Professional Documents
Culture Documents
4th SC Phar 40060-Renal-2web
Uploaded by
Doyin Awodele0 ratings0% found this document useful (0 votes)
19 views24 pagespharmacology
Original Title
4th Sc Phar 40060-Renal-2web
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentpharmacology
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
19 views24 pages4th SC Phar 40060-Renal-2web
Uploaded by
Doyin Awodelepharmacology
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 24
4th Science:40060
ARP lecture - Renal Disease
Dr. Tara McMorrow
tara.mcmorrow@ucd.ie
Tel: 01 716 6819
School of Biomolecular and Biomedical Science
Conway Institute
PHAR 40060 ARP Lecture 2: Objectives
At the end of this lecture, students should
have an understanding of the kidney in
relation to renal disease
Functional unit of the kidney - Nephron
Nephron
Tubular Vascular
component component
Approx. 1 million nephrons in each mammalian kidney
Can lose up to 75% of nephron function and renal
function will be maintained by reserve nephrons
difficult to detect damage early
Renal Disease Background:
Renal disease is a major problem world wide
Increasing incidence 80,000 new cases / year in
USA
Major causes include :
1. Diabetes
2. Hypertension
3. Glomerulonephritis
Mechanisms of development are unknown
Thus limited therapies are available
General Characteristics
Early Renal Disease: Abnormal urine volume
and/or composition
Advanced: Edema, electrolyte abnormalities,
anemia, etc.
Rate of Progression: Disease-dependent
Disease Course: Transient-fatal: Disease-
dependent
Pain: Variable, depending on nature of
disease
Kidney Sites Susceptible to Renal Disease
General: Renal medulla:
Low oxygen environment: Ischemia
Glomeruli:
Structure predisposes it to immune complex deposition
and complement fixation
Tubules
- generally involved in endstage or chronic kidney disease
Post-Renal Structures (ureters, bladder)
Malformations, Obstruction, Masses (i.e. cancer)
Acute Kidney Disease
Prerenal:
Decreased cardiac output and urine volume depletion
Drug-induced or related
Intrarenal:
Inflammatory disease
Acute tubular necrosis
Postrenal:
- Obstruction
Slow decline in kidney function
- eventually progresses to End Stage Renal
Disease (ESRD)
Generally develops as a result of another condition
- Diabetes (28%)
- Hypertension (25%)
- Glomerulonephritis (21%)
- Polycystic Kidney Disease (4%)
- Other (23%): Obstruction, infection, drugs.
Chronic Kidney Disease
Renal diseases are varied and can result from a toxic
insult or may be immune mediated
They may be classified by their location of onset -
Glomerular disease- glomerulonephritis
Tubulointerstitial disease- tubulointerstitial nephritis
Most of the conditions result in a fibrotic or sclerotic
phenotype characterised by excess extracellular matrix
deposition
Regardless of the initial insult, development of renal
fibrosis leads to end-stage renal disease and ultimately
kidney failure
Renal Disease Classification
Renal ultra-structure of normal and fibrotic tissue
(a) Normal kidney architecture displaying a normal glomerulus ( ), bowmans
space ( ), mesangial cells ( ), basement membrane ( ) supporting the tubular
epithelial cells ( ) separated by the interstitial space ( ).
(b) In the glomerular nephritis section there is an enlarged glomerulus, reduced
bowmans space, proliferating mesangial cells, an expansive interstitium and
disruption of tubular function.
(a)
(b)
Kidney Histology
Glomerular Diseases
Glomerulonephritis (GN) is one of the most important causes of
renal disease world-wide.
Examples of GN include:
1. Membranous nephritis
2. Post-infectious glomerulonephritis
3. Lupus glomerulonephritis
4. IgA Nephropathy
5. Goodpastures Syndrome
6. Diabetic Nephropathy
7. Glomerulosclerosis
Glomerulonephritis
Glomerulonephritis is the third most common
cause of end-stage renal disease after
diabetes and hypertension
Accounts for 10-15% of ESRD patients
Immunological events lead to
- complement activation
- fibrin deposition
- platelet aggregation
- inflammation
Acute Glomerulonephritis Chronic Glomerulonephritis
Glomerulonephritis:
scarring of the cortex
Tubular Diseases
The main tubular disease is tubulointerstitial
nephritis
Acute tubulointerstitial nephritis- due to
hypersensitivity reactions to drugs
Chronic tubulointerstitial nephritis- due to
drugs, diabetes, chemicals
Acute Tubulointerstitial Nephritis
Chronic Tubulointerstitial Nephritis
Tubulointerstitial
Nephritis
Progressive Renal Disease
Common histological end point:
Scarring : 1. Glomerulosclerosis
2. Tubulointerstitial Fibrosis
Pathological process resulting from insult / injury
leading to tissue dysfunction and organ failure
Fibrosis - The Final Common Pathway for renal
diseases that progress to ESRF
Level of fibrosis correlates closely with the degree of
renal dysfunction
Glomerulosclerosis
Glomerulosclerosis is a key endpoint in
progressive renal disease
Leads to scarring of the glomeruli which
cannot be repaired
Eventually leads to end stage renal disease
Tubulointerstitial fibrosis
Tubulointerstitial fibrosis is a hallmark of
progressive renal disease
Progression of chronic renal insufficiency is
closely linked to the severity of tubulointerstitial
changes
Level of proximal tubular damage also correlates
closely with the degree of renal dysfunction
FIBROSIS :
1. Increased deposition of fibronectin,
collagens
2. Increased fibroblast proliferation
3. Increase in mononuclear cells
4. Accumulation of matrix proteins :
- inadequate matrix degradation
The End-Stage Kidney
Kidney fibrosis (ESRD)
Tubulointerstitial Fibrosis is the final common pathway leading to
ESRF - correlates most closely with declining renal function
Caused by accumulation of excess extracellular matrix (ECM) in the
renal tubular interstitium
ESRD
Patients with chronic renal impairment
tend to progress to ESRD
No treatment options except renal
replacement therapy i.e. dialysis
Transplantation-long waiting lists and
strict criteria
Kidney Disease Summary
Prevalence of kidney disease
- 1 in 9 adults develop chronic kidney disease
Renal fibrosis is a common final pathway for
numerous kidney dysfunctions
- e.g. Tubulointerstitial fibrosis, diabetic nephropathy
Renal fibrosis is characterised by:
- loss of renal function
- decreased number of epithelial cells
- excess ECM accumulation
- infiltration of fibroblasts
5 Stages of Kidney Disease
Many People With Kidney Disease Still in the Dark- March 2005 Report
Almost 45 percent of people with stage 4 kidney disease only one stage behind
kidney failure had never been told there was anything wrong with their kidneys.
More than 20 million Americansone in nine adultshave chronic kidney
disease. More than 20 million more are at increased risk for developing
kidney disease, and most don't even know it.
Relevant References
Detection and Evaluation of Chronic
Kidney Disease. Snyder S and Pendergraph
B. 2005 AFP 72(9): 1723-1732
Management of Acute Renal Failure.
Needham E. 2005 AFP 72(9): 1739-1746
www.aafp.org/afp
You might also like
- 13 Lecture2 RD-AMD TherapiesDocument15 pages13 Lecture2 RD-AMD TherapiesDoyin AwodeleNo ratings yet
- ImagesDocument2 pagesImagesDoyin AwodeleNo ratings yet
- Science 284, 1322Document7 pagesScience 284, 1322Doyin AwodeleNo ratings yet
- Gli Co Protein ADocument40 pagesGli Co Protein AOmar Cruz BadilloNo ratings yet
- Technical Logical Exam AnswersDocument6 pagesTechnical Logical Exam AnswersDoyin AwodeleNo ratings yet
- Ramsey Et Al 2011Document10 pagesRamsey Et Al 2011Doyin AwodeleNo ratings yet
- StatDocument10 pagesStatDoyin AwodeleNo ratings yet
- Science ReviewDocument10 pagesScience ReviewDoyin AwodeleNo ratings yet
- Drug Development EssayDocument5 pagesDrug Development EssayDoyin AwodeleNo ratings yet
- StatDocument10 pagesStatDoyin AwodeleNo ratings yet
- TypeII Secretion and PathogenesisDocument13 pagesTypeII Secretion and PathogenesisDoyin AwodeleNo ratings yet
- Yersinia PestisDocument6 pagesYersinia PestisDoyin AwodeleNo ratings yet
- Science ReviewDocument10 pagesScience ReviewDoyin AwodeleNo ratings yet
- Putative AD Wit Fast OnsetDocument9 pagesPutative AD Wit Fast OnsetDoyin AwodeleNo ratings yet
- Chemokine ReviewDocument6 pagesChemokine ReviewDoyin AwodeleNo ratings yet
- New Developments in Antidepressant TherapyDocument5 pagesNew Developments in Antidepressant TherapyDoyin AwodeleNo ratings yet
- BDNF TraffikingDocument11 pagesBDNF TraffikingDoyin AwodeleNo ratings yet
- Cassidy Et Al., 2010 - Reelin PFCDocument10 pagesCassidy Et Al., 2010 - Reelin PFCDoyin AwodeleNo ratings yet
- Englehardt Et AlDocument10 pagesEnglehardt Et AlDoyin AwodeleNo ratings yet
- Scully Et Al., 2012 - D-VDocument10 pagesScully Et Al., 2012 - D-VDoyin AwodeleNo ratings yet
- Ketamine Induced Release of BDNFDocument5 pagesKetamine Induced Release of BDNFDoyin AwodeleNo ratings yet
- Fluoxetine TreatmentDocument6 pagesFluoxetine TreatmentDoyin AwodeleNo ratings yet
- Guidelines For Submitting Online Applications - Research PostsDocument4 pagesGuidelines For Submitting Online Applications - Research PostsDoyin AwodeleNo ratings yet
- Weiberg Review Cell PDFDocument29 pagesWeiberg Review Cell PDFThyago CardimNo ratings yet
- John Cryan PaperDocument8 pagesJohn Cryan PaperDoyin AwodeleNo ratings yet
- عقد الحج - ENGLISH 2012Document8 pagesعقد الحج - ENGLISH 2012Doyin AwodeleNo ratings yet
- Onset of ActionDocument13 pagesOnset of ActionDoyin AwodeleNo ratings yet
- Teaching Assistant Life Sciences 10 Month ContractDocument1 pageTeaching Assistant Life Sciences 10 Month ContractDoyin AwodeleNo ratings yet
- It Sligo Careers Office Covering Letter Information SheetDocument1 pageIt Sligo Careers Office Covering Letter Information SheetDoyin AwodeleNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Lesson Plan: Lesson: Projectiles Without Air ResistanceDocument4 pagesLesson Plan: Lesson: Projectiles Without Air ResistanceeltytanNo ratings yet
- Project On Stones & TilesDocument41 pagesProject On Stones & TilesMegha GolaNo ratings yet
- SOR 8th Ed 2013Document467 pagesSOR 8th Ed 2013Durgesh Govil100% (3)
- Are Hypomineralized Primary Molars and Canines Associated With Molar-Incisor HypomineralizationDocument5 pagesAre Hypomineralized Primary Molars and Canines Associated With Molar-Incisor HypomineralizationDr Chevyndra100% (1)
- Tutorial On The ITU GDocument7 pagesTutorial On The ITU GCh RambabuNo ratings yet
- F-16c.1 Ginkgo Ginkgolic AcidDocument2 pagesF-16c.1 Ginkgo Ginkgolic AcidNarongchai PongpanNo ratings yet
- STS Chapter 1 ReviewerDocument4 pagesSTS Chapter 1 ReviewerEunice AdagioNo ratings yet
- Arm BathDocument18 pagesArm Bathddivyasharma12No ratings yet
- Activities and Assessments:: ASSIGNMENT (SUBMIT Your Answers at EDMODO Assignment Section)Document5 pagesActivities and Assessments:: ASSIGNMENT (SUBMIT Your Answers at EDMODO Assignment Section)Quen CuestaNo ratings yet
- Survey Report on Status of Chemical and Microbiological Laboratories in NepalDocument38 pagesSurvey Report on Status of Chemical and Microbiological Laboratories in NepalGautam0% (1)
- BMW Motronic CodesDocument6 pagesBMW Motronic CodesxLibelle100% (3)
- KINETIC THEORY OF GASES TUTORIALDocument6 pagesKINETIC THEORY OF GASES TUTORIALMat SyafiqNo ratings yet
- 9600 DocumentDocument174 pages9600 Documentthom38% (13)
- Apollo TyresDocument78 pagesApollo TyresADITYA33% (3)
- The Temple of ChaosDocument43 pagesThe Temple of ChaosGauthier GohorryNo ratings yet
- FST Handbook 2014-Final Copy 1 PDFDocument382 pagesFST Handbook 2014-Final Copy 1 PDFDelvon DownerNo ratings yet
- Lec9-Rock Cutting ToolsDocument35 pagesLec9-Rock Cutting ToolsAmraha NoorNo ratings yet
- Troubleshooting Hydraulic Circuits: Fluid PowerDocument32 pagesTroubleshooting Hydraulic Circuits: Fluid PowerMi LuanaNo ratings yet
- 2 - Elements of Interior DesignDocument4 pages2 - Elements of Interior DesignYathaarth RastogiNo ratings yet
- ASA 2018 Catalog WebDocument48 pagesASA 2018 Catalog WebglmedinaNo ratings yet
- CANAL (T) Canal Soth FloridaDocument115 pagesCANAL (T) Canal Soth FloridaMIKHA2014No ratings yet
- Problem SolutionsDocument5 pagesProblem SolutionskkappaNo ratings yet
- Abdomen - FRCEM SuccessDocument275 pagesAbdomen - FRCEM SuccessAbin ThomasNo ratings yet
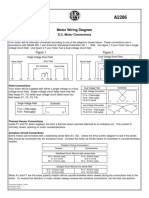
- Motor Wiring Diagram: D.C. Motor ConnectionsDocument1 pageMotor Wiring Diagram: D.C. Motor Connectionsczds6594No ratings yet
- IEQ CompleteDocument19 pagesIEQ Completeharshal patilNo ratings yet
- Monodisperse Droplet Generators As Potential Atomizers For Spray Drying Technology PDFDocument11 pagesMonodisperse Droplet Generators As Potential Atomizers For Spray Drying Technology PDFfishvalNo ratings yet
- The Templist Scroll by :dr. Lawiy-Zodok (C) (R) TMDocument144 pagesThe Templist Scroll by :dr. Lawiy-Zodok (C) (R) TM:Lawiy-Zodok:Shamu:-El100% (5)
- Virchow TriadDocument6 pagesVirchow Triadarif 2006No ratings yet
- Crew Served WeaponsDocument11 pagesCrew Served WeaponsKyle Fagin100% (1)
- MS For Brick WorkDocument7 pagesMS For Brick WorkSumit OmarNo ratings yet