Professional Documents
Culture Documents
4 Lecture Insulin Initiation STENO Approved Asd
Uploaded by
Ricky SetiawanOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
4 Lecture Insulin Initiation STENO Approved Asd
Uploaded by
Ricky SetiawanCopyright:
Available Formats
Slide 1
Lecture:
Insulin Initiation and Monitoring
30 minutes
Slide 2
The Usage of Insulin Lecture Main Learning Points
Understand the insulin mechanism of action and its relationship to blood glucose Understand the current usage of Insulin in Indonesia Understand the different types of insulin, when to use insulin and the different insulin regiments Understand the relationship between insulin dosage and blood glucose measurements
Slide 3
Treatment therapies for Type 2 diabetes
When and How to start treatment
START TREATMENT
OAD TREATMENT
START INSULIN
INSULIN INTENSIFICATION
Lifestyle + Metformin
+-other OAD or GLP-1 agonists
Basal
Basal Insulin Premix Insulin
Basal + Bolus Insulin
HbA1c 7.0%
Adapted from Raccah et al. Diabetes Metab Res Rev 2007;23:257.
Slide 4
Insulin remains the most efficacious glucose lowering agent
Decrease in HbA1c: Potency of monotherapy
HbA1c %
Nathan et al., Diabetes Care 2009;32:193-203.
Slide 5
What is Insulin
After a meal carbohydrates are digested and enter the blood system, which transports them to the cells
Some cells (those of muscles and fat tissue) need assistance to have blood sugar enter into them and to be used for energy production
INSULIN is needed for glucose uptake and storage
The liver needs assistance to start the process of storage of glucose in the form of glycogen
Slide 6
Insulin secretion is delayed and blunted in Type 2 Diabetes
The goal of insulin therapy is to restore normal insulin secretion
800
Meal
Meal
Meal
Gap that needs to be covered Normal
600
Type 2 diabetes
Insulin Secretion 400 (pmol/min)
200
Time (24 hours)
Adapted from: Polonsky KS, et al. N Engl J Med. 1996 Mar 21;334(12):777-783.
Slide 7
How Insulin acts in the body
Insulin
Insulin binds to the insulin receptors on the cell membranes of the target cells in the liver, muscles and adipose tissue
Liver
Muscles
Adipose Tissue
Inhibits glucose production Promotes formation of glycogen and its storage
Promotes uptake and utilization of glucose
Promotes uptake of glucose Suppresses lipolysis
Slide 8
Objectives of Insulin Treatment
Maintain blood glucose levels between 80-140 mg/dl: 1. By promoting uptake of glucose by target cells 2. subsequent breakdown into energy (glycolysis) storage as glycogen (glycogenesis)
By inhibiting new glucose formation from non carbohydrate source (gluconeogenesis) or production of glucose by liver
3.
By suppressing lipolysis (breakdown of fat)
Slide 9
Most people with type 2 diabetes will, in time, need insulin therapy because
60
Patients requiring additional insulin (%)
50 40 30 20 10 0 1 2 3 4 5 6
Years from start of UKPDS (Patients treated with chlorpropramide)
Wright A et al. Diabetes Care 2002;25:3306
Slide 10
diabetes Patients will eventually fail on OADs
UKPDS
9 8.5
Median HbA1c (%) 8
Conventional* Glibenclamide Metformin Insulin
ADOPT
8
Rosiglitazone Metformin Glibenclamide
7.5
7.5 7 Recommended treatment target <7.0% 6.2% upper limit of normal range 0 2 4 6 8 Years from randomisation 10
6.5 6
6.5
6 0 1 2 3 Time (years) 4 5
*Diet initially then sulphonylureas, insulin and/or metformin if FPG>15 mmol/L; ADA clinical practice recommendations. UKPDS 34, n=1704
UKPDS 34. Lancet 1998:352:85465; Kahn et al (ADOPT). NEJM 2006;355(23):242743
Slide 11
Insulin can be initiated at any time Traditionally, insulin has been reserved as the last line of therapy However, considering the benefits of normal glycemic status, Insulin can be initiated earlier and as soon as possible
Inadequate Lifestyle + 1 OAD + 2 OAD + 3 OAD
INITIATE INSULIN
Slide 12
but Insulin usage is currently very low in Indonesia compared to its neighbouring countries
Population Indonesia Bangladesh Philippines Vietnam Thailand Malaysia 104 161 982 417 3,258 2,029 Mega Units Insulin Units / Capita 248 Total Insulin Used 694 3,097 Insulin Usage per Capita
3 19 9 5 49 70
92 67 29
Million People
IMS Full year 2011 Data. CIA World Factbook
Slide 13
Insulin Indications
Absolut Indication Type 1 Diabetes Relative Indication
Patients who fail to reach target with OAD optimal dosage
(3-6 months) Type 2 DM Outpatient with:
Pregnancy not controlled with diet Infected Diabetes Feet High Blood Glucose Fluctuations Repeated History of Ketoacidosis History of Pankreotomi
Besides the above, there are a number of conditions where insulin is required, e.g. chronic liver, kidney function interruption and high dosage steroid therapy
Slide 14
Three Types of Insulin
Schematic Representation Only
BASAL INSULIN PRE-MIX INSULIN
GIR (mg/kg/min)
FAST-ACTING INSULIN
12
Time (h)
16
20
24
Slide 15
Three Types of Insulin
BASAL
GIR (mg/kg/min)
GIR (mg/kg/min)
PRE-MIX
GIR (mg/kg/min)
FAST-ACTING
0 4
8 12 16 20 24
Time (h)
0 4
8 12 16 20 24
Time (h)
0 4
8 12 16 20 24
Time (h)
Basal Insulin provides a steady concentration of insulin in the bloodstream over 24 hours. Initially, basal insulin should be given at 10 units per day at night time or in the morning1
Premixed insulins contain a mixture of rapid-acting and intermediate-acting insulin in a fixed combination to provide coverage of prandial and basal insulin requirements2
Fast-acting insulins include single amino acid replacement that reduce their ability to selfassociate into dimers and hexamers. This means that they are quickly absorbed into the bloodstream, following subcutaneous injection.3
1. Hompesch M. Diabetes Obes Metab 2006; 8:568; 2. Weyer et al. Diabetes Care 1997;10:16121614.; 3. 1. Heinemann et al. Diabetes Care. 1998;21:19104
Slide 16
Pharmacokinetics of the different Types of Insulin available in Indonesia
Profile Type of Insulin Fast-acting Analogue Insulin Insulin Name Insulin Aspart (NovoRapid) Insulin Lispro (HumaLog) Onset (hours) 0.2 0.5 0.2 0.5 Peak (hours) 0.5 - 2 0.5 - 2
Insulin Gluisine (Apidra)
Fast-acting Human Insulin ActRapid Humulin R Intermediate Human Insulin Insulatard Humulin N Long-acting Analogue Insulin Insulin Detemir (Levemir) Insulin Glargine (Lantus) Pre-mix Analogue Insulin Insulin Aspart (NovoMix) Insulin NPL (HumaLog) Pre-mix Human Insulin Mixtard Humulin Mix
Adapted from Mooradian et al. Ann Intern Med 2006; 145: 125-34
0.2 0.5
0.5 1 0.5 1 1.5 4 1.5 4 1-3 1-3 0.2 0.5 0.2 0.5 0.5 1 0.5 1
0.5 - 2
0.5 - 1 0.5 - 1 4 - 10 4 - 10
1-4 1-4 3 - 12 3 - 12
Slide 17
Basic Insulin Start Recommendation
If Fasting Blood Glucose is elevated
Start with Basal Insulin
If both Fasting and Prandial Blood Glucose are elevated
Start with Premix Insulin OR add Basal Insulin to OAD OR Start Basal/Bolus Therapy
Source: ADA Guidelines
Slide 18
Insulin Titration schemes Basal and Fast-Acting Insulin
Fasting Blood Glucose Content (mg/dl) <70 mg/dl Basal Insulin Titration Reduce dosage with 2 units Maintain dosage Increase dosage 2 units per 3 days Increase dosage 4 units per 3 days
BASAL INSULIN
70-130 mg/dl 130-180 mg/dl >180 mg/dl
Once titrated, continue to monitor HbA1c every 3 months
FASTACTING INSULIN
Fasting Blood Glucose Content (mg/dl) Start with 4 units / day
Fast-acting Insulin Titration
Increase by 2 units every 3 days until target is reached
When starting Fast-acting Insulin, secretagogues should be discontinued
Source: KONSENSUS: Insulin Treatment 2011
Slide 19
Insulin Treatment Optimization
How to Optimize Treatment after Initiation
Start with Basal Insulin 10u / daily with meal or before bedtime. Same injection time every day
Basal Insulin Only Usually with OAD
If glycemic target is not reached titrate according to Basal Titration Scheme
Basal Insulin Only Usually with OAD
If glycemic target is not reached within 2-3 months, intensify Insulin treatment
Premix Insulin Usually keep OAD Basal with Prandial Usually keep OAD Basal Bolus Usually keep OAD
Switch to Premix twice-daily. Add Prandial starting Start with equal basal dose, with 4u / day either but give 50% per injection once or twice-daily and and titrate accordingly titrate accordingly
Source: PERKENI Insulin Guidelines 2011
Switch to Basal Bolus (3 daily prandial) start with 4u / day and titrate accordingly)
Slide 20
Primarily one type of Insulin device available in Indonesia
Prefilled devices
Disposable disposed of once empty Less teaching time required Primarily plastic Easy and Convenient for Patients
Slide 21
WE WILL COVER HOW TO START A PATIENT ON INSULIN AND INJECTION TECHNIQUES IN A SEPARATE WORKSHOP
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Hematology Cell Morphology ChartDocument2 pagesHematology Cell Morphology ChartMiaoNo ratings yet
- Jurnal DBD 3 2010Document10 pagesJurnal DBD 3 2010Sukma ArdiNo ratings yet
- Drug Induced HepatotoksikDocument2 pagesDrug Induced HepatotoksikRicky SetiawanNo ratings yet
- Mrs. Risma /22 Y.O/Living Child: - Admission September 11th 2014/ 21.30 PMDocument4 pagesMrs. Risma /22 Y.O/Living Child: - Admission September 11th 2014/ 21.30 PMRicky SetiawanNo ratings yet
- Jadwal Harian PanumDocument1 pageJadwal Harian PanumRicky SetiawanNo ratings yet
- G2P1A0 H 40-41 Wop + Inlabor Stage I Active Phase+ History of Prom + Post Date + Slfiu + Breech Presentation + Efw 3400 GRDocument8 pagesG2P1A0 H 40-41 Wop + Inlabor Stage I Active Phase+ History of Prom + Post Date + Slfiu + Breech Presentation + Efw 3400 GRRicky SetiawanNo ratings yet
- G2P1A0 H 40-41 Wop + Inlabor Stage I Active Phase+ History of Prom + Post Date + Slfiu + Breech Presentation + Efw 3400 GRDocument8 pagesG2P1A0 H 40-41 Wop + Inlabor Stage I Active Phase+ History of Prom + Post Date + Slfiu + Breech Presentation + Efw 3400 GRRicky SetiawanNo ratings yet
- Herpes ZosterDocument13 pagesHerpes ZosterRicky SetiawanNo ratings yet
- Starting Basal Insulin After Oral Agent FailureDocument32 pagesStarting Basal Insulin After Oral Agent FailureRicky SetiawanNo ratings yet
- Government of Andhra Pradesh Andhra Pradesh Medical Services Recruitment BoardDocument13 pagesGovernment of Andhra Pradesh Andhra Pradesh Medical Services Recruitment Boardchandu93152049No ratings yet
- Wilcock 2008Document11 pagesWilcock 2008Nadia SaiNo ratings yet
- Pediatric Asthma Situation in Chengdu, China, During The COVID-19 Pandemic: An Observational StudyDocument10 pagesPediatric Asthma Situation in Chengdu, China, During The COVID-19 Pandemic: An Observational StudyzainabNo ratings yet
- MMS DeptInventoryRepDocument46 pagesMMS DeptInventoryRepGail Martinez MoisesNo ratings yet
- D DimerDocument102 pagesD DimerSayed Nour100% (1)
- Warfarin Reversal Guideline 2012 PDFDocument8 pagesWarfarin Reversal Guideline 2012 PDFVlady78No ratings yet
- Atypical PneumoniaDocument5 pagesAtypical Pneumoniamarkylopez23No ratings yet
- Adultos: 12.5 - 50 MG QD Tableta Atenolol 100 MG + Clortalidona 25 MG Adultos: 12,5 A 50 Mg/dia, Una Sola DosisDocument3 pagesAdultos: 12.5 - 50 MG QD Tableta Atenolol 100 MG + Clortalidona 25 MG Adultos: 12,5 A 50 Mg/dia, Una Sola DosisDarwin QuishpeNo ratings yet
- DigitalisDocument5 pagesDigitalislimentuNo ratings yet
- Digestive Questionnaire (Medical)Document1 pageDigestive Questionnaire (Medical)Mexico EnglishNo ratings yet
- Articles by Dr. Nata ParnesDocument19 pagesArticles by Dr. Nata ParnesWatertown Daily TimesNo ratings yet
- StaphylococcusDocument28 pagesStaphylococcusAliyah SajaNo ratings yet
- Vaginal Discharge GuidelineDocument4 pagesVaginal Discharge GuidelineGung Bagvs SaputraNo ratings yet
- List of PM&DC Recognized JournalsDocument14 pagesList of PM&DC Recognized JournalsSanaa AhmedNo ratings yet
- Autonomic Dysreflexia-Part OneDocument3 pagesAutonomic Dysreflexia-Part OneManuel BucurNo ratings yet
- Somatic Symptom and Related DisordersDocument31 pagesSomatic Symptom and Related DisordersMarinel June Paler100% (2)
- ESR Microsed PermaiDocument20 pagesESR Microsed PermaiHishamudin RaisNo ratings yet
- Form Ringkasan Perawatan Pasien Pulang (Resume Medis)Document1 pageForm Ringkasan Perawatan Pasien Pulang (Resume Medis)gandi mahardika muktiNo ratings yet
- Effect of Iron Containing Supplements On Rats DenDocument6 pagesEffect of Iron Containing Supplements On Rats Dendhea hutabaratNo ratings yet
- Ao2022 0037Document22 pagesAo2022 0037Abigael VianaNo ratings yet
- Art Therapy Can Reduce Pain and Anxiety in Cancer PatientsDocument2 pagesArt Therapy Can Reduce Pain and Anxiety in Cancer PatientspatypappacenaNo ratings yet
- Animal Incident Report Form 02 10 2021Document4 pagesAnimal Incident Report Form 02 10 2021WenaNo ratings yet
- Oxford: ReferenceDocument846 pagesOxford: ReferenceNMC NEPHROLOGYNo ratings yet
- 0824708520Document603 pages0824708520Lasha OsepaishviliNo ratings yet
- H5N1 EngDocument8 pagesH5N1 EngHường ĐỗNo ratings yet
- Treatment Plan Form John Doe - Coun755Document3 pagesTreatment Plan Form John Doe - Coun755api-310813184No ratings yet
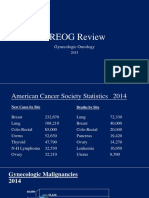
- 2015 Oncology CREOG Review PDFDocument76 pages2015 Oncology CREOG Review PDFRima HajjarNo ratings yet
- AHA Coding Clinic Guidance: Code Number in Lieu of A DiagnosisDocument2 pagesAHA Coding Clinic Guidance: Code Number in Lieu of A Diagnosissyaiful rinantoNo ratings yet
- Nuevo ResumeDocument2 pagesNuevo Resumeapi-380898658No ratings yet