Professional Documents
Culture Documents
Management of Rhinosinusitis in Dutch General Practice: Society UK
Uploaded by
Mohamed Rikarz Ahamed RikarzOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Management of Rhinosinusitis in Dutch General Practice: Society UK
Uploaded by
Mohamed Rikarz Ahamed RikarzCopyright:
Available Formats
Copyright PCRS-UK - reproduction prohibited
Primary Care Respiratory Journal (2011); 20(1): 64-70
ORIGINAL RESEARCH
Management of rhinosinusitis in Dutch general practice
*Ruth Hoffmansa, Tjard Schermerb, Chris van Weelb, Wytske Fokkensa
a b
Department of Otorhinolaryngology, Academic Medical Centre, Amsterdam, The Netherlands Department of Primary and Community Care, Nijmegen Medical Centre, Radboud University, Nijmegen, The Netherlands
Received 18th June 2010; revised 26th July 2010; accepted 28th July 2010; online 10th February 2011
Abstract
Aims: To determine whether general practitioners (GPs) distinguish between the management of acute rhinosinusitis (ARS) and chronic rhinosinusitis (CRS), especially with regard to prescription of antibiotics and nasal steroids.
Conclusions: Most GPs discriminate between ARS and CRS and 54% accepted (the EP3OS-defined) 12 weeks as the division between ARS and CRS. Antibiotics and nasal steroids are commonly used agents, but the management of rhinosinusitis is not always consistent with guidelines. 2011 Primary Care Respiratory Society UK. All rights reserved. R Hoffmans et al. Prim Care Respir J 2011; 20(1): 64-70 doi:10.4104/pcrj.2010.00064
Keywords acute rhinosinusitis, chronic rhinosinusitis, primary care, antibiotics, nasal steroids, guidelines.
College of General Practitioners4 which does not distinguish between ARS and CRS. Treatment is based on the severity of symptoms and the risk of developing complications. The guideline advises treating symptoms initially and states that antibiotics are not indicated for a normal course of rhinosinusitis. Local steroids can be tried in patients with an abnormal course or recurrent complaints.4 The European guideline, The European Position Paper on Rhinosinusitis and Nasal Polyps (EPOS) advises distinguishing between ARS and CRS and basing management on the severity of the disease. Depending on severity, the recommendation for mild ARS (common cold) is to treat symptoms, with nasal steroids being advised in moderate cases. Antibiotics are added only when there are severe symptoms (fever >38C, severe pain). The first choice treatment in the management of CRS is local steroids.1,2 In a cross-sectional study covering 174 GPs from 89 general practices in the Netherlands, 50% of antibiotic prescriptions were prescribed for respiratory disorders.5,6 Twenty-two percent of the antibiotics for respiratory tract infections (RTIs) were
See linked editorial by Levy on pg 11
Rhinosinusitis is defined as a sudden onset of two or more symptoms, one of which should be either nasal blockage or nasal discharge (anterior or posterior nasal drip). Other symptoms are facial pain or pressure, and impairment or loss of smell. When these symptoms are present for less than 12 weeks, this defines acute rhinosinusitis (ARS). When symptoms are present for more than 12 weeks, this represents chronic rhinosinusitis (CRS). ARS can be divided into two groups: common cold/acute viral rhinosinusitis (symptoms disappear in less than 10 days); and acute non-viral/bacterial rhinosinusitis (increase of symptoms after five days or persistent symptoms after 10 days).1-3 In the Netherlands, general practitioners (GPs) generally use the rhinosinusitis management guidelines from the Dutch
* Corresponding author: Mrs Ruth Hoffmans, Department of Otorhinolaryngology , Academic Medical Centre, Meibergdreef 9, Amsterdam, 1105 AZ, The Netherlands. Tel: +31205663789 E-mail: r.hoffmans@amc.uva.nl
PRIMARY CARE RESPIRATORY JOURNAL www.thepcrj.org doi:10.4104/pcrj.2010.00064
op y
Introduction
rig
The full version of this paper, with online Appendix, is available at www.thepcrj.org
ht P
rim R a ep ry ro C du ar ct e R io e n sp pr ir oh at ib ory ite S d o
64
Results: Ninety-six percent discriminated between ARS and CRS. However, the definition of ARS and CRS varied. The percentage of GPs prescribing antibiotics rose as rhinosinusitis severity increased. The prescription rate of nasal corticosteroids was highest for CRS (88.6%). Prescribing nasal corticosteroids in ARS was not very common.
http://www.thepcrj.org
ci et
Methods: A questionnaire on the management of rhinosinusitis was sent to 1000 GPs in the Netherlands.
Copyright PCRS-UK - reproduction prohibited
Management of rhinosinusitis in Dutch general practice
Methods
Study design
Questionnaire (see Appendix A at www.thepcrj.org)
The questionnaire consisted of three parts: 1. GP characteristics (kind of practice, age etc.) 2. A question on whether the GP differentiated between ARS and CRS 3. Two different questionnaires about the management of rhinosinusitis: a) One for GPs differentiating between ARS and CRS b) One for non-differentiating GPs GPs were asked to fill out parts 1 and 2 and, depending on the answer to question 2, either part 3a or 3b. The questionnaire consisted mainly of multiple-choice questions to facilitate participation. The questions about management of rhinosinusitis were sub-divided into questions about three categories: Mild rhinosinusitis: symptoms present for less than five
PRIMARY CARE RESPIRATORY JOURNAL www.thepcrj.org
op y
The Netherlands institute for health services research (NIVEL) was contacted for a random sample of 1000 Dutch GPs (the total GP population on 1 January 2007 was 8,67321). A questionnaire on the management of ARS and CRS was developed by the authors of EPOS and sent to these 1000 GPs. All the GPs were given an ID number to determine which GP returned the questionnaire. When GPs did not respond to the first mailing, a second questionnaire was sent three weeks later.
rig
ht P
rim R a ep ry ro C du ar ct e R io e n sp pr ir oh at ib ory ite S d o
prescribed for rhinosinusitis.6 The prescription rate in sinusitis-like complaints was 67-70%.7,8 In another study, the antibiotic prescription rate in rhinosinusitis was 80%,9 and prescription rates for sinus infection in the UK are 91% - 92%.10,11 Dutch prescription percentages for outpatient antibiotic use are relatively low compared with international figures.12-14 It has been theorised that, by reducing the inflammatory response and mucosal swelling, a topical steroid may promote drainage and increase aeration of the sinuses, hasten the elimination of infectious organisms, and reduce the frequency and severity of recurrences.15 Several studies have concluded that nasal steroids (in combination with antibiotics or alone) are beneficial in ARS and equally or more effective than antibiotics.15-18 Furthermore, nasal steroids are the treatment of first choice in CRS.2,19 Recently available data are based on general practice registries in which no distinction is made between ARS and CRS. As a result, we are not able to determine whether GPs distinguish between ARS and CRS.20 The objective of this study, therefore, was to determine whether GPs distinguish between the management of ARS and CRS, and how Dutch GPs manage these two diseases (especially with regard to the prescription of antibiotics and nasal steroids).
days or improving thereafter Moderate rhinosinusitis: persistent symptoms after 10 days or worsening symptoms after five days Severe rhinosinusitis: persistent symptoms after 10 days or worsening. The GPs ranked their different treatment options from 1 to 10 (most often (1) least often (10)). Since the ranks of the different treatment options were not normally distributed, we calculated the median rank per treatment option to describe the GPs treatment preferences within the severity categories.
Analysis
Data were analysed with SPSS (Statistical Package for the Social Sciences) 16.0. We received information about the characteristics (sex, kind of practice, age and years of practice) of all Dutch GPs from the NIVEL to decide whether the characteristics of the GPs included in this study were representative of the entire GP population.
Results
Five hundred questionnaires were returned (a response rate of 50%). Twenty-nine GPs refused to participate, 46 GPs completed parts 1 and 2 only, 395 filled out the complete questionnaire, and 26 forgot to complete parts 1 and 2 but did fill out part 3a or b. Four GPs said they discriminated between ARS and CRS, but completed part 3b instead of 3a (Figure 1). Four duplicate cases (IDs) were found in the responders. Since we did not know which were the right questionnaires, we used both in our analysis. Most of the parameters of the responder GPs (who returned the questionnaire) were comparable to the nonresponders (GPs who did not respond). Of the responders, 33% worked in a group practice, but this figure was 60% for the non-responders (p=0.000). Furthermore, the responders worked more often alone or in a practice with one other GP than the non-responders. The only age group in which there was a significant difference between responders and nonFigure 1. Organogram.
1000 questionnaires
ci et
500 returned*
504 not returned* 29x refused
395x complete
76x incomplete
4x part 3 incorrect 26x only part 3 46x only part 1 and 2
* Four questionnaires were returned twice
65
http://www.thepcrj.org
Copyright PCRS-UK - reproduction prohibited
R Hoffmans et al.
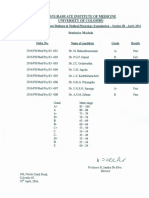
Table 1. Characteristics.
Responders % Male Female Solopractice Duopractice Grouppractice Aged < 30 years Aged 30-34 years Aged 35-39 years Aged 40-44 years Aged 54-49 years Aged 50-54 years Aged 55-59 years Aged 60-64 years Aged > 65 years <5 years of practice 5-10 years of practice 10-15 years of practice 15-20 years of practice 20-25 years of practice >25 years of practice 682 318 339* 335* 326* 04 40 146* 144 162 198 193 108 04 155* 173 155 131 133 252 Non-responders % 713 287 163 235 602 00 32 83 154 147 241 221 110 13 61
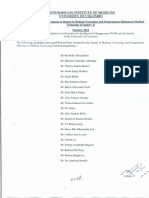
Figure 2. Duration of symptoms to be considered CRS.
60 50 40 30 20 10 0.5 0 1 week 4 weeks 12 weeks half a year 1 year 6.5 0.2 39.1 53.7
% of GPs
Table 2. Treatment of mild ARS.
K
Treatment Decongestives Painkillers Steaming
ci et
No treatment
U y
% prescribing 913 658 558 317 206 194 69 51 32 28 23 23
Mild ARS % 485 515 Median rank % first choice 10 20 20 20 40 30 40 40 90 25 20 65 612 372 184 349 26 26 00 91 00 167 200 00
* Significant difference between responders and non-responders (p<005)
responders was the 35-39-year group (p=0.001). Significantly more responders had worked as GPs for less than five years (Table 1).
ht P
Do you discriminate between ARS and CRS for your treatment?
Ninety-six percent said they differentiated (the differentiating group) between ARS and CRS. The management of GPs differentiating between ARS and CRS will be further evaluated. The group of GPs that do not differentiate between ARS and CRS is too small to draw any significant conclusions.
rig
op y
How long must symptoms have been present before you consider a diagnosis of CRS to be appropriate?
An analysis of the answers from the differentiating group of GPs showed that most GPs see 12 weeks as the critical period (54%), with a slightly smaller group opting for 4 weeks (39%). The other 7% of GPs adopted other periods of time (see Figure 2).
What percentage of your population has been diagnosed with rhinosinusitis in the past 12 months?
The incidence estimate from most of the GPs in the differentiating group was 2-5% for ARS and less than 2% for CRS.
Do you agree with the following statement? To diagnose rhinosinusitis, radiology is not recommended
In the differentiating group, 98% of the GPs reported that
PRIMARY CARE RESPIRATORY JOURNAL www.thepcrj.org
rim R a ep ry ro C du ar ct e R io e n sp pr ir oh at ib ory ite S d o
198 162 128 158 293 Nasal douche Oral antibiotics Nasal steroids Oral antihistamine Mucolytics Systemic steroids Other Topical antibiotics
Alternative treatment
Median rank of the GPs prescribing this medicine (1=most often, 10=least often)
there is no need for radiology in diagnosing ARS. Opinions differed for CRS: 39% still agreed there was no need for radiology, but 54% usually arranged an X-ray, 2% suggested a CT scan and 5% proposed something else.
Do you treat patients with mild acute rhinosinusitis?
Of the differentiating group, 51.5% treated patients with mild ARS. They prescribed decongestives most frequently (91.3%). Decongestives had a median rank of 1 (first-choice treatment). 20.6% of the GPs prescribed oral antibiotics. However, only 2.6% of them reported that antibiotics were their first choice treatment. The median rank for prescribing antibiotics was 4. Nasal steroids were prescribed by 19.4% of the GPs and the median rank was 3 (see Table 2). Again, only 2.6% of them reported nasal steroids to be their first-choice treatment.
66
http://www.thepcrj.org
Copyright PCRS-UK - reproduction prohibited
Management of rhinosinusitis in Dutch general practice
Table 3. Treatment of moderate ARS.
Moderate ARS % No treatment Treatment % prescribing Decongestives Painkillers Steaming Nasal steroids Oral antibiotics Nasal douche Oral antihistamine Mucolytics Systemic steroids Alternative treatment Topical antibiotics Other 835 623 452 373 340 285 72 51 27 18 18 09 175 825 Median rank % first choice 10 20 20 25 30 20 40 50 100 90 90 100 595 387 222 217 172 215 00 00 00 200 167 333
Table 4. Treatment of severe ARS.
Severe ARS % No treatment Treatment % prescribing Oral antibiotics Decongestives Painkillers Steaming Nasal steroids Nasal douche Oral antihistamine Systemic steroids Mucolytics Topical antibiotics Other 840 755 754 402 280 23 51 48 10 990 Median rank % first choice 20 20 20 30 30 30 50 50 50 45 100 100 391 348 477 152 147 145 150 00 83 250 333 200
ci et
Median rank of the GPs prescribing this medicine (1=most often, 10=least often)
Do you treat patients with moderate acute rhinosinusitis?
rig
Most (82.5%) of the differentiating GPs treated patients with moderate rhinosinusitis. Decongestives were most frequently prescribed and were their first choice treatment. Antibiotics were prescribed by 34% of the GPs, and ranked third. 17.2% of the GPs prescribing antibiotics reported this treatment to be their first choice. An even higher percentage (37.3%) prescribed nasal steroids (median rank 2.5). Of these GPs, 21.7% said that nasal steroids were their preferred treatment (see Table 3).
ht P
Nearly all GPs in the differentiating group treated patients with severe ARS (99%). Antibiotics were most frequently prescribed (84%). 39.1% of the GPs prescribing antibiotics reported antibiotics to be their first choice. The median rank for prescribing antibiotics was 2, but there was no median rank 1. The most commonly prescribed antibiotic in mild, moderate and severe (A)RS was doxycycline. Nasal steroids were prescribed by 28% of the GPs treating severe ARS; 14.7% of them said that nasal steroids was their first choice treatment. The median rank for nasal steroids was 3 (see Table 4).
Do you treat patients with severe acute rhinosinusitis?
op y
When do you refer patients with moderate (acute) rhinosinusitis to a specialist?
Almost half of the GPs (46.5%) said that they never refer these patients to a specialist. One-third reported referring after four weeks of treatment without improvement. 6% referred after two weeks of treatment without improvement, and 1.5%
PRIMARY CARE RESPIRATORY JOURNAL www.thepcrj.org
rim R a ep ry ro C du ar ct e R io e n sp pr ir oh at ib ory ite S d o
67
Alternative treatment
Median rank of the GPs prescribing this medicine (1=most often, 10=least often)
referred after one unsuccessful course of antibiotics. The rest had other policies for referring these patients.
When do you refer patients with severe (acute) rhinosinusitis to a specialist?
One-third of the GPs from the differentiating group referred after two weeks of treatment without result. 17.9% did this after four weeks and 14.2% after one course of antibiotics. 10% never referred and 11.4% did after 48 hours if there was no effect from nasal steroids and/or antibiotics. Two GPs (0.5%) always referred.
When do you refer patients with ocular or neurological complications to a specialist?
Most of the differentiating GPs always referred to a specialist (87.8%). 2% reported referring after two weeks of treatment without improvement and 3.5% after 48 hours if there was no effect from nasal steroids and/or antibiotics. 1.7% referred after one course of antibiotics that did not work, 0.5% never referred and 4.5% did something else.
Do you treat patients with CRS?
Seventeen GPs (4.2%) did not treat these patients. Four of them always referred these patients to a specialist. The 95.8% who did treat patients with CRS prescribed nasal steroids most frequently (88.6%). Of these, 71.3% reported nasal steroids as their preferred treatment. They ranked nasal steroids first. Antibiotics were prescribed by 41.3% of the GPs, 36.9% of whom preferred this treatment above others. The median rank of antibiotics was 2 (see Table 5).
When do you refer patients with CRS to a specialist?
Over half of the differentiating GPs (60.8%) reported referring
http://www.thepcrj.org
K
23 13 13
35
Copyright PCRS-UK - reproduction prohibited
R Hoffmans et al.
Table 5. Treatment of CRS.
CRS % No treatment Treatment % prescribing Painkillers Nasal steroids Oral antibiotics Oral antihistamine Decongestives Nasal douche Steaming Systemic steroids Mucolytics Other Alternative treatment Topical antibiotics 475 886 413 245 222 191 142 93 39 21 21 21 42 958 Median rank % first choice 20 10 20 20 20 20 30 30 40 35 65 100 289 713 369 45 229 159 149 161 00 00 00 286
Median rank of the GPs prescribing this medicine (1=most often, 10=least often)
after four weeks of treatment without improvement. 15% referred after two weeks of treatment, 2% never referred, 1.7% always referred to a specialist, and 1.2% referred after one unsuccessful course of antibiotics. The others (19.2%) had various other strategies like on demand of the patient or in case of recurrence.
When do you want patients with CRS to visit you again for reassessment after you start therapy?
ARS and CRS may both be termed rhinosinusitis, meaning inflammation of the nose and sinuses. However, for clinical and research purposes, differentiation between these entities is preferable. Although far from being completely understood, pathological mechanisms in ARS and CRS are better understood today and begin to allow us to differentiate these diseases in terms of their cytokine profile, pattern of inflammation, and their remodelling processes.2 It is therefore important to distinguish ARS from CRS because these two disease entities seem to have different underlying aetiologies and pathogenesis. Although an earlier study did not allow us to determine whether GPs differentiated between ARS and CRS,20 this study proves that they do (96% did differentiate). It is surprising that GPs do differentiate, given that the Dutch College of General Practitioners guideline does not distinguish between
PRIMARY CARE RESPIRATORY JOURNAL www.thepcrj.org
Discussion
op y
rig
Most of the GPs (55.6%) wanted their patients to come back after two weeks and 38.7% after four weeks. Five GPs (1.3%) reassessed after 48 hours and 4.4% after 12 weeks.
ARS and CRS.4 In fact, a guideline for chronic rhinosinusitis that will make this distinction is being developed by (among others) otorhinolaryngologists and GPs.22 In this study, the duration of symptoms after which the GPs consider the condition to be CRS is not consistent. EPOS recommends a period of 12 weeks.2 Approximately half the GPs surveyed said that they used 12 weeks as their criterion. The period used by the rest varied. Almost no GPs use radiology for diagnosing ARS, which is in accordance with current guideline advice.2,4 The conclusion of a Dutch randomised controlled trial in 1997 was that, for patients with acute maxillary rhinosinusitis presenting to general practice, an initial radiographic examination is not necessary.23 This study also concluded that antibiotic treatment (with amoxicillin) did not improve the clinical course of rhinosinusitis presenting in general practice.23 Acute rhinosinusitis will often resolve in most patients without antibiotic treatment, even if it is bacterial in origin.23-26 Common clinical signs and symptoms cannot identify patients with rhinosinusitis for whom treatment with antibiotics is clearly justified. Antibiotics are not justified even if a patient reports symptoms persisting for more than 7-10 days.26 Data from Jacobs et al. demonstrate the continued evolution of bacterial resistance due to the overprescribing of antibiotics and highlight the need for limiting the unnecessary prescription of antimicrobials in community-acquired respiratory tract infections (RTIs).27 It has been shown that countries with high levels of consumption have higher rates of antibiotic resistance.13 Although the antibiotic prescription rate in the Netherlands is extremely low compared to most European countries, and Dutch GPs do well,12-14 a considerable amount of antibiotics is still used unnecessarily. In our study, GPs consider prescribing antibiotics for mild to moderate acute rhinosinusitis, whilst the guidelines recommend otherwise. The results of recent randomised controlled trials constitute a firm scientific basis for restrictive antibiotic prescription behaviour.23,25 Initial management can be limited to symptom treatment.4,23 The EPOS guidelines consider symptoms lasting for less than five days, or improving thereafter, to constitute a common cold in which case symptomatic treatment is advisable. When symptoms worsen after five days or persist after 10 days, a distinction is made between moderate and severe ARS. Severe ARS is ARS with fever > 38C and/or severe pain. For moderate rhinosinusitis, topical steroids are advised, and antibiotics and nasal steroids are advised for severe ARS.2 These recommendations are based on recent studies showing that additional nasal corticosteroids are as effective as, or more effective than, antibiotics.15-18 This provides a welcome alternative to antibiotics without the negative consequences of microbial resistance. In the Dutch
ht P
rim R a ep ry ro C du ar ct e R io e n sp pr ir oh at ib ory ite S d o
68
http://www.thepcrj.org
ci et
Copyright PCRS-UK - reproduction prohibited
Management of rhinosinusitis in Dutch general practice
College of General Practitioners guideline, local corticosteroids are advised only after the failure of other treatment, in persistent or recurring complaints, or in patients with an abnormal course of rhinosinusitis.4 Corticosteroid prescription for moderate and severe ARS in our study was not very common. Only a third of the GPs in our study considered prescribing corticosteroids in moderate or severe ARS. We would like to see a higher prescription rate for the treatment of moderate and severe ARS. In the Dutch College of General Practitioners and the EPOS guidelines, immediate referral is recommended in the presence of alarming symptoms such as periorbital oedema, displaced globe, double vision, ophthalmoplegia, reduced visual acuity, severe unilateral or bilateral headache, frontal swelling, signs of meningitis or focal neurological signs.2,4 It is worrying that 12.2% of the differentiating GPs do not refer immediately. Patients can still die of complications of ARS.28 According to the Dutch College of General Practitioners, referral should be considered when there is an abnormal disease course that does not respond to treatment or does not respond sufficiently.4 EPOS suggests considering referral when there is no improvement after 14 days of treatment in moderate ARS. In severe ARS cases, GPs should refer if there is no improvement in 48 hours.2 In the general practices studied, only 6% of the GPs referred patients with moderate ARS in accordance with the EPOS recommendations. In our study, more than half of the GPs arranged a plain X-ray in CRS cases. The sensitivity of plain film radiography when detecting sinus opacification is unacceptably low for the ethmoid, frontal and sphenoid sinuses compared to a CT scan.29 Especially in chronic rhinosinusitis where mucosal thickening alone may be present the drawback of overlapping structures makes evaluation of the osteomeatal complex, anterior ethmoid sinus, middle meatus and sphenoid sinus limited.30 Plain X-rays are therefore not advisable for CRS. For the treatment of CRS, EPOS advises GPs to prescribe nasal steroids, to advise nasal douching, and to prescribe antihistamines if the patient is allergic.2 In this study, in CRS, the prescribing rate for nasal steroids is rather high (88.6%). Patients with CRS are referred to a specialist as recommended in EPOS (after four weeks of treatment without improvement) by 60.8% of the differentiating GPs.2 EPOS advises the re-evaluation of CRS after 4 weeks2 and 38.7% of the GPs report doing this. The study questionnaire asks GPs what they say they do, but does not check what they actually do. In an earlier study we studied morbidity registrations used by Dutch GPs; we found that 91% of the GPs prescribed medication, 3% referred to a specialist and 8% applied for radiology.20 In conclusion, GPs do not seem to differentiate between
ARS and CRS in the way described in EPOS. Their management of rhinosinusitis is not very consistent. It would be interesting to find out whether patients with rhinosinusitis benefit more from compliance with the EPOS guideline than when GPs make their own decisions about the choice of treatment. We are therefore planning to conduct a randomised study to compare outcomes in patients with ARS presenting to general practice. If compliance with the EPOS guideline proves more effective in treating rhinosinusitis, changes may be required to the Dutch College of General Practitioners guideline.
Conflict of interest declarations
There are no conflicts of interest.
334(7589):358-361. 2. 3.
nasal polyps 2007. Rhinol Suppl 2007;(20):1-136. Rosenfeld RM, Andes D, Bhattacharyya N, et al. Clinical practice guideline: adult sinusitis. Otolaryngol Head Neck Surg 2007;137(3 Suppl):S1-31.
ht P
rig
op y
rim R a ep ry ro C du ar ct e R io e n sp pr ir oh at ib ory ite S d o
4. 48:615-24. 5. 6. 7. 9. general practice.
http://dx.doi.org/10.1016/j.otohns.2007.06.726
De Sutter A, Burgers JS, De Bock GH, et al. [Dutch College of General Practitioners practice guideline rhinosinusitis]. Huisarts en Wetenschap 2005;
Akkerman AE, Kuyvenhoven MM, Verheij TJ, van DL. Antibiotics in Dutch general practice: nationwide electronic GP database and national reimbursement rates. Pharmacoepidemiol Drug Saf 2008;17(4):378-83. and urinary tract disorders and consistency among GPs. J Antimicrob Chemother 2008;62(3):587-92. http://dx.doi.org/10.1093/jac/dkn230 Akkerman AE, van der Wouden JC, Kuyvenhoven MM, Dieleman JP, Verheij TJ. Antibiotic prescribing for respiratory tract infections in Dutch primary care in relation to patient age and clinical entities. J Antimicrob Chemother 2004; 54(6):1116-21. http://dx.doi.org/10.1093/jac/dkh480
Ong DS, Kuyvenhoven MM, van DL, Verheij TJ. Antibiotics for respiratory, ear
8. Akkerman AE, Kuyvenhoven MM, van der Wouden JC, Verheij TJ. Prescribing antibiotics for respiratory tract infections by GPs: management and prescriber characteristics. Br J Gen Pract 2005;55(511):114-18. Akkerman AE, Kuyvenhoven MM, van der Wouden JC, Verheij TJ. Determinants of antibiotic overprescribing in respiratory tract infections in J Antimicrob Chemother 2005;56(5):930-6. http://dx.doi.org/10.1093/jac/dki283 10. Ashworth M, Latinovic R, Charlton J, Cox K, Rowlands G, Gulliford M. Why has antibiotic prescribing for respiratory illness declined in primary care? A longitudinal study using the General Practice Research Database. J Public Health (Oxf) 2004;26(3):268-74. http://dx.doi.org/10.1093/pubmed/fdh160 11. Ashworth M, Charlton J, Ballard K, Latinovic R, Gulliford M. Variations in antibiotic prescribing and consultation rates for acute respiratory infection in UK general practices 1995-2000. Br J Gen Pract 2005;55(517):603-08. 12. Ferech M, Coenen S, Malhotra-Kumar S, et al. European Surveillance of Antimicrobial Consumption (ESAC): outpatient quinolone use in Europe. J Antimicrob Chemother 2006;58(2):423-7. http://dx.doi.org/10.1093/jac/dkl183 13. Goossens H, Ferech M, Vander SR, Elseviers M. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet 2005;365(9459):579-87. 14. Goossens H, Ferech M, Coenen S, Stephens P. Comparison of outpatient systemic antibacterial use in 2004 in the United States and 27 European
PRIMARY CARE RESPIRATORY JOURNAL www.thepcrj.org
69
http://www.thepcrj.org
ci et
Fokkens W, Lund V, Mullol J. European position paper on rhinosinusitis and
1.
Ah-See KW, Evans AS. Sinusitis and its management. BMJ 2007;
References
Copyright PCRS-UK - reproduction prohibited
R Hoffmans et al.
countries. Clin Infect Dis 2007;44(8):1091-5. http://dx.doi.org/10.1086/512810 15. Barlan IB, Erkan E, Bakir M, Berrak S, Basaran MM. Intranasal budesonide spray as an adjunct to oral antibiotic therapy for acute sinusitis in children. Ann Allergy Asthma Immunol 1997;78(6):598-601. http://dx.doi.org/10.1016/ S1081-1206(10)63223-1 16. Bachert C, Meltzer EO. Effect of mometasone furoate nasal spray on quality of life of patients with acute rhinosinusitis. Rhinology 2007;45(3):190-6. 17. Dolor RJ, Witsell DL, Hellkamp AS, Williams JW, Jr., Califf RM, Simel DL. Comparison of cefuroxime with or without intranasal fluticasone for the treatment of rhinosinusitis. The CAFFS Trial: a randomized controlled trial. JAMA 2001;286(24):3097-3105. 18. Meltzer EO, Bachert C, Staudinger H. Treating acute rhinosinusitis: comparing efficacy and safety of mometasone furoate nasal spray, amoxicillin, and placebo. J Allergy Clin Immunol 2005;116(6):1289-1295. http://dx.doi.org/10.1016/j.jaci.2005.08.044 19. Lund VJ, Black JH, Szabo LZ, Schrewelius C, Akerlund A. Efficacy and tolerability of budesonide aqueous nasal spray in chronic rhinosinusitis patients. Rhinology 2004;42(2):57-62. 20. Hoffmans R, Schermer T, van der Linde K, van Weel C, Fokkens W. Chronic Rhinosinusitis is not recognized by Dutch General Practitioners; A study based on morbidity registrations. 2009. Ref Type: Unpublished Work 21. Hingstman L, Kenens RJ. Cijfers uit de registratie van huisartsen - Peiling 2008, NIVEL 2008. 2008. Ref Type: Report 22. Nederlandse Vereniging voor KNO-heelkunde en Heelkunde van het Hoofd11-2007. Ref Type: Unpublished Work
23. van Buchem FL, Knottnerus JA, Schrijnemaekers VJ, Peeters MF. Primary-carebased randomised placebo-controlled trial of antibiotic treatment in acute maxillary sinusitis. Lancet 1997;349(9053):683-687. http://dx.doi.org/10.1016/ S0140-6736(96)07585-X 24. Snow V, Mottur-Pilson C, Hickner JM. Principles of appropriate antibiotic use for acute sinusitis in adults. Ann Intern Med 2001;134(6):495-7. 25. Stalman W, van Essen GA, van der Graaf Y, de Melker RA. The end of antibiotic treatment in adults with acute sinusitis-like complaints in general practice? A placebo-controlled double-blind randomized doxycycline trial. Br J Gen Pract 1997;47(425):794-9. 26. Young J, De SA, Merenstein D, et al. Antibiotics for adults with clinically diagnosed acute rhinosinusitis: a meta-analysis of individual patient data. Lancet 2008; 371(9616):908-14. http://dx.doi.org/10.1016/S01406736(08)60416-X 27. Jacobs MR, Felmingham D, Appelbaum PC, Gruneberg RN. The Alexander Project 1998-2000: susceptibility of pathogens isolated from community-acquired respiratory tract infection to commonly used antimicrobial agents. J Antimicrob 28. Bayonne E, Kania R, Tran P, Huy B, Herman P. Intracranial complications of Chemother 2003;52(2):229-46. http://dx.doi.org/10.1093/jac/dkg321 rhinosinusitis. A review, typical imaging data and algorithm of management. 29. Aalokken TM, Hagtvedt T, Dalen I, Kolbenstvedt A. Conventional sinus radiography compared with CT in the diagnosis of acute sinusitis. Dentomaxillofac Radiol 2003;32(1):60-2. http://dx.doi.org/10.1259/dmfr/65139094 188(2):303-14.
Halsgebied. Conceptrichtlijn Chronische Rhinosinusitis en Neuspoliepen. 26-
Available online at http://www.thepcrj.org
PRIMARY CARE RESPIRATORY JOURNAL www.thepcrj.org
op y
rig
ht P
rim R a ep ry ro C du ar ct e R io e n sp pr ir oh at ib ory ite S d o
70
30. Yousem DM. Imaging of sinonasal inflammatory disease. Radiology 1993;
http://www.thepcrj.org
ci et
Rhinology 2009;47(1):59-65.
Copyright PCRS-UK - reproduction prohibited
R Hoffmans et al.
Questionnaire: Management of rhinosinusitis in general general Appendix A. Questionnaire: Management of rhinosinusitis inpractice practice.
1. How long have you been practicing as a general practitioner? < 5 years 5-10 years 10-15 years 15-20 years 20-25 years 25 years 2. In what kind of practice do you work? Solo practice Duo practice Group practice 3. In which age group are you? < 30 years 30-34 years 35-39 years 40-44 years 45-49 years 50-54 years 55-59 years 60-64 years 65 years
4. From which duration of complaints would/do you speak of chronic rhinosinusitis? 1 week 4 weeks 12 weeks Half a year 1 year
6. Do you differentiate between acute and chronic complaints in your treatment of rhinosinusitis? NO YES
op y
rig
ht P
5. Do you differentiate between mild, moderate and severe complaints in your treatment of rhinosinusitis? YES NO
IF YOU ANSWERED THE
PINK QUESTIONNAIRE.
QUESTION 6 WITH YES
QUESTION 6
WITH
rim R a ep ry ro C du ar ct e R io e n sp pr ir oh at ib ory ite S d o
IF YOU ANSWERED
THE YELLOW QUESTIONNAIRE.
NO
PRIMARY CARE RESPIRATORY JOURNAL www.thepcrj.org
http://www.thepcrj.org
ci et
PLEASE FILL OUT PLEASE FILL OUT
Copyright PCRS-UK - reproduction prohibited
Management of rhinosinusitis in Dutch general practice
Questionnaire: Management of rhinosinusitis in general practice Appendix A. Questionnaire: Management of rhinosinusitis in general practice continued.
YOU DO DISCRIMINATE BETWEEN ACUTE AND CHRONIC RHINOSINUSITIS The next questions are about acute rhinosinusitis. 1. What percentage of your total patients has had a diagnosis of acute rhinosinusitis during the past 12 months? (choose one) <2% 2-5% 6-10% 11-19% 20% or more 2. Do you agree with the following statement? For acute rhinosinusitis it is not recommended to take radiologic investigations. Agree Disagree, I usually request: Plain X-ray , CT , Echo , others _____________(specify please) aan. Disagree, as I request CT scan only, in cases of patients with additional problems such as very severe, immuno-compromised patients with signs of complications. 3. In general, do you treat acute rhinosinusitis patients with symptoms less than 5 days? NO YES If YES, then what is you typical treatment plan? (check all that apply)
_________________________________________________________
op y
Please specify the name, dosage and duration of antibiotics you have commonly used:
rig
ht P
If you answer yes more than once, please rank order each treatment (1=most often, 10=least often) Yes Numbering (1-10) ____ a. Painkillers ____ b. Antibiotics (penicillin / amoxicillin-clavulanate / broad spectrum antibiotics)
rim R a ep ry ro C du ar ct e R io e n sp pr ir oh at ib ory ite S d o
Yes
ci et
c. d. e. f. g. h. i. j. k. l.
Topical antibiotics Systemic steroids Nasal steroids Oral antihistamine Decongestants Nasal douche Steaming Mucolytics Herbal medicine Others (specify) _____________
Numbering ____ ____ ____ ____ ____ ____ ____ ____ ____ ____
(1-10)
PRIMARY CARE RESPIRATORY JOURNAL www.thepcrj.org
http://www.thepcrj.org
Copyright PCRS-UK - reproduction prohibited
R Hoffmans et al.
Appendix A. Questionnaire: Management of rhinosinusitis in general practice continued.
Questionnaire: Management of rhinosinusitis in general practice
4. In general, do you treat patients with acute rhinosinusitis with moderate symptoms (no fever, no NEE severe pain) which persist for more than 5 days? JA If YES, then what is you typical treatment plan? (check all that apply) If you answer yes more than once, please rank order each treatment (1=most often, 10=least often) Yes Numbering (1-10) ____ a. Painkillers ____ b. Antibiotics (penicillin / amoxicillin-clavulanate / broad spectrum antibiotics)
Please specify the name, dosage and duration of antibiotics you have commonly used:
_________________________________________________________ Yes c. d. e. f. g. h. i. j. k. l. Topical antibiotics Systemic steroids Nasal steroids Oral antihistamine Decongestants Nasal douche Steaming Mucolytics Herbal medicine Others (specify) _____________ Numbering ____ ____ ____ ____ ____ ____ ____ ____ ____ ____
K
(1-10) 5. In general, do you treat patients with acute rhinosinusitis with severe symptoms (with fever NEE >38C or severe pain)? JA If YES, then what is you typical treatment plan? (check all that apply) If you answer yes more than once, please rank order each treatment (1=most often, 10=least often) Yes Numbering (1-10) ____ a. Painkillers ____ b. Antibiotics (penicillin / amoxicillin-clavulanate / broad spectrum antibiotics)
Please specify the name, dosage and duration of antibiotics you have commonly used:
_________________________________________________________ Yes c. d. e. f. g. h. i. j. k. l. Topical antibiotics Systemic steroids Nasal steroids Oral antihistamine Decongestants Nasal douche Steaming Mucolytics Herbal medicine Others (specify) _____________ Numbering ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ (1-10)
PRIMARY CARE RESPIRATORY JOURNAL www.thepcrj.org
op y
rig
ht P
rim R a ep ry ro C du ar ct e R io e n sp pr ir oh at ib ory ite S d o
http://www.thepcrj.org
ci et
Copyright PCRS-UK - reproduction prohibited
Management of rhinosinusitis in Dutch general practice
Appendix A. Questionnaire: Management of rhinosinusitis in general practice continued.
Questionnaire: Management of rhinosinusitis in general practice
6. What criteria do you typically use for referring each of the following types of acute rhinosinusitis patients to an ENT specialist? a. Patients with moderate symptoms (choose one) Always refer them to a specialist right after diagnosis When no improvement occurs after 14 days of treatment When no improvement occurs after 4 weeks of treatment After one course of antibiotic treatment which did not work After 48 hours with no effect of intranasal corticosteroids and/or antibiotics Never refer them to a specialist Other (specify):__________________________________________ b. Patients with severe symptoms (fever,pain) (choose one) Always refer them to a specialist right after diagnosis When no improvement occurs after 14 days of treatment When no improvement occurs after 4 weeks of treatment After one course of antibiotic treatment which did not work After 48 hours with no effect of intranasal corticosteroids and/or antibiotics Never refer them to a specialist Other (specify):__________________________________________
c. Patients with ocular or neurological complications (choose one) Always refer them to a specialist right after diagnosis When no improvement occurs after 14 days of treatment When no improvement occurs after 4 weeks of treatment After one course of antibiotic treatment which did not work After 48 hours with no effect of intranasal corticosteroids and/or antibiotics Never refer them to a specialist Other (specify):__________________________________________ The next questions are about chronic rhinosinusitis.
<2% 2-5% 6-10% 11-19% 20% or more
8. Do you agree with the following statement? For chronic rhinosinusitis it is not recommended to take radiologic investigations. Agree Disagree, I usually request: Plain X-ray , CT , Echo , others _____________(specify please) aan. Disagree, as I request CT scan only, in cases of patients with additional problems such as very severe, immuno-compromised patients with signs of complications.
PRIMARY CARE RESPIRATORY JOURNAL www.thepcrj.org
op y
7. What percentage of your total patients has had a diagnosis of chronic rhinosinusitis during the past 12 months? (choose one)
rig
ht P
rim R a ep ry ro C du ar ct e R io e n sp pr ir oh at ib ory ite S d o
http://www.thepcrj.org
ci et
Copyright PCRS-UK - reproduction prohibited
R Hoffmans et al.
Questionnaire: Management of rhinosinusitis in general in general Appendix A. Questionnaire: Management of rhinosinusitis practice practice continued.
9. In general, do you treat patients with chronic rhinosinusitis? YES If YES, then what is you typical treatment plan? (check all that apply) If you answer yes more than once, please rank order each treatment (1=most often, 10=least often) Yes Numbering (1-10) ____ a. Painkillers ____ b. Antibiotics (penicillin / amoxicillin-clavulanate / broad spectrum antibiotics)
NO
Please specify the name, dosage and duration of antibiotics you have commonly used:
Yes c. d. e. f. g. h. i. j. k. l. Topical antibiotics Systemic steroids Nasal steroids Oral antihistamine Decongestants Nasal douche Steaming Mucolytics Herbal medicine Others (specify) _____________ Numbering ____ ____ ____ ____ ____ ____ ____ ____ ____ ____
K y
(1-10)
_________________________________________________________
10. After which duration of treatment do you reassess the complaints of a patient with chronic rhinosinusitits? After 48 hours After 14 days After 4 weeks After 12 weeks
Always refer them to a specialist right after diagnosis When no improvement occurs after 14 days of treatment When no improvement occurs after 4 weeks of treatment After one course of antibiotic treatment which did not work After 48 hours with no effect of intranasal corticosteroids and/or antibiotics Never refer them to a specialist Other (specify):__________________________________________ 12. Can we call you for an interview by telephone with 3 cases. This will take approximately NO 20 minutes. YES Telephone: _______________________________ Thank you very much for you cooperation in this survey!
PRIMARY CARE RESPIRATORY JOURNAL www.thepcrj.org
11. What criteria do you typically use for referring chronic rhinosinusitis patients to an ENT specialist?
op y
rig
ht P
rim R a ep ry ro C du ar ct e R io e n sp pr ir oh at ib ory ite S d o
http://www.thepcrj.org
ci et
Copyright PCRS-UK - reproduction prohibited
Management of rhinosinusitis in Dutch general practice
Questionnaire: Management of rhinosinusitis in general general Appendix A. Questionnaire: Management of rhinosinusitis in practice practice continued.
YOU NOT DISCRIMINATE BETWEEN ACUTE AND CHRONIC RHINOSINUSITIS 1. What percentage of your total patients has had a diagnosis of rhinosinusitis during the past 12 months? (choose one) <2% 2-5% 6-10% 11-19% 20% or more 2. Do you agree with the following statement? For rhinosinusitis it is not recommended to take radiologic investigations. Agree Disagree, I usually request: Plain X-ray , CT , Echo , others _____________(specify please) aan. Disagree, as I request CT scan only, in cases of patients with additional problems such as very severe, immuno-compromised patients with signs of complications.
3. In general, do you treat patients with rhinosinusitis with symptoms for less than 5 days? NO YES If YES, then what is you typical treatment plan? (check all that apply)
_________________________________________________________
op y
rig
Please specify the name, dosage and duration of antibiotics you have commonly used:
Yes Numbering ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ (1-10)
c. d. e. f. g. h. i. j. k. l.
Topical antibiotics Systemic steroids Nasal steroids Oral antihistamine Decongestants Nasal douche Steaming Mucolytics Herbal medicine Others (specify) _____________
PRIMARY CARE RESPIRATORY JOURNAL www.thepcrj.org
ht P
If you answer yes more than once, please rank order each treatment (1=most often, 10=least often) Yes Numbering (1-10) ____ a. Painkillers ____ b. Antibiotics (penicillin / amoxicillin-clavulanate / broad spectrum antibiotics)
rim R a ep ry ro C du ar ct e R io e n sp pr ir oh at ib ory ite S d o
http://www.thepcrj.org
ci et
Copyright PCRS-UK - reproduction prohibited
R Hoffmans et al.
Questionnaire: Management of rhinosinusitis in general in general Appendix A. Questionnaire: Management of rhinosinusitis practice practice continued.
4. In general, do you treat patients with rhinosinusitis with moderate symptoms (no fever, no NO severe pain) which persist more than 5 days? YES If YES, then what is you typical treatment plan? (check all that apply) If you answer yes more than once, please rank order each treatment (1=most often, 10=least often) Yes Numbering (1-10) ____ a. Painkillers ____ b. Antibiotics (penicillin / amoxicillin-clavulanate / broad spectrum antibiotics)
Please specify the name, dosage and duration of antibiotics you have commonly used:
_________________________________________________________ Yes c. d. e. f. g. h. i. j. k. l. Topical antibiotics Systemic steroids Nasal steroids Oral antihistamine Decongestants Nasal douche Steaming Mucolytics Herbal medicine Others (specify) _____________ Numbering ____ ____ ____ ____ ____ ____ ____ ____ ____ ____
K
(1-10) 5. In general, do you treat patients with rhinosinusitis with severe symptoms (with fever >38C o severe pain)? YES NO If YES, then what is you typical treatment plan? (check all that apply) If you answer yes more than once, please rank order each treatment (1=most often, 10=least often) Yes Numbering (1-10) ____ a. Painkillers ____ b. Antibiotics (penicillin / amoxicillin-clavulanate / broad spectrum antibiotics)
Please specify the name, dosage and duration of antibiotics you have commonly used:
_________________________________________________________ Yes c. d. e. f. g. h. i. j. k. l. Topical antibiotics Systemic steroids Nasal steroids Oral antihistamine Decongestants Nasal douche Steaming Mucolytics Herbal medicine Others (specify) _____________ Numbering ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ (1-10)
PRIMARY CARE RESPIRATORY JOURNAL www.thepcrj.org
op y
rig
ht P
rim R a ep ry ro C du ar ct e R io e n sp pr ir oh at ib ory ite S d o
http://www.thepcrj.org
ci et
Copyright PCRS-UK - reproduction prohibited
Management of rhinosinusitis in Dutch general practice
Questionnaire: Management of rhinosinusitis in general practice
Appendix A. Questionnaire: Management of rhinosinusitis in general practice continued.
6. What criteria do you typically use for referring each of the following types of rhinosinusitis patients to an ENT specialist? a. Patients with moderate symptoms (choose one) Always refer them to a specialist right after diagnosis When no improvement occurs after 14 days of treatment When no improvement occurs after 4 weeks of treatment After one course of antibiotic treatment which did not work After 48 hours with no effect of intranasal corticosteroids and/or antibiotics Never refer them to a specialist Other (specify):__________________________________________ b. Patients with severe symptoms (fever,pain) (choose one) Always refer them to a specialist right after diagnosis When no improvement occurs after 14 days of treatment When no improvement occurs after 4 weeks of treatment After one course of antibiotic treatment which did not work After 48 hours with no effect of intranasal corticosteroids and/or antibiotics Never refer them to a specialist Other (specify):__________________________________________
c. Patients with ocular or neurological complications (choose one) Always refer them to a specialist right after diagnosis When no improvement occurs after 14 days of treatment When no improvement occurs after 4 weeks of treatment After one course of antibiotic treatment which did not work After 48 hours with no effect of intranasal corticosteroids and/or antibiotics Never refer them to a specialist Other (specify):__________________________________________ 7. Can we call you for an interview by telephone with 3 cases. This will take approximately NO 20 minutes. YES Telephone: _______________________________ Thank you very much for you cooperation in this survey!
PRIMARY CARE RESPIRATORY JOURNAL www.thepcrj.org
op y
rig
ht P
rim R a ep ry ro C du ar ct e R io e n sp pr ir oh at ib ory ite S d o
http://www.thepcrj.org
ci et
You might also like
- Diagnosis and Treatment of Chronic CoughFrom EverandDiagnosis and Treatment of Chronic CoughSang Heon ChoNo ratings yet
- Lary 26606Document6 pagesLary 26606raghad.bassalNo ratings yet
- Essentials in Lung TransplantationFrom EverandEssentials in Lung TransplantationAllan R. GlanvilleNo ratings yet
- Efficacy of Steroidal Vs Non-Steroidal Agents in Oral Lichen Planus: A Randomised, Open-Label StudyDocument9 pagesEfficacy of Steroidal Vs Non-Steroidal Agents in Oral Lichen Planus: A Randomised, Open-Label StudyRetno ManggalihNo ratings yet
- Lack of Efficacy of Long-Term, Low-Dose Azithromycin in Chronic Rhinosinusitis: A Randomized Controlled TrialDocument12 pagesLack of Efficacy of Long-Term, Low-Dose Azithromycin in Chronic Rhinosinusitis: A Randomized Controlled Trialpaijo09No ratings yet
- Chronic Rhinosinusitis SteroidDocument9 pagesChronic Rhinosinusitis SteroidHan's ChristianNo ratings yet
- Clinical Medicine Insights: Ear, Nose, ThroatDocument5 pagesClinical Medicine Insights: Ear, Nose, ThroatagustinadianasariaguNo ratings yet
- Alifiani-Jurding SNNTDocument9 pagesAlifiani-Jurding SNNTYAHYA Al-HILALNo ratings yet
- Joc 41159Document6 pagesJoc 41159Latansa DinaNo ratings yet
- Treatment of Chronic Rhinosinusitis and Its Effects On AsthmaDocument7 pagesTreatment of Chronic Rhinosinusitis and Its Effects On AsthmaHalilGutajNo ratings yet
- Slide THTDocument15 pagesSlide THTmenthariNo ratings yet
- Treatment Trends in Allergic Rhinitis and Asthma: A British ENT SurveyDocument5 pagesTreatment Trends in Allergic Rhinitis and Asthma: A British ENT SurveymenthariNo ratings yet
- The Global Epidemiology of Chronic Cough in Adults: A Systematic Review and Meta-AnalysisDocument3 pagesThe Global Epidemiology of Chronic Cough in Adults: A Systematic Review and Meta-AnalysisUmmul HayatiNo ratings yet
- Jurnal THTDocument7 pagesJurnal THTFenti FatonahNo ratings yet
- Norlin JM Et Al 2017. Real World Outcomes in 2646 Psoriasis Patients One in Five Has PASI 10 and or DLQI 10 Under Ongoing Systemic TherapyDocument6 pagesNorlin JM Et Al 2017. Real World Outcomes in 2646 Psoriasis Patients One in Five Has PASI 10 and or DLQI 10 Under Ongoing Systemic TherapyAndi MarsaliNo ratings yet
- Treatment Trends in Allergic Rhinitis and Asthma: A British ENT SurveyDocument5 pagesTreatment Trends in Allergic Rhinitis and Asthma: A British ENT SurveyAndra LaszloNo ratings yet
- 30 37Document8 pages30 37Sri HariNo ratings yet
- Research: Corticosteroids For Pain Relief in Sore Throat: Systematic Review and Meta-AnalysisDocument7 pagesResearch: Corticosteroids For Pain Relief in Sore Throat: Systematic Review and Meta-AnalysiswindaintanpNo ratings yet
- Do NotDocument8 pagesDo NotAkhmad AfriantoNo ratings yet
- COPD ProposalDocument8 pagesCOPD Proposalpharmacist2008No ratings yet
- The Besmart (Best Supportive Management For Adults Referred With Tonsillopharyngitis) Multicentre Observational StudyDocument6 pagesThe Besmart (Best Supportive Management For Adults Referred With Tonsillopharyngitis) Multicentre Observational StudyArizkamhNo ratings yet
- Van Der Veen J., Seys S.F., Levie P., Jorissen M, Fokkens W.J., Hellings P.WDocument21 pagesVan Der Veen J., Seys S.F., Levie P., Jorissen M, Fokkens W.J., Hellings P.WLee제노No ratings yet
- Role of Corticosteroids in Functional Endoscopic Sinus Surgery A Systematic Review and Meta Analysis AcceptedDocument39 pagesRole of Corticosteroids in Functional Endoscopic Sinus Surgery A Systematic Review and Meta Analysis AcceptedTIkaNo ratings yet
- Parkinson TerapiaDocument13 pagesParkinson TerapiaIsabela FiuzaNo ratings yet
- Complications of Acute Rhinosinusitis in The Netherlands: F S Hansen, R Hoffmans, C Georgalas and W J FokkensDocument7 pagesComplications of Acute Rhinosinusitis in The Netherlands: F S Hansen, R Hoffmans, C Georgalas and W J Fokkenspanji satryo utomoNo ratings yet
- Intranasal Corticosteroids in Management of Acute Sinusitis: A Systematic Review and Meta-AnalysisDocument9 pagesIntranasal Corticosteroids in Management of Acute Sinusitis: A Systematic Review and Meta-AnalysisagustinadianasariaguNo ratings yet
- Antibiotics For Recurrent Acute Pharyngo-Tonsillitis Systematic Review 2018 PDFDocument10 pagesAntibiotics For Recurrent Acute Pharyngo-Tonsillitis Systematic Review 2018 PDFNoca AriantiNo ratings yet
- Print 1Document8 pagesPrint 1Zaura Meliana MulyadiNo ratings yet
- Common Cold and Acute Rhinosinusitis: Up-to-Date Management in 2020Document10 pagesCommon Cold and Acute Rhinosinusitis: Up-to-Date Management in 2020Shanaz KanandaNo ratings yet
- Chemotherapy of Tuberculosis in Hong KongDocument17 pagesChemotherapy of Tuberculosis in Hong KongChris LeeNo ratings yet
- L4. T2.M2 y M6. Predictive Factors For Induction of Remission in Patients With Active ARDocument5 pagesL4. T2.M2 y M6. Predictive Factors For Induction of Remission in Patients With Active ARJhon Andy RamosNo ratings yet
- 671 - Rhinosinusitis and Nasal Polyps (CompleteDocument89 pages671 - Rhinosinusitis and Nasal Polyps (CompleteAprilla Handayani100% (1)
- The Incidence and Prevalence of Systemic Lupus Erythematosus in The UK, 1999 - 2012Document6 pagesThe Incidence and Prevalence of Systemic Lupus Erythematosus in The UK, 1999 - 2012Bagus MahendraNo ratings yet
- Guia - 4209 Guia Rinitis AlergicaDocument16 pagesGuia - 4209 Guia Rinitis AlergicaJesus Manuel Armenta VelderrainNo ratings yet
- (Acta Pharmaceutica) Medication Adherence and Health-Related Quality of Life Among Patients With Chronic Obstructive Pulmonary DiseaseDocument9 pages(Acta Pharmaceutica) Medication Adherence and Health-Related Quality of Life Among Patients With Chronic Obstructive Pulmonary DiseaseAlexandrahautaNo ratings yet
- Antibiotics 02 00001Document10 pagesAntibiotics 02 00001Jenny AlmagroNo ratings yet
- Jurnal Respirasi PDFDocument14 pagesJurnal Respirasi PDFakhirul_733759154No ratings yet
- RCT Phenotypic Chronic RhinosinusitisDocument11 pagesRCT Phenotypic Chronic RhinosinusitisAyuNo ratings yet
- Xerostomia and Salivary Flow in Patients Taking Antihypertensive DrugsDocument16 pagesXerostomia and Salivary Flow in Patients Taking Antihypertensive DrugsdeboraNo ratings yet
- Bukan jurnal-TreatmentMaxillarySinusitis2014FebDocument1 pageBukan jurnal-TreatmentMaxillarySinusitis2014FebagustinadianasariaguNo ratings yet
- Sinusistis JAMA 2015Document14 pagesSinusistis JAMA 2015IvanCarrilloNo ratings yet
- Polipos y Macrolidos 2Document3 pagesPolipos y Macrolidos 2Jose Luis GonzalezNo ratings yet
- Nasal Smear Eosinophilia For The Diagnosis of Allergic Rhinitis and Eosinophilic Non Allergic RhinitisDocument7 pagesNasal Smear Eosinophilia For The Diagnosis of Allergic Rhinitis and Eosinophilic Non Allergic RhinitisAJITH KUMARNo ratings yet
- Art:10.1186/s13063 016 1456 4Document10 pagesArt:10.1186/s13063 016 1456 4dani yan sNo ratings yet
- Pablos Mendez Et Al 1998 Global Surveillance For TB DRDocument9 pagesPablos Mendez Et Al 1998 Global Surveillance For TB DRashakow8849No ratings yet
- Hospital Aquired Pneumonia - FullDocument26 pagesHospital Aquired Pneumonia - FullSuvad Dedic100% (1)
- Stopp StartDocument11 pagesStopp StartHUONGNo ratings yet
- Paediatric Pneumonia 2016 - 17Document13 pagesPaediatric Pneumonia 2016 - 17JENNY MARGOT HIDALGO QUISPENo ratings yet
- Chapter 7-Atopic Children and Use of Prescribed MeDocument20 pagesChapter 7-Atopic Children and Use of Prescribed MeKuan ChunNo ratings yet
- Polypharmacy in Patients Hospitalised For Acute Exacerbation of COPDDocument4 pagesPolypharmacy in Patients Hospitalised For Acute Exacerbation of COPDpina distefanoNo ratings yet
- Acute Sinusitis and Sore Throat in Primary Care: Chris Del MarDocument3 pagesAcute Sinusitis and Sore Throat in Primary Care: Chris Del MarRhahima SyafrilNo ratings yet
- Prediction of Post-Tuberculosis Lung Function ImpairmentDocument12 pagesPrediction of Post-Tuberculosis Lung Function ImpairmentputriargathyaNo ratings yet
- CMJ 130 943Document7 pagesCMJ 130 943Stella SunurNo ratings yet
- Phenytoininduced DRESSDocument4 pagesPhenytoininduced DRESSCamille MalilayNo ratings yet
- Clinical Management of Asthma in 1999: The Asthma Insights and Reality in Europe (AIRE) StudyDocument6 pagesClinical Management of Asthma in 1999: The Asthma Insights and Reality in Europe (AIRE) StudyarunvklplmNo ratings yet
- Allergen Immunotherapy Expert ExchangeDocument4 pagesAllergen Immunotherapy Expert ExchangeAnna LiachenkoNo ratings yet
- Quality of Life After Functional Endoscopic Sinus Surgery in Patients With Chronic RhinosinusitisDocument15 pagesQuality of Life After Functional Endoscopic Sinus Surgery in Patients With Chronic RhinosinusitisNarendraNo ratings yet
- Devil Lier 2018Document26 pagesDevil Lier 2018risanataliasiburianNo ratings yet
- Azithromycin For Prevention of Exacerbations of COPDDocument10 pagesAzithromycin For Prevention of Exacerbations of COPDAJNo ratings yet
- Yasmeen 2020Document16 pagesYasmeen 2020Rafaela Queiroz MascarenhasNo ratings yet
- 2011 OctoberDocument11 pages2011 OctoberMohamed Rikarz Ahamed RikarzNo ratings yet
- Dengue 208Document3 pagesDengue 208Mohamed Rikarz Ahamed RikarzNo ratings yet
- Hypoxemic Respiratory FailureDocument70 pagesHypoxemic Respiratory FailureMohamed Rikarz Ahamed RikarzNo ratings yet
- Hemodynamic Changes in Hypotensive Shock: Lcs LumDocument2 pagesHemodynamic Changes in Hypotensive Shock: Lcs LumMohamed Rikarz Ahamed RikarzNo ratings yet
- 12 Kasper Notes 2020 OphthalmologyDocument33 pages12 Kasper Notes 2020 OphthalmologyMohamed Rikarz Ahamed RikarzNo ratings yet
- 643 PDFDocument1 page643 PDFMohamed Rikarz Ahamed RikarzNo ratings yet
- Rheumatology Notes For ReadingDocument8 pagesRheumatology Notes For ReadingMohamed Rikarz Ahamed RikarzNo ratings yet
- 642Document1 page642Mohamed Rikarz Ahamed RikarzNo ratings yet
- 640Document1 page640Mohamed Rikarz Ahamed RikarzNo ratings yet
- Dengue 201Document6 pagesDengue 201Mohamed Rikarz Ahamed RikarzNo ratings yet
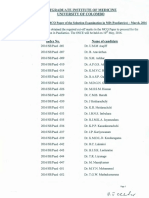
- Results of The Selection Examination in Surgery - .January/February, 2017Document1 pageResults of The Selection Examination in Surgery - .January/February, 2017Mohamed Rikarz Ahamed RikarzNo ratings yet
- Postgraduate Institute of Medicine University of Colombo: 2017/SEIMDIFM - 003Document1 pagePostgraduate Institute of Medicine University of Colombo: 2017/SEIMDIFM - 003Mohamed Rikarz Ahamed RikarzNo ratings yet
- Postgraduate Institute of Medicine University of Colombo: Results of The MD (Medicine) Examination-February/March, 2016Document2 pagesPostgraduate Institute of Medicine University of Colombo: Results of The MD (Medicine) Examination-February/March, 2016Mohamed Rikarz Ahamed RikarzNo ratings yet
- Counter Signed: ST THDocument1 pageCounter Signed: ST THMohamed Rikarz Ahamed RikarzNo ratings yet
- Postgraduate Nstitute of Med C E University of Colombo: LT S T III A Il, 2016Document1 pagePostgraduate Nstitute of Med C E University of Colombo: LT S T III A Il, 2016Mohamed Rikarz Ahamed RikarzNo ratings yet
- Answers To Questions For Volume 11, Number 4: The Surgical Approach To Postpartum HaemorrhageDocument6 pagesAnswers To Questions For Volume 11, Number 4: The Surgical Approach To Postpartum HaemorrhageMohamed Rikarz Ahamed RikarzNo ratings yet
- Postgraduate Institute of Medicine University of ColomboDocument1 pagePostgraduate Institute of Medicine University of ColomboMohamed Rikarz Ahamed RikarzNo ratings yet
- Checked Counter A: by byDocument1 pageChecked Counter A: by byMohamed Rikarz Ahamed RikarzNo ratings yet
- Check dBY - ... - .. By: Counter Signed Ak ExamintuionsDocument1 pageCheck dBY - ... - .. By: Counter Signed Ak ExamintuionsMohamed Rikarz Ahamed RikarzNo ratings yet
- Postgraduate Inst Tute of Medici E Universit of ColomboDocument1 pagePostgraduate Inst Tute of Medici E Universit of ColomboMohamed Rikarz Ahamed RikarzNo ratings yet
- Postg Aduate Institute of Medicine University FC LomboDocument1 pagePostg Aduate Institute of Medicine University FC LomboMohamed Rikarz Ahamed RikarzNo ratings yet
- Postgraduate Institute of Medicine University of ColomboDocument2 pagesPostgraduate Institute of Medicine University of ColomboMohamed Rikarz Ahamed RikarzNo ratings yet
- Postgraduate Institute of Medicine University of Colombo: Index No. Name of CandidateDocument2 pagesPostgraduate Institute of Medicine University of Colombo: Index No. Name of CandidateMohamed Rikarz Ahamed RikarzNo ratings yet
- Postgraduate Institute of Medicine University of ColomboDocument1 pagePostgraduate Institute of Medicine University of ColomboMohamed Rikarz Ahamed RikarzNo ratings yet
- 594 PDFDocument1 page594 PDFMohamed Rikarz Ahamed RikarzNo ratings yet
- Postgraduate Institute of Medicine University of ColomboDocument2 pagesPostgraduate Institute of Medicine University of ColomboMohamed Rikarz Ahamed RikarzNo ratings yet
- Postgraduate Institute of Medicine University of Colombo: (Provisional and SenateDocument1 pagePostgraduate Institute of Medicine University of Colombo: (Provisional and SenateMohamed Rikarz Ahamed RikarzNo ratings yet
- #3 Beydler-2017-AORN - JournalDocument7 pages#3 Beydler-2017-AORN - JournalMarina ENo ratings yet
- Ellie Suse ResumeDocument2 pagesEllie Suse Resumeapi-439303465No ratings yet
- IPED2015CS01 MAC049 PIS&ICF 4.0 Part A and B (18dec2018) - Final VersionDocument24 pagesIPED2015CS01 MAC049 PIS&ICF 4.0 Part A and B (18dec2018) - Final VersionASCRONo ratings yet
- Rheumatoid ArthritisDocument44 pagesRheumatoid ArthritisBulborea Mihaela100% (1)
- FdarDocument33 pagesFdarTatiana's Couture100% (2)
- Effects of Implementation of Focus-Pdca Model To Decrease Patients' Length of Stay in Emergency DepartmentDocument5 pagesEffects of Implementation of Focus-Pdca Model To Decrease Patients' Length of Stay in Emergency DepartmentMuhammad RamadhanNo ratings yet
- Mackenzie Renee Rotella CV FNP 2016Document2 pagesMackenzie Renee Rotella CV FNP 2016api-311611085No ratings yet
- A Study of Correlation Between Subjective Sensation of Nose Block and Objective Assessment of Nasal Patency by Cold Spatula Test in A Patient With Nose BlockDocument5 pagesA Study of Correlation Between Subjective Sensation of Nose Block and Objective Assessment of Nasal Patency by Cold Spatula Test in A Patient With Nose BlockElfa RiniNo ratings yet
- Uterine Anomaly, Fibroid Uterus, Ovarian Tumor, Uterine ProlapseDocument30 pagesUterine Anomaly, Fibroid Uterus, Ovarian Tumor, Uterine ProlapseVijith.V.kumar80% (5)
- SCIF1111 Notes For Susan Hardy First TestDocument5 pagesSCIF1111 Notes For Susan Hardy First TestOliverNo ratings yet
- Neuro Estructural Integracion Tecnica PDF en InglesDocument10 pagesNeuro Estructural Integracion Tecnica PDF en InglesLuulaa Minguin GarciaNo ratings yet
- 1452 A. Lacson St. Sta. Cruz, Manila College of Nursing: The Family Clinic, Inc. - CollegesDocument1 page1452 A. Lacson St. Sta. Cruz, Manila College of Nursing: The Family Clinic, Inc. - CollegesCatherine MetraNo ratings yet
- Clinical MCQ Questions Flashcards - Quizlet PDFDocument5 pagesClinical MCQ Questions Flashcards - Quizlet PDFed alkholidyNo ratings yet
- Counselling in Infertility Individual Couple and Group InterventionsDocument7 pagesCounselling in Infertility Individual Couple and Group InterventionsEliza Martin100% (1)
- Assessment Nursing Diagnosis Planning Implementation Rationale EvaluationDocument1 pageAssessment Nursing Diagnosis Planning Implementation Rationale EvaluationJames PajarilloNo ratings yet
- Short Term Training Curriculum Handbook PHLEBOTOMISTDocument33 pagesShort Term Training Curriculum Handbook PHLEBOTOMISTrokdeNo ratings yet
- Best Practices For Prospect Research in Healthcare Philanthropy - 2nd EditionDocument66 pagesBest Practices For Prospect Research in Healthcare Philanthropy - 2nd EditionPaul Jacob RobertsNo ratings yet
- List of English Speaking Doctors in BerlinDocument19 pagesList of English Speaking Doctors in BerlinAnggêr JamungNo ratings yet
- Outline of A Case Study ReportDocument5 pagesOutline of A Case Study ReportJedda Punzalan100% (1)
- Document PDFDocument12 pagesDocument PDFEviNo ratings yet
- ClubfootDocument1 pageClubfootBheru LalNo ratings yet
- Cipriani Et Al-2013-Cochrane Database of Systematic ReviewsDocument52 pagesCipriani Et Al-2013-Cochrane Database of Systematic ReviewsfiskaderishaNo ratings yet
- Adults GriefDocument8 pagesAdults GriefGuilherme RibeiroNo ratings yet
- Case Study # 3 UNRS 314 Name - Number - Ruptured AppendixDocument2 pagesCase Study # 3 UNRS 314 Name - Number - Ruptured AppendixSapiah RamanNo ratings yet
- Welling 2019Document9 pagesWelling 2019riskiNo ratings yet
- The Security of An Early Warning: Presep Oximetry CatheterDocument4 pagesThe Security of An Early Warning: Presep Oximetry Catheteralejandro sanche mejoradaNo ratings yet
- S RL 31072018 Desmoplastic FibromaDocument23 pagesS RL 31072018 Desmoplastic FibromaAnonymous bE4VegCcNo ratings yet
- Glucose Tolerance Test: By, Prof&Hod Meera ArumugamDocument12 pagesGlucose Tolerance Test: By, Prof&Hod Meera Arumugamshiv gautamNo ratings yet
- NUR 204.intramuscular InjectionDocument65 pagesNUR 204.intramuscular InjectionKouta SanNo ratings yet
- ConclusionDocument2 pagesConclusionJomar PlataNo ratings yet
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsFrom EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsRating: 4.5 out of 5 stars4.5/5 (39)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- Summary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDFrom EverandSummary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDRating: 4.5 out of 5 stars4.5/5 (167)
- Rewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryFrom EverandRewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryRating: 4.5 out of 5 stars4.5/5 (157)
- The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeFrom EverandThe Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeRating: 4.5 out of 5 stars4.5/5 (141)
- Redefining Anxiety: What It Is, What It Isn't, and How to Get Your Life BackFrom EverandRedefining Anxiety: What It Is, What It Isn't, and How to Get Your Life BackRating: 4.5 out of 5 stars4.5/5 (153)
- Vagus Nerve: A Complete Self Help Guide to Stimulate and Activate Vagal Tone — A Self Healing Exercises to Reduce Chronic Illness, PTSD, Anxiety, Inflammation, Depression, Trauma, and AngerFrom EverandVagus Nerve: A Complete Self Help Guide to Stimulate and Activate Vagal Tone — A Self Healing Exercises to Reduce Chronic Illness, PTSD, Anxiety, Inflammation, Depression, Trauma, and AngerRating: 4.5 out of 5 stars4.5/5 (16)
- Somatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionFrom EverandSomatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionNo ratings yet
- Feel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveFrom EverandFeel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveRating: 4 out of 5 stars4/5 (250)
- Uncontrolled Spread: Why COVID-19 Crushed Us and How We Can Defeat the Next PandemicFrom EverandUncontrolled Spread: Why COVID-19 Crushed Us and How We Can Defeat the Next PandemicNo ratings yet
- The Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeFrom EverandThe Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeRating: 4.5 out of 5 stars4.5/5 (49)
- Don't Panic: Taking Control of Anxiety AttacksFrom EverandDon't Panic: Taking Control of Anxiety AttacksRating: 4 out of 5 stars4/5 (12)
- Breaking the Chains of Transgenerational Trauma: My Journey from Surviving to ThrivingFrom EverandBreaking the Chains of Transgenerational Trauma: My Journey from Surviving to ThrivingRating: 4.5 out of 5 stars4.5/5 (30)
- The Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItFrom EverandThe Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItRating: 4.5 out of 5 stars4.5/5 (107)
- Do You Believe in Magic?: The Sense and Nonsense of Alternative MedicineFrom EverandDo You Believe in Magic?: The Sense and Nonsense of Alternative MedicineNo ratings yet
- Feeling Great: The Revolutionary New Treatment for Depression and AnxietyFrom EverandFeeling Great: The Revolutionary New Treatment for Depression and AnxietyNo ratings yet
- Winning the War in Your Mind: Change Your Thinking, Change Your LifeFrom EverandWinning the War in Your Mind: Change Your Thinking, Change Your LifeRating: 5 out of 5 stars5/5 (560)
- My Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesFrom EverandMy Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesRating: 5 out of 5 stars5/5 (70)
- Summary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisFrom EverandSummary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (5)
- Beyond Thoughts: An Exploration Of Who We Are Beyond Our MindsFrom EverandBeyond Thoughts: An Exploration Of Who We Are Beyond Our MindsRating: 4.5 out of 5 stars4.5/5 (7)
- Bedtime Stories for Stressed out Adults: Bedtime Stories for Stressed Out Adults: Relaxing Sleep Stories for Everyday Guided Meditation to Help With Insomnia and AnxietyFrom EverandBedtime Stories for Stressed out Adults: Bedtime Stories for Stressed Out Adults: Relaxing Sleep Stories for Everyday Guided Meditation to Help With Insomnia and AnxietyRating: 4.5 out of 5 stars4.5/5 (8)
- It's All Too Much: An Easy Plan for Living a Richer Life with Less StuffFrom EverandIt's All Too Much: An Easy Plan for Living a Richer Life with Less StuffRating: 4 out of 5 stars4/5 (232)
- Binaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationFrom EverandBinaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationRating: 5 out of 5 stars5/5 (9)
- The Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouFrom EverandThe Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouNo ratings yet