Professional Documents
Culture Documents
Materi Penanganan Asthma
Uploaded by
Yuliarni HasanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Materi Penanganan Asthma
Uploaded by
Yuliarni HasanCopyright:
Available Formats
Penatalaksanaan Asma
di Pelayanan Primer
Dr. Melfia Navratilova, SpP, MKes
© Global Initiative for Asthma
G lobal
INitiative for
A sthma
© Global Initiative for Asthma
Definition and diagnosis of
asthma
GINA Global Strategy for Asthma
Management and Prevention 2016
This slide set is restricted for academic and educational purposes
only. Use of the slide set, or of individual slides, for commercial or
promotional purposes requires approval from GINA.
© Global Initiative for Asthma
What is known about asthma?
Asthma is a common and potentially serious chronic disease
that can be controlled but not cured
Asthma causes symptoms such as wheezing, shortness of
breath, chest tightness and cough that vary over time in their
occurrence, frequency and intensity
Symptoms are associated with variable expiratory airflow,
i.e. difficulty breathing air out of the lungs due to
Bronchoconstriction (airway narrowing)
Airway wall thickening
Increased mucus
Symptoms may be triggered or worsened by factors such as
viral infections, allergens, tobacco smoke, exercise and stress
GINA 2016 © Global Initiative for Asthma
What is known about asthma?
Asthma can be effectively treated
When asthma is well-controlled, patients can
Avoid troublesome symptoms during the day and night
Need little or no reliever medication
Have productive, physically active lives
Have normal or near-normal lung function
Avoid serious asthma flare-ups (also called
exacerbations, or severe attacks)
GINA 2016 © Global Initiative for Asthma
Definition of asthma
Asthma is a heterogeneous disease, usually characterized
by chronic airway inflammation.
It is defined by the history of respiratory symptoms such as
wheeze, shortness of breath, chest tightness and cough
that vary over time and in intensity, together with variable
expiratory airflow limitation.
GINA 2016 © Global Initiative for Asthma
Diagnosis of asthma
The diagnosis of asthma should be based on:
A history of characteristic symptom patterns
Evidence of variable airflow limitation, from bronchodilator
reversibility testing or other tests
Document evidence for the diagnosis in the patient’s notes,
preferably before starting controller treatment
It is often more difficult to confirm the diagnosis after treatment has
been started
Asthma is usually characterized by airway inflammation and
airway hyperresponsiveness, but these are not necessary or
sufficient to make the diagnosis of asthma.
GINA 2016 © Global Initiative for Asthma
Patient with
respiratory symptoms
Are the symptoms typical of asthma?
YES
Detailed history/examination
for asthma
History/examination supports
asthma diagnosis?
YES
Perform spirometry/PEF
with reversibility test
Results support asthma diagnosis?
YES
Treat for ASTHMA
GINA 2016, Box 1-1 (1/4) © Global Initiative for Asthma
Patient with
respiratory symptoms
Are the symptoms typical of asthma?
NO
YES
Detailed history/examination
for asthma
History/examination supports
asthma diagnosis?
Further history and tests for
NO alternative diagnoses
YES Alternative diagnosis confirmed?
Perform spirometry/PEF
with reversibility test
Results support asthma diagnosis?
YES YES
Treat for ASTHMA Treat for alternative diagnosis
GINA 2016, Box 1-1 (2/4) © Global Initiative for Asthma
Patient with
respiratory symptoms
Are the symptoms typical of asthma?
NO
YES
Detailed history/examination
for asthma
History/examination supports
asthma diagnosis?
Further history and tests for
NO alternative diagnoses
YES Alternative diagnosis confirmed?
Perform spirometry/PEF
with reversibility test
Results support asthma diagnosis?
Repeat on another
NO
occasion or arrange
NO
YES other tests
Confirms asthma diagnosis?
YES NO YES
Consider trial of treatment for
most likely diagnosis, or refer
for further investigations
Treat for ASTHMA Treat for alternative diagnosis
GINA 2016, Box 1-1 (3/4) © Global Initiative for Asthma
Patient with
respiratory symptoms
Are the symptoms typical of asthma?
NO
YES
Detailed history/examination
for asthma
History/examination supports
asthma diagnosis?
Further history and tests for
NO alternative diagnoses
Clinical urgency, and
YES Alternative diagnosis confirmed?
other diagnoses unlikely
Perform spirometry/PEF
with reversibility test
Results support asthma diagnosis?
Repeat on another
NO
occasion or arrange
NO
YES other tests
Confirms asthma diagnosis?
Empiric treatment with YES NO YES
ICS and prn SABA
Review response
Consider trial of treatment for
Diagnostic testing most likely diagnosis, or refer
within 1-3 months for further investigations
Treat for ASTHMA Treat for alternative diagnosis
GINA 2016, Box 1-1 (4/4) © Global Initiative for Asthma
Diagnosis of asthma – symptoms
Increased probability that symptoms are due to asthma if:
More than one type of symptom (wheeze, shortness of breath, cough,
chest tightness)
Symptoms often worse at night or in the early morning
Symptoms vary over time and in intensity
Symptoms are triggered by viral infections, exercise, allergen
exposure, changes in weather, laughter, irritants such as car exhaust
fumes, smoke, or strong smells
Decreased probability that symptoms are due to asthma if:
Isolated cough with no other respiratory symptoms
Chronic production of sputum
Shortness of breath associated with dizziness, light-headedness or
peripheral tingling
Chest pain
Exercise-induced dyspnea with noisy inspiration (stridor)
GINA 2016 © Global Initiative for Asthma
Diagnosis of asthma – variable airflow limitation
Confirm presence of airflow limitation
Document that FEV1/FVC is reduced (at least once, when FEV1 is low)
FEV1/ FVC ratio is normally >0.75 – 0.80 in healthy adults, and
>0.90 in children
Confirm variation in lung function is greater than in healthy individuals
The greater the variation, or the more times variation is seen, the
greater probability that the diagnosis is asthma
Excessive bronchodilator reversibility (adults: increase in FEV1 >12%
and >200mL; children: increase >12% predicted)
Excessive diurnal variability from 1-2 weeks’ twice-daily PEF
monitoring (daily amplitude x 100/daily mean, averaged)
Significant increase in FEV1 or PEF after 4 weeks of controller
treatment
If initial testing is negative:
• Repeat when patient is symptomatic, or after withholding bronchodilators
• Refer for additional tests (especially children ≤5 years, or the elderly)
GINA 2016, Box 1-2 © Global Initiative for Asthma
Diagnosis of asthma – physical examination
Physical examination in people with asthma
Often normal
The most frequent finding is wheezing on auscultation, especially
on forced expiration
Wheezing is also found in other conditions, for example:
Respiratory infections
COPD
Upper airway dysfunction
Endobronchial obstruction
Inhaled foreign body
Wheezing may be absent during severe asthma exacerbations
(‘silent chest’)
GINA 2016 © Global Initiative for Asthma
Assessment of risk factors for poor asthma
outcomes
Risk factors for exacerbations include:
• Ever intubated for asthma
• Uncontrolled asthma symptoms
• Having ≥1 exacerbation in last 12 months
• Low FEV1 (measure lung function at start of treatment, at 3-6 months
to assess personal best, and periodically thereafter)
• Incorrect inhaler technique and/or poor adherence
• Smoking
• Obesity, pregnancy, blood eosinophilia
GINA 2016, Box 2-2B (2/4) © Global Initiative for Asthma
Assessment of risk factors for poor asthma
outcomes
Risk factors for exacerbations include:
• Ever intubated for asthma
• Uncontrolled asthma symptoms
• Having ≥1 exacerbation in last 12 months
• Low FEV1 (measure lung function at start of treatment, at 3-6 months
to assess personal best, and periodically thereafter)
• Incorrect inhaler technique and/or poor adherence
• Smoking
• Obesity, pregnancy, blood eosinophilia
Risk factors for fixed airflow limitation include:
• No ICS treatment, smoking, occupational exposure, mucus
hypersecretion, blood eosinophilia
GINA 2016, Box 2-2B (3/4) © Global Initiative for Asthma
Assessment of risk factors for poor asthma
outcomes
Risk factors for exacerbations include:
• Ever intubated for asthma
• Uncontrolled asthma symptoms
• Having ≥1 exacerbation in last 12 months
• Low FEV1 (measure lung function at start of treatment, at 3-6 months
to assess personal best, and periodically thereafter)
• Incorrect inhaler technique and/or poor adherence
• Smoking
• Obesity, pregnancy, blood eosinophilia
Risk factors for fixed airflow limitation include:
• No ICS treatment, smoking, occupational exposure, mucus
hypersecretion, blood eosinophilia
Risk factors for medication side-effects include:
• Frequent oral steroids, high dose/potent ICS, P450 inhibitors
GINA 2016, Box 2-2B (4/4) © Global Initiative for Asthma
Treating asthma to control
symptoms and minimize risk
GINA Global Strategy for Asthma
Management and Prevention 2016
This slide set is restricted for academic and educational purposes
only. Use of the slide set, or of individual slides, for commercial or
promotional purposes requires approval from GINA.
© Global Initiative for Asthma
Goals of asthma management
The long-term goals of asthma management are
1. Symptom control: to achieve good control of symptoms and
maintain normal activity levels
2. Risk reduction: to minimize future risk of exacerbations, fixed
airflow limitation and medication side-effects
Achieving these goals requires a partnership between patient
and their health care providers
Ask the patient about their own goals regarding their asthma
Good communication strategies are essential
Consider the health care system, medication availability, cultural
and personal preferences and health literacy
GINA 2016 © Global Initiative for Asthma
Indications for considering referral, where
available
Difficulty confirming the diagnosis of asthma
Symptoms suggesting chronic infection, cardiac disease etc
Diagnosis unclear even after a trial of treatment
Features of both asthma and COPD, if in doubt about treatment
Suspected occupational asthma
Refer for confirmatory testing, identification of sensitizing agent,
advice about eliminating exposure, pharmacological treatment
Persistent uncontrolled asthma or frequent exacerbations
Uncontrolled symptoms or ongoing exacerbations or low FEV1
despite correct inhaler technique and good adherence with Step 4
Frequent asthma-related health care visits
Risk factors for asthma-related death
Near-fatal exacerbation in past
Anaphylaxis or confirmed food allergy with asthma
© Global Initiative for Asthma
Indications for considering referral, where
available
Significant side-effects (or risk of side-effects)
Significant systemic side-effects
Need for oral corticosteroids long-term or as frequent courses
Symptoms suggesting complications or sub-types of asthma
Nasal polyposis and reactions to NSAIDS (may be aspirin
exacerbated respiratory disease)
Chronic sputum production, fleeting shadows on CXR (may be
allergic bronchopulmonary aspergillosis)
Additional reasons for referral in children 6-11 years
Doubts about diagnosis, e.g. symptoms since birth
Symptoms or exacerbations remain uncontrolled
Suspected side-effects of treatment, e.g. growth delay
Asthma with confirmed food allergy
GINA 2016, Box 3-10 (2/2) © Global Initiative for Asthma
Asthma flare-ups
(exacerbations)
GINA Global Strategy for Asthma
Management and Prevention 2016
This slide set is restricted for academic and educational purposes
only. Use of the slide set, or of individual slides, for commercial or
promotional purposes requires approval from GINA.
© Global Initiative for Asthma
Identify patients at risk of asthma-related death
Patients at increased risk of asthma-related death should be
identified
Any history of near-fatal asthma requiring intubation and ventilation
Hospitalization or emergency care for asthma in last 12 months
Not currently using ICS, or poor adherence with ICS
Currently using or recently stopped using OCS
• (indicating the severity of recent events)
Over-use of SABAs, especially if more than 1 canister/month
Lack of a written asthma action plan
History of psychiatric disease or psychosocial problems
Confirmed food allergy in a patient with asthma
Flag these patients for more frequent review
GINA 2016, Box 4-1 © Global Initiative for Asthma
Managing exacerbations in primary care
PRIMARY CARE Patient presents with acute or sub-acute asthma exacerbation
Is it asthma?
ASSESS the PATIENT Risk factors for asthma-related death?
Severity of exacerbation?
MILD or MODERATE SEVERE
Talks in phrases, prefers
LIFE-THREATENING
Talks in words, sits hunched
sitting to lying, not agitated forwards, agitated Drowsy, confused
Respiratory rate increased Respiratory rate >30/min or silent chest
Accessory muscles not used Accessory muscles in use
Pulse rate 100–120 bpm Pulse rate >120 bpm
O2 saturation (on air) 90–95% O2 saturation (on air) <90%
PEF >50% predicted or best PEF ≤50% predicted or best URGENT
START TREATMENT
SABA 4–10 puffs by pMDI + spacer, TRANSFER TO ACUTE
repeat every 20 minutes for 1 hour CARE FACILITY
WORSENING
Prednisolone: adults 1 mg/kg, max.
50 mg, children 1–2 mg/kg, max. 40 mg While waiting: give inhaled
SABA and ipratropium bromide,
Controlled oxygen (if available): target O2, systemic corticosteroid
saturation 93–95% (children: 94-98%)
CONTINUE TREATMENT with SABA as needed
WORSENING
ASSESS RESPONSE AT 1 HOUR (or earlier)
IMPROVING
ASSESS FOR DISCHARGE ARRANGE at DISCHARGE
Symptoms improved, not needing SABA Reliever: continue as needed
PEF improving, and >60-80% of personal Controller: start, or step up. Check inhaler
best or predicted technique, adherence
Oxygen saturation >94% room air Prednisolone: continue, usually for 5–7 days
(3-5 days for children)
Resources at home adequate
Follow up: within 2–7 days
FOLLOW UP
Reliever: reduce to as-needed
Controller: continue higher dose for short term (1–2 weeks) or long term (3 months), depending
on background to exacerbation
Risk factors: check and correct modifiable risk factors that may have contributed to exacerbation,
including inhaler technique and adherence
Action plan: Is it understood? Was it used appropriately? Does it need modification?
GINA 2016, Box 4-3 (1/7) © Global Initiative for Asthma
PRIMARY CARE Patient presents with acute or sub-acute asthma exacerbation
Is it asthma?
ASSESS the PATIENT Risk factors for asthma-related death?
Severity of exacerbation?
LIFE-THREATENING
Drowsy, confused
or silent chest
URGENT
TRANSFER TO ACUTE
CARE FACILITY
While waiting: give inhaled SABA
and ipratropium bromide, O2,
systemic corticosteroid
GINA 2016, Box 4-3 (2/7) © Global Initiative for Asthma
PRIMARY CARE Patient presents with acute or sub-acute asthma exacerbation
Is it asthma?
ASSESS the PATIENT Risk factors for asthma-related death?
Severity of exacerbation?
MILD or MODERATE SEVERE
Talks in phrases, prefers Talks in words, sits hunched LIFE-THREATENING
sitting to lying, not agitated forwards, agitated Drowsy, confused
Respiratory rate increased Respiratory rate >30/min or silent chest
Accessory muscles not used Accessory muscles in use
Pulse rate 100–120 bpm Pulse rate >120 bpm
O2 saturation (on air) 90–95% O2 saturation (on air) <90%
PEF >50% predicted or best PEF ≤50% predicted or best URGENT
TRANSFER TO ACUTE
CARE FACILITY
While waiting: give inhaled SABA
and ipratropium bromide, O2,
systemic corticosteroid
GINA 2016, Box 4-3 (3/7) © Global Initiative for Asthma
PRIMARY CARE Patient presents with acute or sub-acute asthma exacerbation
Is it asthma?
ASSESS the PATIENT Risk factors for asthma-related death?
Severity of exacerbation?
MILD or MODERATE SEVERE
Talks in phrases, prefers Talks in words, sits hunched LIFE-THREATENING
sitting to lying, not agitated forwards, agitated Drowsy, confused
Respiratory rate increased Respiratory rate >30/min or silent chest
Accessory muscles not used Accessory muscles in use
Pulse rate 100–120 bpm Pulse rate >120 bpm
O2 saturation (on air) 90–95% O2 saturation (on air) <90%
PEF >50% predicted or best PEF ≤50% predicted or best URGENT
START TREATMENT
TRANSFER TO ACUTE
SABA 4–10 puffs by pMDI + spacer,
repeat every 20 minutes for 1 hour CARE FACILITY
WORSENING While waiting: give inhaled SABA
Prednisolone: adults 1 mg/kg, max.
50 mg, children 1–2 mg/kg, max. 40 mg and ipratropium bromide, O2,
Controlled oxygen (if available): target systemic corticosteroid
saturation 93–95% (children: 94-98%)
GINA 2016, Box 4-3 (4/7) © Global Initiative for Asthma
START TREATMENT
SABA 4–10 puffs by pMDI + spacer, TRANSFER TO ACUTE
repeat every 20 minutes for 1 hour CARE FACILITY
Prednisolone: adults 1 mg/kg, max. WORSENING
While waiting: give inhaled SABA
50 mg, children 1–2 mg/kg, max. 40 mg and ipratropium bromide, O2,
Controlled oxygen (if available): target systemic corticosteroid
saturation 93–95% (children: 94-98%)
CONTINUE TREATMENT with SABA as needed
WORSENING
ASSESS RESPONSE AT 1 HOUR (or earlier)
IMPROVING
ASSESS FOR DISCHARGE
Symptoms improved, not needing SABA
PEF improving, and >60-80% of personal
best or predicted
Oxygen saturation >94% room air
Resources at home adequate
GINA 2016, Box 4-3 (5/7) © Global Initiative for Asthma
START TREATMENT
SABA 4–10 puffs by pMDI + spacer, TRANSFER TO ACUTE
repeat every 20 minutes for 1 hour CARE FACILITY
Prednisolone: adults 1 mg/kg, max. WORSENING
While waiting: give inhaled SABA
50 mg, children 1–2 mg/kg, max. 40 mg and ipratropium bromide, O2,
Controlled oxygen (if available): target systemic corticosteroid
saturation 93–95% (children: 94-98%)
CONTINUE TREATMENT with SABA as needed
WORSENING
ASSESS RESPONSE AT 1 HOUR (or earlier)
IMPROVING
ASSESS FOR DISCHARGE ARRANGE at DISCHARGE
Symptoms improved, not needing SABA Reliever: continue as needed
PEF improving, and >60-80% of personal Controller: start, or step up. Check inhaler technique,
best or predicted adherence
Oxygen saturation >94% room air Prednisolone: continue, usually for 5–7 days
(3-5 days for children)
Resources at home adequate
Follow up: within 2–7 days
GINA 2016, Box 4-3 (6/7) © Global Initiative for Asthma
START TREATMENT
SABA 4–10 puffs by pMDI + spacer, TRANSFER TO ACUTE
repeat every 20 minutes for 1 hour CARE FACILITY
Prednisolone: adults 1 mg/kg, max. WORSENING
While waiting: give inhaled SABA
50 mg, children 1–2 mg/kg, max. 40 mg and ipratropium bromide, O2,
Controlled oxygen (if available): target systemic corticosteroid
saturation 93–95% (children: 94-98%)
CONTINUE TREATMENT with SABA as needed
WORSENING
ASSESS RESPONSE AT 1 HOUR (or earlier)
IMPROVING
ASSESS FOR DISCHARGE ARRANGE at DISCHARGE
Symptoms improved, not needing SABA Reliever: continue as needed
PEF improving, and >60-80% of personal Controller: start, or step up. Check inhaler technique,
best or predicted adherence
Oxygen saturation >94% room air Prednisolone: continue, usually for 5–7 days
(3-5 days for children)
Resources at home adequate
Follow up: within 2–7 days
FOLLOW UP
Reliever: reduce to as-needed
Controller: continue higher dose for short term (1–2 weeks) or long term (3 months), depending
on background to exacerbation
Risk factors: check and correct modifiable risk factors that may have contributed to exacerbation,
including inhaler technique and adherence
Action plan: Is it understood? Was it used appropriately? Does it need modification?
GINA 2016, Box 4-3 (7/7) © Global Initiative for Asthma
Managing exacerbations in acute care settings
INITIAL ASSESSMENT Are any of the following present?
A: airway B: breathing C: circulation Drowsiness, Confusion, Silent chest
NO
YES
Further TRIAGE BY CLINICAL STATUS Consult ICU, start SABA and O2,
according to worst feature and prepare patient for intubation
MILD or MODERATE SEVERE
Talks in phrases Talks in words
Prefers sitting to lying Sits hunched forwards
Not agitated Agitated
Respiratory rate increased Respiratory rate >30/min
Accessory muscles not used Accessory muscles being used
Pulse rate 100–120 bpm Pulse rate >120 bpm
O2 saturation (on air) 90–95% O2 saturation (on air) < 90%
PEF >50% predicted or best PEF ≤50% predicted or best
Short-acting beta2-agonists Short-acting beta2-agonists
Consider ipratropium bromide Ipratropium bromide
Controlled O2 to maintain Controlled O2 to maintain
saturation 93–95% (children 94-98%) saturation 93–95% (children 94-98%)
Oral corticosteroids Oral or IV corticosteroids
Consider IV magnesium
Consider high dose ICS
If continuing deterioration, treat as
severe and re-aassess for ICU
ASSESS CLINICAL PROGRESS FREQUENTLY
MEASURE LUNG FUNCTION
in all patients one hour after initial treatment
FEV1 or PEF 60-80% of predicted or FEV1 or PEF <60% of predicted or
personal best and symptoms improved personal best,or lack of clinical response
SEVERE
MODERATE
Continue treatment as above
Consider for discharge planning and reassess frequently
GINA 2016, Box 4-4 (1/4) © Global Initiative for Asthma
INITIAL ASSESSMENT Are any of the following present?
A: airway B: breathing C: circulation Drowsiness, Confusion, Silent chest
NO
YES
Further TRIAGE BY CLINICAL STATUS Consult ICU, start SABA and O2,
according to worst feature and prepare patient for intubation
MILD or MODERATE SEVERE
Talks in phrases Talks in words
Prefers sitting to lying Sits hunched forwards
Not agitated Agitated
Respiratory rate increased Respiratory rate >30/min
Accessory muscles not used Accessory muscles being used
Pulse rate 100–120 bpm Pulse rate >120 bpm
O2 saturation (on air) 90–95% O2 saturation (on air) < 90%
PEF >50% predicted or best PEF ≤50% predicted or best
GINA 2016, Box 4-4 (2/4) © Global Initiative for Asthma
MILD or MODERATE SEVERE
Talks in phrases Talks in words
Prefers sitting to lying Sits hunched forwards
Not agitated Agitated
Respiratory rate increased Respiratory rate >30/min
Accessory muscles not used Accessory muscles being used
Pulse rate 100–120 bpm Pulse rate >120 bpm
O2 saturation (on air) 90–95% O2 saturation (on air) < 90%
PEF >50% predicted or best PEF ≤50% predicted or best
Short-acting beta2-agonists Short-acting beta2-agonists
Consider ipratropium bromide Ipratropium bromide
Controlled O2 to maintain Controlled O2 to maintain
saturation 93–95% (children 94-98%) saturation 93–95% (children 94-98%)
Oral corticosteroids Oral or IV corticosteroids
Consider IV magnesium
Consider high dose ICS
GINA 2016, Box 4-4 (3/4) © Global Initiative for Asthma
Short-acting beta2-agonists Short-acting beta2-agonists
Consider ipratropium bromide Ipratropium bromide
Controlled O2 to maintain Controlled O2 to maintain
saturation 93–95% (children 94-98%) saturation 93–95% (children 94-98%)
Oral corticosteroids Oral or IV corticosteroids
Consider IV magnesium
Consider high dose ICS
If continuing deterioration, treat as
severe and re-assess for ICU
ASSESS CLINICAL PROGRESS FREQUENTLY
MEASURE LUNG FUNCTION
in all patients one hour after initial treatment
FEV1 or PEF <60% of predicted or
FEV1 or PEF 60-80% of predicted or
personal best,or lack of clinical response
personal best and symptoms improved
SEVERE
MODERATE
Continue treatment as above
Consider for discharge planning
and reassess frequently
GINA 2016, Box 4-4 (4/4) © Global Initiative for Asthma
TERIMAKASIH
© Global Initiative for Asthma
You might also like
- Diagnostic and Treatment AsthmaDocument23 pagesDiagnostic and Treatment AsthmaabcdNo ratings yet
- Breathing, Circilation, Airway PDFDocument81 pagesBreathing, Circilation, Airway PDFFiryal SorayaNo ratings yet
- Asthma Management: Perceptor: OlehDocument25 pagesAsthma Management: Perceptor: OlehSutria N. SyatiNo ratings yet
- Novel Mechanisms & Treatment For Asthma: Retno Ariza S SoemarwotoDocument36 pagesNovel Mechanisms & Treatment For Asthma: Retno Ariza S SoemarwotokuntumsuredaNo ratings yet
- Asma 2015Document82 pagesAsma 2015ayuNo ratings yet
- Dr. Ardhi Asma Slide AjarDocument51 pagesDr. Ardhi Asma Slide AjarOkta Dwi Kusuma AyuNo ratings yet
- Acute Exacerbation of AsthmaDocument48 pagesAcute Exacerbation of AsthmaWan Nur AdilahNo ratings yet
- Implementation of Diagnosis Asthma in Primary Care: Susanthy DJDocument27 pagesImplementation of Diagnosis Asthma in Primary Care: Susanthy DJEka PratiwiNo ratings yet
- Bronchiale: DR Salim S Thalib SP.P (K) 2018Document80 pagesBronchiale: DR Salim S Thalib SP.P (K) 2018Umitha Rahmi SaniNo ratings yet
- G IN A: Lobal I'a've For SthmaDocument78 pagesG IN A: Lobal I'a've For SthmaIkrar A. SutjaNo ratings yet
- GINA 2017 Teaching Slide Set FullDocument17 pagesGINA 2017 Teaching Slide Set FullLorenzoVasquezDatul100% (3)
- QRG 153 - British Guideline On The Management of Asthma: Quick Reference Guide September 2016Document28 pagesQRG 153 - British Guideline On The Management of Asthma: Quick Reference Guide September 2016HelmiZunanNo ratings yet
- Gina Asma 2019Document88 pagesGina Asma 2019Naufal HasanNo ratings yet
- Bronchial Asthma 3rd YearDocument50 pagesBronchial Asthma 3rd YearArmoured SpartanNo ratings yet
- BTS - SIGN Asthma Guideline Quick Reference Guide 2019Document28 pagesBTS - SIGN Asthma Guideline Quick Reference Guide 2019Nur Farhana Athirah AzhariNo ratings yet
- Global Strategyfor Asthma ManagementDocument88 pagesGlobal Strategyfor Asthma ManagementkhanhquphamNo ratings yet
- Asthma BronchialeDocument52 pagesAsthma BronchialeMariyatul QibthiyyahNo ratings yet
- Literature Review AADocument8 pagesLiterature Review AAGEDE GUNAWAN MAHARDIKANo ratings yet
- LCP Asthma Club Seminar Teaches Patients to Manage AsthmaDocument2 pagesLCP Asthma Club Seminar Teaches Patients to Manage AsthmaEliseo RamirezNo ratings yet
- Pharmacotheraphy for Gastrointestinal DisordersDocument41 pagesPharmacotheraphy for Gastrointestinal DisordersAlunaficha Melody KiraniaNo ratings yet
- 2013 - Sleep Review - OSA and Asthma - Treatment ImplicationsDocument7 pages2013 - Sleep Review - OSA and Asthma - Treatment ImplicationsManuel MendezNo ratings yet
- 6 DR Arlita Asma Pada AnakDocument36 pages6 DR Arlita Asma Pada AnakoktafNo ratings yet
- Obstructive Pulmonary DiseasesDocument111 pagesObstructive Pulmonary Diseasesmfrehat113No ratings yet
- 1 CPG Asthma GuidelinesDocument19 pages1 CPG Asthma GuidelinesShofiyyatunnisa' WsNo ratings yet
- Asma 3Document12 pagesAsma 3nabilla putriNo ratings yet
- Paediatric AsthmaDocument3 pagesPaediatric AsthmaDr Roelien JefferysNo ratings yet
- Presentasi DR RinaDocument45 pagesPresentasi DR RinaRIta KameliaNo ratings yet
- Asthma: Assessment, Diagnosis, and Treatment Adherence: Gerri KaufmanDocument8 pagesAsthma: Assessment, Diagnosis, and Treatment Adherence: Gerri KaufmandessyNo ratings yet
- Childhood AsthmaDocument40 pagesChildhood AsthmachinchuNo ratings yet
- AthmaDocument47 pagesAthmadrthanallaNo ratings yet
- HSNS 264 - Part BDocument9 pagesHSNS 264 - Part BHarshana Sandaruwan SomarathneNo ratings yet
- Severe AsthmaDocument15 pagesSevere AsthmasuryoNo ratings yet
- Diagnosis of Asthma: Following Initial Assessment: Without Airflow ObstructionDocument5 pagesDiagnosis of Asthma: Following Initial Assessment: Without Airflow ObstructionebookdrNo ratings yet
- Klasifikasi Asma Gina 2015Document34 pagesKlasifikasi Asma Gina 2015Roni Ardian100% (1)
- Asthma MimickersDocument6 pagesAsthma MimickersHarpreet SinghNo ratings yet
- Diagnostic Approach of Dyspepsia SyndromeDocument20 pagesDiagnostic Approach of Dyspepsia SyndromeYaniNo ratings yet
- Gina At-A-Glance Asthma Management Reference: OR ReproduceDocument4 pagesGina At-A-Glance Asthma Management Reference: OR ReproduceWahyuke Hestiyanti TunjungsariNo ratings yet
- History and Physical Write-Up 1Document5 pagesHistory and Physical Write-Up 1AJ PsychNo ratings yet
- 20180212230656-Materi DR Prasetyo, SPP PIT 2018-DikonversiDocument34 pages20180212230656-Materi DR Prasetyo, SPP PIT 2018-DikonversiKlinik Pratama Pertamina Sei PakningNo ratings yet
- health checkDocument9 pageshealth checkamoon08.arNo ratings yet
- CPCgr3 Case03 FinishDocument27 pagesCPCgr3 Case03 FinishPingky khingthongNo ratings yet
- Diagnosing Childhood Respiratory IllnessDocument39 pagesDiagnosing Childhood Respiratory IllnessAngelica StellaNo ratings yet
- Define AsthmaDocument5 pagesDefine Asthmatimie_reyesNo ratings yet
- Topic: Asthma and Copd: Internal Medicine IiDocument8 pagesTopic: Asthma and Copd: Internal Medicine IicarlosNo ratings yet
- A New Approach in The Diagnosis of Upper Airway Resistance Syndrome (UARS) : PAP MethodDocument6 pagesA New Approach in The Diagnosis of Upper Airway Resistance Syndrome (UARS) : PAP MethodRosana PortillaNo ratings yet
- Diagnosis dan Tatalaksana Asma Bronkial pada AnakDocument14 pagesDiagnosis dan Tatalaksana Asma Bronkial pada AnakZuraidaNo ratings yet
- Chronic Dyspepsia GuidelineDocument8 pagesChronic Dyspepsia Guidelinenainggolan Debora15No ratings yet
- FAPS Sperber APT ProofDocument11 pagesFAPS Sperber APT ProofAudricNo ratings yet
- Hepatitis Condensed OutlineDocument6 pagesHepatitis Condensed OutlineTonyNo ratings yet
- AsthmaDocument15 pagesAsthmaLuisa GrassNo ratings yet
- Hepatic Panel Ast/Alt Alkaline Phosphatase BilirubinDocument6 pagesHepatic Panel Ast/Alt Alkaline Phosphatase BilirubinTonyNo ratings yet
- Bronchial AsthmaDocument20 pagesBronchial AsthmaJuliet De GuzmanNo ratings yet
- Laporan Kasus Asma BronkialDocument14 pagesLaporan Kasus Asma BronkialannisanadyapNo ratings yet
- Key Symptoms and History for Diagnosing AsthmaDocument32 pagesKey Symptoms and History for Diagnosing Asthmafurr singhNo ratings yet
- RJP 2007 3 Art-05Document12 pagesRJP 2007 3 Art-05Cristian CondreaNo ratings yet
- Differential Diagnosis of Gastrointestinal DiseasesDocument5 pagesDifferential Diagnosis of Gastrointestinal DiseasesSean Dominique Cruz MaghinayNo ratings yet
- Asthma Pocket Guide For Health Care Professionals in SA 1611853029Document31 pagesAsthma Pocket Guide For Health Care Professionals in SA 1611853029Mans AlghamdiNo ratings yet
- Asthma NicolasDocument21 pagesAsthma NicolasKimberly Mondala (SHS)No ratings yet
- Oleh: Fina Khairunnisa: Diagnosis and Treatment of Gastroesophageal Reflux DiseaseDocument14 pagesOleh: Fina Khairunnisa: Diagnosis and Treatment of Gastroesophageal Reflux DiseaseFina KhairunnisaNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 2: RespiratoryFrom EverandComplementary and Alternative Medical Lab Testing Part 2: RespiratoryNo ratings yet
- IKAFI - DPP4 InhibitorDocument25 pagesIKAFI - DPP4 InhibitorYuliarni Hasan100% (1)
- Blanko Cover JiwaDocument2 pagesBlanko Cover JiwaYuliarni HasanNo ratings yet
- Happiness Inside PDFDocument304 pagesHappiness Inside PDFYuliarni Hasan100% (4)
- Kualitas Hidup Salah Satu Indikator Yogya (DR Maria)Document45 pagesKualitas Hidup Salah Satu Indikator Yogya (DR Maria)Yuliarni HasanNo ratings yet
- Stroke PDFDocument79 pagesStroke PDFYuliarni HasanNo ratings yet
- Happiness InsideDocument304 pagesHappiness InsideYuliarni HasanNo ratings yet
- AsosiasiDocument28 pagesAsosiasiYuliarni HasanNo ratings yet
- Stroke PDFDocument79 pagesStroke PDFYuliarni HasanNo ratings yet
- Sex EnhancerDocument27 pagesSex EnhancerYuliarni Hasan0% (1)
- Body of Knowledge BatraDocument64 pagesBody of Knowledge BatraYuliarni HasanNo ratings yet
- IKAFI ThiazolidinedionesDocument32 pagesIKAFI ThiazolidinedionesYuliarni HasanNo ratings yet
- DPP-4 inhibitors for managing Type 2 DiabetesDocument25 pagesDPP-4 inhibitors for managing Type 2 DiabetesYuliarni HasanNo ratings yet
- Uji Klinik Dan Evidence-Based: Herbal MedicinesDocument119 pagesUji Klinik Dan Evidence-Based: Herbal MedicinesaditNo ratings yet
- Jadwal Audit InternalDocument1 pageJadwal Audit InternalYuliarni HasanNo ratings yet
- Mechanical Ventilation of The Premature NeonateDocument16 pagesMechanical Ventilation of The Premature NeonateHaitham HafezNo ratings yet
- Bronchial Asthma Diagnosis & TreatmentDocument3 pagesBronchial Asthma Diagnosis & TreatmentHugh JacobsNo ratings yet
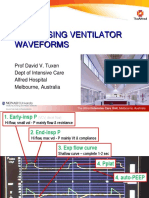
- Ventilator Waveforms DavidTuxen2Document41 pagesVentilator Waveforms DavidTuxen2Syed Shahrul Naz Syed100% (1)
- Compile Nclex - RN Questions and AnswersDocument17 pagesCompile Nclex - RN Questions and Answerseric0% (1)
- Bronchial Asthma: Causes, Symptoms and TreatmentDocument21 pagesBronchial Asthma: Causes, Symptoms and TreatmentshaitabliganNo ratings yet
- Trilogy Evo Quick Start GuideDocument24 pagesTrilogy Evo Quick Start GuideAngeloNo ratings yet
- 4 - Asthma Dan Status AsthmaticusDocument49 pages4 - Asthma Dan Status AsthmaticusMaspupah Widiyanti RachmatNo ratings yet
- Suppurative Lung DIseaseDocument33 pagesSuppurative Lung DIseaseNur Liyana Ahmad ZakiNo ratings yet
- Lagier2022 Atelectasia en AnestesiologiaDocument31 pagesLagier2022 Atelectasia en AnestesiologiaNicolas SuarezNo ratings yet
- Fibroza pulmonara idiopatica (FPIDocument25 pagesFibroza pulmonara idiopatica (FPIAnna HaritonencoNo ratings yet
- Pulmonary Edema Nursing Diagnosis & Care Plan - NurseTogetherDocument10 pagesPulmonary Edema Nursing Diagnosis & Care Plan - NurseTogetherANDREW GOS BNo ratings yet
- RespirationDocument2 pagesRespirationSathyaNo ratings yet
- Oxymag EnglishDocument40 pagesOxymag EnglishAlauddin SyahNo ratings yet
- Protective Mechanical Ventilation in The ObeseDocument5 pagesProtective Mechanical Ventilation in The ObeseEmmanuel FortalezaNo ratings yet
- AtelectasisDocument37 pagesAtelectasisSandara ParkNo ratings yet
- Acapella ProtocolDocument3 pagesAcapella ProtocolRTdadNo ratings yet
- LTV 1200 MR Conditional BrochureDocument4 pagesLTV 1200 MR Conditional BrochureZulkifli IsmailNo ratings yet
- Diagnosis and Management of COPD: A Case Study: RespiratoryDocument4 pagesDiagnosis and Management of COPD: A Case Study: RespiratoryUssy TsnnnNo ratings yet
- Chapter 2 Respiratory AssessmentDocument9 pagesChapter 2 Respiratory AssessmentKathleen Dela CruzNo ratings yet
- Respiratory System Reading 1Document4 pagesRespiratory System Reading 1Trí Nguyễn Vũ CaoNo ratings yet
- Gambaran Faal Paru Pada Pasien Asma Yang Melakukan Senam Asma Dengan Yang Tidak Melakukan Senam Asma Uci Tama Azilla Sri Melati Munir Eka BebasariDocument17 pagesGambaran Faal Paru Pada Pasien Asma Yang Melakukan Senam Asma Dengan Yang Tidak Melakukan Senam Asma Uci Tama Azilla Sri Melati Munir Eka BebasariiqbalNo ratings yet
- Asuhan Keperawatan Pada Pasien COPDDocument17 pagesAsuhan Keperawatan Pada Pasien COPDsuper manggis100% (1)
- Fundamentals of NursingDocument5 pagesFundamentals of NursingLance Sta AnaNo ratings yet
- 2.manajemen Gawat Nafas Pada Bayi Dan Anak - DrlizaDocument89 pages2.manajemen Gawat Nafas Pada Bayi Dan Anak - DrlizayuniayuNo ratings yet
- Endotracheal Intubation Management RPAH PC2022 014Document15 pagesEndotracheal Intubation Management RPAH PC2022 014sinasinaaiNo ratings yet
- PASSMEDICINE MCQs-RESPIRATORY MEDICINEDocument111 pagesPASSMEDICINE MCQs-RESPIRATORY MEDICINEHashim Ahmad75% (4)
- Ineffective Airway Clearance Related To BronchospasmDocument2 pagesIneffective Airway Clearance Related To BronchospasmReylan Garcia100% (4)
- Ventilator ModesDocument3 pagesVentilator ModesLudmila CrenshawNo ratings yet
- Chapter 01Document7 pagesChapter 01Robert Kerwick100% (5)
- Ventilators, Intensive CareDocument48 pagesVentilators, Intensive CarealetripoleNo ratings yet