Professional Documents
Culture Documents
Bio 122 Chapter 18
Uploaded by
cystanarisaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bio 122 Chapter 18
Uploaded by
cystanarisaCopyright:
Available Formats
Chapter 18, Cardiovascular System 1
18
The Cardiovascular System:
The Heart
Anatomy
Chapter 18, Cardiovascular System
2
Heart Anatomy
Approximately the size of your fist
Location
Superior surface of diaphragm
Left of the midline
Anterior to the vertebral column, posterior to the
sternum
Chapter 18, Cardiovascular System
3
Heart Anatomy
Figure 18.1
Chapter 18, Cardiovascular System
4
Coverings of the Heart: Anatomy
Pericardium a double-walled sac around the
heart composed of:
1. A superficial fibrous pericardium
2. A deep two-layer serous pericardium
a. The parietal layer lines the internal surface of
the fibrous pericardium
b. The visceral layer or epicardium lines the
surface of the heart
They are separated by the fluid-filled
pericardial cavity
Chapter 18, Cardiovascular System
5
Coverings of the Heart: Physiology
The Function of the Pericardium:
Protects and anchors the heart
Prevents overfilling of the heart with blood
Allows for the heart to work in a relatively friction-
free environment
Chapter 18, Cardiovascular System
6
Pericardial Layers of the Heart
Figure 18.2
Chapter 18, Cardiovascular System
7
Heart Wall
Epicardium visceral layer of the serous
pericardium
Myocardium cardiac muscle layer forming the
bulk of the heart
Fibrous skeleton of the heart crisscrossing,
interlacing layer of connective tissue
Endocardium endothelial layer of the inner
myocardial surface
Chapter 18, Cardiovascular System
8
Vessels returning blood to the heart include:
1. Superior and inferior venae cavae
2. Right and left pulmonary veins
Vessels conveying blood away from the heart include:
1. Pulmonary trunk, which splits into right and left
pulmonary arteries
2. Ascending aorta (three branches)
a. Brachiocephalic
b. Left common carotid
c. Subclavian arteries
External Heart: Major Vessels of the Heart
(Anterior View)
Chapter 18, Cardiovascular System
9
Arteries right and left coronary (in
atrioventricular groove), marginal, circumflex, and
anterior interventricular arteries
Veins small cardiac, anterior cardiac, and great
cardiac veins
External Heart: Vessels that Supply/Drain the
Heart (Anterior View)
Chapter 18, Cardiovascular System
10
External Heart: Anterior View
Figure 18.4b
Chapter 18, Cardiovascular System
11
Vessels returning blood to the heart include:
1. Right and left pulmonary veins
2. Superior and inferior venae cavae
Vessels conveying blood away from the heart
include:
1. Aorta
2. Right and left pulmonary arteries
External Heart: Major Vessels of the Heart
(Posterior View)
Chapter 18, Cardiovascular System
12
Arteries right coronary artery (in atrioventricular
groove) and the posterior interventricular artery (in
interventricular groove)
Veins great cardiac vein, posterior vein to left
ventricle, coronary sinus, and middle cardiac vein
External Heart: Vessels that Supply/Drain the
Heart (Posterior View)
Chapter 18, Cardiovascular System
13
External Heart: Posterior View
Figure 18.4d
Chapter 18, Cardiovascular System
14
Gross Anatomy of Heart: Frontal Section
Figure 18.4e
Chapter 18, Cardiovascular System
15
Atria of the Heart
Atria are the receiving chambers of the heart
Each atrium has a protruding auricle
Pectinate muscles mark atrial walls
Blood enters right atria from superior and inferior
venae cavae and coronary sinus
Blood enters left atria from pulmonary veins
Chapter 18, Cardiovascular System
16
Ventricles of the Heart
Ventricles are the discharging chambers of the heart
Papillary muscles and trabeculae carneae muscles
mark ventricular walls
Right ventricle pumps blood into the pulmonary
trunk
Left ventricle pumps blood into the aorta
Chapter 18, Cardiovascular System
17
Myocardial Thickness and Function
Thickness of myocardium varies according to the function of the
chamber
Atria are thin walled, deliver blood to adjacent ventricles
Ventricle walls are much thicker and stronger
right ventricle supplies blood to the lungs (little flow resistance)
left ventricle wall is the thickest to supply systemic circulation
Chapter 18, Cardiovascular System
18
Thickness of Cardiac Walls
Myocardium of left ventricle is much thicker than the right.
Chapter 18, Cardiovascular System
19
Atrial Septal Defect
Chapter 18, Cardiovascular System
20
Ventricular Septal Defect
Chapter 18, Cardiovascular System
21
Pathway of Blood Through the Heart and
Lungs
Right atrium tricuspid valve right ventricle
Right ventricle pulmonary semilunar valve
pulmonary arteries lungs
Lungs pulmonary veins left atrium
Left atrium bicuspid valve left ventricle
Left ventricle aortic semilunar valve aorta
Aorta systemic circulation
Chapter 18, Cardiovascular System
22
Pathway of Blood Through the Heart and
Lungs
Figure 18.5
Chapter 18, Cardiovascular System
23
Coronary Circulation
Coronary circulation is the functional blood supply
to the heart muscle itself
Collateral routes ensure blood delivery to heart
even if major vessels are occluded
Chapter 18, Cardiovascular System
24
Coronary Circulation: Arterial Supply
Figure 18.7a
Chapter 18, Cardiovascular System
25
Coronary Circulation: Venous Supply
Figure 18.7b
Chapter 18, Cardiovascular System
26
Heart Valves
Heart valves ensure unidirectional blood flow
through the heart
Atrioventricular (AV) valves lie between the atria
and the ventricles
AV valves prevent backflow into the atria when
ventricles contract
Chordae tendineae anchor AV valves to papillary
muscles
Chapter 18, Cardiovascular System
27
Heart Valves
Semilunar valves prevent backflow of blood into the
ventricles
Aortic semilunar valve lies between the left
ventricle and the aorta
Pulmonary semilunar valve lies between the right
ventricle and pulmonary trunk
Chapter 18, Cardiovascular System
28
Heart Valves
Figure 18.8a, b
Chapter 18, Cardiovascular System
29
Heart Valves
Figure 18.8c, d
Chapter 18, Cardiovascular System
30
Atrioventricular Valve Function
Figure 18.9
Chapter 18, Cardiovascular System
31
Semilunar Valve Function
Figure 18.10
Chapter 18, Cardiovascular System
32
Mitral Valve Prolapse
Chapter 18, Cardiovascular System
33
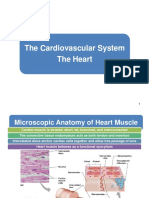
Microscopic Anatomy of Heart Muscle
Cardiac muscle is striated, short, fat, branched, and
interconnected
The connective tissue endomysium acts as both
tendon and insertion
Intercalated discs anchor cardiac cells together and
allow free passage of ions
Heart muscle behaves as a functional syncytium
I nterActive Physiology
:
Cardiovascular System: Anatomy Review: The Heart
PLAY
Chapter 18, Cardiovascular System
34
Microscopic Anatomy of Heart Muscle
Figure 18.11
Chapter 18, Cardiovascular System 35
18
The Cardiovascular System:
The Heart
Physiology
Chapter 18, Cardiovascular System
36
Cardiac Muscle Contraction
Heart muscle:
Is stimulated by nerves and is self-excitable
(automaticity)
Contracts as a unit
Has a long (250 ms) absolute refractory period
Cardiac muscle contraction is similar to skeletal
muscle contraction
Chapter 18, Cardiovascular System
37
Heart Physiology: Intrinsic Conduction
System
Autorhythmic cells:
Initiate action potentials
Have unstable resting potentials called pacemaker
potentials
Use calcium influx (rather than sodium) for rising
phase of the action potential
Chapter 18, Cardiovascular System
38
Pacemaker and Action Potentials of the Heart
Figure 18.13
Chapter 18, Cardiovascular System
39
Heart Physiology: Sequence of Excitation
Sinoatrial (SA) node generates impulses about 75
times/minute
Atrioventricular (AV) node delays the impulse
approximately 0.1 second
Chapter 18, Cardiovascular System
40
Heart Physiology: Sequence of Excitation
Impulse passes from atria to ventricles via the
atrioventricular bundle (bundle of His)
AV bundle splits into two pathways in the
interventricular septum (bundle branches)
1. Bundle branches carry the impulse toward the
apex of the heart
2. Purkinje fibers carry the impulse to the heart
apex and ventricular walls
Chapter 18, Cardiovascular System
41
Heart Physiology: Sequence of Excitation
Figure 18.14a
Chapter 18, Cardiovascular System
42
Heart Excitation Related to ECG
Figure 18.17
Chapter 18, Cardiovascular System
43
Extrinsic Innervation of the Heart
Heart is stimulated
by the sympathetic
cardioacceleratory
center
Heart is inhibited by
the parasympathetic
cardioinhibitory
center
Figure 18.15
Chapter 18, Cardiovascular System
44
Electrocardiography
Electrical activity is recorded by electrocardiogram
(ECG)
P wave corresponds to depolarization of SA node
QRS complex corresponds to ventricular
depolarization
T wave corresponds to ventricular repolarization
Atrial repolarization record is masked by the larger
QRS complex
I nterActive Physiology
:
Cardiovascular System: Intrinsic Conduction System
PLAY
Chapter 18, Cardiovascular System
45
Electrocardiography
Figure 18.16
Chapter 18, Cardiovascular System
46
Heart Sounds
Heart sounds (lub-dup) are associated with closing
of heart valves
First sound occurs as AV valves close and
signifies beginning of systole (contraction)
Second sound occurs when SL valves close at the
beginning of ventricular diastole (relaxation)
Chapter 18, Cardiovascular System
47
Cardiac Cycle
Cardiac cycle refers to all events associated with
blood flow through the heart
Systole contraction of heart muscle
Diastole relaxation of heart muscle
Chapter 18, Cardiovascular System
48
Phases of the Cardiac Cycle
Ventricular filling mid-to-late diastole
Heart blood pressure is low as blood enters atria
(passively) and flows into ventricles
AV valves are open, then atrial systole occurs
Chapter 18, Cardiovascular System
49
Phases of the Cardiac Cycle
Ventricular systole (contraction)
Atria relax
Rising ventricular pressure results in closing of AV
valves
Isovolumetric contraction phase
Ventricular ejection phase opens semilunar valves
Chapter 18, Cardiovascular System
50
Phases of the Cardiac Cycle
Isovolumetric relaxation early diastole
Ventricles relax
Backflow of blood in aorta and pulmonary trunk
closes semilunar valves
Dicrotic notch brief rise in aortic pressure caused
by backflow of blood rebounding off semilunar
valves
I nterActive Physiology
:
Cardiovascular System: Cardiac Cycle
PLAY
Chapter 18, Cardiovascular System
51
Phases of the Cardiac Cycle
Figure 18.20
Chapter 18, Cardiovascular System
52
Cardiac Output (CO) and Reserve
Cardiac Output is the amount of blood pumped by
each ventricle in one minute
CO is the product of heart rate (HR) and stroke
volume (SV)
HR is the number of heart beats per minute
SV is the amount of blood pumped out by a
ventricle with each beat
Cardiac reserve is the difference between resting
and maximal CO
Chapter 18, Cardiovascular System
53
Cardiac Output: Example
CO (ml/min) = HR (75 beats/min) x SV (70 ml/beat)
CO = 5250 ml/min (5.25 L/min)
Chapter 18, Cardiovascular System
54
Regulation of Stroke Volume
SV = end diastolic volume (EDV) minus end
systolic volume (ESV)
EDV = amount of blood collected in a ventricle
during diastole
ESV = amount of blood remaining in a ventricle
after contraction
Chapter 18, Cardiovascular System
55
Factors Affecting Stroke Volume
Preload amount ventricles are stretched by
contained blood
Contractility cardiac cell contractile force due to
factors other than EDV
Afterload back pressure exerted by blood in the
large arteries leaving the heart
Chapter 18, Cardiovascular System
56
Frank-Starling Law of the Heart
Preload, or degree of stretch, of cardiac muscle cells
before they contract is the critical factor controlling
stroke volume
Slow heartbeat and exercise increase venous return
to the heart, increasing SV
Blood loss and extremely rapid heartbeat decrease
SV
Chapter 18, Cardiovascular System
57
Preload and Afterload
Figure 18.21
Chapter 18, Cardiovascular System
58
Extrinsic Factors Influencing Stroke Volume
Contractility is the increase in contractile strength,
independent of stretch and EDV
Increase in contractility comes from:
Increased sympathetic stimuli
Certain hormones
Ca
2+
and some drugs
Chapter 18, Cardiovascular System
59
Extrinsic Factors Influencing Stroke Volume
Agents/factors that decrease contractility include:
Acidosis
Increased extracellular K
+
Calcium channel blockers
Chapter 18, Cardiovascular System
60
Contractility and Norepinephrine
Sympathetic
stimulation
releases
norepinephrine
and initiates a
cyclic AMP
second-
messenger
system
Figure 18.22
Chapter 18, Cardiovascular System
61
Regulation of Heart Rate
Positive chronotropic factors increase heart rate
Caffeine
Negative chronotropic factors decrease heart rate
Sedatives
Chapter 18, Cardiovascular System
62
Sympathetic nervous system (SNS) stimulation is activated
by stress, anxiety, excitement, or exercise
Parasympathetic nervous system (PNS) stimulation is
mediated by acetylcholine and opposes the SNS
PNS dominates the autonomic stimulation, slowing heart
rate and causing vagal tone
If the Vagus Nerver was cut, the heart would lose its
tone. Thus, increasing the heart rate by 25 beats per
minute.
Regulation of Heart Rate: Autonomic Nervous
System
Chapter 18, Cardiovascular System
63
Atrial (Bainbridge) Reflex
Atrial (Bainbridge) reflex a sympathetic reflex
initiated by increased blood in the atria
Causes stimulation of the SA node
Stimulates baroreceptors in the atria, causing
increased SNS stimulation
Chapter 18, Cardiovascular System
64
Chemical Regulation of the Heart
The hormones epinephrine and thyroxine increase
heart rate
Intra- and extracellular ion concentrations must be
maintained for normal heart function
I nterActive Physiology
:
Cardiovascular System: Cardiac Output
PLAY
Chapter 18, Cardiovascular System
65
Factors Involved in Regulation of Cardiac
Output
Figure 18.23
Chapter 18, Cardiovascular System
66
Congestive Heart Failure (CHF)
Congestive heart failure (CHF) is caused by:
Coronary atherosclerosis
Persistent high blood pressure
Multiple myocardial infarcts
Dilated cardiomyopathy (DCM) main pumping
chambers of the heart are dilated and contract
poorly
Chapter 18, Cardiovascular System
67
Developmental Aspects of the Heart
Figure 18.24
Chapter 18, Cardiovascular System
68
Developmental Aspects of the Heart
Fetal heart structures that bypass pulmonary
circulation
Foramen ovale connects the two atria
Ductus arteriosus connects pulmonary trunk and
the aorta
Chapter 18, Cardiovascular System
69
Figure 18.25
Examples of Congenital Heart Defects
Chapter 18, Cardiovascular System
70
Age-Related Changes Affecting the Heart
Sclerosis and thickening of valve flaps
Decline in cardiac reserve
Fibrosis of cardiac muscle
Atherosclerosis
Chapter 18, Cardiovascular System
71
Congestive Heart Failure
Causes of CHF
coronary artery disease, hypertension, MI, valve disorders,
congenital defects
Left side heart failure
less effective pump so more blood remains in ventricle
heart is overstretched & even more blood remains
blood backs up into lungs as pulmonary edema
suffocation & lack of oxygen to the tissues
Right side failure
fluid builds up in tissues as peripheral edema
Chapter 18, Cardiovascular System
72
Coronary Artery Disease
Heart muscle receiving
insufficient blood supply
narrowing of vessels---
atherosclerosis, artery
spasm or clot
atherosclerosis--smooth
muscle & fatty deposits in
walls of arteries
Treatment
drugs, bypass graft,
angioplasty, stent
Chapter 18, Cardiovascular System
73
Clinical Problems
MI = myocardial infarction
death of area of heart muscle from lack of O
2
replaced with scar tissue
results depend on size & location of damage
Blood clot
use clot dissolving drugs streptokinase or t-PA & heparin
balloon angioplasty
Angina pectoris
heart pain from ischemia (lack of blood flow and oxygen )
of cardiac muscle
Chapter 18, Cardiovascular System
74
By-pass Graft
Chapter 18, Cardiovascular System
75
Percutaneous Transluminal Coronary
Angioplasty
Chapter 18, Cardiovascular System
76
Artificial Heart
You might also like
- Sleep Smarter Book SummaryDocument6 pagesSleep Smarter Book SummaryEthanSong100% (18)
- Basic EKG RefresherDocument210 pagesBasic EKG RefresherAaron D. Phoenix100% (6)
- Maximize Muscle Growth Using Bodyweight ExercisesDocument173 pagesMaximize Muscle Growth Using Bodyweight Exerciseshung35% (23)
- Heart Anatomy and Physiology PDFDocument100 pagesHeart Anatomy and Physiology PDFAndrés Menéndez Rojas100% (1)
- Neurotransmitter Cheat Sheet AP ReviewDocument2 pagesNeurotransmitter Cheat Sheet AP ReviewNathania DawitNo ratings yet
- Heart Anatomy & Physiology GuideDocument56 pagesHeart Anatomy & Physiology Guidepreet kaurNo ratings yet
- Cath Lab Basics: A Guide to Cardiac Catheterization ProceduresDocument121 pagesCath Lab Basics: A Guide to Cardiac Catheterization ProceduresizalxrayNo ratings yet
- Cardiovascular System Anatomy and PhysiologyDocument93 pagesCardiovascular System Anatomy and PhysiologyJonald Pulgo IcoyNo ratings yet
- Deer, Timothy R. - Pope, Jason E - Treatment of Chronic Pain Conditions - A Comprehensive Handbook-Springer (2017)Document319 pagesDeer, Timothy R. - Pope, Jason E - Treatment of Chronic Pain Conditions - A Comprehensive Handbook-Springer (2017)paticex241100% (2)
- GIC CASTest 2.1 AUG 2021 V1Document1 pageGIC CASTest 2.1 AUG 2021 V1Bishoy BishayNo ratings yet
- The Heart's Chambers and ValvesDocument29 pagesThe Heart's Chambers and ValvesomarNo ratings yet
- The human body facts guide: Cells, organs, systems & moreDocument6 pagesThe human body facts guide: Cells, organs, systems & moreجنید سلیم چوہدری100% (4)
- Heart Failure - 2022Document106 pagesHeart Failure - 2022Rana Khaled AwwadNo ratings yet
- Cardiovascular SystemDocument26 pagesCardiovascular SystemdumbledoreaaaaNo ratings yet
- Essentials of Psychiatric Mental Health Nursing 7th Edition Townsend Test BankDocument15 pagesEssentials of Psychiatric Mental Health Nursing 7th Edition Townsend Test Bankkimberlymorriscntsoqmyjw100% (6)
- Human Anatomy: The Cardiovascular System: The HeartDocument46 pagesHuman Anatomy: The Cardiovascular System: The HeartOliviaMirzaNuswantari100% (1)
- Cardio SlidesDocument309 pagesCardio SlidesGina VasquezNo ratings yet
- Heart Anatomy: LocationDocument45 pagesHeart Anatomy: LocationZaira100% (1)
- Principles Dialysis 12-09-3Document35 pagesPrinciples Dialysis 12-09-3cystanarisaNo ratings yet
- HeartDocument72 pagesHeartfyzanfroshie100% (1)
- 2 Lecture CardioDocument46 pages2 Lecture Cardiodr_mohanad100% (1)
- Anatomi JantungDocument54 pagesAnatomi JantungsaifudinNo ratings yet
- Atlas of Sleep MedicineDocument362 pagesAtlas of Sleep MedicinekattbattNo ratings yet
- DX Intracranial Pressure PDFDocument8 pagesDX Intracranial Pressure PDFSherree HayesNo ratings yet
- Lesson 3Document71 pagesLesson 3Angel joyce ValenciaNo ratings yet
- The Cardiovascular System: The Heart: AnatomyDocument76 pagesThe Cardiovascular System: The Heart: AnatomyDeepuNo ratings yet
- Cardiovascular System IcdDocument56 pagesCardiovascular System IcdNaveen ChNo ratings yet
- The Cardiovascular System: The Heart: AnatomyDocument76 pagesThe Cardiovascular System: The Heart: AnatomyJoy Mazo FaderagaoNo ratings yet
- The Cardiovascular System: The Heart: AnatomyDocument76 pagesThe Cardiovascular System: The Heart: AnatomyadnanNo ratings yet
- Anatomi CardiovaskulerDocument76 pagesAnatomi CardiovaskulerPUTRINo ratings yet
- heartDocument37 pagesheartpm7197362No ratings yet
- Anatomy CorDocument76 pagesAnatomy CormayNo ratings yet
- Cardiovascular System Anatomy and PhysiologyDocument93 pagesCardiovascular System Anatomy and PhysiologyJonald Pulgo IcoyNo ratings yet
- The Cardiovascular System: The Heart: AnatomyDocument62 pagesThe Cardiovascular System: The Heart: AnatomyLingga GumelarNo ratings yet
- Circulatory SystemDocument31 pagesCirculatory SystemMHKNo ratings yet
- Cardiovascular SystemDocument34 pagesCardiovascular SystemAyesha SaleemNo ratings yet
- The Cardiovascular System: Anatomy of the HeartDocument32 pagesThe Cardiovascular System: Anatomy of the HeartGlen DaleNo ratings yet
- The Cardiovascular System: The Heart: AnatomyDocument35 pagesThe Cardiovascular System: The Heart: AnatomyPraneethaNo ratings yet
- Hemodinamik Pada Sistem Kardiovaskuler - PPTDocument114 pagesHemodinamik Pada Sistem Kardiovaskuler - PPTIsna ZalwaNo ratings yet
- The Cardiovascular System: The Heart: Anatomy and PhysiologyDocument30 pagesThe Cardiovascular System: The Heart: Anatomy and PhysiologyZachary CohenNo ratings yet
- The Heart: Basis of Life .?Document94 pagesThe Heart: Basis of Life .?Diksha AgrawalNo ratings yet
- Sistem Dan Fungsi KardiovaskulerDocument72 pagesSistem Dan Fungsi KardiovaskulerOncix PermanaNo ratings yet
- 81: Mammalian Heart and Its RegulationDocument75 pages81: Mammalian Heart and Its RegulationIt's Ika100% (1)
- 08 Human Physiology The HeartDocument107 pages08 Human Physiology The HeartsuNo ratings yet
- CH 21: Cardiovascular System - The Heart - : GoalsDocument21 pagesCH 21: Cardiovascular System - The Heart - : GoalsgopscharanNo ratings yet
- Cardiovascular System: Dr. Mohanad R. AlwanDocument46 pagesCardiovascular System: Dr. Mohanad R. Alwanmohanad11No ratings yet
- Cardiac Muscle Physiology and Cardiovascular System FunctionDocument183 pagesCardiac Muscle Physiology and Cardiovascular System FunctionArdhian Yudha CandraNo ratings yet
- Cardiovascular System: Unit 3 Slide 1Document79 pagesCardiovascular System: Unit 3 Slide 1Nestor BalboaNo ratings yet
- Cardiovascular System: The Heart: Chapter 19 - Lecture NotesDocument73 pagesCardiovascular System: The Heart: Chapter 19 - Lecture Noteshersheys72002No ratings yet
- The Anatomy and Physiology of the Respiratory and Nervous SystemsDocument50 pagesThe Anatomy and Physiology of the Respiratory and Nervous SystemsKartika SariNo ratings yet
- Circulatory SDocument110 pagesCirculatory SMohammed HabibNo ratings yet
- Internal Structure of HeartDocument1 pageInternal Structure of Heartmbudhathoki3000No ratings yet
- Cardiac Anatomy and Physiology: Iris Ken R. Rico, OTRPDocument90 pagesCardiac Anatomy and Physiology: Iris Ken R. Rico, OTRPAndra HijratulNo ratings yet
- The Circulatory SystemDocument53 pagesThe Circulatory SystemVera June RañesesNo ratings yet
- A Muscular Double Pump: The HeartDocument43 pagesA Muscular Double Pump: The HeartConeisa ConanNo ratings yet
- Lec 4 HeartDocument42 pagesLec 4 HeartEntesarNo ratings yet
- HUMAN ANATOMY AND PHYSIOLOGY LABORATORY Cardiovascular SystemDocument12 pagesHUMAN ANATOMY AND PHYSIOLOGY LABORATORY Cardiovascular SystemZaira MangalimanNo ratings yet
- 8.cardiovascular SystemDocument13 pages8.cardiovascular Systempodki gurungNo ratings yet
- TH e Circulatory System: HeartDocument68 pagesTH e Circulatory System: HeartMica BernardoNo ratings yet
- Week 9 CVS WorkbookDocument24 pagesWeek 9 CVS Workbooksupriyakunwar2019No ratings yet
- Blood Vessels and Circulation PDFDocument87 pagesBlood Vessels and Circulation PDFMay Flor VerdaderoNo ratings yet
- Chapter I - Cardiovascular System: HeartDocument2 pagesChapter I - Cardiovascular System: HeartIndranil SinhaNo ratings yet
- BMED 66 Chapter 14 HeartDocument7 pagesBMED 66 Chapter 14 HeartBSMT 1-1, TAN, NICOLE SELINA L.No ratings yet
- Circulatory SystemDocument155 pagesCirculatory SystemTrisha Mae BolotaoloNo ratings yet
- Heart ChambersDocument14 pagesHeart Chambersberniebernie20No ratings yet
- Heart Anatomy For LabDocument55 pagesHeart Anatomy For LabdrmarybethNo ratings yet
- Chapter 20 - Introduction To The Cardiovascular System: Away From To BetweenDocument6 pagesChapter 20 - Introduction To The Cardiovascular System: Away From To Betweentomorrow.today.yesterday .yesterdayNo ratings yet
- CARDIOVASCULARDocument41 pagesCARDIOVASCULARNor Jeannah PolaoNo ratings yet
- Maintenance of The Body: Cardiovascular SystemDocument74 pagesMaintenance of The Body: Cardiovascular Systemdania mauriyanaNo ratings yet
- Chapter 20-Cardiovascular System The HeartDocument44 pagesChapter 20-Cardiovascular System The HeartleoNo ratings yet
- Beating with Precision: The Science of Cardiology: Understand the Intricacies of the Human HeartFrom EverandBeating with Precision: The Science of Cardiology: Understand the Intricacies of the Human HeartNo ratings yet
- English Conversation-Ebook PDFDocument36 pagesEnglish Conversation-Ebook PDFRizka Sitti MuliyaNo ratings yet
- Gambar BioDocument2 pagesGambar BiocystanarisaNo ratings yet
- TOAIPKIDocument1 pageTOAIPKIcystanarisaNo ratings yet
- 8 9 FistulasDocument9 pages8 9 FistulascystanarisaNo ratings yet
- Abstrak Indo Japan EditDocument1 pageAbstrak Indo Japan EditcystanarisaNo ratings yet
- 427 833 1 SM PDFDocument8 pages427 833 1 SM PDFcystanarisaNo ratings yet
- Introduksi Kesehatan Reproduksi WanitaDocument27 pagesIntroduksi Kesehatan Reproduksi WanitacystanarisaNo ratings yet
- Obstetric and Gynecology Notes: FK Udayana 2016Document1 pageObstetric and Gynecology Notes: FK Udayana 2016cystanarisaNo ratings yet
- AKI New GuidelineDocument39 pagesAKI New GuidelineMohd RafiNo ratings yet
- Soap PediatriDocument1 pageSoap PediatricystanarisaNo ratings yet
- 2014 Report National Diabetes Statistics Report Data Sources PDFDocument9 pages2014 Report National Diabetes Statistics Report Data Sources PDFcystanarisaNo ratings yet
- B3 Histo Heart White PDFDocument29 pagesB3 Histo Heart White PDFcystanarisaNo ratings yet
- HEART ReducedDocument43 pagesHEART ReducedcystanarisaNo ratings yet
- 135Document25 pages135cystanarisaNo ratings yet
- 02 Diagnosis of AcuteDocument6 pages02 Diagnosis of AcutecystanarisaNo ratings yet
- Anatomi Fisiologi Kardiovaskular 2013Document64 pagesAnatomi Fisiologi Kardiovaskular 2013Sally WirawanNo ratings yet
- 2 1 - 9 13 PDFDocument5 pages2 1 - 9 13 PDFcystanarisaNo ratings yet
- Anatomy ReviewDocument17 pagesAnatomy ReviewcystanarisaNo ratings yet
- Kindermann Aneurysm May2014Document14 pagesKindermann Aneurysm May2014cystanarisaNo ratings yet
- B3 Histo Heart White PDFDocument29 pagesB3 Histo Heart White PDFcystanarisaNo ratings yet
- HEART ReducedDocument43 pagesHEART ReducedcystanarisaNo ratings yet
- Jordan Symons - The Physiology of DialysisDocument11 pagesJordan Symons - The Physiology of DialysiscystanarisaNo ratings yet
- Cardiovascular System Part 1Document62 pagesCardiovascular System Part 1cystanarisaNo ratings yet
- Arrhythmias 3Document21 pagesArrhythmias 3Omer SabirNo ratings yet
- B3 Histo Heart White PDFDocument29 pagesB3 Histo Heart White PDFcystanarisaNo ratings yet
- HEART ReducedDocument43 pagesHEART ReducedcystanarisaNo ratings yet
- Trinity CVS Lecture 1-ECG 12.13.Ppt (Read-Only)Document24 pagesTrinity CVS Lecture 1-ECG 12.13.Ppt (Read-Only)cystanarisaNo ratings yet
- Zhen Qi Quotes PDFDocument1 pageZhen Qi Quotes PDFAllanNo ratings yet
- ABG Made EasyDocument9 pagesABG Made EasyDrShruthi PradeepNo ratings yet
- Pe102 Prelim HandoutDocument2 pagesPe102 Prelim HandoutKiana Alexa BrigondoNo ratings yet
- Physiology Course OutlineDocument4 pagesPhysiology Course OutlineSAVIOUR BANDANo ratings yet
- Gluconeogenesis: Preventing Hypoglycemia Through De Novo Glucose SynthesisDocument12 pagesGluconeogenesis: Preventing Hypoglycemia Through De Novo Glucose SynthesisDayledaniel SorvetoNo ratings yet
- Manage Stress Through Physical ActivityDocument23 pagesManage Stress Through Physical ActivityNhedzCaidoNo ratings yet
- Vasoactive Peptides: Vasodilators and VasoconstrictorsDocument6 pagesVasoactive Peptides: Vasodilators and VasoconstrictorsMehwish HammadNo ratings yet
- DLL - Science 6 - Q2 - W1Document7 pagesDLL - Science 6 - Q2 - W1Kaye Goc-ongNo ratings yet
- Citizen Blood Pressure Monitor CH-452Document14 pagesCitizen Blood Pressure Monitor CH-452Carlos AguilarNo ratings yet
- Drug Study LabetalolDocument2 pagesDrug Study LabetalolJanzelvine Lee MontenegroNo ratings yet
- Cmca RleDocument13 pagesCmca RleABIGAIL ANNE DAPHNE ADANo ratings yet
- Hipoxemia RefratariaDocument4 pagesHipoxemia RefratariaThiago LacerdaNo ratings yet
- Yang Et Al, 2020 - O Papel Do BDNF Na Plasticidade Neural Na DepressãoDocument12 pagesYang Et Al, 2020 - O Papel Do BDNF Na Plasticidade Neural Na Depressãoprofessor do valeNo ratings yet
- Effect of Nadi Shuddhi Pranayama On Perceived Stress and Cardiovascular Autonomic Functions in 1st Year Undergraduate Medical StudentsDocument6 pagesEffect of Nadi Shuddhi Pranayama On Perceived Stress and Cardiovascular Autonomic Functions in 1st Year Undergraduate Medical StudentsBabuNo ratings yet
- Physical ExamDocument25 pagesPhysical Examlady birdNo ratings yet
- Handheld RelaxationDocument8 pagesHandheld RelaxationSiska Prima OlimvianiNo ratings yet
- Holy Angel University: School of Nursing and Allied Medical SciencesDocument2 pagesHoly Angel University: School of Nursing and Allied Medical SciencesMichal VillanuevaNo ratings yet
- AP Psychology Chapter 3 Notes: Biopsychology NeuroanatomyDocument5 pagesAP Psychology Chapter 3 Notes: Biopsychology NeuroanatomyKloie WalkerNo ratings yet
- Respiratory System ExplainedDocument48 pagesRespiratory System ExplainedMary Jane LubricoNo ratings yet
- Blood CoagulationDocument10 pagesBlood CoagulationgauravkokraNo ratings yet