Professional Documents
Culture Documents
Osce Emergenciesj
Uploaded by
Tess Williams0 ratings0% found this document useful (0 votes)
109 views31 pagesjj
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentjj
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
109 views31 pagesOsce Emergenciesj
Uploaded by
Tess Williamsjj
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 31
OSCE Emergencies
ECLAMPSIA / PRE ECLAMPSIA
A dangerous multiorgan disease of pregnancy, concerning hypertension. There are three levels: -
Pregnancy Induced Hypertension - Raised Blood Pressure after the point of viability
Severe Hypertension - two BP readings (15 mins + apart) > 170 systolic or >110 diastolic or >125 MAP
Pre eclampsia - More severe form, coupled with proteinuria with or without
oedema or epigastric pain or visual disturbances
Eclampsia - More severe, coupled with seizures and/or coma
Severe Pre eclampsia affects 1% of all pregnancies. Eclampsia affects 4.9 per 1000 maternities. (38% antenatally, 18%
intrapartum period, 44% postnatally).
Causes of Pre eclampsia / Eclampsia
There is no known cause of this disease. However theories are listed below
Genetic disposition
Immunological disorder
Abnormal placental implantation
Platelet activation
Coagulation abnormalities
Cardiovascular system not adapting to pregnancy
Risk factors
Nulliparity
>40 years old
multiple pregnancy
family history
renal disease
chronic hypertension
diabetes
previous pre-eclampsia (with same partner)
Signs of Pre eclampsia
BP >160/180 mmHg systolic or > 110 mmHg diastolic (or >30 mmHg rise from booking BP)
Proteinuria
&c^y; serum creatinine
'I urine output - ogliuria <500mls a day
Pulmonary oedema
Thrombocytopaenia (reduced platelets)
Hepatic dysfunction
IUGR
Headaches
Visual disturbances
Epigastric pain
Seizures (in Eclampsia)
Symptoms / Effects of Severe Pre eclampsia
Severe Hypertension AND one or more out of
++ proteinuria on dipstick (or >1g on 24 hour collection)
<100mls urine in 4 hours (or creatinine >100)
CNS signs - altered consciousness, increased muscle tone
Flashing lights, blurred vision
Persistent headaches
Epigastric pain
LFT raised (alanine aminotransferase (ALT) > 50 iu/L)
Symptoms / Effects of Eclampsia
Convulsion between viability and 10 days postpartum which has no other known cause
Usually preceded by Pre eclampsia or CNS excitability
Usually within 48 hours of delivery
Symptoms / Effects of HELLP Syndrome, a severe variant of pre eclampsia
Haemolysis Red Blood Cells are damaged as they pass through blood vessels with a damaged
endothelium tissue and fibrin deposits
Elevated Liver Enzymes Fibrin is deposited in the hepatic sinusoids, creating liver damage and elevated enzymes
Low Platelets There is a decrease in the life span of the platelets and wide aggregation
Management of Severe Hypertension
Try to keep BP in region of 140-150 / 90-100
Compare BP with manual sphygmometer (or take
with if different)
Use 4th karotkoff sound for diastolic
Avoid sharp drop in BP
Continuous CTG up to 1 hour after BP stable
following treatment
Labetalol is first drug of choice
Monitor Fluid Balance hourly - total of 85mls per
hour in
Too little = renal failure
Too much = pleural effusion
Don't forget fluid leaks into the extra vascular space
Start 24 hour urine collection
Take bloods
FBC
Urates and electrolytes
Liver Function Test
Clotting (including platelets)
Group and Save
Repeat U&Es and LFT bloods every 6 - 12 hours
Management of severe pre eclampsia antenally
Should be in consultant led unit with NICU facilities
Inform relevant staff
Consultant Obstetrician
On call Anaesthetist
Senior Midwife
SCBU / Neonatologist
Mode and Timing of Delivery must be considered
Delay to stabilise woman or to give steroids to mature fetal lungs
Transfer to an area where 1 to 1 care can be given
Labour ward or other high dependency area
Site two large bore venflons
Take bloods
FBC
Urates and electrolytes
Liver Function Test
Clotting (including platelets)
Group and Save
Repeat bloods every 6 - 12 hours
Monitor Mother (at this level until 24 hours after delivery)
Monitor Fluid Balance
Too little = renal failure
Too much = pleural effusion
Don't forget fluid leaks into the extra vascular space
Catheterise
Indwelling catheter with hourly measurement bag
Send sample for culture
Start 24 hour urine collection
Pulse oximeter & Sats continuously
Blood Pressure every 15 minutes (30 if stable)
Temperature hourly
Dipstick for urine hourly
Monitor fetus
CTG for at least 1 hour 3* daily
If non-reassuring then continuous
Ultrasound scan
Growth and liquor volume
Umbilical Cord Doppler Flow
Deliver
Induce labour
Caesarean Section
Management of Eclampsia
Call for help
Senior obstetrician
Obstetrician to assist (potential caesarean section)
Anaesthetist
ODP
Senior midwife
Scribe
Paediatrician (if antenatal)
Inform SCBU (if antenatal)
Notify Haematologist
Porter
Turn onto left lateral
Remove pillows
Aspirate material from mouth
Give facial oxygen (10L)
Insert guedal airway (when/if possible)
Give magnesium sulphate
4 - 6g loading dose IV over 15-20 minutes
2g IV for secondary fit
1-3g/hr for maintenance
Cannot use at same time as nifedipine
Diazepam PR (if magnesium fails or no IV access)
Then site IV access if none
Catheterise
Indwelling catheter with hourly measurement bag
Consider delivery (if antenatal)
Monitor mother hourly while on magnesium sulphate
Knee jerk (stop if absent)
Respiratory (stop if <10breaths a minute)
Urine output (reduce to 0.5g/hr if <30mls)
Give antidote to magnesium sulphate
Calcium Gulgonate 10mls of 10% (1g) IV over 3 minutes
Blood levels should be 2-4mmols/l for therapeutic levels
5mmols/l loss of knee jerk reflex, weakness, blurred vision, slurred speech
7.5mmols/l muscle paralysis & respiratory arrest
12mmols/l cardiac arrest
Bloods (order with vaccutainer system as preservatives can affect results) Blue - Clotting
Screen
Purple - FBC Pink - Group & Save
Contentious issues
In the last triennium there were 16 maternal deaths from Pre eclampsia/eclampsia (8 from HELLP) - this decreased due to antenatal detection and
treatment up to 1999. Now roughly constant, but two deaths were alone in hospital so still improvements and 6 had substandard care.
Chien et al (1996) found that magnesium sulfate was associated with 60 to 70 percent fewer recurrent seizures than were diazepam and
phenytoin
MATERNAL RESUSCITATION
Maternal resuscitation is usually needed following cardiac arrest, when a pregnant woman needs help to restart her
cardio-pulmonary system. It
occurs in every 30,000 pregnancies.
Some potential causes of collapse, necessitating CPR
Pulmonary Embolism
Amniotic Fluid Embolism
Trauma
Haemorrage
Eclampsia
Anaesthetic Problems
Anaphylaxis
Cardiac Problems
Anatomy and Physiology changes in pregnancy
affecting resuscitation
90% of term pregnant women completely occlude
the vena cava when lying supine
Stroke volume is 30% of a non-pregnant woman
(returns almost to normal when fetus is delivered)
20% decrease in lung volume due pressure from
the uterus on lungs and diaphragm
20% increase in oxygen demands to meet needs of
fetus and uterus
Increase in progesterone means the
oesophageal sphincter is relaxed so more likely to
force air into the stomach or regurgitate stomach
contents
Treatment of visibly pregnant woman
Lie flat
Call for help
Senior obstetrician
Obstetrician to assist (potential caesarean section)
Anaesthetist
ODP
Senior midwife
Scribe
Paediatrician
Inform SCBU
Porter
Displace uterus to remove aorto-caval compression (15-30)
Cardiff Wedge / other support under right hip to place into left lateral position
And/or lift uterus up and to the left
Check Airways
Place hand on mother's forehead and gently tilt head back.
Put fingertips under the point of mother's chin and lift the chin
A jaw thrust may be required - fingers behind the angle of the jaw and
moving jaw anteriorly to displace tongue from the pharynx.
Remove visible debris
Check Breathing
Cheek near mouth to feel breath and watch chest for rising and falling
Agonal gasps are not a sign of life
Check circulation
Simultaneously feel carotid artery for pulse
Don't spend more than 10 seconds
If no circulation (or unsure)
30 chest compressions
Middle of lower half of sternum
Arms straight
Depress about 4-5cm
Rate of 100 beats a minute
2 ventilation breaths (lasting 1 second)
Change staff frequently if exhausted
If no breathing but circulation
Ventilation breaths
Rate of 10 per minute
Recheck each minute
Anaesthetist will intubate as soon as possible
Gain IV access
If no signs of life within 5 minutes
Perimortem caesarean section
No need to go to theatre
Minimal blood loss if no cardiac output
Continue CPR throughout
May consider open cardiac massage when abdomen open
Stopping CPR is a consultant decision
Consider Defibrillation if appropriate
Consider Adrenaline
1:10,000 -1ml (10mls) IV every 3-5minutes for cardiac arrest
1:1,000 500mcg (0.50ml) IM every 5 minutes for general anaphylaxis
If successful make mother as comfortable as possible
Give oxygen via facemask (15L/minute)
Record Keeping, as contemporaneously as possible, when writing up notes
include original scribe's transcripts
Contentious issues
In a comprehensive review of post-mortem caesarean deliveries
between 1900 and 1985 (n=61) by Katz et al., 70% of infants delivered
within five minutes (42) survived and all developed normally. However,
only 13% of those delivered at 10 minutes (8) and 12% of infants
delivered at 15 minutes (7) survived. One infant in both of these groups of
later survivors had neurological sequelae.
No doctor has been found liable for performing a post-mortem
caesarean section. Despite no consent they are seen as acting in the best
interest of the patient
A perimortem caesarean is performed to try and increase the chance
of saving the mothers life, as CPR is unlikely to succeed with a gravid
uterus. The fetus has no rights in law
NEONATAL RESUSCITATION
Occurs when the neonate has problems transitioning to extrauterine life, and refers to the additional means given to aid
this transition. This is usually a respiratory problem.
Who is at increased risk?
Mother under 17
Mother over 35
Diabetic mothers
Drug Abuse
Pre-eclampsia
Abruption
Prolonged labour
Prolonged rupture of membranes
pethidine
rapid birth
prematurity
breech
meconium
multiple pregnancy
congenital abnormalities
Fetal Heart rate abnormalities
Types of Apnea
First / Primary Apnea.
^heart rate ^tone
pH levels 7 - 7.2
If baby born now will respond well to
stimulation and oxygen
If pregnancy continues fetus will deteriorate
Start deep, irregular gasps
Then stop breathing
Now in Secondary / Terminal Apnea
^heart rate ^fetal BP ^tone
pH levels <7
If baby born now will need full CPR, possible
ventilation
Will take longer to resuscitate, may not be
successful
How to resuscitate a neonate
If suspect a need for resuscitation then leave a long (at
least 2inches) umbilical cord stump.
Note time of birth / start clock on resuscitaire
Call for help
Paediatrician
Senior Midwife
Take baby to resusitaire or resuscitation area
Dry and stimulate baby
Change towel
Airway place head in a neutral position -
hyperextension or flexion can block the airway
Assess breathing and heartrate
Inflate the lungs
Inflation breaths *5 (Pressure at 30cm of water for at
least 2-3 seconds)
Check by seeing abdomen rise & HR ­
Repeat if lungs not inflated
Recheck head position
Need help maintaining airway? (second person/guedel
airway)
Blockage? Do you need suction
Only suction under direct supervision be careful not to
stimulate vagal reflex
Reassess per cycle (30 seconds)
If HR <60bpm then start chest compression
Two thumbs at midpoint between the nipples
Hands enclosing baby
Press down 1/3 of width
Rate 3chest compressions to 1 breath
120 interventions per minute
Reassess per cycle (30 seconds)
If HR>100 or increasing but no breathing
Ventilation breaths *15
Every other second
Reassess per cycle (30 seconds)
Continue until spontaneous breathing by baby or
paediatrician makes decision to end treatment (may be
considered after 10 minutes effective resuscitation if no
signs of life)
APGARs should be noted every 5 minutes, until above 8
If no signs of improvement the paediatrician may
consider drugs
These are administered through an umbilical vein
cannula
Adrenaline 0.1ml/kg of 1:10,000 solution (10
micrograms)
If this fails 0.3ml/kg can be used (30 micrograms)
Sodium Bicarbonate 2-4ml/kg of 4.2% solution
Dextrose 2.5ml/kg of 10% dextrose
Contentious issues
Wrap very preterm infants in food grade plastic
wrapping to maintain body temperature (if
hypothermia sets in very difficult to resuscitate)
With asphyxia the pH drops by 0.04 per minute, so
will decrease 0.28 in 7 minutes. Much more difficult to
resuscitate if pH below 7.
There is not enough evidence to recommend
suctioning meconium on the perineum
No evidence to support waving oxygen, this may
stimulate baby but also cools them down
There is a debate over resuscitating with air or
oxygen. Pure oxygen should not be used (can cause
retinal damage), but if no improvement with room air
then add supplementary oxygen
POSTPARTUM HAEMORRHAGE
A postpartum haemorrhage is any bleeding from the genital tract, following the birth of a baby, of more than 500mls or any
amount that adversely affects the mother. A primary postpartum haemorrhage occurs within the first 24 hours, a secondary
postpartum haemorrhage occurs after this - usually around day 10. Variance ranges from 4 -11% of all births.
Potential risk factors for postpartum haemorrhage
Multiple pregnancy
Macrosomia
Polyhydramnios
Grandmultiparity
Retained placenta
Augmented labour
Placenta previa
Antepartum haemorrhage
Instrumental birth
Caesarean Section
Clotting Disorders
Previous PPH
There are 4 categories that cause postpartum
haemorrhage
Tone (70%) Trauma Tissue Thrombin
Grand Multiparity
Multiple pregnancy
Polyhydraminos
Macrosomia
Abnormalities: fibroids
Prolonged labour
Precipitate labour
Dysfunsctional labour
Intrauterine infection
Uterine relaxing agents
(Magnesium / general anaesthetic/ tocolytics)
Operative delivery
Cervical / vaginal lacerations
Previous caesarean section increases risk of morbidly
adherent placenta
Retained placental tissue or membranes
Pre-eclampsia
HELLP Syndrome
Placental abruption
Amniotic Fluid Embolism
Sepsis
Bleeding disorders
Drugs (aspirin / heparin)
Potential Con sequences of PPH
Shock
Maternal Death
DIC
Hysterectomy
Treating a Primary Postpartum Haemorrhage
Call for help
Senior Obstetrician
Senior Midwife
Anaesthetist
ODP
Senior midwife
Scribe
Porter
Notify Haematologist
Site two large bore venflons
Take bloods
FBC
Clotting (including platelets)
Crossmatch
Get 4-6 units of blood ready in case of blood transfusion
Stabilise mother
Frequently assess maternal observations (usually Anaesthetists job)
Maternal oxygen 8L/min
Monitor fluid input/output
IV Crystalloid or Colloid Hartmanns/normal Saline (NOT DEXTROSE) fast i.e. 5-
10mins if major PPH
IV Plasma substitute (Haemacell 500mls)
Include blood transfusion in fluid in balance
Catheterise
Need at least 30mls/hr
Continually assess volume of blood loss
Check uterine tone
If lax/boggy
Rub up a contraction
Repeat/give syntometrine (or ergometrine)
Syntometrine (1ml = 5IU of syntocinon and 500mcg ergometrine)
Ergometrine 0.5mg (500mcg) IV
Do not give if hypertensive
Set up IV syntocinon 40IU/500mls normal saline over 4 hours (check policy)
Haemobate/Carboprost 0.2mg IM every 15 minutes (max 8 doses 2mg)
Obstetrician can give myometrically (directly into uterus)
Transfer to theatre for surgery if bleeding not stopped
Tie off/cauterise all ligaments (blood flow) to the uterus
Assess quickly for bleeding from trauma site
If obvious trauma transfer to theatre for suturing of cervix, perineum etc
Is placenta in situ?
Try to deliver placenta
Careful not to invert uterus
Get someone to check for completeness if out
Transfer to theatre for manual removal if adherent or pieces missing
Haematologist will instruct if clotting disorders
May need additional clotting factors infused
If no idea why bleeding is occurring / cannot stop it
Get Consultant if not already present
Apply bimanual compression
Or compress aorta
(fist just above umbilicus and to the left if you can feel the femoral pulse you
arent pressing hard enough)
Consider CVP line (Anaesthetist to insert)
Transfer to theatre if not already there
GA
Obstetrician to carry out manual exploration
Possible ruptured uterus
Possible Intrabdominal Bleeding
Broad Ligament Haematoma
Consider transfer to ITU when bleeding under control
May need additional blood transfusion / iron supplements
Record Keeping, as contemporaneously as possible, when writing up notes
include original scribes transcripts
Contentious issues
10 women died of PPH in the last triennium (ten fold increase from previous triennium), although
2 were concealed pregnancies with an unattended PPH at home possibly could have been treated
and saved?
The main problem with such a catastrophic bleed is that DIC can occur (disseminated intravascular
coagulation) when this happens the clotting mechanism in the blood 'goes all to ****' with little
blood clots forming in the capillaries - this uses up all the clotting factors and means that it cant
clot where its meant to. If heparin is given it can cause those mini-clots to break down and reset
the system. However its a balancing act, too little wont do a thing, too much can kill her
Breastfeeding causes the body to release oxytocin, useful in case of minor bleed or to encourage
placenta to come out
Anaemia does not increase the risk of a postpartum haemorrhage, however it will affect how the
woman can cope with the blood loss, so may become symptomatic much early than someone with
a high Hb.
RCOG recommend that an arterial balloon occlusion and embolism are used to reduce need for
transfusions and hysterectomy where there is a known high risk of PPH the balloon is placed in
the iliac and uterine arteries prior to section for previa over old scar or known placenta accreta.
Due to the increased blood volume of a healthy pregnant woman at term, the woman wont show
signs of shock until she has lost a good deal of blood (over 1L) dont assume there is no danger
because BP is normal
A B-lynch suture, where the uterus is sown up and over, in a belt and braces fashion, can stop
haemorrhage effectively and preserve future fertility.
SHOULDER DYSTOCIA
There is no one definition for shoulder dystocia, but it occurs when the shoulders do not deliver spontaneously with gentle
traction. It is caused by the anterior shoulder becoming impacted against the symphysis pubis, after delivery of the head.
It occurs when the breadth of the shoulders is greater than the biparietal diameter of the head. It occurs in between 0.3 -
1% of all births. If birth weight >4kg then 5-7% risk & birth weight <4.5kg 8-10% risk but 50% occur in normal birth
weight babies
Who is at greater risk?
Age over 35
short mother (under 5 2)
small pelvis
postdates
macrosomia
maternal weight over 90kg
mother was macrosomic
diabetic
previous shoulder dystocia
male fetus
ocytocin
prolonged 1st stage
prolonged 2nd stage
head bobbing / turtling
instrumental delivery
Remember not all shoulder dystocias are not predicted by the existing risk
factors.
What to do when you identify a case of shoulder dystocia
Call for help
Senior obstetrician
Senior midwife
Scribe
Paediatrician
Inform SCBU
Note time of birth of head
Decide if episiotomy is required
Abduct and flex the womans legs to as close as her shoulders as
possible (McRoberts position). This straightens the symphysis pubis
and allows the coccyx to drop to give extra room. Lurie et al (1994)
found this resolved 88% cases of shoulder dystocia (n=76)
Try delivering shoulders & note time
Apply suprapubic pressure in the direction of the fetal back, this is
to try and rotate the anterior shoulder into the oblique position.
(Rubins I)
Apply continuous pressure for 30 seconds
Apply intermittent pressure for 30 seconds
If feel movements try delivering shoulders
Note time
Enter the vagina to perform internal manoeuvres
Rubins II enter along the fetal back then apply posterior pressure
to the anterior shoulder. This is to try and rotate the anterior
shoulder into the oblique.
Woods Screw leave first hand where it is, use other hand to enter
with two fingers along the fetal front while using same pressure as
before add anterior pressure to the posterior shoulder. This is to try
and rotate the anterior shoulder into the oblique and as it moves it
will screw forward and down.
Reverse woods screw remove second hand then drop the two
fingers from the first hand to the posterior aspect of the posterior
shoulder and apply pressure. This is to try and rotate the posterior
shoulder to the anterior position as it moves it will screw forward
and down. Swap hands halfway through movement to complete
rotation.
If feel movements try delivering shoulders
Note time of each manoeuvre
Try to remove the posterior arm
Insert your whole hand (hand which the fetus is facing) under the
fetus
Splint the posterior arm and bend at the elbow
Sweep over the chest and face in a cat lick manoeuvre
This should cause the fetus to drop down and allow the shoulders
to deliver
Note time
Roll the mother onto all fours known as the Gaskin Manoeuvre.
The movement can help the fetus to rotate and prevent pressure on
the coccyx
Note time of delivery
Be prepared for resuscitating neonate, have paediatrician there if
possible
Record Keeping, as contemporaneously as possible, when writing
up notes include original scribes transcripts
Manoeuvres can be performed in any order.
Complications - Maternal
3rd/4th degree tears or extended episiotomy
Vaginal lacerations
Postpartum haemorrhage
Uterine rupture
Death
Complications - Baby
Brachial Plexus injuries
Erb's palsy
Klumpke's palsy)
Fractures
Clavicle
Humerus
Hypoxia
Death
Contentious issues
You have roughly 7 minutes to get baby out before
irreversible brain damage sets in. The pH drops by 0.04 per
minute, so will decrease 0.28 in 7 minutes. Much more difficult to
resuscitate if pH below 7.
Alternative methods to deliver fetus - can't be done by midwife:
Zavanelli manoeuvre - replacing the fetal head into the vagina
to perform caesarean section
Cleidotomy -deliberately breaking the clavicle to reduce
diameter of the shoulders, occasionally happens by accident
during internal manoeuvres
Symphysiotomy - surgically separating the symphysis pubis to
allow extra room
- not often done in the Western world
Despite a small study by Bruner et al (1998) (n=82) showing
all cases resolved by Gaskin Manoeuvre, with no mortality or
brachial plexus injuries most don't use this as a first line, often as
unable to move mother especially if an epidural in situ. Often used
in community.
Sometimes McRoberts is done in anticipation - there is no proof
this works
The Advanced Life Suport In Obstetrics (ALSO) course teaches
the HELPERR pneumonic, which is used in the UK as good
practice
You can have a posterior shoulder dystocia, where the
posterior shoulder is impacted behind the sacral prominary.
VAGINAL BREECH BIRTH
A breech presentation, where the feet or buttocks lie nearest the cervix,
occurs in 3-4% of all TERM pregnancies.
There are four types of breech presentation: (incomplete breech encompasses a partially flexed (one leg crossed) breech,
footling and knee presentations)
frank breech (both legs straight against the abdomen, feet by the head) - 6070%
complete (or flexed) breech (legs are crossed) - 30-40%
footling breech (one or both feet below the buttocks) - 1%
knee breech (one or both knees below the buttocks) - rare
Potential Causes
Prematurity (20% at 28 weeks)
hydrocephaly
polyhydramnios
oligohydramnios
multiple pregnancy
bicornate uterus (septate uterus)
fibroids
placenta previa
fundal placenta
IntraUterineDeath
primigravida
grandmultips
Recommended Management of breech at term
At 37 weeks (or 36) women with an uncomplicated pregnancy should be offered
an ECV. A cochrane review (Hofmeyr, 2003) showed that 67% of babies turn to
cephalic with ECV, rather than the 22% who turn spontaneously. Babies aren't at
increased risk with ECV.
In 2000 an international RCT - the Hannah trial (n=2088) showed that it the
perinatal mortality and morbidity rates were decreased by three quarters.
People including one of the authors have criticised the study - but even when
ability of practitioner, footling breech and augmentation of labour are taken into
account there is a higher risk. This has lead to most hospitals recommending
elective caesareans for all breech presentations. However Glazerman (2006) (one
of the authors of the Hannah trial) did a 5 year follow up to the Term Breech Trial
and found that despite this new policy the perinatal mortality and morbidity rates
were unchanged.
How to diagnose a breech
Woman complaining of a pain/ hard lump under her ribs
States feels most movements low down
On palpation - Hard, ballotable pole in the fundus
Softer presenting part on VE, may feel the anus, or a very prominent ridge (between buttocks)
Thick toothpaste' meconium following rupture of membranes
FHHR at or above umbilicus
Confirm by USS
Risks involved with breech babies
Cerebral Palsy (with presentation NOT method
of birth)
Congenital Hip Dysplasia (with presentation
NOT method of birth)
Cord Prolapse
Premature placenta separation (if too upright
in second stage)
Intracranial haemorrhage and tentorial tears
(too rapid delivery of the head or by anoxia)
Fractures (mismanagement of manoeuvres)
Rupture of internal organs (mismanagement -
holding abdomen)
Genital damage
Dislocation of jaw (if mauriceau-smellie-veit
done incorrectly)
Hypoxia (cord compression)
Hypothermia
How to conduct a vaginal breech birth HANDS OFF THE
BREECH
Due to increased risk of hypoxia and cord prolapse, it is
recommended that for a known breech presentation there is
continuous monitoring (obviously this is for hospital births)
Confirm full dilatation by a vaginal examination
In the second stage move the mother into a position to
allow the baby to hang with gravity, either lithotomy or all
fours
Consider episiotomy when the breech is distending the
perineum - theory being it will prevent the head getting stuck
by the tissue, not always needed, use judgement. In a term
well grown fetus the bitrochanteric diameter is 9.5cm so if
bum gets through the head, if flexed, should be fine.
Some say cover/wrap baby to prevent hypothermia
Let mother push baby out on her own, if baby continues to
descend on it's own then let it be. If stops descending with
contraction, you may need to help as below at each point -
after each intervention go back to hands off. Hands on can
stimulate baby to breathe while in utero or stimulate the
morrow reflex and extend the arms.
Baby needs to have its back to symphysis pubis
If the extended legs hold baby up, then use popliteal
pressure. Splint the leg with your fingers, then abduct to the
side and then flex the knee. Do same for other leg if needed.
Note time of birth up to umbilicus - the umbilical
cord will start to be compressed and fetus will stand 7
minutes without oxygen, so don't panic
If the arms are extended then you need to bring them
down using Lovset's manoeuvre.
First hold by pelvic girdle and rotate up to 180 to bring
the arm in front of the face.
Then the arm can be swept down and across the face as
in a cat's lick, bringing the arm in front of the face.
If necessary repeat for the other arm.
Turn back to the original position afterwards
Back to hands off until you can see the nape of the neck
(hairline) - hanging will keep baby well flexed.
Use mauriceau-smellie-veit to slowly deliver the head. Too
fast may cause tentorial tears. Keep the head flexed by
pressing forward with one hand, baby straddles your arm. The
lower hand is on baby's cheeks and chin NOT in the mouth
Baby is more likely to need resuscitation so be prepared. If
possible have a paediatrician present for the birth.
Record Keeping, as contemporaneously as possible, when
writing up notes include original scribe's transcripts
Contentious issues
If there is any delay in the first (or second) stages, most people experienced in breech births will not augment and will
proceed to caesarean - for this reason only about 57% of attempted vaginal breech births result in a vaginal birth.
The preterm breech is often more severely compromised during a vaginal birth
- however a cochrane review (Grant and Glazer, 2003) said there was not enough evidence to routinely performed
caesareans in this situation, although most obstetricians will.
The biggest fear is that of an entrapped head, hence why full dilation is confirmed by VE, this is more likely with a
preterm or IUGR fetus. This can be managed by :
Durrssen's incisions (cutting the cervix) however this will result in a large blood loss
symphysiotomy (surgically separating the symphysis pubis to allow extra room)
- not often done in the Western world
You might also like
- Bimanual Vaginal Examination - OSCE Guide - Geeky MedicsDocument6 pagesBimanual Vaginal Examination - OSCE Guide - Geeky MedicsJahangir AlamNo ratings yet
- Abdominal HysterectomyDocument23 pagesAbdominal Hysterectomytata marethaNo ratings yet
- Peds and Med OSCE GuideDocument8 pagesPeds and Med OSCE GuideAbdulNo ratings yet
- MBCHB OSCE PaediatricsDocument18 pagesMBCHB OSCE PaediatricsRhythm VasudevaNo ratings yet
- Nursing care for a family experiencing postpartum hemorrhageDocument68 pagesNursing care for a family experiencing postpartum hemorrhagePrecious SorianoNo ratings yet
- Management of Third and Fourth Degree TearsDocument4 pagesManagement of Third and Fourth Degree TearsYwagar YwagarNo ratings yet
- Pharmacology of Drugs For PPHDocument55 pagesPharmacology of Drugs For PPHFaye CagayanNo ratings yet
- Surgical Drains .Document30 pagesSurgical Drains .SAlemsaNo ratings yet
- Ob/Gyn Instruments: Done byDocument30 pagesOb/Gyn Instruments: Done byDrHassan Ahmed ShaikhNo ratings yet
- Pediatric mini osce 1: Developmental milestones and reflexesDocument138 pagesPediatric mini osce 1: Developmental milestones and reflexesabdelaheem arabiatNo ratings yet
- OSCE OB - PDF Version 1Document15 pagesOSCE OB - PDF Version 1FNaF is love FNaF is lifeNo ratings yet
- Breast Lump History: Opening The ConsultationDocument2 pagesBreast Lump History: Opening The ConsultationYoyoguyNo ratings yet
- Post Partum HemorrhageDocument59 pagesPost Partum HemorrhageMahima SharmaNo ratings yet
- A System of Operative Surgery, Volume IV (of 4)From EverandA System of Operative Surgery, Volume IV (of 4)Rating: 4 out of 5 stars4/5 (1)
- Ambulatory Hysteroscopy Evidence-Based Guide To Diagnosis and TherapyDocument23 pagesAmbulatory Hysteroscopy Evidence-Based Guide To Diagnosis and TherapyAngela EstevesNo ratings yet
- Pre 3 NP 2 2Document25 pagesPre 3 NP 2 2cristina baker80% (5)
- OSCE Gynae-OSCE-MMSSDocument24 pagesOSCE Gynae-OSCE-MMSSMohammad Saifullah100% (1)
- OSCE Counselling NotesDocument3 pagesOSCE Counselling NotesjuweriyNo ratings yet
- Nursing Care of Postpartum ComplicationsDocument13 pagesNursing Care of Postpartum ComplicationsLyca Mae AurelioNo ratings yet
- Vaginal Swabs OSCE Guide PDFDocument8 pagesVaginal Swabs OSCE Guide PDFParsaant SinghNo ratings yet
- The Average Blood Loss Following Vaginal Delivery, Cesarean Delivery and Cesarean Hysterectomy Is 500 ML, 1000 ML and 1500 ML RespectivelyDocument11 pagesThe Average Blood Loss Following Vaginal Delivery, Cesarean Delivery and Cesarean Hysterectomy Is 500 ML, 1000 ML and 1500 ML RespectivelypriyankaNo ratings yet
- ObsGyn OSCE Notes PDFDocument52 pagesObsGyn OSCE Notes PDFNorman Ahmad RiyandiNo ratings yet
- Obs Gynae Full Summary NotesDocument41 pagesObs Gynae Full Summary NotesJana Aldour100% (1)
- 3rd Stage of LabourDocument10 pages3rd Stage of LabourBhawna JoshiNo ratings yet
- 3rd and 4th Stage of Labor Dr. BaduaDocument8 pages3rd and 4th Stage of Labor Dr. BaduaMarco Paulo Reyes NaoeNo ratings yet
- The Ten-Step Vaginal Hysterectomy - A Newer and Better ApproachDocument8 pagesThe Ten-Step Vaginal Hysterectomy - A Newer and Better ApproachqisthiaufaNo ratings yet
- Endocrinology OSCEDocument17 pagesEndocrinology OSCEswamy rao100% (1)
- Vaginal Swabs: OSCE ChecklistDocument2 pagesVaginal Swabs: OSCE ChecklistNeeta Ananda100% (1)
- May 8, Tuesday May 10, Thursday 12:45 PM Onwards: TestDocument7 pagesMay 8, Tuesday May 10, Thursday 12:45 PM Onwards: TestJonathan ChanNo ratings yet
- Time - 1hour (60 Minutes) : Final Mbbs - OsceDocument59 pagesTime - 1hour (60 Minutes) : Final Mbbs - OscekbNo ratings yet
- Ospe Bank PDFDocument318 pagesOspe Bank PDFMed StudentNo ratings yet
- Done By: Abdul Hakeem Hady. Gynecology SlidesDocument16 pagesDone By: Abdul Hakeem Hady. Gynecology Slidesعمر احمد شاكرNo ratings yet
- Recurrent UTI Case Presentation in Child with Obstructive UropathyDocument26 pagesRecurrent UTI Case Presentation in Child with Obstructive UropathyAminath MeesanNo ratings yet
- Pelvic Exam PDFDocument2 pagesPelvic Exam PDFRosu GeorgeNo ratings yet
- Obstetric Gynaecology Jan 11Document32 pagesObstetric Gynaecology Jan 11selvie87No ratings yet
- FGE Report August/September 2002Document12 pagesFGE Report August/September 2002mnigam64No ratings yet
- Surgery OSCE SpotsDocument1 pageSurgery OSCE SpotsAbdulNo ratings yet
- West Bengal University of Health Sciences: Name of The InstitutionDocument9 pagesWest Bengal University of Health Sciences: Name of The InstitutionVarun Mohanakumaran RajambikaNo ratings yet
- Menorrhagia DDx HistoryDocument2 pagesMenorrhagia DDx HistoryShi Yi ChuaNo ratings yet
- Blood Glucose Measurement - Geeky MedicsDocument3 pagesBlood Glucose Measurement - Geeky MedicsJahangir AlamNo ratings yet
- Practice OSCE - Breaking Bad NewsDocument1 pagePractice OSCE - Breaking Bad NewssilverangelkickinNo ratings yet
- Gynaecology & Obstetrics Sorted Questions 8 SemesterDocument4 pagesGynaecology & Obstetrics Sorted Questions 8 SemesterSaikat MondalNo ratings yet
- Obstetrics History Taking in and Examination PowerpointDocument15 pagesObstetrics History Taking in and Examination Powerpointياسر كوثر هانيNo ratings yet
- Mohsen AttiaDocument3 pagesMohsen AttiaAloah122346100% (1)
- Reading of PartographDocument33 pagesReading of PartographAtya ShabrinaNo ratings yet
- Essays For Obs N GYn 1Document8 pagesEssays For Obs N GYn 1whoosh2008No ratings yet
- HysterectomyDocument70 pagesHysterectomyYudhistira AdiNo ratings yet
- Shoulder Examination Mark SchemeDocument1 pageShoulder Examination Mark SchemeGeorge GeorgeNo ratings yet
- Medical History Taking Study GuideDocument6 pagesMedical History Taking Study GuideSarra Mood ImanNo ratings yet
- 03 OSCE SlideShowDocument113 pages03 OSCE SlideShowMohamed FlefelNo ratings yet
- Systemic Surgery NuggetsDocument17 pagesSystemic Surgery NuggetsAhmad UsmanNo ratings yet
- Urology Case Presentation - Scrotal Mass 1Document20 pagesUrology Case Presentation - Scrotal Mass 1Hakimah K. Suhaimi100% (1)
- Endometriosis, ovarian cancer stages, infertility factors, missed abortion, accidental hemorrhage, pre-requests for forcepsDocument20 pagesEndometriosis, ovarian cancer stages, infertility factors, missed abortion, accidental hemorrhage, pre-requests for forcepsDr-Amr Yakout MohamedNo ratings yet
- Introduction of Pediatric Nursing: Om Nursing Academy Anil Kantiwal Gudha (Whatsapp 9694936335)Document4 pagesIntroduction of Pediatric Nursing: Om Nursing Academy Anil Kantiwal Gudha (Whatsapp 9694936335)Preeti ChouhanNo ratings yet
- Osce PG 1Document18 pagesOsce PG 1Mobin Ur Rehman Khan100% (1)
- Abdominal HysterectomyDocument28 pagesAbdominal HysterectomyNatanael SusantoNo ratings yet
- Pregnant Abdomen Exam GuideDocument16 pagesPregnant Abdomen Exam GuideMuhammad Aamir IqbalNo ratings yet
- OSCE Must Knows For All SubjectsDocument8 pagesOSCE Must Knows For All SubjectsPrincess Jeanne Roque GairanodNo ratings yet
- Idea of OSCE in Obstetric.4012829.Powerpoint 1Document19 pagesIdea of OSCE in Obstetric.4012829.Powerpoint 1Aitzaz AhmedNo ratings yet
- Obgy Instruments Drugs SpecimensDocument336 pagesObgy Instruments Drugs SpecimensDeepesh NaikNo ratings yet
- Cesarean Surgical Techniques - GLOWMDocument36 pagesCesarean Surgical Techniques - GLOWMOana BalintNo ratings yet
- Surgery BookDocument95 pagesSurgery BookKhaled Mahmud100% (1)
- Instrumental DeliveryDocument25 pagesInstrumental DeliveryAhmed ElmohandesNo ratings yet
- Guide to Dysfunctional Labour and Cephalopelvic Disproportion (CPDDocument128 pagesGuide to Dysfunctional Labour and Cephalopelvic Disproportion (CPDDebjyoti KarmakarNo ratings yet
- OSCE Revision OBG DocumentDocument60 pagesOSCE Revision OBG DocumentshreyaNo ratings yet
- Golden Pearls of Gynecology and Obstetrics by DR Nadeem SHBDocument10 pagesGolden Pearls of Gynecology and Obstetrics by DR Nadeem SHBusamaNo ratings yet
- SYNOPSISDocument25 pagesSYNOPSISpriyankaNo ratings yet
- Antepartum & Postpartum Hemorrhage (APH &PPH) : Anita DeodharDocument81 pagesAntepartum & Postpartum Hemorrhage (APH &PPH) : Anita DeodharAnjali Rahul AjmeriNo ratings yet
- MCN Reviewer DefinitionOfTermsDocument10 pagesMCN Reviewer DefinitionOfTermsJenessel Ann P DaugNo ratings yet
- Post-Partum Haemorrhage: Causes and Risk FactorsDocument12 pagesPost-Partum Haemorrhage: Causes and Risk FactorsLindha GraNo ratings yet
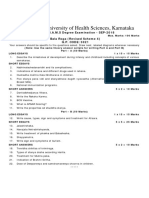
- Rajiv Gandhi University of Health Sciences, Karnataka III Year B.A.M.S Degree Examination - SEP-2018Document8 pagesRajiv Gandhi University of Health Sciences, Karnataka III Year B.A.M.S Degree Examination - SEP-2018Shravanthi SubrahmanyaNo ratings yet
- Oxytocin and Ergot DerivativesDocument36 pagesOxytocin and Ergot Derivativesrevathidadam55555No ratings yet
- 302340KWDocument22 pages302340KWValarmathiNo ratings yet
- Amniotic Fluid EmbolismDocument10 pagesAmniotic Fluid EmbolismRebecca ApeladoNo ratings yet
- 2019 Hubungan Riwayat Preeklamsi Dengan Kejadian PerdarahanDocument8 pages2019 Hubungan Riwayat Preeklamsi Dengan Kejadian Perdarahanmuhammadimron287No ratings yet
- JurnalDocument7 pagesJurnalKarina GoysalNo ratings yet
- DR Fleischer Obstetric Hemorrhage PresentationDocument66 pagesDR Fleischer Obstetric Hemorrhage PresentationHabebt MusabNo ratings yet
- FINAL AddisMeetingReport 0627Document125 pagesFINAL AddisMeetingReport 0627Yusuf KamaruddinNo ratings yet
- Postpartum HemorrhageDocument30 pagesPostpartum HemorrhageMusekhirNo ratings yet
- Pharmacology Reproductive Maternity NewbornDocument24 pagesPharmacology Reproductive Maternity Newbornamasoud96 amasoud96No ratings yet
- Hubungan Karakteristik Ibu Inpartu Terhadap Kejadian Perdarahan Postpartum Di Rsu Budi Kemuliaan Periode Tahun 2019Document10 pagesHubungan Karakteristik Ibu Inpartu Terhadap Kejadian Perdarahan Postpartum Di Rsu Budi Kemuliaan Periode Tahun 2019MiMa Muach LadyzNo ratings yet
- Postpartum Haemorrhage Causes and ManagementDocument51 pagesPostpartum Haemorrhage Causes and ManagementBasudev chNo ratings yet
- Labor and Delivery: By: Ma. Kizianne Krystel ManioDocument43 pagesLabor and Delivery: By: Ma. Kizianne Krystel ManioJohn Christian LasalitaNo ratings yet
- PPH ProcedureDocument15 pagesPPH ProceduremodelelevenNo ratings yet
- Management of Normal Labor and PartographDocument89 pagesManagement of Normal Labor and PartographKIPA SHRESTHANo ratings yet
- The Normal and Pathologic Postpartum UterusDocument10 pagesThe Normal and Pathologic Postpartum UterusAlberto BrahmNo ratings yet
- The Normal and Pathologic Postpartum Uterus: P. Kelehan and E. E. MooneyDocument10 pagesThe Normal and Pathologic Postpartum Uterus: P. Kelehan and E. E. MooneyAlberto BrahmNo ratings yet
- DR Ward ClassDocument36 pagesDR Ward ClassChristy Mutia AlumbroNo ratings yet