Professional Documents
Culture Documents
MR Dr. Andre
Uploaded by
LipatOla123Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MR Dr. Andre
Uploaded by
LipatOla123Copyright:
Available Formats
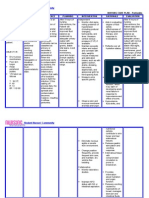
Buat pengkajian dan membahas kasus ini, pemeriksaan diagnostik, diagnosa pasien, rencana tindak
lanjut.
No. 1
A 72-year-old man presents to the clinic complaining of several weeks of worsening exertional
dyspnea. Previously, he had been able to work in his garden and mow the lawn, but now he feels
short of breath after walking 100 feet. He does not have chest pain when he walks, although in the
past he has experienced episodes of retrosternal chest pressure with strenuous exertion. Once
recently he had felt lightheaded, as if he were about to faint while climbing a flight of stairs, but the
symptom passed after he sat down. He has been having some difficulty sleeping at night and has to
prop himself up with two pillows. Occasionally, he wakes up at night feeling quite short of breath,
which is relieved within minutes by sitting upright and dangling his legs over the bed. His feet have
become swollen, especially by the end of the day. He denies any significant medical history, takes no
medications, and prides himself on the fact that he has not seen a doctor in years. He does not
smoke or drink alcohol. On physical examination, he is afebrile, with a heart rate of 86 bpm, blood
pressure of 115/92 mm Hg, and respiratory rate of 16 breaths per minute. Examination of the head
and neck reveals pink mucosa without pallor, a normal thyroid gland, and distended neck veins.
Bibasilar inspiratory crackles are heard on examination. On cardiac examination, his heart rhythm is
regular with a normal S 1 and a second heart sound that splits during expiration, an S 4 at the apex,
a nondisplaced apical impulse, and a late-peaking systolic murmur at the right-upper sternal border
that radiates to his carotids. The carotid upstrokes have diminished amplitude.
What is the most likely diagnosis?
What test would confirm the diagnosis?
A 37-year-old executive returns to your clinic for follow-up of recurrent upper
abdominal pain. He initially presented 3 weeks ago, complaining of an increase
in frequency and severity of burning epigastric pain, which he has experienced
occasionally for more than 2 years. Now the pain occurs three or four times per
week, usually when he has an empty stomach, and it often awakens him at
night. The pain usually is relieved within minutes by food or over-the-counter
antacids, but then recurs within 2 to 3 hours. He admitted that stress at work
had recently increased and that because of long working hours, he was
drinking more caffeine and eating a lot of take-out foods. His medical history
and review of systems were otherwise unremarkable, and, other than the
antacids, he takes no medications. His physical examination was normal,
including stool guaiac that was negative for occult blood. You advised a change
in diet and started him on a proton-pump inhibitor. His symptoms resolved
completely with the diet changes and daily use of the medication. Results of
laboratory tests performed at his first visit show no anemia, but his serum
Helicobacter pylori antibody test was positive.
What is your diagnosis?
What is your next step?
You might also like
- Urinary EliminationDocument80 pagesUrinary EliminationMentari WardhaniNo ratings yet
- Case Study - Dengue Fever V - S UtiDocument12 pagesCase Study - Dengue Fever V - S UtiHarlene Joyce ReyNo ratings yet
- A Case Presentation On CholedocholithiasisDocument11 pagesA Case Presentation On CholedocholithiasisPaul Vincent EspereNo ratings yet
- Managing Upper GI Bleeding in a Male PatientDocument19 pagesManaging Upper GI Bleeding in a Male PatientMary Ann Garcia100% (1)
- ABDOMINAL ObjectiveDocument9 pagesABDOMINAL ObjectiveXing-Jin RomeroNo ratings yet
- CHH Drug Study Week 3Document21 pagesCHH Drug Study Week 3maryxtine24No ratings yet
- Abruption Placenta Definition Causes Symptoms ManagementDocument30 pagesAbruption Placenta Definition Causes Symptoms ManagementArchana MaharjanNo ratings yet
- Normal Spontaneous DeliveryDocument64 pagesNormal Spontaneous DeliveryMichellin Andres MarianoNo ratings yet
- Stages of Labor: Latent, Active, Transition & PlacentalDocument18 pagesStages of Labor: Latent, Active, Transition & Placentallushxene84No ratings yet
- Reflective Journal 1Document4 pagesReflective Journal 1api-365605511No ratings yet
- Case Scenario Dengue FeverDocument2 pagesCase Scenario Dengue FeverJaslir MendozaNo ratings yet
- Discharge PlanningDocument2 pagesDischarge PlanningAthena Irish LastimosaNo ratings yet
- Nursing Management Pancreatic CancerDocument2 pagesNursing Management Pancreatic CancerKit NameKo100% (2)
- Live Preterm Baby Delivered NSDDocument13 pagesLive Preterm Baby Delivered NSDKristine Anne SorianoNo ratings yet
- Hydrocephalus Nursing CareDocument27 pagesHydrocephalus Nursing CareyounggirldavidNo ratings yet
- Acute TonsillopharyngitisDocument39 pagesAcute TonsillopharyngitisCin AtianzarNo ratings yet
- Report - For MaamDocument7 pagesReport - For MaamSherchen Antonio-CortesNo ratings yet
- Maternal Final Exam ReviewerDocument5 pagesMaternal Final Exam Reviewercassy SadieNo ratings yet
- Assessment of Digestive and Gastrointestinal FunctionDocument5 pagesAssessment of Digestive and Gastrointestinal FunctionBoom PastranaNo ratings yet
- Optimizing Perioperative CareDocument8 pagesOptimizing Perioperative CareJan Crizza Dale R. FrancoNo ratings yet
- PeritonitisDocument6 pagesPeritonitisDiane ArgoteNo ratings yet
- Hypertension: Colegio de San Juan de LetranDocument13 pagesHypertension: Colegio de San Juan de LetranJenna AbuanNo ratings yet
- Client Care Study on CholedocholithiasisDocument29 pagesClient Care Study on CholedocholithiasisNehdu AkahNo ratings yet
- AdpieDocument11 pagesAdpieChucky Vergara0% (1)
- Assessment of The Elderly 3Document32 pagesAssessment of The Elderly 3Tanwir Houssayn100% (1)
- Case Presentation Hypokalemic ManDocument61 pagesCase Presentation Hypokalemic ManHussain AzharNo ratings yet
- Complication During PregnancyDocument43 pagesComplication During PregnancyRizza Domalaon BalangitanNo ratings yet
- Congenital Hypothyroidism Follow Up of A Case For 13 Years PDFDocument14 pagesCongenital Hypothyroidism Follow Up of A Case For 13 Years PDFMeutia sariNo ratings yet
- Managing Diabetes and RisksDocument8 pagesManaging Diabetes and RisksChristopher LontocNo ratings yet
- 5 Nursing Management TBDocument2 pages5 Nursing Management TBًNo ratings yet
- Lab 5 RebolosDocument5 pagesLab 5 RebolosAisha MarieNo ratings yet
- History of Past IllnessDocument4 pagesHistory of Past IllnessKrisianne Mae Lorenzo FranciscoNo ratings yet
- Cholecystitis Litiasis EctomyDocument23 pagesCholecystitis Litiasis EctomyTimothy WilliamsNo ratings yet
- A. Indicate Whether The Progress of Labor in The Following Partographs Are Normal or Abnormal. (1point Each)Document5 pagesA. Indicate Whether The Progress of Labor in The Following Partographs Are Normal or Abnormal. (1point Each)Charisse Arriane BelasotoNo ratings yet
- Post-Partum Hemorrhage Pathophysiology PaperDocument5 pagesPost-Partum Hemorrhage Pathophysiology Paperapi-399619969No ratings yet
- Fluid Volume Deficit and Excess: Types, Causes, Signs and Nursing ManagementDocument32 pagesFluid Volume Deficit and Excess: Types, Causes, Signs and Nursing ManagementAcohCChaoNo ratings yet
- Bulacan State University College of Nursing: Bulsu-Op-Con-23F15 Revision: 0Document6 pagesBulacan State University College of Nursing: Bulsu-Op-Con-23F15 Revision: 0Richmon SantosNo ratings yet
- UTI (Urinary Tract Infection)Document9 pagesUTI (Urinary Tract Infection)Carson BirthNo ratings yet
- Uterine Myoma Case Study Group A FinalDocument88 pagesUterine Myoma Case Study Group A Finallowell cerezoNo ratings yet
- Patient Response: Self IntroductionDocument3 pagesPatient Response: Self IntroductionMercy Anne EcatNo ratings yet
- HA-RLE-WS # 8 Assessing CultureDocument5 pagesHA-RLE-WS # 8 Assessing CultureJULIE ANNE CORTEZNo ratings yet
- Final - Mrs. X - Case Study (Group 3-RR21)Document45 pagesFinal - Mrs. X - Case Study (Group 3-RR21)Gabriel Andrei C. RelayoNo ratings yet
- Stages of Labor and Nursing Care During ChildbirthDocument3 pagesStages of Labor and Nursing Care During ChildbirthCleo Pabilic100% (1)
- Laws Affecting Nursing PracticeDocument52 pagesLaws Affecting Nursing Practiceapi-3731845100% (3)
- Abortionsource 100605123737 Phpapp01Document38 pagesAbortionsource 100605123737 Phpapp01Erina Erichan OtoNo ratings yet
- Case Study #117: Intrapartal CareDocument21 pagesCase Study #117: Intrapartal CareDudong SasakiNo ratings yet
- Case Study-Infant With Fluid Imbalance08-10-KEYDocument3 pagesCase Study-Infant With Fluid Imbalance08-10-KEYreecoleNo ratings yet
- Lower Limb Trauma - 5Document12 pagesLower Limb Trauma - 5Renee RoSeNo ratings yet
- N. Bacalso Ave., Cebu City Philippines: Page 1 of 32Document32 pagesN. Bacalso Ave., Cebu City Philippines: Page 1 of 32Joule PeirreNo ratings yet
- Modified CaseDocument22 pagesModified CaseAli HawamdeNo ratings yet
- Ba GastrectomyDocument10 pagesBa GastrectomyHope3750% (2)
- NUR C307 - M1 - Concepts, Principles and Theories in The Care of Older AdultsDocument38 pagesNUR C307 - M1 - Concepts, Principles and Theories in The Care of Older Adultsnoo.wannNo ratings yet
- NCM 114 RevsDocument8 pagesNCM 114 RevsKryza B. CASTILLONo ratings yet
- CholecystitisDocument34 pagesCholecystitisapi-26762768100% (1)
- Module 12 ContempoDocument5 pagesModule 12 ContempoJericho CunananNo ratings yet
- St. Paul University Nursing Care PlansDocument6 pagesSt. Paul University Nursing Care PlansRoxanne MariÑas Delvo0% (1)
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Journal Reading - Myringitis - Elisabeth PattyDocument14 pagesJournal Reading - Myringitis - Elisabeth PattyLipatOla123No ratings yet
- Daftr PustakaDocument1 pageDaftr PustakaLipatOla123No ratings yet
- Usia Kehamilan 32 Minggu, Perdarahan, Uterus Tegang, His Positif. DX ? Plasenta Abruption/ Solusio 2. Factor Resikonya? Kekurangan Asam Folat 3. 4Document1 pageUsia Kehamilan 32 Minggu, Perdarahan, Uterus Tegang, His Positif. DX ? Plasenta Abruption/ Solusio 2. Factor Resikonya? Kekurangan Asam Folat 3. 4LipatOla123No ratings yet
- Medical report template for patient assessmentDocument4 pagesMedical report template for patient assessmentLipatOla123No ratings yet
- Leaflet PHBSDocument1 pageLeaflet PHBSLipatOla123No ratings yet
- TGL Subjetive Objective Pem. Penunjang Assessment PlanningDocument4 pagesTGL Subjetive Objective Pem. Penunjang Assessment PlanningLipatOla123No ratings yet
- Premature Rupture of MembranesDocument4 pagesPremature Rupture of MembranesLipatOla123No ratings yet
- P ('t':'3', 'I':'668096276') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document31 pagesP ('t':'3', 'I':'668096276') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)LipatOla123No ratings yet
- Bab 121 HematuriaDocument2 pagesBab 121 HematuriaKabhithra ThiayagarajanNo ratings yet
- Bab 55 Asma BronkialDocument6 pagesBab 55 Asma BronkialAudrey BudionoNo ratings yet
- Early Childhood EducationDocument3 pagesEarly Childhood EducationLipatOla123No ratings yet
- Ds Gigavue FM Fabric ManagerDocument9 pagesDs Gigavue FM Fabric ManagerMARCELOTRIVELATTONo ratings yet
- Grade6 Integers Multiple Additions Subtractions PDFDocument9 pagesGrade6 Integers Multiple Additions Subtractions PDFEduGainNo ratings yet
- E No Ad Release NotesDocument6 pagesE No Ad Release NotesKostyantinBondarenkoNo ratings yet
- Chapter 10Document28 pagesChapter 10ahmedNo ratings yet
- Andhra Pradesh Land Reforms (Ceiling On Agricultural Holdings) (Amendment) Act, 2009Document3 pagesAndhra Pradesh Land Reforms (Ceiling On Agricultural Holdings) (Amendment) Act, 2009Latest Laws TeamNo ratings yet
- Tough Turkish TBM Moves Through Fractured and Faulted Rock: Issue 1 + 2014Document8 pagesTough Turkish TBM Moves Through Fractured and Faulted Rock: Issue 1 + 2014sCoRPion_trNo ratings yet
- 3 IT18 Information Assurance and Security 2 Prelim ExamDocument2 pages3 IT18 Information Assurance and Security 2 Prelim Examsarah miinggNo ratings yet
- Secure Password-Driven Fingerprint Biometrics AuthenticationDocument5 pagesSecure Password-Driven Fingerprint Biometrics AuthenticationDorothy ManriqueNo ratings yet
- Cement Lined Piping SpecificationDocument167 pagesCement Lined Piping SpecificationvenkateshwaranNo ratings yet
- 2 - Brief Report On Logistics Workforce 2019Document39 pages2 - Brief Report On Logistics Workforce 2019mohammadNo ratings yet
- 2021-2022 Reopening Plan 2.0Document22 pages2021-2022 Reopening Plan 2.0Dan LehrNo ratings yet
- (Lecture 10 & 11) - Gearing & Capital StructureDocument18 pages(Lecture 10 & 11) - Gearing & Capital StructureAjay Kumar TakiarNo ratings yet
- 2.2 Access CT Networking Rev20150728Document5 pages2.2 Access CT Networking Rev20150728F CNo ratings yet
- Dyna PDFDocument12 pagesDyna PDFVernadette VenturaNo ratings yet
- PHB 55n03lta Logic Level FetDocument15 pagesPHB 55n03lta Logic Level FetyusufwpNo ratings yet
- Abm Trial Balance ActivityDocument3 pagesAbm Trial Balance ActivityRoxanne RoldanNo ratings yet
- Project ProposalDocument6 pagesProject Proposalapi-386094460No ratings yet
- Face Detection PythonDocument5 pagesFace Detection PythonAADISH JAINNo ratings yet
- Banking DictionaryDocument499 pagesBanking DictionaryVanessa Jenkins100% (4)
- 365) - The Income Tax Rate Is 40%. Additional Expenses Are Estimated As FollowsDocument3 pages365) - The Income Tax Rate Is 40%. Additional Expenses Are Estimated As FollowsMihir HareetNo ratings yet
- Speech ExamplesDocument6 pagesSpeech Examplesjayz_mateo9762100% (1)
- Computer Security: Principles and PracticeDocument21 pagesComputer Security: Principles and Practicekrishnakumar velapanNo ratings yet
- Lecture No 5Document41 pagesLecture No 5sami ul haqNo ratings yet
- Portarlington Parish NewsletterDocument2 pagesPortarlington Parish NewsletterJohn HayesNo ratings yet
- FFT FundamentalsDocument27 pagesFFT FundamentalsVivien VilladelreyNo ratings yet
- FSK Demodulator With PLLDocument5 pagesFSK Demodulator With PLLHema100% (1)
- DigitalForensics 05 NOV2010Document84 pagesDigitalForensics 05 NOV2010hhhzineNo ratings yet
- RTC Ruling on Land Ownership Upheld by CADocument12 pagesRTC Ruling on Land Ownership Upheld by CAGladys BantilanNo ratings yet
- Development Approach PlanDocument15 pagesDevelopment Approach PlanGaurav UpretiNo ratings yet
- Gram-Charlier para Aproximar DensidadesDocument10 pagesGram-Charlier para Aproximar DensidadesAlejandro LopezNo ratings yet