Professional Documents
Culture Documents
Prof. Mutti Ullah Khan Medical Unit III Services Hospital
Uploaded by
Musa Azhar0 ratings0% found this document useful (0 votes)
135 views41 pagesFibers of the cricopharyngeus muscle represent the upper esophageal sphincter (UES) in thoracic cavity it lies in posterior mediastinum, posterior to the trachea. LES: tonically closed at rest, pressure 20 mmHg, cholinergic mediated, relaxes with swallowing is the major cause of reflux.
Original Description:
Original Title
Esophageal Diseases (1)
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentFibers of the cricopharyngeus muscle represent the upper esophageal sphincter (UES) in thoracic cavity it lies in posterior mediastinum, posterior to the trachea. LES: tonically closed at rest, pressure 20 mmHg, cholinergic mediated, relaxes with swallowing is the major cause of reflux.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
135 views41 pagesProf. Mutti Ullah Khan Medical Unit III Services Hospital
Uploaded by
Musa AzharFibers of the cricopharyngeus muscle represent the upper esophageal sphincter (UES) in thoracic cavity it lies in posterior mediastinum, posterior to the trachea. LES: tonically closed at rest, pressure 20 mmHg, cholinergic mediated, relaxes with swallowing is the major cause of reflux.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 41
Prof.
Mutti Ullah Khan
Medical Unit III
Services Hospital
Anatomy of Esophagus
Hollow tube formed of striated muscle (upper
part) and smooth muscle (lower part).
Length about 20-30 cm in adults.
Fibers of the cricopharyngeus muscle
represent the upper esophageal sphincter
(UES).
In thoracic cavity it lies in posterior
mediastinum, posterior to the trachea.
Leaves thorax through diaphragmatic hiatus
Lower esophageal sphincter (LES) about 3-5
cm long, ?physiological sphincter.
Microscopic Anatomy of esophagus
Mucosa:
Lined with stratified squamous epithelium, rich
in glycogen.
Lamina propria
muscularis mucosa : thin layer of smooth
muscle
Submucosa
The outer muscular layers: striated in the
upper part and smooth in lower 2/3
No serosal covering.
Physiology
UES: tonically closed, opens 0.2-0.3 sec
after a swallow.
Peristaltic contractions, duration less than
7 sec and amplitude less than 150 mmHg,
velocity less than 8 cm/sec
LES: tonically closed at rest, pressure 20
mmHg, cholinergic mediated, relaxes with
swallowing.
Transient LES relaxation, independent of
swallowing is the major cause of reflux.
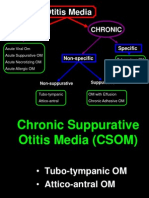
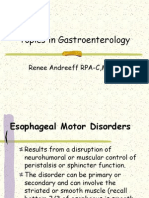
Motor disorders of the esophagus
Achalasia
Localized esophageal spasm
Diffuse esophageal spasm
Nutcracker esophagus
Non-specific motor abnormalities
Achalasia
Failure of relaxation of the LES
with swallowing and aperistalsis
in lower esophagus.
Due to decreased or absent
intramural esophageal ganglion
cells.
Symptoms of Achalasia
Dysphagia to fluids and solids, intermittent, long
-standing.
Regurgitation of undigested food
Chest pain
Aspiration
Weight loss
Diagnosis of achalasia
Esophageal manometry:
Absent peristalsis
High LES pressure
Failure of relaxation of LES.
Radiographic studies
Endoscopy to exclude organic disease.
Normal Achalasia
TREATMENT OF ACHALASIA
Management Goals
Relieve symptoms
Improve esophageal emptying
Prevent development of megaesophagus
TREATMENT OF ACHALASIA
Drug therapy
Smooth muscle relaxants
Botulinum toxin injection
1 to 2 years relief
Symptomatic relief
Semisoft bland diet
Eating slowly
Drinking with meals
Sleeping with Head end elevated
Endoscopic pneumatic dilation
Outpatient procedure
LES disrupted using balloons of progressively larger diameters
Repeat dilations are often required
Surgical myotomy
DEFINITIONS
Gasrtoesophageal reflux: Reflux of gastric
contents to the esophagus
Gastroesophageal reflux disease (GERD): Any
significant symptomatic clinical condition or
histopathological changes resulting from
reflux.
Reflux esophagitis: GERD patients with
histopathologically demonstrable changes in
the esophageal mucosa.
Epidemiology of GERD
Heartburn is a very common condition:
3% of population experience heartburn daily
7% frequently
15% weekly
25% monthly
Most common in pregnant women: 80%
Common in obese and smokers
Mechanisms of GERD
Transient LES relaxation
Hypotensive LES
Decreased esophageal acid clearance
Hiatus hernia
Impaired salivation.
CLINICAL PICTURE OF GERD
ESOPHAGEAL SYMPTOMS
EXTRAESOPHAGEAL SYMPTOMS
ESOPHAGEAL SYMPTOMS OF
GERD
HEARTBURN
REGURGITATION
Bad Breath
Dysphagia
Chest pain
Water brash
Nausea and vomiting
Belching
Hiccup
EXTRAESOPHAGEAL SYMPTOMS OF
GERD
Chronic cough
Asthma
recurrent pneumonitis
nocturnal choking
hoarseness of voice
posterior laryngitis with ulceration and
granuloma formation.
sore throat
dental disease
Earache
Globus sensation
Diagnosis of GERD
Clinical picture.
UGI endoscopy.
24 hour pH monitoring
Radioisotope scanning
Barium swallow.
Complications of GERD
Stricture formation
Chronic blood loss
Barrett’s epithelium
Narrow band imaging & chromoendoscopy with
methylene blue are used as diagnostic tool.
Adenocarcinoma
Savary Gillard dilator used for
dilatation of esophageal strictures
Barrett’s epithelium
Barrett’s epithelium
Narrow Band Imaging used for diagnosis of barrett’s epthelium
Barrett’s epithelium
Chromoendoscopy using methylene blue used for diagnosis of Barrett’s
Natural history of GERD
May be acute condition in a small percentage
Mostly chronic condition with recurrent
symptoms
Majority can be controlled on drugs
Majority may require a sort of acid
suppressive therapy at 5 years
No clear relation exists between symptoms of
reflux, amount of reflux or degree of
esophagitis.
Management of GERD
Life- style modification:
avoid cigarette smoking
dietary manipulation: decrease fatty, spicy and
acidic foods
decrease weight
elevation of the head of the bed
avoid tight abdominal binders
avoid constipation
avoid large meals
avoid drugs which decrease LES pressure
avoid sleeping after meals for at least 3 hours.
Pharmacologic therapy of GERD
Antacids:
Mg trisilicate
Aluminium hydroxide
Ca carbonate
sodium bicarbonate.
H2-blockers:
Cimetidine
ranitidine
famotidine
nizatidine
Pharmacologic therapy of GERD
Proton pump inhibitors:
Omeprazole
lansoprazole
pantoprazole
rabeprazole
Esomeprazole
Tenatoprazole
Prokinetic drugs:
metoclopramide
domperidone.
Endoscopic therapy for GERD
Sterrata procedure
Entyrex
Gate keeper anti-reflux repair
Gastric plication
Antireflux
surgery
Indications:
complicated reflux
non compliance for medication
refractory GERD
patient’s preference
severe disease in young person
Most popular operation now is
laparoscopic fundoplication
Treatment of Barrett’s epithelium
BE usually occurs in longstanding severe
reflux disease
BE does not regress after fundoplication or
PPI therapy
Screening for dysplasia?
If high grade dysplasia found:
esophagectomy
Ablation of BE:
Photodynamic therapy
Argon plasma coagulation
Endoscopic mucosal resection
You might also like
- Disorder of Oral CavityDocument4 pagesDisorder of Oral CavitySiva0726No ratings yet
- GERDDocument38 pagesGERDss33% (3)
- GERD ManagementDocument43 pagesGERD ManagementpashaNo ratings yet
- Burn ManagementDocument91 pagesBurn ManagementMaham Baqai100% (1)
- CSOM TreatmentDocument21 pagesCSOM TreatmentSarwinder SinghNo ratings yet
- Stomach Peptic UlcerDocument38 pagesStomach Peptic UlcermohamedNo ratings yet
- Child Ear Infection CausesDocument9 pagesChild Ear Infection CausesMona Santi NainggolanNo ratings yet
- Management of Asthma ExacerbationDocument13 pagesManagement of Asthma ExacerbationAini Shofa HaniahNo ratings yet
- Case Presentation - GASTRODocument46 pagesCase Presentation - GASTROalidudeNo ratings yet
- Dermatological PharmacologyDocument53 pagesDermatological PharmacologyDesta BelachewNo ratings yet
- ThyroidectomyDocument17 pagesThyroidectomyDaryl Joshua SaturnoNo ratings yet
- Chest Injuries GuideDocument19 pagesChest Injuries GuideAbdi Kumala100% (1)
- What Is AchalasiaDocument6 pagesWhat Is AchalasiaDonnaliza Delos ReyesNo ratings yet
- Isabela State University City of Ilagan Campus: Care of The Clients With Endocrine and Metabolic DisorderDocument15 pagesIsabela State University City of Ilagan Campus: Care of The Clients With Endocrine and Metabolic DisorderCharlz ZipaganNo ratings yet
- What Is Gas Gangrene? Causes, Symptoms, Treatment & PreventionDocument6 pagesWhat Is Gas Gangrene? Causes, Symptoms, Treatment & PreventionIwan AchmadiNo ratings yet
- Hernias Types and TreatmentDocument19 pagesHernias Types and Treatmenthussain AltaherNo ratings yet
- PancreatitisDocument59 pagesPancreatitisAarif RanaNo ratings yet
- Aiman - Patient Case Study ReportDocument14 pagesAiman - Patient Case Study Reportezwan007100% (1)
- Cough: PHR Sangita ShakyaDocument21 pagesCough: PHR Sangita ShakyaCurex QANo ratings yet
- BurnsDocument16 pagesBurnsSalman KhanNo ratings yet
- Portal hypertension diagnosis and managementDocument23 pagesPortal hypertension diagnosis and managementSumathi Gopinath100% (1)
- Case Study: MYXEDEMATOUS COMADocument5 pagesCase Study: MYXEDEMATOUS COMAjisooNo ratings yet
- Lower Respiratory Tract Infections: Manali H Solanki F.Y.M.Sc - Nursing J G College of NursingDocument95 pagesLower Respiratory Tract Infections: Manali H Solanki F.Y.M.Sc - Nursing J G College of NursingRI NANo ratings yet
- Bronchial AsthmaDocument45 pagesBronchial Asthmamuluken mulatieNo ratings yet
- Upper Respıratory Tract InfectıonsDocument68 pagesUpper Respıratory Tract InfectıonsMekdes ZewdeNo ratings yet
- COPD: Chronic Obstructive Pulmonary DiseaseDocument3 pagesCOPD: Chronic Obstructive Pulmonary DiseaseRichard TanNo ratings yet
- Otitis Media: Prepared By: - Priyanka ThapaDocument38 pagesOtitis Media: Prepared By: - Priyanka ThapaKalo kajiNo ratings yet
- Drug Used in Skin and Mucus MembraneDocument35 pagesDrug Used in Skin and Mucus MembraneMamta Yadav100% (1)
- Anal FistulaDocument26 pagesAnal FistulaBeverly PagcaliwaganNo ratings yet
- First Aide 2023Document97 pagesFirst Aide 2023jrfdcafprescomNo ratings yet
- C C W - B C - T M: U R T I (P, Urti, S, B) : (1) PharyngitisDocument5 pagesC C W - B C - T M: U R T I (P, Urti, S, B) : (1) PharyngitiscorsaruNo ratings yet
- Case Study 2Document37 pagesCase Study 2api-391842100No ratings yet
- HypertensionDocument21 pagesHypertensionM RaisNo ratings yet
- ENT Nursing Care GuideDocument32 pagesENT Nursing Care GuideabdulNo ratings yet
- Pulmonary Embolism Guide: Causes, Symptoms & DiagnosisDocument60 pagesPulmonary Embolism Guide: Causes, Symptoms & DiagnosisRafika RaraNo ratings yet
- Burns Practice TeachingDocument58 pagesBurns Practice TeachingSakthi Devi100% (1)
- Case Presentation: by Michael ArmstrongDocument21 pagesCase Presentation: by Michael ArmstrongWirawan Amirul BahriNo ratings yet
- 1.case Presentation CHDDocument23 pages1.case Presentation CHDDHARM MEENANo ratings yet
- InhalDocument33 pagesInhallupeNo ratings yet
- Overview of Diabetes MellitusDocument30 pagesOverview of Diabetes MellitusCristina Iulia100% (1)
- Empyema 171013100219Document23 pagesEmpyema 171013100219Mahmoud Abdel MoneimNo ratings yet
- SL NO Content NODocument12 pagesSL NO Content NOPdianghunNo ratings yet
- Osh State UniversityDocument14 pagesOsh State Universitykhuzaima9No ratings yet
- Hernias: Daniel IgoDocument46 pagesHernias: Daniel Igobigboss80s100% (1)
- Nutrition and Malnutrition Resource UnitDocument22 pagesNutrition and Malnutrition Resource UnitMitch GatdulaNo ratings yet
- Esophageal Carcinoma: Preceptor: Dr. Ratesh KhillanDocument37 pagesEsophageal Carcinoma: Preceptor: Dr. Ratesh KhillanVarun VarnNo ratings yet
- HIV/AIDS Determinants and Control FactorsDocument4 pagesHIV/AIDS Determinants and Control FactorsahiNo ratings yet
- Goitre: Dr. Sandhya Gupta Assistant Professor General SurgeryDocument59 pagesGoitre: Dr. Sandhya Gupta Assistant Professor General SurgerySandhya guptaNo ratings yet
- 46-Year-Old Man With Abnormal Lipid ProfileDocument3 pages46-Year-Old Man With Abnormal Lipid ProfileCamiiliita Fernández La TorreNo ratings yet
- Myocardial InfarctionDocument15 pagesMyocardial Infarctionanon_877280340No ratings yet
- Bronchial AsthmaDocument11 pagesBronchial AsthmaFaria Islam JuhiNo ratings yet
- Otitis Media OtolaryngologyDocument45 pagesOtitis Media OtolaryngologyDr.Sherif Bugnah100% (5)
- Common Cold Symptoms, Treatment, and PreventionDocument3 pagesCommon Cold Symptoms, Treatment, and Preventionanisa rimadhaniNo ratings yet
- Nephrotic Syndrome: Prepared By: Manisha Praharaj Msc. Nursing 2Nd YearDocument28 pagesNephrotic Syndrome: Prepared By: Manisha Praharaj Msc. Nursing 2Nd YearMaria YaseenNo ratings yet
- ENT Emergencies LectureDocument29 pagesENT Emergencies LectureThea Bertea100% (1)
- ABSITE EsophagusDocument48 pagesABSITE Esophagussgod34No ratings yet
- Motility Disorders of The GITDocument57 pagesMotility Disorders of The GITMahmoud AjinehNo ratings yet
- Topics in Gastroenterology - 2014Document79 pagesTopics in Gastroenterology - 2014BwatNo ratings yet
- St. Anthony College of Roxas CityDocument14 pagesSt. Anthony College of Roxas CityMykristie Jho B. MendezNo ratings yet
- EVS - CO-5 - PPT - UO 5fDocument22 pagesEVS - CO-5 - PPT - UO 5fGirish KhedikarNo ratings yet
- PED011 Final Req 15Document3 pagesPED011 Final Req 15macabalang.yd501No ratings yet
- AHA Activity Hazard AnalysisDocument24 pagesAHA Activity Hazard AnalysisElvyn Fabellore HerreraNo ratings yet
- SADES18 DikonversiDocument90 pagesSADES18 DikonversiIc-tika Siee ChuabbieNo ratings yet
- Functions of Agriculture DronesDocument2 pagesFunctions of Agriculture DronesShahraz AliNo ratings yet
- Article Review: Health Belief ModelDocument2 pagesArticle Review: Health Belief ModelRipe Marcelino-BulfaNo ratings yet
- Public Availability of Labeling CBE Guidance PDFDocument6 pagesPublic Availability of Labeling CBE Guidance PDFMichael wangNo ratings yet
- Milrinone As Compared With DobutamineDocument10 pagesMilrinone As Compared With DobutamineArquivos DiversosNo ratings yet
- Coping StrategyDocument2 pagesCoping StrategyJeffson BalmoresNo ratings yet
- Review Exercises XiDocument14 pagesReview Exercises XiP. GilbertNo ratings yet
- VaanannanDocument53 pagesVaanannankevalNo ratings yet
- hw320 Unit 9 Final Assigment Stacey StoryDocument15 pageshw320 Unit 9 Final Assigment Stacey Storyapi-651674228No ratings yet
- FAO, WHO - Assuring Food Safety and Quality. Guidelines.2003 PDFDocument80 pagesFAO, WHO - Assuring Food Safety and Quality. Guidelines.2003 PDFAlexandra Soares100% (1)
- 17 SDGsDocument48 pages17 SDGsKiều Ngọc DungNo ratings yet
- 2019 - Asupan Zat Gizi Makro Dan Mikro Terhadap Kejadian Stunting Pada BalitaDocument6 pages2019 - Asupan Zat Gizi Makro Dan Mikro Terhadap Kejadian Stunting Pada BalitaDemsa SimbolonNo ratings yet
- Vitamin D and CalciumDocument33 pagesVitamin D and CalciumAkhmadRoziNo ratings yet
- APA Reply HofferDocument128 pagesAPA Reply HofferVictoria VictoriaNo ratings yet
- Agriculture, biotech, bioethics challenges of globalized food systemsDocument28 pagesAgriculture, biotech, bioethics challenges of globalized food systemsperoooNo ratings yet
- Eneza Ujumbe: The Voices of Mathare YouthDocument4 pagesEneza Ujumbe: The Voices of Mathare YouthakellewagumaNo ratings yet
- Chronic Liver Disease and CirrhosisDocument5 pagesChronic Liver Disease and Cirrhosisaqil ithninNo ratings yet
- Medical BacteriologyDocument108 pagesMedical BacteriologyTamarah YassinNo ratings yet
- Package Pricing at Mission Hospital IMB527 PDFDocument9 pagesPackage Pricing at Mission Hospital IMB527 PDFMasooma SheikhNo ratings yet
- PT Behavioral ProblemsDocument11 pagesPT Behavioral ProblemsAmy LalringhluaniNo ratings yet
- MR T Balakrishnan PDFDocument19 pagesMR T Balakrishnan PDFvinnyNo ratings yet
- Maximizing NICU Care Through Cost-Effective TechnologiesDocument29 pagesMaximizing NICU Care Through Cost-Effective TechnologiesVonrey Tiana73% (11)
- CV FormatDocument1 pageCV FormatpanchodomNo ratings yet
- FAMILY DEVELOPMENTAL SESSIONS ON Healthy Lifestyle and NutritionDocument66 pagesFAMILY DEVELOPMENTAL SESSIONS ON Healthy Lifestyle and NutritionMariaLea Serrano AlmosuraNo ratings yet
- What is hepatitis B virus infection and how is it treatedDocument2 pagesWhat is hepatitis B virus infection and how is it treatedVictor Iv MirandaNo ratings yet
- BHS INGGRIS Proper Hand WashingDocument11 pagesBHS INGGRIS Proper Hand WashingAfifa RahmahNo ratings yet
- First Aid in Orthopedic PatientDocument17 pagesFirst Aid in Orthopedic PatientDrRajkumar PatelNo ratings yet