Professional Documents
Culture Documents
Optic Neuritis
Uploaded by
Chikita Artia Sari0 ratings0% found this document useful (0 votes)
168 views25 pagesOptic neuritis is inflammation of the optic nerve that causes painless vision loss. It is usually unilateral and affects young women most commonly. Symptoms include sudden vision loss, eye pain on movement, and visual field defects. Signs include reduced visual acuity, afferent pupillary defect, and sometimes optic disc swelling. The diagnosis is based on symptoms and signs, and testing is done to rule out other causes or assess risk of multiple sclerosis. Treatment involves steroids to reduce inflammation and speed recovery, though vision often improves on its own over weeks. Left untreated, most patients recover significant vision but some experience permanent visual defects.
Original Description:
OPTIC NEURITIS
Original Title
OPTIC NEURITIS
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentOptic neuritis is inflammation of the optic nerve that causes painless vision loss. It is usually unilateral and affects young women most commonly. Symptoms include sudden vision loss, eye pain on movement, and visual field defects. Signs include reduced visual acuity, afferent pupillary defect, and sometimes optic disc swelling. The diagnosis is based on symptoms and signs, and testing is done to rule out other causes or assess risk of multiple sclerosis. Treatment involves steroids to reduce inflammation and speed recovery, though vision often improves on its own over weeks. Left untreated, most patients recover significant vision but some experience permanent visual defects.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
168 views25 pagesOptic Neuritis
Uploaded by
Chikita Artia SariOptic neuritis is inflammation of the optic nerve that causes painless vision loss. It is usually unilateral and affects young women most commonly. Symptoms include sudden vision loss, eye pain on movement, and visual field defects. Signs include reduced visual acuity, afferent pupillary defect, and sometimes optic disc swelling. The diagnosis is based on symptoms and signs, and testing is done to rule out other causes or assess risk of multiple sclerosis. Treatment involves steroids to reduce inflammation and speed recovery, though vision often improves on its own over weeks. Left untreated, most patients recover significant vision but some experience permanent visual defects.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 25
OPTIC NEURITIS
Chikita Artia Sari / I 11109014
Definition
Optic neuritis, or primary inflammation of the
optic nerve, is referred to as papillitis when the
optic disc is swollen and retrobulbar neuritis
when the disc appears normal.
The most common form of optic neuritis is acute
demyelinating optic neuritis.
Epidemiology
The annual incidence of optic neuritis, as
estimated in population-based studies, is
approximately 35 per 100,000 per year, while
the prevalence is 115 per 100,000.
The majority of patients who develop optic
neuritis are between the ages of 20 and 50
years.
77% of the patients were women, 85% were
white, and the mean age was 32 7 years.
Symptoms
Painless loss of vision over hours to days. Vision
loss can be subtle or profound.
Reduced visual acuity, colour and contrast
vision.
Usually unilateral, but may rarely be bilateral.
More often affecting females aged between 18-
45.
Orbital pain usually associated with eye
movement.
May have other focal neurological symptoms.
Ocular Manifestasions
Loss of vision in patients with acute
demyelinating optic neuritis is usually abrupt and
occurs over several hours to days.
Progression for more than one week or failure of
recovery to begin within four weeks is possible
but suggests an alternative underlying cause.
Visual loss is usually monocular, although
occasionally both eyes are affected
simultaneously, particularly in children.
Ocular Manifestasions
Mild pain in or around the eye is present in more
than 90% of patients. Such pain may precede or
occur concomitantly with visual loss, is usually
exacerbated by eye movement, and generally
lasts no more than a few days.
The presence of pain, particularly on eye
movement, is a helpful (although not definitive)
clinical feature that differentiates acute
demyelinating optic neuritis from nonarteritic
anterior ischemic optic neuropathy (AION)
Ocular Manifestasions
The severity of visual loss varies from a mild
visual field defect to severe loss of central acuity
(3% of ONTT participants had no light
perception, and 90% described at least some
loss of central acuity).
Severe loss of visual acuity is more common in
children.
Color vision and contrast sensitivity are impaired
in almost all cases, often out of proportion to
visual acuity.
Visual field loss, which may be diffuse (48%) or
focal (i.e. nerve fiber bundle defects, central or
cecocentral scotomas, hemianopic defects), is
also common in acute optic neuritis.
Ocular Manifestasions
Altitudinal defects (focal visual field loss above or
below the horizontal meridian) are less common
and should prompt consideration of a diagnosis
of anterior ischemic optic neuropathy (AION).
Low-contrast letter acuity has recently emerged
as a very sensitive test for optic neuropathy.
An afferent pupillary defect (APD) is detected in
almost all unilateral cases of optic neuritis. If an
APD is not present, a pre-existing optic
neuropathy in the fellow eye must be suspected.
Ocular Manifestasions
In fact, asymptomatic visual dysfunction is fairly
common among fellow eyes of patients who
have apparent unilateral optic neuritis.
The optic disc appears normal in approximately
two thirds of adults with acute demyelinating
optic neuritis (retrobulbar optic neuritis), while
disc swelling is present in about one third of adult
cases (papillitis); children with optic neuritis
experience optic disc swelling more frequently
than do adults.
Signs
Relative Afferent Pupillary Defect (RAPD)
Decreased visual acuity.
Decreased colour vision.
+/- Patchy visual field defects.
+/-Swollen optic disc.
May have other focal neurological signs.
Funduscopic features of optic disc swelling
include elevation of the optic nerve head, disk
hyperemia, blurring of the disc margins, and
edema of the nerve fiber layer.
Diagnosis
Based on an appropriate history (typical versus
atypical course) and clinical signs and symptoms
as described above.
Diagnostic tests, including magnetic resonance
imaging (MRI), cerebrospinal fluid (CSF)
analysis, and serological studies, usually are
performed for the following reasons:
o To determine if the cause is noninflammatory
(such as a compressive lesion), or a
nonidiopathic inflammatory or infectious process
in cases that are not typical for acute
demyelinating optic neuritis.
o To determine the prognosis or risk for
subsequent development of MS in
monosymptomatic cases for which the history
and clinical signs are typical.
Investigation and Management
Complete ophthalmic and neurological
examination.
Blood count/Erythrocyte Sedimentation Rate
(ESR).
Urgent referral to ophthalmologist - immediate
consult by phone - may be indicated for further
MRI investigation and intravenous steroid
treatment may be required.
There are NO indications for oral cortico-steroids
as initial treatment.
Differential Diagnosis
Anterior ischemic optic
neuropathy
Tumor
Aneurysm
Vasculitis
Neuroretinitis
Metastatic carcinoma
Lymphoreticular
disorder
Sinusitis
Granulomatous
inflammation
Leber's hereditary optic
neuropathy (although
always bilateral, this
frequently presents
initially with visual loss
in only one eye)
Pathology
Although the exact underlying cause is unknown,
the pathophysiology of acute optic neuritis and
MS is that of primary inflammatory
demyelination.
Very little is written about the pathology of
isolated optic neuritis, and no autopsy data
have been reported.
The inflammatory response in MS plaques is
marked by perivascular cuffing, T cells, and
plasma cells.
Although MS, itself, previously was thought to be
exclusively a disease of myelin with sparing of
nerve axons, neuronal and axonal loss have
been demonstrated to occur pathologically
Idiopathic Demyelinative Optic
Neuritis
In adults, idiopathic demyelinative optic neuritis
is usually unilateral and occurs chiefly in women
(about 3:1), with onset mostly in the third or
fourth decade of life.
It has been reported to be associated with
multiple sclerosis in up to 85% of cases,
depending on several factors, including gender,
racial origin, and duration of follow-up.
Optic neuritis affects both eyes simultaneously
and produces papillitis more commonly in
children than in adults, but the risk of progression
to multiple sclerosis is lower in children.
Idiopathic Demyelinative Optic
Neuritis
Steroid therapy
intravenously (methylprednisolone, 1 g/d for 3
days with or without a subsequent tapering
course of oral prednisolone)
orally (methylprednisolone, 500 mg/d to 2 g/d for
35 days with or without subsequent oral
prednisolone, or prednisolone, 1 mg/kg/d tapered
over 1021 days)
retrobulbar injectionprobably accelerates
recovery of vision but does not influence the
ultimate visual outcome.
Idiopathic Demyelinative Optic
Neuritis
Without treatment, vision characteristically
begins to improve 23 weeks after onset and
sometimes recovers within a few days.
Improvement may continue slowly over many
months, with recovery of acuity to 20/40 or better
occurring in over 90% of cases at both 1 year
and 10 years from onset, providing that there are
no further episodes of optic neuritis.
Idiopathic Demyelinative Optic
Neuritis
Poorer vision during the acute episode is
correlated with poorer visual outcome, but even
loss of all perception of light can be followed by
recovery of acuity to 20/20.
A poor visual outcome is also associated with
longer lesions in the optic nerve, especially if
there is involvement of the nerve within the optic
canal.
In very severe or recurrent cases, a chalky white
disk with sharp outlines results, although disk
pallor does not necessarily correlate with poor
visual acuity.
Multiple Sclerosis
Multiple sclerosis is typically a chronic relapsing
and remitting demyelinating disorder of the
central nervous system.
Some patients develop a chronically progressive
form of the disease, either following a period of
relapses and remissions (secondary progressive)
or, less commonly, from the outset (primary
progressive).
Onset is usually in young adult life; this disease
rarely begins before 15 years or after 55 years of
age.
Multiple Sclerosis
There is a
tendency to involve
the optic nerves
and chiasm,
brainstem,
cerebellar
peduncles, and
spinal cord,
although no part of
the central nervous
system is
protected.
The peripheral
nervous system is
seldom involved.
Multiple Sclerosis
Steroid treatment, usually oral or intravenous
methylprednisolone, is useful in hastening
recovery from acute relapses but does not
influence the final disability or the frequency of
subsequent relapses.
Interferon and glatiramer acetate (copolymer 1)
reduce the rate and severity of relapses and slow
the progression of brain MRI abnormalities.
Mitoxantrone, a chemotherapeutic agent, and
monoclonal antibody therapy have produce
encouraging results for progressive and
recalcitrant relapsing-remitting disease.
Optic Neuropathy
Optic neuropathy in systemic lupus
erythematosus may be immune-mediated, with
features of inflammatory disease, or due to small
blood vessel occlusion, with features of ischemic
disease (see below).
Such disease occurring in individuals in whom no
evidence of sarcoidosis or other systemic
disease can be identified is known as idiopathic
granulomatous optic neuropathy or chronic
relapsing inflammatory optic neuropathy
(CRION).
Neuromyelitis Optica
Neuromyelitis optica (Devic's disease) is a rare
syndrome characterized by usually bilateral optic
neuritis and transverse myelitis.
Approximately 50% of patients progress to death
within the first decade due to the paraplegia, but
the remainder may have a prolonged remission
and, ultimately, a better prognosis than patients
with multiple sclerosis.
THANK YOU
You might also like
- ParticipantCaseWorksheets 072018Document11 pagesParticipantCaseWorksheets 072018Saul0% (7)
- Persuasive Speech Outline CFDocument4 pagesPersuasive Speech Outline CFThanh Trần100% (1)
- FC Ophth (SA) Primary IA Past Papers - 2019 1st Semester 18-3-2019Document2 pagesFC Ophth (SA) Primary IA Past Papers - 2019 1st Semester 18-3-2019Richard100% (1)
- Opthamology MnemonicsDocument103 pagesOpthamology MnemonicsIzaz Khan100% (2)
- Incomitant SquintDocument41 pagesIncomitant Squintshreeja maheshwari100% (3)
- Maloy, Katherine - A Case-Based Approach To Emergency Psychiatry-Oxford University Press (2016)Document225 pagesMaloy, Katherine - A Case-Based Approach To Emergency Psychiatry-Oxford University Press (2016)Cristina Lefter100% (1)
- Optic Neuritis: DR Rishi JhalaniDocument64 pagesOptic Neuritis: DR Rishi JhalaniRishi Jhalani100% (1)
- Astigmatism, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandAstigmatism, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Diabetic Retinopathy: From Diagnosis to TreatmentFrom EverandDiabetic Retinopathy: From Diagnosis to TreatmentRating: 3 out of 5 stars3/5 (3)
- NystagmusDocument22 pagesNystagmusKarolina Chandra100% (1)
- StrabismusDocument27 pagesStrabismuspason1988No ratings yet
- StrabismusDocument31 pagesStrabismusalma palupi100% (1)
- 12 Kasper Notes 2020 OphthalmologyDocument33 pages12 Kasper Notes 2020 OphthalmologyMohamed Rikarz Ahamed RikarzNo ratings yet
- Pterygium Ambreen ppt1Document87 pagesPterygium Ambreen ppt1Syeda F AmbreenNo ratings yet
- Periorbital and Orbital CellulitisDocument51 pagesPeriorbital and Orbital CellulitisJoanne BlancoNo ratings yet
- Neuro-Ophthalmology: DR Jusuf Wijaya, SPM FK - Uki CawangDocument65 pagesNeuro-Ophthalmology: DR Jusuf Wijaya, SPM FK - Uki CawanggeorgyNo ratings yet
- 432 OSCE Revision File PDFDocument20 pages432 OSCE Revision File PDFReza Affandi MohamadNo ratings yet
- AAO - External Disease and CorneaDocument19 pagesAAO - External Disease and CorneaJohn Paul VillaflorNo ratings yet
- Diseases of Lens DR D.JLDocument113 pagesDiseases of Lens DR D.JLNithya GunasekaranNo ratings yet
- AION Anterior Ischemic Optic Neuropathy AIONDocument22 pagesAION Anterior Ischemic Optic Neuropathy AIONNyak Rahmat100% (1)
- Vernal Keratoconjunctivitis: Moderator-Dr. Seema Meena Presenter - Dr. Sulabh SahuDocument58 pagesVernal Keratoconjunctivitis: Moderator-Dr. Seema Meena Presenter - Dr. Sulabh SahuSulabh SahuNo ratings yet
- Ophthalmology Board Review Notes: Intermediate and Posterior UveitisDocument12 pagesOphthalmology Board Review Notes: Intermediate and Posterior Uveitissharu4291No ratings yet
- Case Based Ophthalmology GuideDocument12 pagesCase Based Ophthalmology GuideGradestack100% (2)
- 2735 Pediatric Cataract Manual - CompressedDocument66 pages2735 Pediatric Cataract Manual - CompressedKevin RamsahaiNo ratings yet
- MCQ From 14046Document66 pagesMCQ From 14046deevannNo ratings yet
- Congenital CataractDocument40 pagesCongenital CataractRaymonde UyNo ratings yet
- Optical Coherence Tomography (OCT) in Neurologic DiseasesDocument232 pagesOptical Coherence Tomography (OCT) in Neurologic DiseasesirodalexandraNo ratings yet
- Memorize ophtha layers, structures, and diseasesDocument51 pagesMemorize ophtha layers, structures, and diseasesPatryk Dionisio100% (1)
- Seizures and EpilepsyDocument76 pagesSeizures and EpilepsyManoj GhimireNo ratings yet
- Laban - Sub Kamal Salman Mahmoud Jaber Mustafa: Done byDocument40 pagesLaban - Sub Kamal Salman Mahmoud Jaber Mustafa: Done byKool Kaish100% (1)
- Ophtha SGD 1Document4 pagesOphtha SGD 1Richelle IgnacioNo ratings yet
- Ophthalmology QuizDocument45 pagesOphthalmology QuizLana LocoNo ratings yet
- Ophthalmology MnemonicsDocument4 pagesOphthalmology MnemonicsMuhammad Luqman Nul HakimNo ratings yet
- Glaucoma and LensDocument4 pagesGlaucoma and Lenssarguss14No ratings yet
- Retinal Drawing A Lost Art of MedicineDocument3 pagesRetinal Drawing A Lost Art of MedicinekavyaNo ratings yet
- Ophthalmology NotesDocument22 pagesOphthalmology NotesdrusmansaleemNo ratings yet
- Ophthalmology 0201B Blurring3Document11 pagesOphthalmology 0201B Blurring3Rea Dominique CabanillaNo ratings yet
- StrabismusDocument56 pagesStrabismusraniNo ratings yet
- Regulations Relating To The Surgical Fellowship Examination in Ophthalmology Parts 1, 2 and 3Document13 pagesRegulations Relating To The Surgical Fellowship Examination in Ophthalmology Parts 1, 2 and 3NoorNo ratings yet
- External Disease and CorneaDocument105 pagesExternal Disease and CorneaNova CiNg CiNgNo ratings yet
- Neurology TipsDocument455 pagesNeurology TipsAsad Khan KhalilNo ratings yet
- KERATOCONUSDocument22 pagesKERATOCONUSAarush DeoraNo ratings yet
- Pediatric OpthDocument10 pagesPediatric OpthZaher Al ObeydNo ratings yet
- Basic Sciences in Ophthalmology - 9788184486087-EmailDocument446 pagesBasic Sciences in Ophthalmology - 9788184486087-EmailwulanfarichahNo ratings yet
- Ospe Ophthalmology CorrectedDocument55 pagesOspe Ophthalmology CorrectedGgah Vgggagagsg100% (1)
- Congenital Nasolacrimal Duct ObstructionDocument43 pagesCongenital Nasolacrimal Duct ObstructionAnumeha JindalNo ratings yet
- College of Medicine and Health Science, Department of OptometryDocument47 pagesCollege of Medicine and Health Science, Department of Optometryhenok birukNo ratings yet
- Hypertensive RetinopathyDocument46 pagesHypertensive RetinopathyAnadia RahmaNo ratings yet
- Blurring of Vision Ii: Retinal Vascular Disorders: Dr. Jose BondocDocument15 pagesBlurring of Vision Ii: Retinal Vascular Disorders: Dr. Jose BondocRea Dominique CabanillaNo ratings yet
- Case Reviews in Ophthalmology Expert Consult - OnlDocument2 pagesCase Reviews in Ophthalmology Expert Consult - Onldr. mostakNo ratings yet
- Fundus Examination PDFDocument125 pagesFundus Examination PDFAravind Kumar100% (5)
- Understand NystagmusDocument2 pagesUnderstand NystagmusVera DianwariNo ratings yet
- Case of A.D.G.: San Beda University - College of Medicine Bautista, Bayona, Boñula Ophthalmology RotationDocument18 pagesCase of A.D.G.: San Beda University - College of Medicine Bautista, Bayona, Boñula Ophthalmology RotationRonel MarkNo ratings yet
- Tele-Ophthalmology: By-Abhishek Yadav Optometrist Dr. R.P. Centre For Ophthalmic Sciences AiimsDocument11 pagesTele-Ophthalmology: By-Abhishek Yadav Optometrist Dr. R.P. Centre For Ophthalmic Sciences AiimsAbhishek Yadav0% (1)
- Hyphema 140917144203 Phpapp02thsDocument20 pagesHyphema 140917144203 Phpapp02thsYuda Arie DharmawanNo ratings yet
- Eye Docs RetinaDocument279 pagesEye Docs RetinaRahul LokhandeNo ratings yet
- Notes To Remember: For Clinical Ophthalmology MCQ ExamsDocument89 pagesNotes To Remember: For Clinical Ophthalmology MCQ ExamsMohamed Gaber100% (1)
- I Notes StrabismusDocument92 pagesI Notes StrabismusPrincess EzzlynnNo ratings yet
- Degenerative MyopiaDocument53 pagesDegenerative MyopiaNiloy BasakNo ratings yet
- Anti VEGF Therapy in OphthalmologyDocument27 pagesAnti VEGF Therapy in OphthalmologyAtreyee Bhattacharya100% (3)
- I Notes Ophthalmology PDFDocument690 pagesI Notes Ophthalmology PDFpriya arrachman0% (1)
- Cranial NervesDocument67 pagesCranial NervesBahaa ShaabanNo ratings yet
- Retinopathy of Prematurity Definition, Stages, Risk Factors and ManagementDocument20 pagesRetinopathy of Prematurity Definition, Stages, Risk Factors and ManagementChikita Artia SariNo ratings yet
- Hypertensive RetinopathyDocument27 pagesHypertensive RetinopathyChikita Artia SariNo ratings yet
- Diabetic RetinopathyDocument12 pagesDiabetic Retinopathyc4rm3LNo ratings yet
- Nopi PRDocument1 pageNopi PRChikita Artia SariNo ratings yet
- Daftar PustakaDocument4 pagesDaftar PustakaChikita Artia SariNo ratings yet
- Case Report Mature Cataract: Created By: Chikita Artia Sari I 11109014Document1 pageCase Report Mature Cataract: Created By: Chikita Artia Sari I 11109014Chikita Artia SariNo ratings yet
- Cover 2Document1 pageCover 2Chikita Artia SariNo ratings yet
- Retinal Detachment Causes, Symptoms, and TreatmentDocument14 pagesRetinal Detachment Causes, Symptoms, and TreatmentChikita Artia Sari100% (1)
- Daftar PustakaDocument4 pagesDaftar PustakaChikita Artia SariNo ratings yet
- ROP Screening, Stages, Treatment and PreventionDocument16 pagesROP Screening, Stages, Treatment and PreventionChikita Artia SariNo ratings yet
- Lembar PersetujuanDocument1 pageLembar PersetujuanChikita Artia SariNo ratings yet
- Dia Care-2005-Boulton-956-62 PDFDocument7 pagesDia Care-2005-Boulton-956-62 PDFChikita Artia SariNo ratings yet
- Diagnosis and Management of Red EyeDocument8 pagesDiagnosis and Management of Red EyeNelly AstikaNo ratings yet
- EPISCLERITIS & ScleritisDocument14 pagesEPISCLERITIS & ScleritisChikita Artia SariNo ratings yet
- Cover Journal ResumeDocument1 pageCover Journal ResumeChikita Artia SariNo ratings yet
- Photophobia in Viral Conjunctivitis: Homework Ophtalmology DepartementDocument1 pagePhotophobia in Viral Conjunctivitis: Homework Ophtalmology DepartementChikita Artia SariNo ratings yet
- PSSS - Red Eyes With Visual LossDocument33 pagesPSSS - Red Eyes With Visual LossChikita Artia SariNo ratings yet
- 2007 Primary Open Glaucoma and MyopiaDocument7 pages2007 Primary Open Glaucoma and MyopiaChikita Artia SariNo ratings yet
- PSSS - Red Eyes With Visual LossDocument33 pagesPSSS - Red Eyes With Visual LossChikita Artia SariNo ratings yet
- Daftar PustakaDocument4 pagesDaftar PustakaChikita Artia SariNo ratings yet
- Patogenesis Retinopati DiabetikumDocument1 pagePatogenesis Retinopati DiabetikumChikita Artia SariNo ratings yet
- Retinal Detachment and PeripheralDocument41 pagesRetinal Detachment and PeripheralAkhmad FauzanNo ratings yet
- Dia Care-2005-Boulton-956-62 PDFDocument7 pagesDia Care-2005-Boulton-956-62 PDFChikita Artia SariNo ratings yet
- Optic Neuritis 07 - 11 - 12 - FINAL PDFDocument4 pagesOptic Neuritis 07 - 11 - 12 - FINAL PDFChikita Artia SariNo ratings yet
- CataractDocument12 pagesCataractChikita Artia SariNo ratings yet
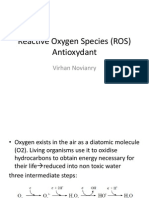
- Reactive Oxygen Species (ROS) KJPDocument24 pagesReactive Oxygen Species (ROS) KJPAbdul Fahma FirmanaNo ratings yet
- Association of Vascular Endothelial Growth FactorDocument5 pagesAssociation of Vascular Endothelial Growth FactorChikita Artia SariNo ratings yet
- Glycemic Thresholds For Diabetes-Speci CDocument6 pagesGlycemic Thresholds For Diabetes-Speci CChikita Artia SariNo ratings yet
- Association of Vascular Endothelial Growth FactorDocument5 pagesAssociation of Vascular Endothelial Growth FactorChikita Artia SariNo ratings yet
- Steroids Drug ListDocument2 pagesSteroids Drug ListJezKagandahanNo ratings yet
- Sugarcane DiseasesDocument6 pagesSugarcane DiseasesNkanyisoNo ratings yet
- Dah011 BFD Livestock Diseases (PPP Sept 2021)Document672 pagesDah011 BFD Livestock Diseases (PPP Sept 2021)Kevin KagambiNo ratings yet
- WEANING FROM MECHANICAL VENTILATION GUIDEDocument55 pagesWEANING FROM MECHANICAL VENTILATION GUIDEKamal Mohamed100% (1)
- 12 Physical Education Chapter 3Document24 pages12 Physical Education Chapter 3akanksha nayanNo ratings yet
- Medical MarijuanaDocument4 pagesMedical MarijuanaDanielZepedaPereaNo ratings yet
- Childhood Asthma Prediction Model Using SVMDocument9 pagesChildhood Asthma Prediction Model Using SVMajextopeNo ratings yet
- Concept MapDocument2 pagesConcept MapRAYAMAE LUMOGDANGNo ratings yet
- ICT Project: "Curbing Malnutrition Among Filipino Children"Document7 pagesICT Project: "Curbing Malnutrition Among Filipino Children"Janea ArinyaNo ratings yet
- Ardy TinitusDocument4 pagesArdy TinitusArdy SantosoNo ratings yet
- DALY Ischaemic and Rheumatic Diseases Country WiseDocument23 pagesDALY Ischaemic and Rheumatic Diseases Country Wisesagvid25No ratings yet
- Assessment Exam in Cc2and3Document7 pagesAssessment Exam in Cc2and3mika de guzmanNo ratings yet
- The World Healthiest Foods Part III - FruitsDocument39 pagesThe World Healthiest Foods Part III - FruitsKyle J. NortonNo ratings yet
- Ineffective Airway ClearanceDocument2 pagesIneffective Airway ClearanceMaria ArregoitiaNo ratings yet
- Avoiding Back Pain in Bus and Coach DriversDocument4 pagesAvoiding Back Pain in Bus and Coach DriversNur HasanahNo ratings yet
- Writing Project 3-5Document10 pagesWriting Project 3-5api-456365943No ratings yet
- Internal Medicine Board ReviewDocument64 pagesInternal Medicine Board Reviewgrahamabra50% (2)
- Epidemiology of Diabetes MellitusDocument5 pagesEpidemiology of Diabetes Mellitusarkanthos77No ratings yet
- Dr. Jean Dodds Expert Report (Plaintiff)Document2 pagesDr. Jean Dodds Expert Report (Plaintiff)Osiris-KhentamentiuNo ratings yet
- Nutrition ManualDocument405 pagesNutrition ManualRaghavendra Prasad100% (1)
- Agbede DanielDocument18 pagesAgbede DanielDaniel AgbedeNo ratings yet
- Carte SemioDocument279 pagesCarte SemioJoão Vitor LacerdaNo ratings yet
- PorphyriaDocument17 pagesPorphyriaSotir LakoNo ratings yet
- Healthy Gut SummitDocument1 pageHealthy Gut Summitgreym111No ratings yet
- Types Causes Signs and Symptomps Intellectual DisabilityDocument2 pagesTypes Causes Signs and Symptomps Intellectual DisabilityMae Ann Jean JustolNo ratings yet
- Z Benefits Capsule Mar 19 2014Document20 pagesZ Benefits Capsule Mar 19 2014Richard SonsingNo ratings yet
- Case Study Bactegroup 3Document19 pagesCase Study Bactegroup 3Marjune DimayugaNo ratings yet