Professional Documents
Culture Documents
Antituberculosis Drugs
Uploaded by
Shafira Vidiastri0 ratings0% found this document useful (0 votes)
8 views35 pagesDo'a belajar Wiwik Kusumawati, MD, Master of Health science lecturer of pharmacycology (1996 to now) Lecturer of Medical Education (2004 to now) Vice Dean for academic affair (2004 to 2007) Coordinator of Medical Education Unit (2004 to 2010)
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentDo'a belajar Wiwik Kusumawati, MD, Master of Health science lecturer of pharmacycology (1996 to now) Lecturer of Medical Education (2004 to now) Vice Dean for academic affair (2004 to 2007) Coordinator of Medical Education Unit (2004 to 2010)
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
8 views35 pagesAntituberculosis Drugs
Uploaded by
Shafira VidiastriDo'a belajar Wiwik Kusumawati, MD, Master of Health science lecturer of pharmacycology (1996 to now) Lecturer of Medical Education (2004 to now) Vice Dean for academic affair (2004 to 2007) Coordinator of Medical Education Unit (2004 to 2010)
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 35
Bismillahirrohmaanirrohiim
Asyhadu anlaa ilaaha illalloh
wa asyhadu anna Muhammadan rasuululloh
Rodliitu billahi robbaa
wa bil-islaami diinaa
wa bi Muhammadin nabiyyaw wa rosuulaa
Robbii zidni ilmaa
warzuqnii fahmaa
Aamiin....
Doa belajar
Wiwik Kusumawati, MD, Master of Health
Science
Lecturer of Pharmacology (1996 to now)
Lecturer of Medical Education (2004 to now)
Vice Dean for academic affair (2004 to 2007)
Coordinator of Pharmacology Dept (1996 to
2002)
Coordinator of Medical Education Unit (2004 to
2010)
PhD Cand. of Medical Education of Faculty of
Medicine Gadjah Mada University, Yogyakarta
(2007 now)
Magister of Health Sciences from Faculty of
Medicine of Gadjah Mada University,
Yogyakarta (1997 2000)
Medical Doctor from Faculty of Medicine of
Airlangga University, Surabaya (1985 1991)
General Practitioner (PTT doctor) at Ende,
Flores, NTT (1992 1995)
By
Wiwik Kusumawati
Tuberculosis Infection
?
Pulmonary tuberculosis
7.5 to10.2 million new cases of tbc (WHO)
2.5 to 3.5 million tuberculosis death
Develop and developing countries
Immunodeficiency virus (HIV) infection
Up 80 % tbc px are HIV positive
3.5 million, dual infection
Reactivation dormant infection
Pulmonary tuberculosis
Prompt diagnosis and effective treatment
General symptoms
Weight loss, malaise, fevers
Respiratory symptoms
Cough, sputum and haemoptysis
Resistance of M. tuberculosis
Spontaneous mutation
Improperly prescribed therapy
Erratic drug ingestion
Inadequate dosage
Incomplete therapy
Lack of compliance by px
Resistance of M. tuberculosis
MDR : INH and Rifampicin
XDR : + Fluoroquinolone + 1 injection
drug
Primary
Secondary
Distribution of Primary MDR
Compliance ?
DIRECTLY OBSERVE THERAPY
Patient compliance
Health care
CLASS ROUTE MAJOR INDICATION
Isoniazid PO Primary
Rifampin IV, PO Primary
Streptomycin IM Primary
Ethambutol PO Primary
Pyrazinamide PO Primary CNS or
secondary
Capreomycin IM Secondary or atypical
Kanamycin IM Secondary
Cycloserine PO Secondary
Ethionamide PO Secondary or atypical
Aminosalicylic acid PO Secondary
Clofazimine PO Atypical in HIV px
Rifabutin PO Atypical in HIV px
INH & Rifampin
Tuberculocidal for both extracellular intracellular
organism
Streptomycin
Tuberculocidal for extracellular organism only
Pyrazinamide
Tuberculocidal for intracellular organism
Ethambutol, p-aminosalicylic acid &
ethionamide
Tuberculostatic
Bactericidal cell wall synthesis
Combination
Active infection
Secondary chemoprophylaxis should be given with
2 or more effective drugs
Should never be used as a single to treat
active tbc
Single agent (monotherapy)
Primary chemoprophylaxis
PO: well and rapidly absorbed
Peak concentration 1 to 2 hours
The distribution is extensive
3 to 5 mg/kg/day 20 mg/kg/day
Metabolism by acetylation and hydroxylation
Slow acetylators (Scandinavia, North Africa)
adverse effects
Rapid acetylators (Japan, Escimo) intermittent
regimen
No influence both the effect of therapy and side
effect if INH given everyday
Side effect
Peripheral neuropathy 10 mg/day of
pyridoxine
Induced hepatic injury
A first-line bactericidal anti-tuberculosis
Inhibits RNA-polymerase
Combination with pyrazinamide : persisters
PO, IV
PO : well and completely absorbtion (empty
stomach)
Peak concentration 2 to 4 hours
Combination with INH not influence absorbtion
Distribution is extensive, protein
(albumin) binding 80%
Red-brown colouration of body fluid
Metabolism deacetylation active
metabolite
Excretion : biliary and renal (30%)
Resistant rifampicine rifabutine
Dose 450 600 mg/day (adult); 10 20 mg/kg
BW/day (children)
Side effect
Rash, fever, nausea, vomiting
Flu like syndrome
Hepatotoxic hepatitis
Enzyme hepatic inducer (increase metabolism
of oral contraception, corticosteroid,
hypoglycemic agent, vitamine D)
PAS inhibits absorbtion of rifampicine
Rifampicine + INH (slow acetlators)
Bactericidal to mycobacteria multiplying
intracellularly at low pH level
The first 2 months of a treatment regimen
Reduce later relaps rates
A shorter duration of therapy
PO : well absorbed
Penetrates well in CSF
Nausea, flushing, arthralgia, hepatotoxic
reactions
An aminoglycoside
Extracellular bacteria
Single drug no effective
Must be given by injection (IM)
Widely distributions doesnt cross well
into CSF
30 % protein binding
90 % drugs excreted via urine
Dose
20 mg/kg BW maximally 1 gram/day
Side effect
Neurotoxic and nephrotoxic
8 cranial nerve damage, vestibular
toxicity, rash
Caution
Pregnancy, elderly, renal disease, etc
An essentially bacteriostatic
Inhibits mycobacterial cell wall synthesis
PO : well absorbed (75% to 80 %)
Doesnt cross BBB
Excretion : unchanged in the urine
Dose 15 mg/kg BW/day
Side effect
Retrobulbar neuritis (bilateral)
Rash, fever, Increasing blood uric acid,
etc
At least 3 drugs
INH, Rifampicin, Pyrazinamide
For at least 8 weeks sensitivity
established
Rifampicin and INH
Further 4 months
2HRZ/4HR 6 months
2EHR/7HR 9 month
Rifampicin not included : 18 months
Monitoring adverse effect and efficacy of
drugs
Monitoring up to 1 year after a regimen
completely
Treatment during pregnancy
INH, Ethambutol, Rifampicin (safely)
INH, Pyrazinamide, Rifampicin (poorly tolerated)
Ethionamide is contra indication
Streptomycin is best avoided
Treatment in renal disease
Rifampicin (normal dose)
Other drugs (reduced dose)
Pyrazinamide precipitate gout
Streptomycin if essential
Ethambutol is best avoided in renal failure (GFR 50
ml/min or 3 L/h)
Treatment in liver disease
INH, rifampicin, ethionamide and pyrazinamide can
all be hapatotoxic
Ethambutol, Streptomycin, INH
Regular liver function monitoring
Treatment in children
Standard initial regimen
INH, rifampicin and pyrazinamide
if 2 drugs regimen (INH and rifampicin) : 9 months
Ethambutol is best avoided
Averys Drug Treatment 4
th
edition
(Trevor & Nicholas) : 1047 1054
Clinical Pharmacology, Basic Principles
in Therapeutics (Melmon and Morellis) :
711 712
Subhaanakallohumma
wabihamdika
asyhadu anlaa illaaha illa anta
astaghfiruka wa atuubu ilaika
Doa penutup majelis
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Drug Nomenclature HintsDocument1 pageDrug Nomenclature HintsJordynNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Medication Dosage and CalculationsDocument32 pagesMedication Dosage and CalculationsGavinTLDNo ratings yet
- Chapter 4 Practice TestDocument6 pagesChapter 4 Practice Testnursingstudentd100% (1)
- What Is 21 CFR Part 11Document26 pagesWhat Is 21 CFR Part 11chemtabNo ratings yet
- Pharmacology Study GuideDocument61 pagesPharmacology Study Guide32bballgoNo ratings yet
- A Sandpiper To Bring You JoyDocument3 pagesA Sandpiper To Bring You JoyShafira VidiastriNo ratings yet
- Happy IedDocument2 pagesHappy IedShafira VidiastriNo ratings yet
- Who Packs Your ParachuteDocument1 pageWho Packs Your ParachuteShafira VidiastriNo ratings yet
- Journal of Young InvestigatorsDocument3 pagesJournal of Young InvestigatorsShafira VidiastriNo ratings yet
- The 100 Most Beautiful Words in EnglishDocument5 pagesThe 100 Most Beautiful Words in EnglishShafira VidiastriNo ratings yet
- You Are Loved - A Story of FriendshipDocument3 pagesYou Are Loved - A Story of FriendshipShafira VidiastriNo ratings yet
- Types of ListeningDocument2 pagesTypes of ListeningShafira Vidiastri100% (1)
- Happy IedDocument2 pagesHappy IedShafira VidiastriNo ratings yet
- Yaris LeafletDocument2 pagesYaris Leafletnatta_anggoroNo ratings yet
- 5 Steps To Be Empathic ListenerDocument1 page5 Steps To Be Empathic ListenerShafira VidiastriNo ratings yet
- Starch1500 BrouchureDocument2 pagesStarch1500 BrouchureHeristiana PratiwiNo ratings yet
- 2023 NJ FormularyDocument104 pages2023 NJ FormularyPrince LiNo ratings yet
- Activity 7 Calculations Involved in Parenteral Therapy: University of Santo TomasDocument3 pagesActivity 7 Calculations Involved in Parenteral Therapy: University of Santo TomasJANNIE BELLE RODRIGUEZ100% (1)
- 2019-01 Introduction To Pharmaceutical EngineeringDocument7 pages2019-01 Introduction To Pharmaceutical EngineeringAndy HermanNo ratings yet
- ALL in 1Document1 pageALL in 1Shawn Gaurav JhaNo ratings yet
- 1 - State GMP 1Document52 pages1 - State GMP 1biocoalNo ratings yet
- Item Test Results Method Instrument: PKT 1 OF 6 - Lab Report-Released - (90385) PDFDocument2 pagesItem Test Results Method Instrument: PKT 1 OF 6 - Lab Report-Released - (90385) PDFinforumdocsNo ratings yet
- List Obat Salinan SalinanDocument3 pagesList Obat Salinan SalinanShishil LyaNo ratings yet
- Data Lemari Obat FixDocument7 pagesData Lemari Obat FixNuroniah Nuri LestariNo ratings yet
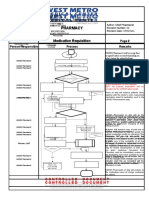
- Pharmacy Pharmacy: Medication Requisition Medication RequisitionDocument1 pagePharmacy Pharmacy: Medication Requisition Medication RequisitionSharie Grace ImlanNo ratings yet
- CTD Question and AnswersDocument17 pagesCTD Question and AnswersPraveenaNo ratings yet
- Dietary Effects On Drug Metabolism and Transport: Robert Z. Harris, Graham R. JangDocument18 pagesDietary Effects On Drug Metabolism and Transport: Robert Z. Harris, Graham R. JangFarah Fadhilah RamadhaniNo ratings yet
- Obat TemepelDocument7 pagesObat Temepelpuskesmas KalitiduNo ratings yet
- Smt. B.N.B Swaminarayan Pharmacy College, Salvav Dr. Kantilal Narkhede BP103TP Pharmaceutics 1 Question BankDocument6 pagesSmt. B.N.B Swaminarayan Pharmacy College, Salvav Dr. Kantilal Narkhede BP103TP Pharmaceutics 1 Question BankAvinash MansukNo ratings yet
- Drugs Approving AuthoritiesDocument38 pagesDrugs Approving AuthoritiesTariq HaqueNo ratings yet
- Pharmacology - PDFDocument41 pagesPharmacology - PDFTanaka KobayashiNo ratings yet
- Waktu Tunggu Pelayanan Resep Bpjs Rawat Jalan Di Instalasi Farmasi Rsia Anugrah Medical Center MetroDocument8 pagesWaktu Tunggu Pelayanan Resep Bpjs Rawat Jalan Di Instalasi Farmasi Rsia Anugrah Medical Center MetrohermaNo ratings yet
- ChloramphenicolDocument17 pagesChloramphenicolApurba Sarker Apu100% (1)
- Biosans LifecareDocument17 pagesBiosans LifecareLORD'S E PHARMACYNo ratings yet
- Medicine Update 2021 Section 14Document56 pagesMedicine Update 2021 Section 14Huda AminNo ratings yet
- Tingkat Signifikansi Kejadian Efek Samping Obat Berdasarkan Skala NaranjoDocument2 pagesTingkat Signifikansi Kejadian Efek Samping Obat Berdasarkan Skala Naranjolab pkmsekolaqNo ratings yet
- Worksheet 8Document2 pagesWorksheet 8Jocel OclaritNo ratings yet
- Vera Internship ReportDocument26 pagesVera Internship ReportLoïc steve Nyamsi BefouraNo ratings yet
- Prodrug Strategy: Concept & Applications)Document45 pagesProdrug Strategy: Concept & Applications)Nuwaira BalochNo ratings yet
- Cadd Question Bank 8 SemDocument8 pagesCadd Question Bank 8 SemMohammed KhalidNo ratings yet