Professional Documents
Culture Documents
Guillain Barre Syndrome by DR Gireesh Kumar K P
Uploaded by
AETCM Emergency medicine0 ratings0% found this document useful (0 votes)
175 views10 pagesGuillain Barre Syndrome by Dr Gireesh Kumar K P
Original Title
Guillain Barre Syndrome by Dr Gireesh Kumar K P
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentGuillain Barre Syndrome by Dr Gireesh Kumar K P
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
175 views10 pagesGuillain Barre Syndrome by DR Gireesh Kumar K P
Uploaded by
AETCM Emergency medicineGuillain Barre Syndrome by Dr Gireesh Kumar K P
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 10
GUILLAIN BARRE SYNDROME
GUILLAIN BARRE SYNDROME
• It is the most common type of acute
polyneuropathy
• It is an acute diffuse post infective disease
involving spinal roots, peripheral nerves and
occasionally cranial nerves causing generalized
paralysis
Causes
• Viral infection – CMV, HIV, EBV, Chickenpox
• Bacterial – Campylobacter jejuni, Mycoplasma
Pneumonia
• Others
• Lymphoma (Hodgkin’s)
• Systemic Lupus Erythematosus
• Sarcoidosis
• Post vaccination – Older type of Rabies vaccine
Weakness
• Ascending type of progressive weakness (Acute
onset):The weakness usually starts in lower limbs, but
it may start in the upper limbs or facial muscles in
about 10% of patients.
• Weakness of proximal muscles > distal muscles
• Cranial nerves: Facial nerve weakness seen in >50%,
and oropharyngeal weakness seen in 50%.
Oculomotor weakness seen in 15 %.
• Severe respiratory muscle weakness necessitating
ventilatory support seen in 10 to 30%
Other features
• Absent deep tendon reflexes (in 90%)
• Paresthesias (No sensory impairment) Paresthesias in
the hands and feet accompany the weakness in more
than 80%, but sensory abnormalities on examination
are frequently mild or nil.
• Pain due to nerve root inflammation, mainly located
in the back and extremities, during the acute phase by
two-thirds of patients with all forms of GBS
• Dysautonomia occurs in around 70%. SIADH, which
may be due to autonomic involvement, is also seen in
GBS
DDs
• Periodic paralysis ( Variation in serum potassium , normal cerebrospinal fluid)
• Botulism (descending paralysis)
• Hypophosphatemia (irritable, apprehensive, hyperventilation, normal
cerebrospinal fluid)
• Myasthenia gravis (weakness and fatigue that improves with rest)
• Tick paralysis (sensory changes absent, normal cerebrospinal fluid)
• Transverse myelitis (abrupt bilateral leg weakness, ascending sensory)
• Vasculitic neuropathies (mononeuropathy)
• Basilar artery thrombosis (asymmetric limb paresis)
• Metabolic myopathies (cerebral and cerebellar symptoms)
• Poliomyelitis (purely motor disorder with meningitis)
• Polymyositis (chronic, affects proximal limb muscles)
Diagnostic criteria
Required • Supportive
•Progressive weakness of 2 or more • Relatively symmetric weakness
limbs due to neuropathy • No sensory involvement
• Facial nerve or other cranial nerve
•Areflexia involvement
•Progression of disease less than 4 • Absence of fever
weeks • CSF study (Albumino-cytological
dissociation)
•Exclusion of other causes like
• Electrophysiological evidence of
• Vasculitis (PAN, SLE, CSS) demyelination
• Toxins (Organophosphorus poisoning,
Lead) • Features making the diagnosis
• Infections (Diphtheria, Botulism) doubtful
• Porphyria • Sensory loss
• Marked asymmetry or symptoms and
signs
• Severe bladder and bowel dysfunction
CSF study
• CSF – (Albumino-cytological dissociation - in up
to 66% of patients with GBS at one week after
onset of symptoms.)
• Protein – elevated
• Cells – Normal
• A CSF pleocytosis can be seen in GBS patients who
have HIV infection
NCV study
• Electrodiagnostic features(nerve conduction study)
• In demyelination prolonged distal latencies,
conduction velocity slowing, evidence of conduction
block, and temporal dispersion of compound action
potential are the usual features.
• In primary axonal pathology, the principal
electrodiagnostic finding is reduced amplitude of
compound action potentials without conduction
slowing or prolongation of distal latencies.
Management
• IV immunoglobulin (IVIG) - IVIG (400 mg/kg/d for 5
days)
• Plasmapheresis :
• Plasmapheresis is an extracorporeal blood purification
technique designed for the removal of large molecular
weight substances from the plasma.
• Patients with mild GBS on admission should receive 2 PEs.
Patients with moderate and severe forms should benefit
from 2 further exchanges , 1 to 1.5 plasma volume
exchanges per procedure
• Corticosteroids (oral or IV): not recommended
You might also like
- SARS-CoV2 Ag Kit - Biosensor PDFDocument2 pagesSARS-CoV2 Ag Kit - Biosensor PDFAETCM Emergency medicineNo ratings yet
- SVT PediatricDocument1 pageSVT PediatricAETCM Emergency medicineNo ratings yet
- SARS-CoV2 Ag Kit - Biosensor PDFDocument2 pagesSARS-CoV2 Ag Kit - Biosensor PDFAETCM Emergency medicineNo ratings yet
- Snake Bite ToxiconDocument14 pagesSnake Bite ToxiconAETCM Emergency medicine100% (1)
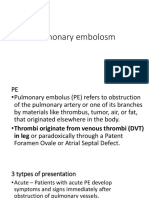
- Pulmonary EmbolosmDocument15 pagesPulmonary EmbolosmAETCM Emergency medicineNo ratings yet
- SARS-CoV2 Ag Kit - Biosensor PDFDocument2 pagesSARS-CoV2 Ag Kit - Biosensor PDFAETCM Emergency medicineNo ratings yet
- Pulmonary EmbolosmDocument15 pagesPulmonary EmbolosmAETCM Emergency medicineNo ratings yet
- Post Exposure Prophylaxis in HIVDocument9 pagesPost Exposure Prophylaxis in HIVAETCM Emergency medicineNo ratings yet
- Innovation EDDocument32 pagesInnovation EDAETCM Emergency medicineNo ratings yet
- HyponatremiaDocument19 pagesHyponatremiaAETCM Emergency medicine100% (1)
- Stroke ManagementDocument18 pagesStroke ManagementAETCM Emergency medicineNo ratings yet
- Bells Palsy by DR Gireesh Kumar K PDocument6 pagesBells Palsy by DR Gireesh Kumar K PAETCM Emergency medicineNo ratings yet
- Stroke ManagementDocument18 pagesStroke ManagementAETCM Emergency medicineNo ratings yet
- HyponatremiaDocument19 pagesHyponatremiaAETCM Emergency medicine100% (1)
- Post Exposure Prophylaxis in HIV by DR Gireesh Kumar KPDocument9 pagesPost Exposure Prophylaxis in HIV by DR Gireesh Kumar KPAETCM Emergency medicineNo ratings yet
- Acute Exacerbation of COPD by DR Gireesh Kumar KPDocument12 pagesAcute Exacerbation of COPD by DR Gireesh Kumar KPAETCM Emergency medicineNo ratings yet
- Acute Myocardial Infarction by DR Gireesh Kumar K PDocument18 pagesAcute Myocardial Infarction by DR Gireesh Kumar K PAETCM Emergency medicine50% (2)
- Status Epilepticus by DR Gireesh Kumar K PDocument18 pagesStatus Epilepticus by DR Gireesh Kumar K PAETCM Emergency medicineNo ratings yet
- Acute Asthma by DR Gireesh Kumar KPDocument15 pagesAcute Asthma by DR Gireesh Kumar KPAETCM Emergency medicineNo ratings yet
- Hepatic Encephalopathy Is by DR Gireesh Kumar K PDocument16 pagesHepatic Encephalopathy Is by DR Gireesh Kumar K PAETCM Emergency medicineNo ratings yet
- Status Epileptic Us by DR Gireesh Kumar K PDocument18 pagesStatus Epileptic Us by DR Gireesh Kumar K PAETCM Emergency medicineNo ratings yet
- Platelet, FFP and Cryoprecipitate Transfusion in Emergency Room by DR Riaz AhamedDocument31 pagesPlatelet, FFP and Cryoprecipitate Transfusion in Emergency Room by DR Riaz AhamedAETCM Emergency medicineNo ratings yet
- Pulmonary Edema by DR Gireesh Kumar K PDocument16 pagesPulmonary Edema by DR Gireesh Kumar K PAETCM Emergency medicineNo ratings yet
- Snake Bite by DR Gireesh Kumar KPDocument13 pagesSnake Bite by DR Gireesh Kumar KPAETCM Emergency medicineNo ratings yet
- Hyperkalemia by DR Gireesh Kumar K PDocument15 pagesHyperkalemia by DR Gireesh Kumar K PAETCM Emergency medicineNo ratings yet
- Organo Phosphate Poisoning by DR Gireesh Kumar K PDocument16 pagesOrgano Phosphate Poisoning by DR Gireesh Kumar K PAETCM Emergency medicineNo ratings yet
- Pulmonary Edema by DR Gireesh Kumar K PDocument16 pagesPulmonary Edema by DR Gireesh Kumar K PAETCM Emergency medicineNo ratings yet
- Nipah Viral Infection by DR Gireesh Kumar KPDocument10 pagesNipah Viral Infection by DR Gireesh Kumar KPAETCM Emergency medicineNo ratings yet
- Diabetic Emergencies by DR Gireesh Kumar K P, Department of Emergency Medicine, Amrita Institute of Medical Sciences, KochiDocument23 pagesDiabetic Emergencies by DR Gireesh Kumar K P, Department of Emergency Medicine, Amrita Institute of Medical Sciences, KochiSreekrishnan Trikkur100% (2)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Malaria & Cerebral Malaria: Livia Hanisamurti, S.Ked 71 2018 045Document40 pagesMalaria & Cerebral Malaria: Livia Hanisamurti, S.Ked 71 2018 045Livia HanisamurtiNo ratings yet
- Colonoscopy Is Mandatory AfterDocument3 pagesColonoscopy Is Mandatory AfterLaurice BarronNo ratings yet
- Asperger SyndromeDocument4 pagesAsperger SyndromeJonald AlvaranNo ratings yet
- Mineral Nutrition Contributes To Plant Disease and Pest ResistanceDocument5 pagesMineral Nutrition Contributes To Plant Disease and Pest ResistanceHectorSHNo ratings yet
- Grand Case Pres FDARDocument11 pagesGrand Case Pres FDARMika SaldañaNo ratings yet
- UT Dallas Syllabus For Biol1318.001 05f Taught by Lee Bulla (Bulla)Document1 pageUT Dallas Syllabus For Biol1318.001 05f Taught by Lee Bulla (Bulla)UT Dallas Provost's Technology GroupNo ratings yet
- Cardiology UQU 2022Document29 pagesCardiology UQU 2022Elyas MehdarNo ratings yet
- S 0140525 X 00003368 ADocument59 pagesS 0140525 X 00003368 AEnver OruroNo ratings yet
- SMH Annual Report 2016Document12 pagesSMH Annual Report 2016Chelsey BoyleNo ratings yet
- MSDS Jun-Air SJ-27FDocument8 pagesMSDS Jun-Air SJ-27FJuan Eduardo LoayzaNo ratings yet
- SECOND Semester, AY 2022-2023: Mission VisionDocument34 pagesSECOND Semester, AY 2022-2023: Mission Visionjeyyy BonesssNo ratings yet
- WHO International Standards For Drinking Water PDFDocument204 pagesWHO International Standards For Drinking Water PDFAnonymous G6ceYCzwt100% (1)
- IAA Protein Conjugadotes 2008Document6 pagesIAA Protein Conjugadotes 2008shady182No ratings yet
- 3 Pocket Size-CriminalisticsDocument77 pages3 Pocket Size-CriminalisticsCriminology Criminology CriminologyNo ratings yet
- ElectrocardiogramDocument17 pagesElectrocardiogramvinnu kalyanNo ratings yet
- TAPSE AgainDocument8 pagesTAPSE Againomotola ajayiNo ratings yet
- Cases and Doctrines On Legal MedicineDocument44 pagesCases and Doctrines On Legal MedicineEliza MontemayorNo ratings yet
- Clinico-Pathological Study On Haemophilia: An Analysis of 50 CasesDocument4 pagesClinico-Pathological Study On Haemophilia: An Analysis of 50 CasesSajjad Hossain ShuvoNo ratings yet
- Aioh Position Paper DPM jdk2gdDocument26 pagesAioh Position Paper DPM jdk2gdRichardNo ratings yet
- Prof. Eman Rushdy Sulphonylurea A Golden Therapy For DiabetesDocument51 pagesProf. Eman Rushdy Sulphonylurea A Golden Therapy For Diabetestorr123No ratings yet
- Presentation On Hysterosalpingography: BY Mahmud M Alkali I.D: 12/01/09/069 Radiography, Unimaid. 2014/2015 SESSIONDocument23 pagesPresentation On Hysterosalpingography: BY Mahmud M Alkali I.D: 12/01/09/069 Radiography, Unimaid. 2014/2015 SESSIONMubarak M AlkaliNo ratings yet
- DoxycolDocument13 pagesDoxycolMark CastilloNo ratings yet
- OMFC Application RequirementsDocument1 pageOMFC Application RequirementshakimNo ratings yet
- Chi Cards 1Document43 pagesChi Cards 1SwordAceNo ratings yet
- Meta Health Social Media Toolkit - EnglishDocument18 pagesMeta Health Social Media Toolkit - EnglishAndri MayasariNo ratings yet
- Strabismus and Eye Muscle SurgeryDocument68 pagesStrabismus and Eye Muscle SurgeryOpeyemi IdaeworNo ratings yet
- Rubber Dam Isolation For Endodontic Treatment in Difficult Clinical SituationsDocument8 pagesRubber Dam Isolation For Endodontic Treatment in Difficult Clinical SituationsDavid ColonNo ratings yet
- LamaDocument3 pagesLamarockyNo ratings yet
- 302 PpJ. Grayson, Freedom From Obsessive Compulsive Disorder A Personalized Recovery Program For LivingDocument2 pages302 PpJ. Grayson, Freedom From Obsessive Compulsive Disorder A Personalized Recovery Program For LivingMohammad Shoyyad L IkhsanNo ratings yet
- UntitledDocument75 pagesUntitledMelissa DrakeNo ratings yet