients a more widespread neurological examination is required). Hypoxia or hypercapnia (increased blood levels of carbon dioxide) are possible causes, together with certain sedative or analgesic drugs. It is important to exclude hypoxia or hypotension and attention to the airway, giving supplemental oxygen and supporting the patients circulation (by lying them supine and raising their legs) will in many cases solve the problem. All unconscious patients who are breathing and have a pulse should be placed in the recovery position if they are unable to maintain their own airway. A rapid gross assessment can be made of a patients level of consciousness using the AVPU method: Are they Alert? Do they respond to Vocal stimuli? DentalUpdate 207
MedicalEmergencies
Arrhythmia (most common type ventricular fibrillation or VF) Myocardial infarction (may lead to an arrhythmia) Choking Bleeding Drug overdose Hypoxia
Table 6. Possible causes of cardiac arrest.
and unable to sustain its function as a pump. The only effective treatment for VF is defibrillation, and the sooner the shock is given, the greater the chance of survival.7 The provision of defibrillation has been made easier by the development of AEDs (Figure 5). AEDs are sophisticated, reliable, safe, computerized devices which use voice and visual prompts to guide rescuers and are suitable for use by lay people and healthcare professionals.8 The device analyses the victims heart rhythm, determines the need for a shock and then delivers a shock. The AED algorithm is given in Figure 6. CPR should not be interrupted/ delayed to set up the AED.
Placement of AED pads
Figure 5. An Automated External Defibrillator (AED).
Do they respond to Painful stimuli? or Are they Unresponsive? A lapse into unconsciousness may be due to hypoglycaemia if the blood glucose level is less than 3mmol/litre as checked by a glucose measuring device (Table 2) then glucagon should be given (see second paper in this series).
Exposure (E)
Exposure refers to loosening or removal of some of the patients clothes. For example, for the application of defibrillator paddles (in dental practice), or if the patient has been involved in a traumatic incident (usually in hospital), for examination purposes. It is important to bear in mind the patients dignity as well as the potential for clinically significant heat loss.
Cardiac arrest other considerations
and are associated with a reduced chance of survival.6 The ideal situation is to be able to deliver continuous chest compressions whilst giving ventilations independently. This is only possible, however, when an advanced airway is placed. Chest compression-only CPR is another way to increase the number of compressions but is only effective for a period of about five minutes.6 For this reason this technique is not recommended. The principle on which compression only CPR works is that, during the first few minutes after a non-asphyxial cardiac arrest, the blood oxygen content remains high and therefore, at this stage, ventilation is less important than chest compression.
Use of the AED is a skill which requires practical training and experience. The victims chest must be sufficiently exposed. Excessive chest hair can stop the pads adhering properly and, if this is markedly the case, must be rapidly removed if possible. Razors are available in AED kits. Resuscitation should never be delayed for this reason, however. One pad should be placed to the right of the sternum below the clavicle. The other pad should be placed in the left side mid-axillary line, centred on the fifth intercostal space. This electrode works best if orientated vertically. This position should be clear of any breast tissue. Although most AED pads are labelled or carry a picture of their position, it does not matter if they are reversed. Once familiarity with this item of equipment is achieved, its use is simple.
Principles of management after the initial treatment of a medical emergency
An ambulance should be called at the earliest opportunity as part of the management of any significant medical event. If the dental practitioner feels competent and confident that the emergency has been managed satisfactorily, and the patient is stable, they should still not be allowed to leave the dental practice unaccompanied or be allowed to drive a motor vehicle. The decision will be easier to take in some circumstances than others. For example, the patient who has an angina attack in May 2009
Use of defibrillation
Defibrillation is the term which refers to the termination of fibrillation. It is achieved by administering a controlled electrical shock to the heart which may restore an organized rhythm, enabling the heart to contract effectively. It is now well recognized that early defibrillation is important. Ventricular fibrillation (VF) is the most common cause of cardiac arrest. It is a rapid and chaotic rhythm and, as a result, the heart is unable to contract effectively
Cardiac arrest can occur for a variety of reasons which are summarized in Table 6. It has been suggested5 that cardiopulmonary resuscitation can be performed effectively in the dental chair, but it should always be confirmed that this is the case. Interruptions to chest compression in resuscitation are common
208 DentalUpdate
MedicalEmergencies
is documenting the fact that a patient has been given aspirin or undergone dental surgery, making them prone to haemorrhage, which may influence the decision to give antithrombolytic therapy.
Summary
Medical emergencies in dental practice are not common but could occur at any time. Such events are less alarming and best managed if they have been anticipated and if mechanisms are in place (and regularly reviewed) for dealing with them. Adherence to basic principles is key for effective management. Specific medical emergencies, requiring measures in addition to the general considerations discussed here, are discussed in the second paper.
References
1. Atherton GJ, McCaul JA, Williams SA. Medical emergencies in general dental practice in Great Britain. Part 1: their prevalence over a 10-year period. Br Dent J 1999; 186: 7279. Medical Emergencies and Resuscitation Standards for Clinical Practice and Training for Dental Practitioners and Dental Care Professionals in General Dental Practice A statement from the Resuscitation Council (UK), London, July 2006. Revised May 2008. Adult Basic Life Support Resuscitation Guidelines 2005. London: Resuscitation Council (UK). Bahr J, Klingler H, Panzer W, Rode H, Kettler D. Skills of lay people in checking the carotid pulse. Resuscitation 1997; 35: 2326. Lepere AJ, Finn J, Jacobs I. Efficacy of cardiopulmonary resuscitation performed in a dental chair. Aust Dent J 2003; 48: 244247. Hallstrom A, Cobb L, Johnson E, Copass M. Cardiopulmonary resuscitation by chest compression alone or with mouth-tomouth ventilation. N Engl J Med 2000; 342: 15461553. Leitch J, Schmulian C, Scott A. Automatic external defibrillators time for a change? Br Dent J 2005; 198: 209210. Boyd BC, Fantuzzo JJ, Votta T. The role of automated external defibrillators in dental practice. N Y State Dent J 2006; 72: 2023. DentalUpdate 211
2.
3.
4.
5.
Figure 6. Automated External Defibrillator (AED) algorithm. Continue until victim able to breathe normally (Resuscitation Council UK).
6.
the surgery, responds very quickly to their normal GTN, and who has a clear history of similar episodes and makes a complete recovery, will usually be well enough to be allowed home. If a patient remains unwell, or there is any doubt at all, they should undergo May 2009
assessment by a medical practitioner. Before any transfer is made, the patients condition should be stabilized as long as that does not delay ongoing treatment. It is important that a written summary is given to the receiving team so that treatment that has been undertaken is made clear. A good example
7.
8.
You might also like
- Dental Diet and Fluoride Advice for ChildDocument13 pagesDental Diet and Fluoride Advice for ChildbabukanchaNo ratings yet
- A Guide To Succeeding in The Df1 Interview (Sample Pages Only)Document15 pagesA Guide To Succeeding in The Df1 Interview (Sample Pages Only)jaipald9067% (3)
- Dental Update 2009. Consequences of Tooth Loss 1. The Patient Perspective Aesthetic and Functional ImplicationsDocument4 pagesDental Update 2009. Consequences of Tooth Loss 1. The Patient Perspective Aesthetic and Functional ImplicationsHasan KhanaferNo ratings yet
- Endodontic Failures-A Review: Dr. Sadashiv Daokar, DR - Anita.KalekarDocument6 pagesEndodontic Failures-A Review: Dr. Sadashiv Daokar, DR - Anita.KalekarGunjan GargNo ratings yet
- Sample Questions MJDF Part 1 Sample Questions MJDF Part 1Document21 pagesSample Questions MJDF Part 1 Sample Questions MJDF Part 1HarkanNo ratings yet
- Australian Dental Journal: Rhinosinusitis in Oral Medicine and DentistryDocument7 pagesAustralian Dental Journal: Rhinosinusitis in Oral Medicine and DentistryVishakha SabooNo ratings yet
- Changing Concepts in Cariology - Forty Years OnDocument7 pagesChanging Concepts in Cariology - Forty Years OnDavid CaminoNo ratings yet
- Department of Pedodontics: Submitted By: Shayoni Sen Bds Ivth YearDocument29 pagesDepartment of Pedodontics: Submitted By: Shayoni Sen Bds Ivth YearFarzana ShereenNo ratings yet
- What Is Root Canal Treatment?Document2 pagesWhat Is Root Canal Treatment?Vishakha SabooNo ratings yet
- The Single-Tooth RestorationDocument5 pagesThe Single-Tooth Restorationumerjaved86No ratings yet
- Sorting Out Endodontic Symptoms: ©JK Mitchell, DDS, Med April 2012Document2 pagesSorting Out Endodontic Symptoms: ©JK Mitchell, DDS, Med April 2012sao_tren_troi100% (1)
- What After BDS Career OptionsDocument10 pagesWhat After BDS Career OptionsDENTALORG.COM100% (1)
- OSCEs For DentistryDocument3 pagesOSCEs For DentistryMohammed IssaNo ratings yet
- Vital Therapy in Carious ToothDocument9 pagesVital Therapy in Carious ToothAsh PeiNo ratings yet
- Lecture 4 Diagnosis of Dental CariesDocument12 pagesLecture 4 Diagnosis of Dental CariesDt omarNo ratings yet
- MdsDocument356 pagesMdsARJUN SreenivasNo ratings yet
- Interpretation of OpgDocument6 pagesInterpretation of Opgjawaad29375% (8)
- AAE Newsletter Covers Endodontic TreatmentDocument6 pagesAAE Newsletter Covers Endodontic TreatmentMehwish MunawarNo ratings yet
- Cavity design techniques for optimizing Class IV composite restorationsDocument6 pagesCavity design techniques for optimizing Class IV composite restorationselokfaiqNo ratings yet
- Root FracturesDocument9 pagesRoot FracturesAbhilashPadmanabhanNo ratings yet
- Pickard's Manual-Tooth Wear (Dragged)Document8 pagesPickard's Manual-Tooth Wear (Dragged)Adit MehtaNo ratings yet
- Endo NotesDocument184 pagesEndo NotesSOMVIR KUMARNo ratings yet
- Pediatric DentistryDocument15 pagesPediatric Dentistrymirfanulhaq100% (2)
- MFD Last LastDocument56 pagesMFD Last LastFree PizzaNo ratings yet
- Dental AuxiliariesDocument14 pagesDental AuxiliariesnainaNo ratings yet
- Overprotective parenting and dental varnishDocument11 pagesOverprotective parenting and dental varnishQq qNo ratings yet
- Caldwell TechniqueDocument4 pagesCaldwell TechniqueNurul RamadhantyNo ratings yet
- Iotn Ruler Made EasyDocument7 pagesIotn Ruler Made EasyZahid Ahmad100% (1)
- MJDF April 2019Document5 pagesMJDF April 2019Ali Al-QaysiNo ratings yet
- Journal ClubDocument2 pagesJournal ClubWaseem AhmedNo ratings yet
- ORE MCQsDocument268 pagesORE MCQspawi18No ratings yet
- Basics of Endodontics GuideDocument26 pagesBasics of Endodontics GuideAreebaKhalidNo ratings yet
- 2 Nonsurgical Periodontal Therapy - Pocket DentistryDocument14 pages2 Nonsurgical Periodontal Therapy - Pocket DentistryRizki OktavianiNo ratings yet
- Lecture 5 Laser in Operative DentistryDocument7 pagesLecture 5 Laser in Operative DentistryDt omarNo ratings yet
- Aae Endodonticglossary2016Document50 pagesAae Endodonticglossary2016h20pologtNo ratings yet
- Comprehensive Review for Saudi Licence Exam for General DentistDocument4 pagesComprehensive Review for Saudi Licence Exam for General Dentistzoaib aliNo ratings yet
- A Road To TOACSDocument33 pagesA Road To TOACSSoha Jan KhuhawarNo ratings yet
- U of T Faculty of Dentistry Restorative Clinic ManualDocument245 pagesU of T Faculty of Dentistry Restorative Clinic ManualHelen ShNo ratings yet
- Overseas Registration Examination Reading ListDocument3 pagesOverseas Registration Examination Reading ListyoNo ratings yet
- 9.factors Controlling The Dental X-Ray Beam PDFDocument9 pages9.factors Controlling The Dental X-Ray Beam PDFAnonymous lbPSiuHjNo ratings yet
- Emergency Drugs in Dental PracticeDocument3 pagesEmergency Drugs in Dental PracticeRishwan Omer SalihNo ratings yet
- Vertical Root Fracture !Document42 pagesVertical Root Fracture !Dr Dithy kkNo ratings yet
- Pulp Therapy For Primary and Immature Permanent TeethDocument11 pagesPulp Therapy For Primary and Immature Permanent TeethPrabhjot KaurNo ratings yet
- 2014 Osce ProtocolDocument15 pages2014 Osce ProtocolAamir BugtiNo ratings yet
- MJDF Part 1 QuestionsDocument21 pagesMJDF Part 1 QuestionsHabeeb AL-AbsiNo ratings yet
- Literature GuideDocument60 pagesLiterature Guide12345sagarNo ratings yet
- Biomechanics and Clinical Implications of Complete Edentulous StateDocument4 pagesBiomechanics and Clinical Implications of Complete Edentulous StateDorobantuMihaiGabiNo ratings yet
- 1-2-3 Steps in Endodontic Irrigation PDFDocument4 pages1-2-3 Steps in Endodontic Irrigation PDFAnn M.No ratings yet
- Effective Cutting with Cross-Cut Fissure BursDocument45 pagesEffective Cutting with Cross-Cut Fissure BursMustapha RammalNo ratings yet
- Mock Answers PDFDocument19 pagesMock Answers PDFHarjotBrar100% (1)
- Pediatric DentistryDocument15 pagesPediatric DentistryPeyman Dhg100% (2)
- Past Papers 1 200Document55 pagesPast Papers 1 200AmarAldujaili100% (1)
- Pediatric Dentistry Exam QuestionnaireDocument2 pagesPediatric Dentistry Exam QuestionnaireVagelis RaftopoulosNo ratings yet
- FSBGD MCQ Study Questions 2000Document68 pagesFSBGD MCQ Study Questions 2000Sara IskanderNo ratings yet
- Dental MCQ Exam PrepDocument65 pagesDental MCQ Exam PrepGloria JaisonNo ratings yet
- Evidence Based Management Third MolarsDocument73 pagesEvidence Based Management Third MolarsCiutac ŞtefanNo ratings yet
- Essential Tissue Healing of the Face and NeckFrom EverandEssential Tissue Healing of the Face and NeckRating: 5 out of 5 stars5/5 (2)
- Fixed Orthodontic Appliances: A Practical GuideFrom EverandFixed Orthodontic Appliances: A Practical GuideRating: 1 out of 5 stars1/5 (1)
- NATIONAL DENTAL BOARDS (NDB) / PART I: Passbooks Study GuideFrom EverandNATIONAL DENTAL BOARDS (NDB) / PART I: Passbooks Study GuideRating: 1 out of 5 stars1/5 (1)
- The ADA Practical Guide to Patients with Medical ConditionsFrom EverandThe ADA Practical Guide to Patients with Medical ConditionsNo ratings yet
- Modelo de NDA (English)Document2 pagesModelo de NDA (English)Jorge Partidas100% (3)
- GPL 12800 (80) AhDocument1 pageGPL 12800 (80) AhismailNo ratings yet
- Alcalel-Lucent WLAN OmniAcces StellarDocument6 pagesAlcalel-Lucent WLAN OmniAcces StellarJBELDNo ratings yet
- Frequently Asked Questions (And Answers) About eFPSDocument10 pagesFrequently Asked Questions (And Answers) About eFPSghingker_blopNo ratings yet
- Lilypad Hotels & Resorts: Paul DidriksenDocument15 pagesLilypad Hotels & Resorts: Paul DidriksenN.a. M. TandayagNo ratings yet
- Imantanout LLGDDocument4 pagesImantanout LLGDNABILNo ratings yet
- Seaflo Outdoor - New Pedal Kayak Recommendation July 2022Document8 pagesSeaflo Outdoor - New Pedal Kayak Recommendation July 2022wgcvNo ratings yet
- Swilliams Lesson6Document11 pagesSwilliams Lesson6api-276783092No ratings yet
- Econometrics ProjectDocument17 pagesEconometrics ProjectAkash ChoudharyNo ratings yet
- DB51 BTP 160 8PDocument1 pageDB51 BTP 160 8Pnagaraj.ss@quest-global.comNo ratings yet
- Reinforced and Filled Poly (Phenylene Sulfide) (PPS) Injection Molding and Extrusion Materials Using ASTM MethodsDocument6 pagesReinforced and Filled Poly (Phenylene Sulfide) (PPS) Injection Molding and Extrusion Materials Using ASTM MethodsJosé Miguel Palomino GarciaNo ratings yet
- Resume DaniellaAmatoDocument2 pagesResume DaniellaAmatoDaniellaNo ratings yet
- BVM Type B Casing Tong ManualDocument3 pagesBVM Type B Casing Tong ManualJuan Gabriel GomezNo ratings yet
- Garments & Tailoring Business: Submitted byDocument6 pagesGarments & Tailoring Business: Submitted bykartik DebnathNo ratings yet
- Caterpillar Cat 330L EXCAVATOR (Prefix 8FK) Service Repair Manual (8FK00001 and Up)Document27 pagesCaterpillar Cat 330L EXCAVATOR (Prefix 8FK) Service Repair Manual (8FK00001 and Up)kfm8seuuduNo ratings yet
- S-S-, AXXX XXX 008 (BIA Sept. 15, 2017)Document7 pagesS-S-, AXXX XXX 008 (BIA Sept. 15, 2017)Immigrant & Refugee Appellate Center, LLCNo ratings yet
- Plastic Waste Powerpoint TemplateDocument39 pagesPlastic Waste Powerpoint TemplateVinh Lê KhảiNo ratings yet
- Built For Your Business and The Environment.: WORKFORCE PRO WF-C5290/C5790Document4 pagesBuilt For Your Business and The Environment.: WORKFORCE PRO WF-C5290/C5790abe cedeevNo ratings yet
- Money and Financial InstitutionsDocument26 pagesMoney and Financial InstitutionsSorgot Ilie-Liviu100% (1)
- Reconciling Informal and Formal TradeDocument194 pagesReconciling Informal and Formal TradeBaterias BateriasNo ratings yet
- Ed TechDocument19 pagesEd TechAlexie AlmohallasNo ratings yet
- TG Comply With WP Hygiene Proc 270812 PDFDocument224 pagesTG Comply With WP Hygiene Proc 270812 PDFEmelita MendezNo ratings yet
- Financial Ratios ActivityDocument3 pagesFinancial Ratios ActivityNCF- Student Assistants' OrganizationNo ratings yet
- Training Prospectus 2020 WebDocument89 pagesTraining Prospectus 2020 Webamila_vithanageNo ratings yet
- What is a Server ClusterDocument2 pagesWhat is a Server Clusterfikru tesefayeNo ratings yet
- Pass Microsoft 74-343 Exam: Number: 74-343 Passing Score: 800 Time Limit: 120 Min File Version: 40.2Document26 pagesPass Microsoft 74-343 Exam: Number: 74-343 Passing Score: 800 Time Limit: 120 Min File Version: 40.2tapera_mangeziNo ratings yet
- Q.850 ISDN Cause CodesDocument12 pagesQ.850 ISDN Cause CodesJack CastineNo ratings yet
- Deploy A REST API Using Serverless, Express and Node - JsDocument13 pagesDeploy A REST API Using Serverless, Express and Node - JszaninnNo ratings yet
- Instructions Manual Skatey 150/250/400/600Document19 pagesInstructions Manual Skatey 150/250/400/600Denys GavrylovNo ratings yet
- 11 EngineDocument556 pages11 Enginerumen80100% (3)