Professional Documents
Culture Documents
Cholesterol Synthesis, Transport, and Excretion
Uploaded by
abcdshOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cholesterol Synthesis, Transport, and Excretion
Uploaded by
abcdshCopyright:
Available Formats
Abdul Salam M Sofro
Faculty of Medicine
YARSI University
Learning objectives
By the end of lectures, students are
expected to understand:
The process of cholesterol synthesis
and excretion
Cholesterol transport in blood
circulation
Introduction
Cholesterol present in tissue & in plasma
lipoproteins either as free cholesterol or, combined
with a long chain FA as cholesteryl ester
It is synthesized in many tissues from acetyl-CoA
and is ultimately eliminated from the body in the
bile as cholesterol or bile salts
Cholesterol is precursor of all other steroids in the
body (corticosteroids, sex hormones, bile acids &
vitamin D)
It is typically a product of animal metabolism
occurs in food of animal origin (egg yolk, meat,
liver, brain)
Slightly less than half of the cholesterol in the
body derives from biosynthesis de novo.
Biosynthesis in the liver accounts for
approximately 10%, and in the intestines
approximately 15%, of the amount produced
each day.
Cholesterol synthesis occurs in the cytoplasm
and microsomes from the two-carbon acetate
group of acetyl-CoA.
Biomedical importance
Cholesteryl ester is a storage form of cholesterol
found in most tissues
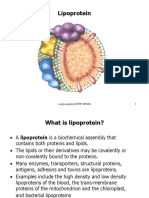
It is transported as cargo in the hydrophobic core
of lipoprotein
LDL is the mediator of cholesterol & cholesteryl
ester uptake into many tissues
Free cholesterol is removed from tissues by HDL
and transported to liver for conversion to bile
acids (cholesterol is major constituent of
gallstones)
Cholesterol plays major role in the genesis of
atherosclerosis
Acetyl-CoA is the source of all carbon atom
in cholesterol
Five stages in biosynthesis of cholesterol:
Synthesis of Mevalonate, a six-carbon compound,
from acetyl-CoA
Isoprenoid units are formed from mevalonate by
loss of CO2
Six isoprenoid units condense to form the
intermediate squalene
Squalene cyclisized to parent steroid, lanosterol
Cholesterol is formed from lanosterol after several
further steps including the loss of three methyl
groups
Pathway of cholesterol biosynthesis. Synthesis begins with the transport of acetyl-CoA ffrom
the mitochondrion to the cytosol. The rate limiting step occurs at the 3-hydroxy-3-
methylglutaryl-CoA (HMG-CoA) reducatase, HMGR catalyzed step. The phosphorylation
reactions are required to solubilize the isoprenoid intermediates in the pathway.
Regulating Cholesterol Synthesis
Normal healthy adults synthesize cholesterol
at a rate of approximately 1g/day and
consume approximately 0.3g/day. A relatively
constant level of cholesterol in the body (150
- 200 mg/dL) is maintained primarily by
controlling the level of de novo synthesis.
The level of cholesterol synthesis is
regulated in part by the dietary intake of
cholesterol.
Regulation of HMG-CoA reductase:
Reduced activity in fasting animals
(reduced synthesis of cholesterol during
fasting)
Feedback mechanism whereby HMG-
CoA reductase in liver in inhibited by
mevalonate, the immediate product &
cholesterol, the main product of the
pathway (cholesterol metabolite, eg.
oxygenated sterol is considered to
repress transcription of the HMG-CoA
reductase gene
Many factors influence the cholesterol balance
in tissues:
Increase is due to uptake of cholesterol-
containing lipoproteins by receptors;
uptake of free cholesterol from
cholesterol-rich lipoproteins to the cell
membrane; cholesterol synthesis; and
hydrolysis of cholesteryl-ester by the
enzyme cholesteryl ester hydrolase
Decrease is due to efflux of cholesterol
from the membrane to lipoproteins of low
cholesterol potential; esterification of
cholesterol by acyl-CoA:cholesterol
acyltransferase (ACAT); and utilization of
cholesterol for synthesis of other steroids,
such as hormones or bile acids in liver
The cellular supply of cholesterol is maintained
at a steady level by three distinct mechanisms:
1. Regulation of HMGR activity and levels
2. Regulation of excess intracellular free
cholesterol through the activity of acyl-
CoA:cholesterol acyltransferase, ACAT
3. Regulation of plasma cholesterol levels via
LDL receptor-mediated uptake and HDL-
mediated reverse transport.
Cholesterol is transported between
tissues in plasma lipoproteins
In human on westernized diets, the total plasma
cholesterol is about 5.2 mmol/L (rising with age
& wide variations between individuals)
Mostly in esterified form & transported in plasma
lipoproteins being the highest in the LDL (or in
VLDL if VLDL is quantitatively more prominent)
Dietary cholesterol takes several days to
equilibrate with cholesterol in the plasma &
several weeks to equilibrate with cholesterol of
the tissues
Good & bad Cholesterol and their effect on
health
It is commonly known that a high level
of cholesterol in the blood
hypercholesterolemia poses a risk for
coronary heart disease (CHD) & heart
attack.
Cholesterol is insoluble in the blood, it is
transported to and from the cells by
carriers known as lipoproteins
Low-density lipoprotein (LDL) or Bad
Cholesterol
Is the major cholesterol carrier in the
blood if too much LDL cholesterol
circulates in the blood.
It can slowly build up in the walls of the
arteries feeding the heart and brain.
Together with other substances it can
form plaque, a thick, hard deposit that
can clog those arteries (a condition
known as atherosclerosis)
High-density lipoprotein (HDL) or Good
Cholesterol
Carries about one-third to one-fourth of blood
cholesterol
Experts think HDL tends to carry cholesterol
away from the arteries and back to the liver,
where it is metabolized and removed.
It is believed that HDL can remove excess
cholesterol from plaques and therefore slow
their growth. However, while a high level of HDL
decreases the associated risks, a low level of
HDL cholesterol level may increase the
possibility of stroke or heart attack.
Cholesterol excretion
Cholesterol must enter the liver & be excreted in
the bile as cholesterol or bile acids (salts)
About 1 g of cholesterol is eliminated from the
body per day. Approx. half is excreted in the
feces after conversion to bile acids, the
remainder is excreted as cholesterol.
Much of the cholesterol excreted in the bile is
reabsorbed & at least some of the cholesterol
that serves as precursor for the fecal sterols is
derived from the intestinal mucosa.
Coprostanol is the principal sterol in the
feces (formed from cholesterol by the
bacteria in lower intestine)
Cholesterol
7-OH-Cholesterol
Cholyl-CoA
Chenodeoxy-
cholyl-CoA
Taurocholic acid
Glycocholic acid
Deoxycholic acid
Lithocholic acid
Tauro- & glyco-
Chenodeoxycholic acid
(primary bile acid)
(primary bile acid)
(primary bile acid)
(secondary bile acid)
(secondary bile acid)
7-hydroxylase
Vit. C
(-)
Bile acids
Vit. C defic.
Cholesterol
(+)
Most bile acids return to the liver in
the enterohepatic circulation
Product of fat digestion including
cholesterol are absorbed in the first 100
cm of small intestinum
Primary & secondary bile acids are
absorbed almost exclusively on the
ileum, returning to the liver by way of
portal circulation about 98-99% of the
bile acids secreted into the intestine
(called enterohepatic circulation)
Perhaps only as little as 400 mg/d escapes
absorption & eliminated in the feces
(represent a major pathway for the
elimination of cholesterol)
About 3-5 g bile salts can be cycled through
the intestine 6-10 times with only a small
amount lost in the feces each day an
amount of bile acid equivalent to that lost in
the feces is synthesized from cholesterol by
the liver.
You might also like
- Cholesterol Synthesis, Transport, and ExcretionDocument37 pagesCholesterol Synthesis, Transport, and ExcretionEdo Pramana Putra100% (2)
- UK Guidelines Iron Deficiency in Pregnancy PDFDocument34 pagesUK Guidelines Iron Deficiency in Pregnancy PDFYoga Rhamada SiregarNo ratings yet
- Introduction To MetabolismDocument27 pagesIntroduction To Metabolismcream oNo ratings yet
- Gluconeogenesis, Glycogen MetabolismDocument35 pagesGluconeogenesis, Glycogen MetabolismdanielachynaNo ratings yet
- Digestion and Absorption of Carbohydrates: by Arpitha 3 BnysDocument31 pagesDigestion and Absorption of Carbohydrates: by Arpitha 3 BnysBig ZeroNo ratings yet
- Cholesterol Synthesis, Transport, and Excretion: Abdul Salam M Sofro Faculty of Medicine YARSI UniversityDocument39 pagesCholesterol Synthesis, Transport, and Excretion: Abdul Salam M Sofro Faculty of Medicine YARSI UniversitySofie Hanafiah NuruddhuhaNo ratings yet
- BCH 206 CholesterolDocument3 pagesBCH 206 CholesterolNewtonNo ratings yet
- Digestion of Lipids. Transport Forms of LipidsDocument91 pagesDigestion of Lipids. Transport Forms of LipidsAhmed FtsNo ratings yet
- Lipid Metabolism - (V) - Cholesterol and LipoproteinsDocument35 pagesLipid Metabolism - (V) - Cholesterol and Lipoproteinslightning proNo ratings yet
- Metabolism of Lipids 2Document71 pagesMetabolism of Lipids 2Mi PatelNo ratings yet
- Metabolism of CholesterolDocument17 pagesMetabolism of CholesterolAvhishek PatelNo ratings yet
- Cholesterol: Synthesis and MetabolismDocument45 pagesCholesterol: Synthesis and MetabolismSoffa ShmuelNo ratings yet
- Cholesterol FinalDocument55 pagesCholesterol FinalSobha MatthewNo ratings yet
- CholestrolDocument6 pagesCholestrolprince_woondNo ratings yet
- Cholesterol: by Arooj Fatima Roll Number:MCHF18M028Document23 pagesCholesterol: by Arooj Fatima Roll Number:MCHF18M028ماہ نور فاطمہNo ratings yet
- Pharmacology :MIT:Lees:8Document8 pagesPharmacology :MIT:Lees:8Louis FortunatoNo ratings yet
- Cholesterol SphingolipidsDocument31 pagesCholesterol SphingolipidsMaryam KNo ratings yet
- Reverse Cholesterol TransportDocument29 pagesReverse Cholesterol TransportSolomon RotimiNo ratings yet
- Cholesterol Metabolism BC100Document27 pagesCholesterol Metabolism BC100Anthony KabadiNo ratings yet
- Biosynthesis of CholesterolDocument20 pagesBiosynthesis of CholesterolAboubakar Moalim Mahad moh'dNo ratings yet
- Biochemistry Board Review 1 PDFDocument15 pagesBiochemistry Board Review 1 PDFKgerbNo ratings yet
- Fatty Acid Size Location of Beta-OxidationDocument19 pagesFatty Acid Size Location of Beta-OxidationJann Leslie NinadaNo ratings yet
- Metabolism of LipidsDocument98 pagesMetabolism of LipidsLyra GetNo ratings yet
- Biochemistry of Lipoprotein & DyslipidemiaDocument79 pagesBiochemistry of Lipoprotein & DyslipidemiaDamal An NasherNo ratings yet
- Metabolism of CholesterolDocument65 pagesMetabolism of CholesterolSafura IjazNo ratings yet
- Metabolism: CholesterolDocument4 pagesMetabolism: CholesterolAnomar MRgNo ratings yet
- Metabolism of CholesterolDocument9 pagesMetabolism of CholesterolRushikesh EwareNo ratings yet
- Metabolism of CholesterolDocument9 pagesMetabolism of CholesterolRushikesh EwareNo ratings yet
- Atherosclerosis: Reporter: Collera, Charissa Constantino, Venice Clemena, Adnan Coronel, Romeo Cordova, KarlaDocument73 pagesAtherosclerosis: Reporter: Collera, Charissa Constantino, Venice Clemena, Adnan Coronel, Romeo Cordova, Karlaprecious_bustosNo ratings yet
- LIPDocument28 pagesLIPsamar yousif mohamedNo ratings yet
- Sirera, DyslipidemiaDocument68 pagesSirera, Dyslipidemiarsirera6409No ratings yet
- Energy Production 2. Energy Storage 3. Energy UtilizationDocument14 pagesEnergy Production 2. Energy Storage 3. Energy UtilizationLALITH SAI KNo ratings yet
- Metabolism of LipidsDocument37 pagesMetabolism of LipidsSafura IjazNo ratings yet
- Kuliah Biokimia Blok 2.4.1Document44 pagesKuliah Biokimia Blok 2.4.1Prajna PNo ratings yet
- Cholesterol Metabolism 2021Document43 pagesCholesterol Metabolism 2021Eniola abdullahi AduagbaNo ratings yet
- Lipoprotein & Dyslipidemia DR Lin Oswari Blok 8Document97 pagesLipoprotein & Dyslipidemia DR Lin Oswari Blok 8Izzah AtqaNo ratings yet
- 3 Lipid MetabolismDocument54 pages3 Lipid MetabolismRahadatul Aisy100% (1)
- B978012391909050061X PDFDocument7 pagesB978012391909050061X PDFLaura Melo ArenasNo ratings yet
- DyslipidemiaDocument3 pagesDyslipidemiaRaine ValdezNo ratings yet
- Metabolismoflipoproteins 171020040454Document66 pagesMetabolismoflipoproteins 171020040454Afeeda RazikNo ratings yet
- 1.overview of MetabolismDocument6 pages1.overview of Metabolismقتيبه خالد دحام خلفNo ratings yet
- Biochem 9-10Document2 pagesBiochem 9-10Christine Arellano IIINo ratings yet
- Case StudyDocument1 pageCase Studyapi-311718939No ratings yet
- Physiotherapy (Post.) Lipid Metabolism DR - Amal BadrDocument35 pagesPhysiotherapy (Post.) Lipid Metabolism DR - Amal BadrthestaffforpediatricptNo ratings yet
- Ketone Bodies: Uses in The Heart, Brain and Muscle (But Not The Liver)Document7 pagesKetone Bodies: Uses in The Heart, Brain and Muscle (But Not The Liver)galuhNo ratings yet
- Lipid Disorders PathophysiologyDocument72 pagesLipid Disorders PathophysiologyBlodin ZylfiuNo ratings yet
- (WWW - Indowebster.com) Lipid Transport Amp StorageDocument33 pages(WWW - Indowebster.com) Lipid Transport Amp StorageRs93No ratings yet
- LipoproteinDocument12 pagesLipoproteinridho azha100% (2)
- Lipid Metabolism L3+4Document50 pagesLipid Metabolism L3+4bgj9cddvxhNo ratings yet
- Lipids Digestion and AbsorptionDocument34 pagesLipids Digestion and Absorptionglenn johnstonNo ratings yet
- The Truth About Dietary Cholesterol - Based On The Teachings Of Dr. Andrew Huberman: Separating Truth From MythsFrom EverandThe Truth About Dietary Cholesterol - Based On The Teachings Of Dr. Andrew Huberman: Separating Truth From MythsNo ratings yet
- LipidsDocument13 pagesLipidsalianaNo ratings yet
- Lipoproteins: SummaryDocument3 pagesLipoproteins: SummaryEzekiel Morena RiveraNo ratings yet
- CCHM Lec - Chole DeterDocument6 pagesCCHM Lec - Chole DeterAbigrael TangcoNo ratings yet
- Farmakoterapi DislipidemiaDocument52 pagesFarmakoterapi DislipidemialisaNo ratings yet
- DyslipidemiaDocument50 pagesDyslipidemiaTitin Tria UtamiNo ratings yet
- Metabolism of Lipids And: LipoproteinsDocument50 pagesMetabolism of Lipids And: LipoproteinsRichoco SapoetraNo ratings yet
- Metabolism of FatsDocument13 pagesMetabolism of FatsBaap ko Mat sikhaNo ratings yet
- Effect of Blocking Cholesterol AbsorptionDocument12 pagesEffect of Blocking Cholesterol AbsorptionYomal AmarathungeNo ratings yet
- CHE 311 Lecture 12 CHOLESTEROL METABOLISMDocument36 pagesCHE 311 Lecture 12 CHOLESTEROL METABOLISMisaac mwanzaNo ratings yet
- 08 - GlaucomaDocument80 pages08 - GlaucomaabcdshNo ratings yet
- ShockDocument75 pagesShockMichael UrrutiaNo ratings yet
- Fluid & Electrolyte Balance 2011Document22 pagesFluid & Electrolyte Balance 2011abcdshNo ratings yet
- Growth and Development - IntroductionDocument40 pagesGrowth and Development - IntroductionabcdshNo ratings yet
- Hipertensi jnc8Document20 pagesHipertensi jnc8abcdshNo ratings yet
- Lipid Transport & StorageDocument33 pagesLipid Transport & StorageRaja Friska YulandaNo ratings yet
- 7.ketuban Pecah Dini-PromDocument21 pages7.ketuban Pecah Dini-PromabcdshNo ratings yet
- Mineral (Cairan)Document18 pagesMineral (Cairan)WahidinSchleidenNo ratings yet
- Tentang MetabolismeDocument24 pagesTentang MetabolismeFerry JuniansyahNo ratings yet
- DiagnosisDocument9 pagesDiagnosisabcdshNo ratings yet
- PA Neoplasia DR SalmyDocument36 pagesPA Neoplasia DR SalmyJuwitaNo ratings yet
- Kuliah Konversi AaDocument11 pagesKuliah Konversi AaabcdshNo ratings yet
- Kul Katab Kerangka CDocument4 pagesKul Katab Kerangka CabcdshNo ratings yet
- Emergency THTDocument37 pagesEmergency THTIndah D. RahmahNo ratings yet
- An Overview of PathophysiologyDocument6 pagesAn Overview of PathophysiologyabcdshNo ratings yet
- Status Neurologis YARSIDocument7 pagesStatus Neurologis YARSIabcdshNo ratings yet
- Bahan2 Zat KimiaDocument3 pagesBahan2 Zat KimiaDahlia Ardhyagarini PNo ratings yet
- Diagnosis and The Clinical Spectrum of LeprosyDocument17 pagesDiagnosis and The Clinical Spectrum of LeprosyabcdshNo ratings yet
- CorticosteroidsDocument9 pagesCorticosteroidsabcdshNo ratings yet
- Bahan2 Zat KimiaDocument3 pagesBahan2 Zat KimiaDahlia Ardhyagarini PNo ratings yet
- Cholesterol Synthesis, Transport, and ExcretionDocument36 pagesCholesterol Synthesis, Transport, and ExcretionabcdshNo ratings yet
- Poorer Survival Outcomes For Male Breast Cancer Compared With Female Breast Cancer May Be Attributable To In-Stage MigrationDocument9 pagesPoorer Survival Outcomes For Male Breast Cancer Compared With Female Breast Cancer May Be Attributable To In-Stage MigrationabcdshNo ratings yet
- The Hippocratic OathDocument9 pagesThe Hippocratic OathabcdshNo ratings yet
- MiasisDocument20 pagesMiasisYuke PutriNo ratings yet
- Exogenous Glucocorticoids and Adverse Cerebral Effects in ChildrenDocument13 pagesExogenous Glucocorticoids and Adverse Cerebral Effects in ChildrenabcdshNo ratings yet
- An Overview of PathophysiologyDocument6 pagesAn Overview of PathophysiologyabcdshNo ratings yet
- DiagnosisDocument9 pagesDiagnosisabcdshNo ratings yet
- The Hippocratic OathDocument9 pagesThe Hippocratic OathabcdshNo ratings yet
- IY Facts: Interconnections - Protective Factors - PreventionDocument0 pagesIY Facts: Interconnections - Protective Factors - PreventionabcdshNo ratings yet