Professional Documents
Culture Documents
Eczema
Uploaded by
Minerva StanciuCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Eczema
Uploaded by
Minerva StanciuCopyright:
Available Formats
ECZEMA
Introduction
Case Scenarios
Conclusions
Introduction
Eczema = Dermatitis
Effect on Quality of Life
(Burden of Disability)
10-15% children suffer from atopic
dermatitis
Asteototic dermatitis is becoming more
and more common in the elderly
Hand dermatitis is a major cause of
absence from work
Basic assessment and treatment
Case 1
6 months old child
Onset of problems at
age 2 months
Formula fed child-
several changes in
milk tried
None of the
ointments work
Sleeping poorly
Allergy tests?
Basic Management of Atopic
Dermatitis
Explanation expectations of treatment
Emollients
Topical Corticosteroids
Explanation
Incredibly common
Cause unknown NOT allergy
Self-limiting in most cases (eventually)
Waxing and waning natural history
Emollients
Bath
General
No limit to their use
Topical Corticosteroids
Mainstay of treatment
Not dangerous if properly used
Most steroid phobias allayed by
explanation
Awareness of different strengths
Package of Care
Time
Explain
Prescribe a package of emollient(s) and
topical steroid(s)
Empower the parents to alter strengths of
corticosteroids depending on clinical
severity
Role of Nursing Colleagues
Ideal disease for follow-up by practice
nurses and health visitors
Offer support through chronic disease
Easy access for flares of disease
Support from specialist dermatology
nurses in secondary care
What about Infection?
Staphylococcus aureus on 100% of skin
lesions
But antibiotics dont cure atopic dermatitis
But some cases improve when either
topical or systemic antibiotics added
Eczema Herpeticum
Unwell patient
Severe pain
Typical umbilicated,
coalescing papules
Herpes simplex virus
(usually type 1)
Urgent hospital
admission
What to Try if Adequate control
NOT Achieved
Concordance (social issues)
Infection
Pulse of stronger topical corticosteroid
Bandaging
Referral
Case 2
75 year old man
Retirement apartment
Likes to keep clean
Diuretics
Itching started on legs and spread to arms
and trunk
Pathogenesis
Dryness and suppleness = state of
hydration of Stratum corneum
State of hydration of stratum corneum
dependant on rate of migration of water
through stratum corneum and rate of
evaporation from its surface
Natural level of skin lipids decreases as
age increases
Management
Is the patient clinically or sub-clinically
dehydrated?
Is the environment too dry?
Is the skin being degreased too frequently
or too harshly?
Emollient
Topical corticosteroid dip in and out after
initial pulse
Case 3
40 year old man
Fed-up with years of dandruff
Recent onset of itchy, red scaling of
eyebrows, naso-labial folds
Seborrheic Eczema
Pathogenesis
Tentative
Increased numbers of Pityrosporum ovale
coupled with ? Genetic tendency
Treatment
Targeted against both P.ovale and
inflammation
Chronic condition therefore need for
repeated periods of treatment
Anti-Pityrosporum shampoo eg Selsun,
Head & Shoulders, Nizoral (contact time)
Combination anti-Pityrosporum and anti-
inflammatory cream eg Cannesten HC,
Daktacort, Nizoral
Case 4
35 year old car mechanic
Eczema as a toddler but clear for years
Recent onset dry, itchy, red rash both
hands
Some improvement when goes on holiday
Hand dermatitis
Multifactorial
Endogenous
Irritant
Allergic
Infection Bacterial and Fungal
Management
Package of treatment
Address any precipitating cause
Scrapings for mycology and swab for
bacterial contamination/infection if
indicated
General hand care
Emollients
Topical Corticosteroid
Conclusions
Diagnosis
Precipitating causes
Time for explanation natural history
Empower the patient to treat their disease
Package of treatment
Point of follow-up
What to Try if Adequate control
NOT Achieved
Concordance (social issues)
Infection
Pulse of stronger topical corticosteroid
Bandaging
Referral
Any eczema questions?
You might also like
- Administrare Diazepam RectalDocument1 pageAdministrare Diazepam RectalMinerva StanciuNo ratings yet
- 12 - CHEER Predicting PreDM CVD Risk Obese TeensDocument61 pages12 - CHEER Predicting PreDM CVD Risk Obese TeensMinerva StanciuNo ratings yet
- Strategic Multiannual Programme 2014 2020Document63 pagesStrategic Multiannual Programme 2014 2020Minerva StanciuNo ratings yet
- 17 173583Document15 pages17 173583Minerva StanciuNo ratings yet
- Kapil Sethi - Paroxysmal Dyskinesias Newest-NO VIDEOSDocument43 pagesKapil Sethi - Paroxysmal Dyskinesias Newest-NO VIDEOSMinerva StanciuNo ratings yet
- 19en V68n1a2Document13 pages19en V68n1a2Minerva StanciuNo ratings yet
- Tutorial - DMDocument52 pagesTutorial - DMMinerva StanciuNo ratings yet
- Early Metabolic ImprintingDocument14 pagesEarly Metabolic ImprintingMinerva StanciuNo ratings yet
- Role of Hcps in The Prevention of Obesity: Dr. Abdul JabbarDocument73 pagesRole of Hcps in The Prevention of Obesity: Dr. Abdul JabbarMinerva StanciuNo ratings yet
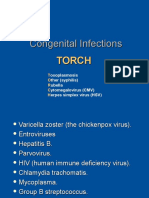
- 1congenital Infections - DRSQDocument21 pages1congenital Infections - DRSQMinerva StanciuNo ratings yet
- CongenitalDocument25 pagesCongenitalSUTHANNo ratings yet
- Congenital CMV Infection in Symptomatic Infants in Delhi and Surrounding AreasDocument3 pagesCongenital CMV Infection in Symptomatic Infants in Delhi and Surrounding AreasMinerva StanciuNo ratings yet
- 18 Garweg PDFDocument40 pages18 Garweg PDFMinerva StanciuNo ratings yet
- 214 FullDocument8 pages214 FullMinerva StanciuNo ratings yet
- 22britt William FINALDocument15 pages22britt William FINALMinerva StanciuNo ratings yet
- Ocular Pathology in Congenital Infections: Swiss Eye Institute and University of Bern, SwitzerlandDocument40 pagesOcular Pathology in Congenital Infections: Swiss Eye Institute and University of Bern, SwitzerlandMinerva StanciuNo ratings yet
- Congenital CMV Infection in Symptomatic Infants in Delhi and Surrounding AreasDocument3 pagesCongenital CMV Infection in Symptomatic Infants in Delhi and Surrounding AreasMinerva StanciuNo ratings yet
- 17 173583Document15 pages17 173583Minerva StanciuNo ratings yet
- Congenital Cytomegalovirus Infection: Description of VirusDocument6 pagesCongenital Cytomegalovirus Infection: Description of VirusMinerva StanciuNo ratings yet
- TGF-b1 Genotype in Pediatric Migraine PatientsDocument5 pagesTGF-b1 Genotype in Pediatric Migraine PatientsMinerva StanciuNo ratings yet
- 15MonicaLahra PerinatalInfectionDocument40 pages15MonicaLahra PerinatalInfectionMinerva StanciuNo ratings yet
- 12 Child Neurol 2015 Urger 9 20Document12 pages12 Child Neurol 2015 Urger 9 20Minerva StanciuNo ratings yet
- Congenital Cytomegalovirus Infection: Description of VirusDocument6 pagesCongenital Cytomegalovirus Infection: Description of VirusMinerva StanciuNo ratings yet
- 13Lec-Approach To Neonates With Suspected Congenital InfectionsDocument56 pages13Lec-Approach To Neonates With Suspected Congenital InfectionsMinerva Stanciu100% (1)
- Other Congenital and Perinatal InfectionsDocument3 pagesOther Congenital and Perinatal InfectionsRabi SyedNo ratings yet
- 15MonicaLahra PerinatalInfectionDocument40 pages15MonicaLahra PerinatalInfectionMinerva StanciuNo ratings yet
- Corticosteroid Use in Duchenne Muscular Dystrophy Increased Over TimeDocument6 pagesCorticosteroid Use in Duchenne Muscular Dystrophy Increased Over TimeMinerva StanciuNo ratings yet
- 11pediatrics in Review 2011 Del Pizzo 537 42Document8 pages11pediatrics in Review 2011 Del Pizzo 537 42Minerva StanciuNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)