Professional Documents
Culture Documents
Predictors of Acute, Subacute and Late Stent Thrombosis After Acute MI Primary Angioplasty in The Horizons AMI Trial
Uploaded by
Bayu Setia0 ratings0% found this document useful (0 votes)
12 views28 pagesinvasive
Original Title
stennnn trombosis
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentinvasive
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
12 views28 pagesPredictors of Acute, Subacute and Late Stent Thrombosis After Acute MI Primary Angioplasty in The Horizons AMI Trial
Uploaded by
Bayu Setiainvasive
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 28
Predictors of Acute, Subacute and
Late Stent Thrombosis After Acute
MI Primary Angioplasty in the
Horizons AMI Trial
George D. Dangas, Alexandra J. Lansky,
Bruce R. Brodie, Bernhard Witzenbichler,
Giulio Guagliumi, Jan Z. Peruga, Dariusz Dudek,
Martin Moeckel, Helen Parise, Roxana Mehran,
and Gregg W. Stone
Disclosures
Speaker honoraria Sanofi-Aventis and BMS (not
a sponsor of this study) significant
Speaker honoraria and consulting fees
Medicines Co modest
Boston Scientific modest
Both provided research grant support for the
Horizons Trial
Background
Stent thrombosis (ST) is a serious adverse event
which occurs more frequently in pts with STEMI
Since the pathophysiologic mechanisms of ST
may vary, it is conventionally categorized
according to its timing after stenting:
0-24 hours (acute ST)
1-30 days (subacute ST)
1-12 months (late ST)
We sought to determine the clinical and
angiographic predictors of ST according to its
timing in pts with STEMI undergoing primary PCI
Harmonizing Outcomes with Revascularization and Stents in AMI
3602 pts with STEMI with symptom onset 12 hours
Emergent angiography, followed by triage to
Primary PCI CABG Medical Rx
UFH + GP IIb/IIIa inhibitor
(abciximab or eptifibatide)
Bivalirudin monotherapy
( provisional GP IIb/IIIa)
Aspirin, thienopyridine
R
1:1
3006 pts eligible for stent randomization
R
3:1
Bare metal EXPRESS stent Paclitaxel-eluting TAXUS stent
Clinical FU at 30 days, 6 months, 1 year, and then
yearly through 5 years; angio FU at 13 months
Diff = 0.0% [-1.6, 1.5]
RR = 0.99 [0.76, 1.30]
P
sup
= 0.95
Primary Endpoints at 30 Days
Diff = -3.3% [-5.0, -1.6]
RR = 0.60 [0.46, 0.77]
P
NI
0.0001
P
sup
0.0001
Diff = -2.9% [-4.9, -0.8]
RR = 0.76 [0.63, 0.92]
P
NI
0.0001
P
sup
= 0.005
1 endpoint 1 endpoint
Stone GW et al. NEJ M 2008;358:2218-30
Major 2 endpoint
1-Year Mortality (All-Cause)
Number at risk
Bivalirudin alone
Heparin+GPIIb/IIIa
1800 1705 1684 1669 1520
1802 1679 1664 1647 1487
M
o
r
t
a
l
i
t
y
(
%
)
0
1
2
3
4
5
Time in Months
0 1 2 3 4 5 6 7 8 9 10 11 12
Bivalirudin alone (n=1800)
Heparin + GPIIb/IIIa (n=1802)
4.8%
3.4%
Diff [95%CI] =
-1.4% [-2.7,-0.1]
HR [95%CI] =
0.70 [0.51, 0.98]
P=0.036
3.1%
2.1%
= 1.0%
P=0.049
= 1.4%
Stent Thrombosis Analysis
In the current analysis we included all
HORIZONS-AMI pts who received a stent,
either DES (any type) or only BMS (n=3203)
Stent thrombosis (n=107 [3.3%] within 1-year)
was defined as Definite or Probable by the
ARC criteria, as adjudicated by an
independent CEC blinded to stent and
pharmacology use
Objectives
Stent thrombosis and timing according to:
Stent type (any DES vs. onlyBMS, 94% rand)
Antithrombin type (UFH+GPI vs. Bival, 100% rand)
GPI selection (abciximab vs. eptifibatide, stratified)
Clopidogrel loading dose (300 vs. 600 mg, stratified)
Pre randomization UFH (yes vs. no, stratified)
Univariate and multivariable predictors of stent
thrombosis (ARC Def/Prob) from 36 variables
Acute, subacute, late, and 1-year
Statistical Methods
Kaplan-Meier methods were used to plot landmark time-to-event
curves, compared using the logrank test
Cox proportional hazards used to derive the independent
predictors of ST via stepwise regression (=0.05)
Potential covariates (36) for inclusion in the models:
CLINICAL (20): Bivalirudin (randomized v. UFH+IIb/IIIa), Any DES (v. BMS
only), Age, Sex (Male), US clinical center, Clopidogrel Loading Dose, Pre-
Randomization Heparin, Current Smoking, History of IDDM, History of MI,
History of CHF, Killip Class 2-4, History of PVD, Anemia, Baseline Platelet
Count, Renal Insufficiency (Baseline CrCl<60), Anterior MI, Direct Stenting
Attempted, Post Dilation balloon used, Max Balloon Pressure
ANGIOGRAPHIC (16): Baseline RVD, Total Lesion Length, Stent to Lesion
Length Ratio, Number of stents, Worst angiographic view - Thrombus, Worst
angiographic view - Ulceration, Aneurysm, Baseline TIMI flow 0/1, Bifurcation
lesion, Moderate/Severe Calcification, Multiple Vessels Treated, Sustained
ventricular tachycardia or fibrillation on admission, Final TIMI flow 0/1, Final
Lesion MLD , Final Lesion DS>50%, Final Angiography with No Reflow
1-Year Stent Thrombosis: Impact of
Implanted Stent Type
3.3%
3.4%
HR [95%CI] =
0.98 [0.64-1.51]
P = 0.93
2261 2171 2147 2123 2097 1900
872 832 818 805 791 720
Number at risk
Any DES
BMS only
D
e
f
/
P
r
o
b
S
t
e
n
t
T
h
r
o
m
b
o
s
i
s
(
%
)
0
1
2
3
4
Time in days
0 30 60 90 120 150 180 210 240 270 300 330 365
Any DES
BMS Only
1-Year Stent Thrombosis: Impact of
Antithrombin (Primary Randomization)
3.2%
3.6%
HR [95%CI] =
1.13 [0.77-1.65]
P = 0.53
1611 1540 1525 1506 1485 1355
1591 1518 1495 1476 1457 1315
Number at risk
Bivalirudin
UFH+GPIIb/IIIa
D
e
f
/
P
r
o
b
S
t
e
n
t
T
h
r
o
m
b
o
s
i
s
(
%
)
0
1
2
3
4
Time in days
0 30 60 90 120 150 180 210 240 270 300 330 365
Bivalirudin monotherapy
Heparin + GPIIb/IIIa inhibitor
Acute Stent Thrombosis: Impact of
Antithrombin (Primary Randomization)
0.3%
1.5%
HR (95%CI) =
5.93 [2.06,17.04]
P = 0.0002
1611 1583 1580 1578 1577
1591 1587 1584 1583 1583
Number at risk
Bivalirudin
UFH+GPIIb/IIIa
D
e
f
/
P
r
o
b
S
t
e
n
t
T
h
r
o
m
b
o
s
i
s
(
%
)
0.0
0.5
1.0
1.5
2.0
2.5
3.0
3.5
Time in Hours
0 6 12 18 24
Bivalirudin monotherapy
Heparin + GPIIb/IIIa inhibitor
2.2%
3.0%
1.5%
0.3%
HR [95%CI] =
1.73 [0.47-1.13]
P = 0.06
HR [95%CI] =
5.93 [2.06-17.04]
P = 0.0002
1611
1591
1600 1562 1525 1506 1485 1355
1587 1521 1495 1476 1457 1315
Number at risk
Bivalirudin
UFH+GPIIb/IIIa
D
e
f
/
P
r
o
b
S
t
e
n
t
T
h
r
o
m
b
o
s
i
s
(
%
)
0.0
0.5
1.0
1.5
2.0
2.5
3.0
3.5
Time in Days
0 1 30 90 180 270 365
Stent Thrombosis 1-Day Landmark
Analysis: Impact of Antithrombin
Bivalirudin monotherapy
Heparin + GPIIb/IIIa inhibitor
2.8%
3.6%
HR [95%CI] =
0.78 [0.44-1.37]
P = 0.38
727 693 685 678 668 592
829 793 778 768 759 698
Number at risk
Eptifibatide
Abciximab
D
e
f
/
P
r
o
b
S
t
e
n
t
T
h
r
o
m
b
o
s
i
s
(
%
)
0
1
2
3
4
Time in days
0 30 60 90 120 150 180 210 240 270 300 330 365
Eptifibatide
Abciximab
1-Year Stent Thrombosis: Impact of
GPI in the UFH Group
3.0%
3.8%
HR [95%CI] =
1.30 [0.86-1.95]
P = 0.10
1-Year Stent Thrombosis: Impact of
Clopidogrel Loading Dose (all pts)
1983 1906 1881 1858 1832 1653
1034 983 974 965 952 871
Number at risk
600 mg
300 mg
600mg Clopidogrel
300mg Clopidogrel
D
e
f
/
P
r
o
b
S
t
e
n
t
T
h
r
o
m
b
o
s
i
s
(
%
)
0
1
2
3
4
5
Time in days
0 30 60 90 120 150 180 210 240 270 300 330 365
0.8%
2.2%
3.2%
0.8%
HR [95%CI] =
0.96 [0.41-2.23]
P = 0.92
HR [95%CI] =
1.47 [0.93,2.33]
P = 0.18
1983
1034
1978 1920 1881 1858 1832 1653
1027 990 974 965 952 871
Number at risk
600 mg
300 mg
D
e
f
/
P
r
o
b
S
t
e
n
t
T
h
r
o
m
b
o
s
i
s
(
%
)
0
1
2
3
4
5
Time in Days
0 1 30 90 180 270 365
Stent Thrombosis 1-Day Landmark
Analysis: Impact of Clopidogrel Loading
600mg Clopidogrel
300mg Clopidogrel
1.6%
3.4%
1.5%
1.2%
HR [95%CI] =
1.30 [0.54-3.16]
P = 0.56
HR [95%CI] =2.11
[1.07,4.17]
P = 0.03
1013
519
1009 990 969 957 943 863
514 497 486 480 474 430
Number at risk
600 mg
300 mg
D
e
f
/
P
r
o
b
S
t
e
n
t
T
h
r
o
m
b
o
s
i
s
(
%
)
0
1
2
3
4
5
Time in Days
0 1 30 90 180 270 365
Stent Thrombosis 1-Day Landmark Analysis:
Impact of Clopidogrel Loading (Bivalirudin)
600mg Clopidogrel
300mg Clopidogrel
600mg Clopidogrel
300mg Clopidogrel
2.8%
2.9%
0.4%
0%
HR=0.21
CI=0.01-3.88
P = 0.30
HR=1.08
CI= [0.57,2.05]
P = 0.81
1035
559
1034 995 977 963 951 852
557 537 531 528 521 482
Number at risk
600 mg
300 mg
D
e
f
/
P
r
o
b
S
t
e
n
t
T
h
r
o
m
b
o
s
i
s
(
%
)
0
1
2
3
4
5
Time in Days
0 1 30 90 180 270 365
P
int
antithrombin x clopidogrel LD = 0.16
Stent Thrombosis 1-Day Landmark Analysis:
Impact of Clopidogrel Loading (UFH+GPI)
Acute Stent Thrombosis: Impact of
Pre-Randomization Heparin
1066 1052 1051 1050 1049
545 531 529 528 528
Number at risk
P-R Heparin
No P-R Heparin
D
e
f
/
P
r
o
b
S
t
e
n
t
T
h
r
o
m
b
o
s
i
s
(
%
)
0.0
0.5
1.0
1.5
2.0
2.5
3.0
3.5
Time in Hours
0 6 12 18 24
Pre-Randomization Heparin
No Pre-Randomization Heparin
UFH+GPI
UFH+GPI
1211 1208 1207 1207 1207
378 377 375 374 374
P-R Heparin
No P-R Heparin
Bivalirudin
Bivalirudin
0.1%
0.8%
HR [95%CI] = 9.64 [1.00,92.70]
P = 0.02
0.9%
2.6%
HR [95%CI] =
3.07 [1.33,7.09]
P = 0.006
P
int
antithrombin x pre-rand hep = 0.39
Angiographic Characteristics (QCA)
ST
(N=107)
No ST
(N=3096)
P-
Value
Target lesion vessel
LAD 39.8% 40.2% 0.93
RCA 41.4% 43.9% 0.57
LCX 17.3% 15.0% 0.47
SVG 1.5% 0.9% 0.37
Lesion characteristics
Eccentric 4.5% 7.0% 0.27
Bend >45 degrees 7.6% 10.0% 0.37
Thrombus 70.7% 70.4% 0.95
Thrombus area mean 31.7 [23.0,43.4] 27.4 [17.1,40.4] 0.01
Calcification: Moderate/severe 34.6% 35.1% 0.90
Ulceration 4.5% 2.3% 0.14
Aneurysm 3.8% 1.4% 0.05
Mod. ACC/AHA lesion class B2/C 87.2% 85.5% 0.58
ST
(N=107)
No ST
(N=3096)
P-
Value
Baseline
Lesion length (mm) 14.2 [10.4,20.0] 14.7 [10.2,20.3] 0.84
Baseline RVD (mm) 2.87 [2.53,3.21] 2.87 [2.53,3.22] 0.94
Pre TIMI Flow 0/1 75.7% 59.4% 0.0006
Post procedure
Lesion MLD (mm) 2.30 [1.94,2.61] 2.34 [2.01,2.70] 0.20
Lesion DS% 20.1 [12.8,27.4] 18.4 [12.5,25.1] 0.11
Stent length 22.1 [16.5,33.1] 21.34 [16.0,28.3] 0.23
Stent overlap (mm) 3.1 [2.1,4.2] 2.8 [2.1,3.9] 0.41
Final TIMI flow 3 79.3% 88.1% 0.005
Index PCI Procedure QCA
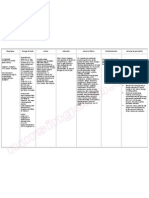
Independent Predictors of 1-Year ST
(Cox Model)
Variable HR [95% CI] P-value
Insulin-treated diabetes 3.42 [1.81, 6.47] 0.0002
Lesion ulceration 2.28 [0.99, 5.27] 0.05
Pre-PCI TIMI flow 0/1 2.22 [1.37, 3.61] 0.001
Current smoking 1.81 [1.20, 2.72] 0.005
Number of stents 1.31 [1.07, 1.60] 0.04
Clopidogrel loading dose 600mg 0.65 [0.44, 0.97] 0.04
Independent Predictors of Acute ST
(Cox Model)
Variable HR [95% CI] P-value
Pre-PCI TIMI flow 0/1 6.10 [1.43, 26.04] 0.01
Lesion ulceration 4.80 [1.41, 16.37] 0.01
Bivalirudin (v. UFH+GPI) 4.65 [1.59, 13.54] 0.005
Number of stents 1.50 [1.06, 2.12] 0.02
Pre-rand heparin 0.27 [0.12, 0.60] 0.002
Independent Predictors of Subacute ST
(Cox Model)
Variable HR [95% CI] P-value
Insulin-treated diabetes 4.43 [2.03, 9.65] 0.0002
History of CHF 4.16 [1.61, 10.76] 0.003
Pre-PCI TIMI flow 0/1 2.21 [1.05, 4.63] 0.04
Final TIMI flow 0/1 3.72 [1.10, 12.55] 0.03
Stent to lesion length ratio 1.44 [1.20, 1.71] <0.0001
Clopidogrel loading dose
600 mg (vs. 300 mg)
0.49 [0.27, 0.89] 0.01
Independent Predictors of Late ST
(Cox Model)
Variable HR [95% CI] P-value
Current smoking 4.05 [1.73, 9.48] 0.001
Insulin-treated diabetes 3.17 [0.95, 10.61] 0.06
History of prior MI 3.15 [1.39, 7.13] 0.006
Post stent dilation
balloon used
2.75 [1.31, 5.80] 0.008
Conclusions (1)
Following stent implantation in STEMI, ST
occurs frequently within the first 24 hours (0.9%),
between 1 and 30 days (1.6%), and between 1
month and 1 year (1.0%) 3.3% in total by 1 year
Acute, subacute and late ST appear to be related
to different factors
Pharmacological therapy, vessel flow, lesion
characteristics and number and length of stents
are the most important predictors of acute and
subacute ST events
Patient related factors including cigarette smoking
and prior MI are the most important predictors of
late ST events
Conclusions (2)
The type of stent implanted (DES vs. BMS)
was not related to ST during any time
interval up to 1-year
ST within 1-year occurred with similar
frequency in patients treated with UFH+GPI
and bivalirudin alone
However, acute ST was more common
with bivalirudin, especially within the 1
st
5
hours, whereas ST tended to be less
common with bivalirudin than with
UFH+GPI between 24 hours and 1-year
In the primary results of the HORIZONS-AMI trial,
bivalirudin monotherapy resulted in less major bleeding,
comparable rates of ischemia and improved survival
compared to UFH+GPI at 30 days and 1-year
The results of the present analysis suggest that
optimizing adjunct pharmacology with bivalirudin during
primary PCI may further improve outcomes:
Pre-randomization UFH attenuated the risk of acute ST
A 600 mg clopidogrel LD attenuated the risk of subacute ST
Whether a prolonged bivalirudin infusion (4-6 hrs) post-
PCI and/or an even more potent and rapid acting
thienopyridine agent might further reduce early ST in pts
with STEMI treated with bivalirudin (without increasing
bleeding) warrants further study
Implications
You might also like
- CRESTOR Launch Presentation January 2011Document40 pagesCRESTOR Launch Presentation January 2011Chikezie Onwukwe67% (3)
- 13-5-2010 MCQ FrcaDocument79 pages13-5-2010 MCQ FrcaMohmd Abdulhameed Sayed100% (2)
- Taxenes in Breast Cancer (Sharm)Document76 pagesTaxenes in Breast Cancer (Sharm)safasayedNo ratings yet
- Practice Intersection: How I Approach Thrombus in My Daily Clinical PracticeDocument57 pagesPractice Intersection: How I Approach Thrombus in My Daily Clinical PracticeSOLACI - Sociedad Latinoamericana de Cardiología IntervencionistaNo ratings yet
- TWILIGHT DM AjitDocument21 pagesTWILIGHT DM Ajitajit jadhavNo ratings yet
- Updated Hypertension GuidelineDocument88 pagesUpdated Hypertension Guidelinekenny631653No ratings yet
- Digoxin Reduces 30-Day All-Cause Hospital Admission in Ambulatory Older Patients With Chronic Heart Failure and Reduced Ejection FractionDocument31 pagesDigoxin Reduces 30-Day All-Cause Hospital Admission in Ambulatory Older Patients With Chronic Heart Failure and Reduced Ejection FractionYanely AlmaguerNo ratings yet
- Coronary Artery DiseaseDocument82 pagesCoronary Artery Diseasecortassa265No ratings yet
- Bladder Preservation in Muscle Invasive Disease: Nick James University of Birmingham @prof - Nick - James #NjbladdercancerDocument38 pagesBladder Preservation in Muscle Invasive Disease: Nick James University of Birmingham @prof - Nick - James #NjbladdercancerProf_Nick_JamesNo ratings yet
- Bhatt CogentDocument21 pagesBhatt CogentdoctordocsNo ratings yet
- ViewDocument1 pageViewmoche_raulNo ratings yet
- Essay Komstat Farhan HF RahmanDocument5 pagesEssay Komstat Farhan HF RahmantaufikramadhaniNo ratings yet
- Critical Analysis Journal ArticleDocument5 pagesCritical Analysis Journal Articlesarah javedNo ratings yet
- 01 Ortel BRIDGEDocument24 pages01 Ortel BRIDGEWallnut StreetNo ratings yet
- Kol Slide Kit Atac 100Document43 pagesKol Slide Kit Atac 100api-26302710No ratings yet
- WCLC2013 Alimta Final JB-1Document1 pageWCLC2013 Alimta Final JB-1Shru2611No ratings yet
- 6 Studii StatineDocument37 pages6 Studii Statinejust4uhopeNo ratings yet
- Rosuvastatina Disminuye La Incidencia de Nefropatía Por Contraste en Pacientes Con Síndrome Coronarios Agudos Que Reciben Estrategia Invasiva PrecozDocument22 pagesRosuvastatina Disminuye La Incidencia de Nefropatía Por Contraste en Pacientes Con Síndrome Coronarios Agudos Que Reciben Estrategia Invasiva PrecozSOLACI - Sociedad Latinoamericana de Cardiología IntervencionistaNo ratings yet
- Graves Disease: Dr. Bobby Fildian Siswanto Rumah Sakit Mitra KemayoranDocument28 pagesGraves Disease: Dr. Bobby Fildian Siswanto Rumah Sakit Mitra KemayoranBobby Fildian SiswantoNo ratings yet
- Usefulness of quantiFERON 174 TB Gold On LTBI deDocument14 pagesUsefulness of quantiFERON 174 TB Gold On LTBI deConstantin PopescuNo ratings yet
- 1 EndometriozaDocument33 pages1 EndometriozaMandici ConstantinNo ratings yet
- Berg RRP TalkDocument39 pagesBerg RRP TalkΕμμανουήλ ΚακαβελάκηςNo ratings yet
- Impact of High Sensitivity Troponins For 6nov Cardiac ForumDocument39 pagesImpact of High Sensitivity Troponins For 6nov Cardiac Forummouna6685No ratings yet
- Nejmoa1113162 AppendixDocument35 pagesNejmoa1113162 AppendixayuannisahusnaNo ratings yet
- Effect of Nateglinide On The Incidence of DiabetesDocument31 pagesEffect of Nateglinide On The Incidence of Diabetesfred opinionNo ratings yet
- ACCP Cardiology PRN JC June 2022Document16 pagesACCP Cardiology PRN JC June 2022topNo ratings yet
- Ezaa034 Supplementary DataDocument3 pagesEzaa034 Supplementary DataElena CamposNo ratings yet
- Barb Melo SkyDocument17 pagesBarb Melo SkyAfiqah So JasmiNo ratings yet
- Evolve Study Journal Club PresentationDocument62 pagesEvolve Study Journal Club PresentationsantoshvelloreNo ratings yet
- Bladder Preservation in Muscle Invasive Disease: Nick James University of WarwickDocument41 pagesBladder Preservation in Muscle Invasive Disease: Nick James University of WarwickProf_Nick_JamesNo ratings yet
- Adj Her 2 SlidesDocument37 pagesAdj Her 2 SlidesDr. Luis M. Zetina ToacheNo ratings yet
- 2 TishleDocument38 pages2 TishleIRANo ratings yet
- Sepsis-3: Jeffrey Ariesta PutraDocument35 pagesSepsis-3: Jeffrey Ariesta PutraMaria FernandezNo ratings yet
- Trombólisis Tromboembolia Pulmonar Dosis Media Total 2022 CartaDocument4 pagesTrombólisis Tromboembolia Pulmonar Dosis Media Total 2022 CartaOscar BushNo ratings yet
- Zhes055740 ww1Document8 pagesZhes055740 ww1Vincent PratamaNo ratings yet
- 2 Imaging of Stroke - January 2011Document40 pages2 Imaging of Stroke - January 2011Rika FitriaNo ratings yet
- Stampede M0 ASTRO Presentation Sept 2014Document24 pagesStampede M0 ASTRO Presentation Sept 2014Prof_Nick_JamesNo ratings yet
- Circinterventions Circcvint-2018-006837 Supp1 JR CathDocument5 pagesCircinterventions Circcvint-2018-006837 Supp1 JR CathRahayu SeptiariniNo ratings yet
- Jarir Atthobari - Clinical TrialDocument38 pagesJarir Atthobari - Clinical TrialLilian KusumaNo ratings yet
- Table 1: Odds Ratio (CI) : Ulcer SA Positive Chi-Square P-ValueDocument3 pagesTable 1: Odds Ratio (CI) : Ulcer SA Positive Chi-Square P-ValueHerni MulianiNo ratings yet
- ASCO Bladder Cancer Talk Jun 2013 v2Document37 pagesASCO Bladder Cancer Talk Jun 2013 v2Prof_Nick_JamesNo ratings yet
- ACS Management and ESC GuidelinesDocument56 pagesACS Management and ESC GuidelinesAnonymous NeRC5JYiSNo ratings yet
- Clear PlateletsDocument17 pagesClear PlateletsJorge Peregrino BragaNo ratings yet
- Clopidogrel in Patients With Cerebrovascular Disease: Part 2: Clinical EvidenceDocument51 pagesClopidogrel in Patients With Cerebrovascular Disease: Part 2: Clinical Evidenceward2713No ratings yet
- Risks of Nsaids: Focus On Gi Risks of Over-The-Counter NsaidsDocument40 pagesRisks of Nsaids: Focus On Gi Risks of Over-The-Counter Nsaidspaul_calburean7899No ratings yet
- FLAD1 Is Up-Regulated in Gastric Cancer and Is A Potential Prediction of PrognosisDocument10 pagesFLAD1 Is Up-Regulated in Gastric Cancer and Is A Potential Prediction of PrognosisAriani ArinNo ratings yet
- Management of DVTDocument46 pagesManagement of DVTSteven Hartanto Kurniawan50% (2)
- MMC 1Document18 pagesMMC 1henryweiNo ratings yet
- Gist WorkshopDocument38 pagesGist WorkshopRuki HartawanNo ratings yet
- DDD Vs VVIDocument48 pagesDDD Vs VVIGreen ButtercupNo ratings yet
- Diagnostic TestingDocument55 pagesDiagnostic TestingMoldovan Nicolae-AndreiNo ratings yet
- Adjuvant and Neoadjuvant ChemotherapyDocument22 pagesAdjuvant and Neoadjuvant Chemotherapyprabushankar7No ratings yet
- Osteoporosis - Detection and TreatmentDocument35 pagesOsteoporosis - Detection and TreatmentKa ManNo ratings yet
- Analisis Deskriptif Variable Numerik HendraDocument7 pagesAnalisis Deskriptif Variable Numerik HendraEvi MaisyariNo ratings yet
- DIABertelt2017 14Document7 pagesDIABertelt2017 14marsim92No ratings yet
- SupplementaryDocument5 pagesSupplementaryResidenPatKlin Juli2022No ratings yet
- William C. Cushman, MD, FACP, FAHA: Veterans Affairs Medical Center, Memphis, TN For The ACCORD Study GroupDocument24 pagesWilliam C. Cushman, MD, FACP, FAHA: Veterans Affairs Medical Center, Memphis, TN For The ACCORD Study GroupCardiologyNetwork.comNo ratings yet
- PROVE IT Results - ACC LBCT Final 3-4-04Document18 pagesPROVE IT Results - ACC LBCT Final 3-4-04Em PeceroNo ratings yet
- The New Trauma Score (NTS) : A Modification of The Revised Trauma Score For Better Trauma Mortality PredictionDocument9 pagesThe New Trauma Score (NTS) : A Modification of The Revised Trauma Score For Better Trauma Mortality PredictionاوكتافياNo ratings yet
- Disorders of Potassium Balance: Zhao Chenghai PathophysiologyDocument24 pagesDisorders of Potassium Balance: Zhao Chenghai PathophysiologyBayu SetiaNo ratings yet
- Radiographics 2007 7-8 27 (4) 989-1004Document1 pageRadiographics 2007 7-8 27 (4) 989-1004Bayu SetiaNo ratings yet
- Gizi Ari ChandraDocument13 pagesGizi Ari ChandraBayu SetiaNo ratings yet
- Kawasaki Disease: Focus On Clinical Manifestation: Dr. I B Agung Winaya, SpaDocument24 pagesKawasaki Disease: Focus On Clinical Manifestation: Dr. I B Agung Winaya, SpaBayu SetiaNo ratings yet
- High Alert MedicationDocument46 pagesHigh Alert MedicationDewi Wara ShintaNo ratings yet
- Aug31 Committee On Ways & Means Approves Tax Exemption of Donations To Proposed Office of Rare DiseasesDocument2 pagesAug31 Committee On Ways & Means Approves Tax Exemption of Donations To Proposed Office of Rare Diseasespribhor2No ratings yet
- Therapy in TuberculosisDocument4 pagesTherapy in TuberculosisSamir SkejicNo ratings yet
- 2019 Intake and Output MeasurementDocument2 pages2019 Intake and Output Measurementharley dela cruzNo ratings yet
- Hydrocephalus and ADHD OverviewDocument4 pagesHydrocephalus and ADHD OverviewAlthea Ninotschka AgaloosNo ratings yet
- Perspectives On Episodic and Semantic Memory Retrieval. Chaprer 1.1 of The Book Handbook of Episodic Memory.Document2 pagesPerspectives On Episodic and Semantic Memory Retrieval. Chaprer 1.1 of The Book Handbook of Episodic Memory.Tahi GuzmánNo ratings yet
- Uterine Sub Mucosal Leiomyoma (Fibroid) - A Case ReportDocument5 pagesUterine Sub Mucosal Leiomyoma (Fibroid) - A Case ReportInternational Organization of Scientific Research (IOSR)No ratings yet
- Med Surg Test AnswersDocument9 pagesMed Surg Test AnswersAshley Rose100% (3)
- Ewout JasperDocument400 pagesEwout JasperJohnny AtmanNo ratings yet
- Caregiving Body TemperatureDocument69 pagesCaregiving Body TemperatureDanny Line100% (1)
- Lap InstrumentsDocument7 pagesLap InstrumentskhaleeltahaNo ratings yet
- Curofy Best Ophthalmology CasesDocument24 pagesCurofy Best Ophthalmology Casespradeep100% (1)
- Key Topics in General SurgeryDocument455 pagesKey Topics in General SurgeryAlbano Hall75% (16)
- Dental Implants PerioDocument54 pagesDental Implants PerioFourthMolar.com0% (1)
- Parts of The Body and Health Problem Learning Objectives Students Should Be Able To Express The Location of The Pain in The Body VocabularyDocument13 pagesParts of The Body and Health Problem Learning Objectives Students Should Be Able To Express The Location of The Pain in The Body VocabularyLini Pisti22No ratings yet
- What Is Gastritis (ESP)Document1 pageWhat Is Gastritis (ESP)Rova Lavi SynNo ratings yet
- HCP EngDocument109 pagesHCP Engclap smrNo ratings yet
- Hyperemesis Gravidarum AND Wernicke'S Encephalopathy SyndromeDocument18 pagesHyperemesis Gravidarum AND Wernicke'S Encephalopathy SyndromeRaden Atika PermadiNo ratings yet
- Hands On: The Approach To The Patient Presenting With Multiple Joint PainDocument12 pagesHands On: The Approach To The Patient Presenting With Multiple Joint PainMithun CbNo ratings yet
- Imci Case StudyDocument10 pagesImci Case StudyRhika Mae Flores Valdez100% (1)
- Oregon V Azar ComplaintDocument109 pagesOregon V Azar ComplaintHonolulu Star-Advertiser100% (1)
- Ivp Dari WikipediaDocument6 pagesIvp Dari Wikipediabellatrix orionNo ratings yet
- Clonidine HydrochlorideDocument1 pageClonidine HydrochlorideLovelyn Joy Abubo CortezNo ratings yet
- Pathology Mcqs 2Document6 pagesPathology Mcqs 2Numan Rox100% (5)
- Hipo - Hiper SubDocument123 pagesHipo - Hiper SubdankouzielNo ratings yet
- HSV Keratitis Treatment Guideline HarvardDocument69 pagesHSV Keratitis Treatment Guideline HarvardabciximabNo ratings yet
- FryetteDocument2 pagesFryetteSaba KhanNo ratings yet
- Dermatitis Perioral 2015Document7 pagesDermatitis Perioral 2015Carlos Augusto Morales ChaconNo ratings yet
- Woodcutters TechniqueDocument3 pagesWoodcutters TechniqueToo SmallNo ratings yet