Professional Documents
Culture Documents
Ketogenic Diet - An Intro
Uploaded by
py80100%(1)100% found this document useful (1 vote)
955 views62 pagesA intro to what is Ketogenic Diet and its role for therapeutic seizure control in paediatric patient.
Original Title
Ketogenic Diet – an Intro
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentA intro to what is Ketogenic Diet and its role for therapeutic seizure control in paediatric patient.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
100%(1)100% found this document useful (1 vote)
955 views62 pagesKetogenic Diet - An Intro
Uploaded by
py80A intro to what is Ketogenic Diet and its role for therapeutic seizure control in paediatric patient.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 62
Ketogenic Diet
Dr Tan Pek Yong
Case Illustration 1
YJW, 14 year old, healthy girl
No known medical illness
Presented with refractory status epilepticus
for 1 month in the context of fever
All investigation including CSF sampling, MRI
brain was normal.
Diagnosis : FIRES
On admission to GICU:
On Thiopentone,
Propofol, Midazolam
& multiple AED
Ketogenic Diet
After 1 week of Ketogenic diet
After 3 week of Ketogenic diet
After 6 week of Ketogenic diet
(extubated !!)
Case Illustration 2
NAD, 14 mths old girl
Presented with epileptic encephalopathy with
underlying GDD, central hypotonia and subtle
dysmorphism.
All genetic and IEM screening normal.
MRI brain show mild lost of white matter
(non-specific)
EEG epileptic encephalopathy
Ketogenic Diet
EEG marked improvement after 2 3 wks of KD
Ketogenic Diet
What is Ketogenic diet?
A therapeutic diet for epilepsy
High fat, low protein and low carbohydrate
diet, with calorie control
The goal: alter the bodys fuel source from
glucose to fat.
A Story from
A Parents Prespective
Sam, 9 years old
Diagnosed to have myoclonic epilepsy at age
of 5 but was able to control with AED
Had absence seizure since 7 which was very
difficult to control
Tried 11 antiepileptic drugs
Had 100-130 seizures per day
A Parents Prespective
Sam couldnt even cry without interruption:
he would cry for 15 seconds; have a 15-second
seizure; and then continue sobbing.
Sam had trouble even watching a movie.
Dad, I think the DVD is scratched. When I was
watching, it kept leaving words out.
Ketogenic Diet
Breakfast: eggs are mixed with heavy cream and served
with bacon.
Lunch: full-fat Greek yogurt mixed with coconut oil.
Dinner:hot dogs, bacon, macadamia nuts and cheese.
An average week, Sam consumes a quart and a third of
heavy cream, nearly a stick and a half of butter, 13
teaspoons of coconut oil, 20 slices of bacon and 9 eggs.
That is twice the fat content of a McDonalds Happy Meal
and about 25 percent more than the most fat-laden phase
of the Atkins diet.
A Parents Prespective
Time consuming to prepare keto meals
Doing all this once is fascinating.
But administering the diet for three meals and
two snacks a day, seven days a week for two years
is relentless.
There is no Lets just order pizza, no matter how
busy.
A Parents Prespective
To deal with childs craving for common snacks
Ice cream, pizza, candy, cake, cookies, tortilla chips
and soda and the list goes on......
A Parents Prespective
Ultimately what makes the diet so stressful is that on
top of all the gross recipes and weird mechanics, there
is no margin for error.
Every last drop counts and that is from food
preparation till the child finish every bite of every
meal.
The penalty for cheating, at least in Sams case, is
seizures.
took a piece of toast: lost seizure control for a week.
Does it work?
For Sam:
After 2 years on ketogenic diet
75% reduction in seizure
Effectiveness
20-25% seizures were completely controlled
30-40% - seizure frequency decreased by 50%
25-30% - not effective
Ketogenic Diet
History
Ancient Greece
Biblical times
1920s at Johns Hopkins University School of
Medicine.
Popularity faded in the 40s and 50s when new
anticonvulsant drugs were discovered
Resurgence in 1990s because of the TV movie
based on Charlie Abrahams
Charlie Foundation funded a 7-center study of the diet
designed to allow these centers to treat the patients resulting
from the anticipated publicity.
The multicenter study was started in 1994 and presented to
the American Epilepsy Society in 1996.
This later lead to an exponential increase in number of
publications on KD.
Who is it for?
For children with poorly controlled seizures or failed to
respond to AEDs.
Emerging evidence:
Severe myoclonic epilepsy of infancy (Dravet syndrome)
Myoclonic astatic epilespy
Tuberous sclerosis complex
Infantile spasms
Uncontrolled absence seizures
Metabolic disease:
Glucose Transporter 1 Deficiency syndrome Rx of choice
Pyruvate dehydrogenase (PDH) deficiency
Contraindication / Caution
Contraindicated, or caution should be exercised for those with:
Fatty acid oxidation defects
Organic acidurias
Diagnosis of diabetes mellitus
Hypoglycaemia under investigation
Familial hyperlipidaemia
Severe gastro oesophageal reflux
Feeding difficulties or food refusual
How does it work?
Glucose Fat (as the primary fuel source)
Ketone bodies the acidic products formed
from excessive breakdown of fat.
The brain uses the ketones as fuel.
No one knows why this works!
Before starting KD
Initial assessment by Paediatric Neurologist
experienced in KD
Types of Seizures
Frequency and type of seizures must be documented
for one month prior to commencing the ketogenic diet
and throughout the course of the diet.
The neurologist will review medications before the
diet is commenced, changing syrup medications to
tablet form, due to their high sugar content.
Before starting KD
Education and commitment by parents
Areas covered include:
Aims of the diet,
How the diet works,
The advantages and disadvantages of the diet,
How the diet is calculated,
Examples of the types of meals a child would eat on the diet,
Duration of diet,
Admission process and
Ongoing management at home
Cost of KD
Family Expectation
How long to know its effect?
How long to go on with KD?
Seizure reduction?
What about AED reduction?
What about improvement in cognition?
Initiating KD
Hospitalization to induce ketosis
Under the supervision of Paeds Neurologist
and trained dietician
Blood sugar and ketone levels monitored
Baseline Ix:
FBC / RP / LFT / FLP / Ufeme
Initiating KD
Start with ketogenic formula, encourage to drink
more water
If ketosis is being established and the ketogenic
formula tolerated, food is introduced after a 48 hour
period until the calculated ratio and energy level is
reached.
The dietitian calculates all energy requirements and
grades the fat ratio up slowly.
Calculation of KD
The ketogenic ratio 4:1
Calculate the # of calories needed a day
(based on RDAs)
Fortunately leave it to the DIETICIAN!!!
Ketogenic Ratio
Ratio of fat to protein plus carbohydrate in the diet.
(by weight, not calories)
The ratio determines how "ketogenic" the diet is - the higher
the ratio, the more ketogenic (ie stronger) the diet.
Typical ketogenic diets are operated in the range from 2:1 to
5:1.
By comparison, a normal everyday diet has a ketogenic ratio
in the range 1:2 to 1:3.
Sample Meals
Meal 1:
melted butter
heavy whipping cream
chicken
apple
sugar free Jell-O
Meal 2:
Hot dog slices w/ sugar-free catsup
Asparagus w/ butter
Chopped lettuce w/ mayo
Sugar-free vanilla cream popsicle
Variations of the Diet
MCT oil
MCT oil is more "ketogenic", it is possible to increase
the levels of carbohydrate and protein, and still
achieve the basic objective of the diet which is the
body going into ketosis.
The increase in carbohydrates and protein enables a
wider range of foods within the diet, so it looks more
like a normal diet.
More and more studies show that there is no
difference in efficacy on both diet as long as
calculations are correct.
Variations of the Diet
Modified Atkins diet
No fluid or calorie restriction.
Fats are strongly encouraged, but no restrictions on
proteins.
Foods are not weighed and measured, but
carbohydrate counts are monitored.
Foods can be eaten more freely in restaurants and
outside the home, and families can do it as well.
Modified" = allow for less carbohydrates than
traditional Atkins (10-20g/day) and more strongly
encourages fat intake.
Supplementation
Calcium & Vitamins
Adequate fluids
carnitine
laxatives
Maintenance of the Diet
All medications are continued
Constant calculations!
BE VERY PRECISE!
Watch for cheating!
Special toothpaste
No added seasonings
Problems that may arise
Low blood sugar
Lethargy
Nausea
Vomiting
Elevated cholesterol
Kidney stones
Constipation
Weight loss or gain
Dehydration
Cheating
Side Effects
Metabolic
Hyperuricemia (2%26%)
Hypocalcemia (2%)
Hypomagnesemia (5%)
Decreased amino acid levels and acidosis (2%5%)
Gastrointestinal symptoms
vomiting, constipation, diarrhea, and abdominal pain occur in 12%50% of children
Carnitine
Hypercholesterolemia (14%59%)
Renal calculi (3%7%)
Stone composition includes uric acid (50% of stones), calcium oxalate, calcium phosphate, and
mixed calcium/uric acid stones.
They typically do not require diet discontinuation and lithotripsy is only rarely necessary.
Polycitra K appears to help prevent stone formation
Side Effects
There is conflicting data on the effect of the KD on growth in children.
One retrospective review of linear growth found that 86% of children on the
diet had slowed growth.
A prospective study of 237 children found that the while older children grew
almost normally; younger children grew poorly.
There does not appear to be a difference between diets used despite the
greater protein content of the MCT diet.
Cardiac abnormalities (rare)
cardiomyopathy and prolonged QT interval
Long Term Side Effects
> 2 years on KD
higher risk of bone fractures, kidney stones, and
decreased growth, but dyslipidemia was not identified
Periodic dual energy x-ray absorptiometry (DEXA)
screening for bone health recommended.
The long-term effects of this high-fat diet on the
cardiovascular system remain to be determined.
Advantages & Disadvantages
It works for many
children!
Frequently medications
are greatly decreased or
discontinued.
VERY STRICT!
Long duration
Stunted Growth?
Heart Problems?
Discontinuation
Unsuccessful: consider stopping after 3 months
Sussessful: consider stopping after 2 years
Longer diet durations are necessary for GLUT-1 and PDHD.
Before discontinuation in seizure-free children, a routine
EEG and review of clinical data should be performed to
counsel families regarding recurrence risk, which is 20%
overall.
Children with an epileptiform EEG, abnormal MRI, and
tuberous sclerosis complex are at higher risk.
Trouble Shooting
Hypoglycaemia
Treating hypoglycaemia using rapidly absorbed carbohydrate
100ml of NON DIET Coca Cola
55ml of Lucozade, Energy Original
100ml of pure fruit juice
2tsp of sugar, ordinary jam, honey or syrup
10g (two level teaspoons) Dextrose powder in 100ml water.
If the response to the above treatment is inadequate, more can be
administered after 10-15 minutes.
For patients with reduced consciousness level or/and seizures
Give 5 -10ml/kg 10% dextrose intravenously
GI Illness
Vomiting or Diarrhoea
Check blood glucose levels two- to four-hourly if children are
unwell, especially if nil by mouth (note that if the child is ketotic,
blood sugar may be low but still acceptable, ie > 2.5 mmol/L.)
Test urine for ketones every time child passes urine.
Rehydrate with low carbohydrate clear fluids if tolerated orally.
If IV fluids are required use normal saline (0.9% NaCl)
Reflo < 3mmol/L - 2.5% or 5% dextrose/saline solution to maintain
Reflo between 3 and 4 mmol/l.
NBM
The high fat diet regimen of the ketogenic diet (70-90% of calories)
forces the body into a dietary induced ketosis. The acidosis that
occurs when the diet is first initiated corrects itself with days and is
not sustained.
The literature on ketogenic diet and general anaesthetic is scarce,
with very little consensus on management.
The most comprehensive study undertaken so far suggests that
carbohydrate-free solutions are safe and blood glucose remains
stable throughout surgical procedures up to 1.5 hours.
Current advice suggest therefore monitoring blood pH in
procedures > three hours and administering IV bicarbonate where
necessary.
PICU Admission
Intravenous fluids: use normal saline (0.9% NaCl) or Ringers lactate, unless blood
glucose levels are low (< 3 mmol/l).
If low then give dextrose / saline solutions (2.5% or 5%), aim to maintain blood
glucose between 3 and 4 mmol/l.
Monitor for hypoglycaemia and metabolic acidosis: blood glucose levels and blood
gas one- to two- hourly as appropriate.
Investigations should also include measurement of ketones (urine or blood),
excessive ketosis and acidosis may require treatment with iv bicarbonate
A base excess of -10 indicates significant metabolic acidosis and should be half
corrected over four hours with intravenous bicarbonate.
If acidosis is explained by excess ketosis, dextrose containing maintenance fluids (2.5% or 5 %
dextrose) would be appropriate.
If acidosis is not completely explained by excess ketosis ie high blood lactate this could be
discussed with the Metabolic team (choice of maintenance fluids (normal saline/saline).
Medication: must be in lowest carbohydrate form.
Enteral feeding: please contact dietitians
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Immunological Tolerance, Pregnancy, and Preeclampsia: The Roles of Semen Microbes and The FatherDocument39 pagesImmunological Tolerance, Pregnancy, and Preeclampsia: The Roles of Semen Microbes and The FatherAnanda Yuliastri DewiNo ratings yet
- A Case Study On Renal CancerDocument30 pagesA Case Study On Renal CancerAiyish CapunoNo ratings yet
- Ralph's ProposalDocument15 pagesRalph's ProposalHeilene Ethel AngcayaNo ratings yet
- Complication PopDocument16 pagesComplication PopkristinNo ratings yet
- Notices About Filtered ResultsDocument5 pagesNotices About Filtered ResultsJoshua TerceñoNo ratings yet
- Audit On BFHIDocument40 pagesAudit On BFHIYoung MilkNo ratings yet
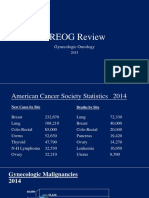
- 2015 Oncology CREOG Review PDFDocument76 pages2015 Oncology CREOG Review PDFRima HajjarNo ratings yet
- Erectile Dysfunction: Management Update: Review SynthèseDocument9 pagesErectile Dysfunction: Management Update: Review SynthèseAditya Villas-BoasNo ratings yet
- Drug Education in The PhilippinesDocument32 pagesDrug Education in The PhilippinesTrixie Ann MenesesNo ratings yet
- Pentacam GuidelineDocument43 pagesPentacam GuidelineEvelyn SepulvedaNo ratings yet
- Small For Gestational Age: I. Definition/ DescriptionDocument11 pagesSmall For Gestational Age: I. Definition/ Descriptionfaye kimNo ratings yet
- Glossopharyngeal Nerve Injury Following Tonsillectomy 5542Document4 pagesGlossopharyngeal Nerve Injury Following Tonsillectomy 5542Kenza SeddikNo ratings yet
- Guideline Elaboración de AcDocument3 pagesGuideline Elaboración de AcsilviazulNo ratings yet
- Stabilis-Monographie-Doxorubicin Hydrochloride Liposome PegDocument9 pagesStabilis-Monographie-Doxorubicin Hydrochloride Liposome PegSepti Marta SariNo ratings yet
- MCQDocument6 pagesMCQalirbidiNo ratings yet
- Limfoma Kutis Pada Pasien Yang Semula Di DiagnosisDocument34 pagesLimfoma Kutis Pada Pasien Yang Semula Di DiagnosisChris MulyoNo ratings yet
- Berra 2020Document12 pagesBerra 2020Indri AswariNo ratings yet
- Death Anxiety Care PlanDocument4 pagesDeath Anxiety Care PlanAaLona Robinson86% (7)
- Hepatic Encephalopathy in Adults - Treatment - UpToDateDocument8 pagesHepatic Encephalopathy in Adults - Treatment - UpToDatenaka_thanatosNo ratings yet
- SddaDocument2 pagesSddaJeny Alva RojasNo ratings yet
- DiabetesDocument12 pagesDiabetessshiffanaNo ratings yet
- Clinical Usefulness of Propofol As An Anesthetic Induction Agent in Dogs and CatsDocument3 pagesClinical Usefulness of Propofol As An Anesthetic Induction Agent in Dogs and CatsSatria Adi MarhendraNo ratings yet
- Polyphenols, and Physical PerformanceDocument7 pagesPolyphenols, and Physical PerformancezoliteamlavylitesNo ratings yet
- Doctor'S Order and Progress NotesDocument3 pagesDoctor'S Order and Progress NotesDienizs LabiniNo ratings yet
- NGT LavageDocument16 pagesNGT LavageTina Alteran100% (1)
- ICF SwallowingDocument2 pagesICF SwallowingMarcela Sanhueza GarridoNo ratings yet
- Wilcock 2008Document11 pagesWilcock 2008Nadia SaiNo ratings yet
- Shortening of A Penrose DrainDocument2 pagesShortening of A Penrose DrainHeidi Avediz Del FuerteNo ratings yet
- BTL-Aesthetics ED AE-guide-supplement EN100Document8 pagesBTL-Aesthetics ED AE-guide-supplement EN100joaquina.espinoza20No ratings yet
- Harjïa, H. C. L. (0 1 ) - Sfjdldhïa Hckcral (:a. CM.) - Japïtuld:, Páhfka : A 8 . Oæxfjd, M.E., OR7 Lardussc - Hrupd Cmftdrfal Atrfa. Pcjupcramd MCDocument7 pagesHarjïa, H. C. L. (0 1 ) - Sfjdldhïa Hckcral (:a. CM.) - Japïtuld:, Páhfka : A 8 . Oæxfjd, M.E., OR7 Lardussc - Hrupd Cmftdrfal Atrfa. Pcjupcramd MCSofia PerezNo ratings yet