Professional Documents
Culture Documents
Acrf C
Uploaded by
Hussain AzharOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acrf C
Uploaded by
Hussain AzharCopyright:
Available Formats
BY DR ANUM YAQOOB H.
O MED-4
Acute renal failure (ARF), or acute kidney injury (AKI), as it is now referred to in the literature, is defined as an abrupt or rapid decline in renal filtration function. This condition is usually marked by a rise in serum creatinine concentration or by azotemia (a rise in blood urea nitrogen [BUN] concentration)
However, immediately after a kidney injury, BUN or creatinine levels may be normal, and the only sign of a kidney injury may be decreased urine production
AKI may be classified into 3 general categories, as follows: Prerenal - as an adaptive response to severe volume depletion and hypotension, with structurally intact nephrons Intrinsic - in response to cytotoxic, ischemic, or inflammatory insults to the kidney, with structural and functional damage Postrenal - from obstruction to the passage of urine While this classification is useful in establishing a differential diagnosis, many pathophysiologic features are shared among the different categories.
In 2004, the Acute Dialysis Quality Initiative work group set forth a definition and classification system for acute renal failure, described by the acronym RIFLE (Risk of renal dysfunction, Injury to the kidney, Failure or Loss of kidney function, and End-stage kidney disease. Investigators have since applied the RIFLE System to the clinical evaluation of AKI, although it was not originally intended for that purpose. AKI research increasingly uses RIFLE.
Stage Risk
GFR** Criteria SCreat increased 1.5
Urine Output Criteria UO < 0.5 mL/kg/h 6 h
Probability High sensitivity (Risk >Injury >Failure)
or
GFR decreased >25%
Injury
SCreat increased 2
or
GFR decreased >50%
UO < 0.5 mL/kg/h 12 h
Failure
SCreat increased 3
or
GFR decreased 75%
UO < 0.3 mL/kg/h 24 h (oliguria)
or
SCreat 4 mg/dL; acute rise 0.5 mg/dL
or
anuria 12 h
Loss ESKD*
Persistent acute renal failure: complete loss of kidney function >4 wk Complete loss of kidney function >3 mo
High specificity
Note: Patients can be classified by GFR criteria and/or UO criteria. The criteria that support the most severe classification should be used. The superimposition of acute on chronic failure is indicated with the designation RIFLE-FC; failure is present in such cases even if the increase in SCreat is less than 3-fold, provided that the new SCreat is greater than 4.0 mg/dL (350 mol/L) and results from an acute increase of at least 0.5 mg/dL (44 mol/L).
The driving force for glomerular filtration is the pressure gradient from the glomerulus to the Bowmans space. Glomerular pressure is primarily dependent on renal blood flow (RBF) and is controlled by combined resistances of renal afferent and efferent arterioles
Prerenal failure - Defined by conditions with normal tubular and glomerular function; GFR is depressed by compromised renal perfusion Intrinsic renal failure - Includes diseases of the kidney itself, predominantly affecting the glomerulus or tubule, which are associated with release of renal afferent vasoconstrictors; ischemic renal injury can ultimately leads to intrinsic renal failure b/c of the death of tubular cells and is the most common cause.
A physiologic hallmark of ATN is a failure to maximally dilute or concentrate urine (isosthenuria). The injured kidney fails to generate and maintain a high medullary solute gradient, because the accumulation of solute in the medulla depends on normal distal nephron function. (Failure to excrete concentrated urine even in the presence of oliguria is a helpful diagnostic clue in distinguishing prerenal from intrinsic renal disease; in prerenal azotemia, urine osmolality is typically more than 500 mOsm/kg, whereas in intrinsic renal disease, urine osmolality is less than 300 mOsm/kg.)
Postobstructive renal failure - Initially causes an increase in tubular pressure, decreasing the filtration driving force; this pressure gradient soon equalizes, and maintenance of a depressed GFR is then dependent on renal efferent vasoconstrictionwhich ultimately fails.
PRE RENAL AKI: Volume depletion which can result from: Renal losses (diuretics, polyuria) GI losses (vomiting, diarrhea) Cutaneous losses (burns, Stevens-Johnson syndrome) Hemorrhage Pancreatitis
DECREASED CARDIAC OUTPUT: Heart failure Pulmonary embolus Acute myocardial infarction Severe valvular disease Abdominal compartment syndrome (tense ascites
SYSTEMIC VASODILATION: Sepsis Anaphylaxis Anesthetics Drug overdose AFFERENT ARTEIOLAR VASOCONSTRICTION: Hypercalcemia Drugs (NSAIDs, amphotericin B, norepinephrine, radiocontrast agents) Hepatorenal syndrome
INTRINSIC RENAL DISEASE:(VASCULAR CAUSES) Renal artery obstruction (throm bosis, emboli, dissection, vasculitis) Renal vein obstruction (thrombosis) Microangiopathy (TTP, HUS, disseminated intravascular coagulation [DIC], preeclampsia) Malignant hypertension Scleroderma renal crisis Transplant rejection Atheroembolic disease
GLOMERULAR CAUSES: Anti-glomerular basement membrane (GBM) disease (Goodpasture syndrome) Anti-neutrophil cytoplasmic antibodyassociated glomerulonephritis (ANCAassociated GN) (Wegener granulomatosis, Churg-Strauss syndrome, microscopic polyangiitis) Immune complex GN (lupus, postinfectious, cryoglobulinemia, primary membranoproliferative glomerulonephritis)
TUBULAR CAUSES: Heme pigment (rhabdomyolysis, intravascular hemolysis) Crystals (tumor lysis syndrome, seizures, ethylene glycol poisoning, megadose vitamin C, acyclovir, indinavir, methotrexate) Drugs (aminoglycosides, lithium, amphotericin B, pentamidine, cisplatin, ifosfamide, radiocontrast agents)
INTERSTITIAL CAUSES: Drugs (penicillins, cephalosporins, NSAIDs, proton-pump inhibitors, allopurinol, rifampin, indinavir, mesalamine, sulfonamides) Infection (pyelonephritis, viral nephritides) Systemic disease (Sjgren syndrome, sarcoid, lupus, lymphoma, leukemia, tubulonephritis, uveitis)
Ureteric obstruction (stone disease, tumor, fibrosis, ligation during pelvic surgery) Bladder neck obstruction (benign prostatic hypertrophy [BPH], cancer of the prostate [CA prostate or prostatic CA], neurogenic bladder, tricyclic antidepressants, ganglion blockers, bladder tumor, stone disease, hemorrhage/clot) Urethral obstruction (strictures, tumor, phimosis) Intra-abdominal hypertension (tense ascites) Renal vein thrombosis
Retroperitoneal tumor, retroperitoneal fibrosis (methysergide, propranolol, hydralazine), urolithiasis, or papillary necrosis.
A detailed and accurate history is crucial to the diagnosis of the type of acute kidney injury (AKI) that a patient has and to determining the diseases subsequent treatment. Distinguishing AKI from chronic renal failure is important, yet making the distinction can be difficult. A history of chronic symptoms fatigue, weight loss, anorexia, nocturia, and pruritussuggests chronic renal failure
Nephrotoxic drug ingestion History of trauma or unaccustomed exertion Blood loss or transfusions Evidence of connective tissue disorders or autoimmune diseases Exposure to toxic substances, such as ethyl alcohol or ethylene glycol Exposure to mercury vapors, lead, cadmium, or other heavy metals, which can be encountered in welders and miners
Hypertension Congestive cardiac failure Diabetes Multiple myeloma Chronic infection Myeloproliferative disorder
Urine output history can be useful. Oliguria generally favors AKI. Abrupt anuria suggests acute urinary obstruction, acute and severe glomerulonephritis, or embolic renal artery occlusion. A gradually diminishing urine output may indicate a urethral stricture or bladder outlet obstruction due to prostate enlargement.
Patients commonly present with symptoms related to hypovolemia, including thirst, decreased urine output, dizziness, and orthostatic hypotension. Elders with vague mental status change are commonly found to have prerenal or normotensive ischemic AKI. Ask about volume loss from vomiting, diarrhea, sweating, polyuria, or hemorrhage. Patients with advanced cardiac failure leading to depressed renal perfusion may present with orthopnea and paroxysmal nocturnal dyspnea. Insensible fluid losses can result in severe hypovolemia in patients with restricted fluid access and should be suspected in elderly patients and in comatose or sedated patients.
Intravascular volume depletion
Altered Intrarenal hemodynamics
Etiologies of Pre renal ARF
Decreased effective arterial blood volume
Abdominal Compartment Syndrome
Nephritic syndrome of hematuria, edema, and HTN indicates a glomerular etiology of AKI. Query about prior throat or skin infections.
ATN should be suspected in any patient presenting after a period of hypotension secondary to cardiac arrest, hemorrhage, sepsis, drug overdose, or surgery. A careful search for exposure to nephrotoxins should include a detailed list of all current medications and any recent radiologic examinations (ie, exposure to radiologic contrast agents). Pigment-induced AKI should be suspected in patients with possible rhabdomyolysis (muscular pain, recent coma, seizure, intoxication, excessive exercise, limb ischemia) or hemolysis (recent blood transfusion). Allergic interstitial nephritis should be suspected with fevers, rash, arthralgias, and exposure to certain medications, including NSAIDs and antibiotics.
GLOMERULAR
TUBULAR
Postrenal failure usually occurs in older men with prostatic obstruction and symptoms of urgency, frequency, and hesitancy. Patients may present with asymptomatic, high-grade urinary obstruction because of the chronicity of their symptoms. A history of prior gynecologic surgery or abdominopelvic malignancy often can be helpful in providing clues to the level of obstruction. Flank pain and hematuria should raise a concern about renal calculi or papillary necrosis as the source of urinary obstruction. Use of acyclovir, methotrexate, triamterene, indinavir, or sulfonamides implies the possibility of tubular obstruction by crystals of these medication
Skin Skin examination may reveal the following: Livido reticularis, digital ischemia, butterfly rash, palpable purpura - Systemic vasculitis Maculopapular rash - Allergic interstitial nephritis Track marks (ie, intravenous drug abuse) Endocarditis Petechiae, purpura, ecchymosis, and livedo reticularis provide clues to inflammatory and vascular causes of AK. Infectious diseases, TTP, DIC, and embolic phenomena can produce typical cutaneous changes.
Eyes Eye examination may reveal the following: Keratitis, iritis, uveitis, dry conjunctivae - Autoimmune vasculitis Jaundice - Liver diseases Band keratopathy (ie, hypercalcemia) - Multiple myeloma Signs of diabetes mellitus Signs of hypertension Atheroemboli (retinopathy) Evidence of uveitis may indicate interstitial nephritis and necrotizing vasculitis. Findings suggestive of severe hypertension, atheroembolic disease, and endocarditis may be observed on careful examination of the eyes.
Ears Ear examination may reveal the following: Hearing loss - Alport disease and aminoglycoside toxicity Mucosal or cartilage ulcerations - Wegener granulomatosis Cardiovascular system Cardiovascular examination may reveal the following: Irregular rhythms (ie, atrial fibrillation) Thromboemboli Murmurs - Endocarditis Increased jugulovenous distention, rales, S3 - CHF
Abdomen Abdominal examination may reveal the following: Pulsatile mass or bruit - Atheroemboli Costovertebral angle tenderness - Nephrolithiasis, papillary necrosis Pelvic, rectal masses; prostatic hypertrophy; distended bladder Urinary obstruction Limb ischemia, edema - Rhabdomyolysis Abdominal examination findings can be useful to help detect obstruction at the bladder outlet as the cause of renal failure, which may be due to cancer or an enlarged prostate. (P/R examination) The presence of tense ascites can indicate elevated intraabdominal pressure that can retard renal venous return and result in AKI. The presence of an epigastric bruit suggests renal vascular hypertension, which may predispose to AKI.
Pulmonary Pulmonary examination may reveal the following: Rales - Goodpasture syndrome, Wegener granulomatosis Hemoptysis - Wegener granulomatosis
The physical examination must include pulse rate and blood pressure recordings measured in the supine position and the standing position; close inspection of the jugular venous pulse; careful examination of the heart, lungs, skin turgor, and mucous membranes; and assessment for the presence of peripheral edema. In hospitalized patients, accurate daily records of fluid intake and urine output and daily measurements of patient weight are important. Hypovolemia leads to hypotension; however, hypotension may not necessarily indicate hypovolemia. Severe CHF may also cause hypotension. . Severe hypertension with renal failure suggests renovascular disease, glomerulonephritis, vasculitis, or atheroembolic disease.
Anuria (< 100 mL/d) - Urinary tract obstruction, renal artery obstruction, rapidly progressive glomerulonephritis, bilateral diffuse renal cortical necrosis Oliguria (100-400 mL/d) - Prerenal failure, hepatorenal syndrome Nonoliguria (>400 mL/d) - Acute interstitial nephritis, acute glomerulonephritis, partial obstructive nephropathy, nephrotoxic and ischemic ATN, radiocontrast-induced AKI, and rhabdomyolysis
Alcoholic Ketoacidosis Anemia, Sickle Cell Aneurysm, Abdominal CHF and Pulmonary Edema Diabetic Ketoacidosis Obstructive Uropathy GI Bleeding Protein Overloading Steroid Use
Renal Calculi Renal Failure, Chronic and Dialysis Complications Toxicity, Alcohols Urinary Obstruction Urinary Tract Infection Metabolic Acidosis
Blood Urea Nitrogen and Serum Creatinine CBC Peripheral Smear and Serology Urinalysis Urine Electrolytes Bladder Pressure Emerging Biomarkers Ultrasonography Nuclear Scanning Aortorenal Angiography Renal Biopsy.
Although increased levels of BUN and creatinine are the hallmarks of renal failure, the rate of rise is dependent on the degree of renal insult as well as on protein intake with respect to BUN. The ratio of BUN to creatinine is an important finding, because the ratio can exceed 20:1 in conditions in which enhanced reabsorption of urea is favored (eg, in volume contraction); this suggests prerenal acute kidney injury (AKI). BUN may be elevated in patients with GI or mucosal bleeding, steroid treatment, or protein loading.
Assuming no renal function, the rise in BUN over 24 hours can be roughly predicted using the following formula: 24-hour protein intake in milligrams X 0.16 divided by total body water in mg/dL added to the BUN value. Assuming no renal function, the rise in creatinine can be predicted using the following formulas: For males: weight in kilograms X [28 - 0.2(age)] divided by total body water in mg/dL added to the creatinine value For females: weight in kilograms X [23.8 - 0.17(age)] divided by total body water added to the creatinine value As a general rule, if serum creatinine increases to more than 1.5 mg/dL/d, rhabdomyolysis must be ruled out.
The peripheral smear may show schistocytes in conditions such as HUS or TTP. A finding of increased rouleaux formation suggests multiple myeloma, and the workup should be directed toward immunoelectrophoresis of serum and urine. The presence of myoglobin or free hemoglobin, increased serum uric acid level, and other related findings may help to further define the etiology of acute kidney injury (AKI). Serologic tests for antinuclear antibody (ANA), ANCA, antiGBM antibody, hepatitis, and antistreptolysin (ASO) and complement levels may help to include and exclude glomerular disease. Although serologic tests can be informative, the costs can be prohibitive if these tests are not ordered judiciously.
Findings of granular, muddy-brown casts are suggestive of tubular necrosis . The presence of tubular cells or tubular cell casts also supports the diagnosis of ATN. Often, oxalate crystals are observed in cases of ATN. Reddish brown or cola-colored urine suggests the presence of myoglobin or hemoglobin, especially in the setting of a positive dipstick for heme and no red blood cells (RBCs) on the microscopic examination. The dipstick assay may reveal significant proteinuria as a result of tubular injury. The presence of RBCs in the urine is always pathologic. Eumorphic RBCs suggest bleeding along the collecting system. Dysmorphic RBCs or RBC casts indicate glomerular inflammation, suggesting glomerulonephritis is present.
The presence of WBCs or WBC casts suggests pyelonephritis or acute interstitial nephritis. The presence of urine eosinophils is helpful in establishing a diagnosis but is not necessary for allergic interstitial nephritis to be present. The presence of eosinophils, as visualized with Wright stain or Hansel stain, suggests interstitial nephritis but can also be seen in urinary tract infections, glomerulonephritis, and atheroembolic disease. The presence of uric acid crystals may represent ATN associated with uric acid nephropathy. Calcium oxalate crystals are usually present in cases of ethylene glycol poisoning.
Urine electrolyte findings also can serve as valuable indicators of functioning renal tubules. The fractional excretion of sodium (FENa) is the commonly used indicator. However, the interpretation of results from patients in nonoliguric states, those with glomerulonephritis, and those receiving or ingesting diuretics can lead to an erroneous diagnosis. FENa can be a valuable test for helping to detect extreme renal avidity for sodium in conditions such as hepatorenal syndrome. The formula for calculating the FENa is as follows: FENa = (UNa/PNa) / (UCr/PCr) X 100 Calculating the FENa is useful in acute kidney injury (AKI) only in the presence of oliguria.
In patients with prerenal azotemia, the FENa is usually less than 1%. In ATN, the FENa is greater than 1%. Exceptions to this rule are ATN caused by radiocontrast nephropathy, severe burns, acute glomerulonephritis, and rhabdomyolysis. In the presence of liver disease, FENa can be less than 1% in the presence of ATN. On the other hand, because administration of diuretics may cause the FENa to be greater than 1%, these findings cannot be used as the sole indicators in AKI.
In patients who are receiving diuretics, a fractional excretion of urea (FEUrea) can be obtained, since urea transport is not affected by diuretics. The formula for calculating the FEUrea is as follows: FEUrea = (Uurea/Purea) / (UCr/PCr) X 100 FEUrea of less than 35% is suggestive of a prerenal state
An intra-abdominal pressure of less than 10 mm Hg is considered normal and suggests that abdominal compartment syndrome is not the cause of AKI. Patients with an intraabdominal pressure below 15-25 mm Hg are at risk for abdominal compartment syndrome, and those with bladder pressures above 25 mm Hg should be suspected of having AKI as a result of abdominal compartment syndrome.
A number of biomarkers are being investigated to risk stratify and predict acute kidney injury (AKI) in patients at risk for the disease. The reason for this is because creatinine is a late marker for renal dysfunction and, once elevated, reflects a severe reduction in GFR. The most promising biomarker to date is urinary neutrophil gelatinase-associated lipocalin (NGAL), which has been shown to predict AKI in children undergoing cardiopulmonary bypass surgery.
Renal ultrasonography is useful for evaluating existing renal disease and obstruction of the urinary collecting system. The degree of hydronephrosis does not necessarily correlate with the degree of obstruction. Mild hydronephrosis may be observed with complete obstruction if found early. Ultrasonographic scans or other imaging studies showing small kidneys suggest chronic renal failure
Doppler scans are useful for detecting the presence and nature of renal blood flow. Because renal blood flow is reduced in prerenal or intrarenal AKI, test findings are of little use in the diagnosis of AKI. However, Doppler scans can be quite useful in the diagnosis of thromboembolic or renovascular disease. Increased resistive indices can be observed in patients with hepatorenal syndrome.
Because of a marked delay in tubular excretion of radionuclide in prerenal disease and intrarenal disease, the value of these scans is limited
This can be helpful in establishing the diagnosis of renal vascular diseases, including renal artery stenosis, renal atheroembolic disease, and atherosclerosis with aortorenal occlusion, and in certain cases of necrotizing vasculitis (eg, polyarteritis nodosa).
A renal biopsy may also be indicated when renal function does not return for a prolonged period and a prognosis is required to develop long-term management. Acute cellular or humoral rejection in a transplanted kidney can be definitively diagnosed only by performing a renal biopsy.
Measures to correct underlying causes of acute kidney injury (AKI) should begin at the earliest indication of renal dysfunction. A large proportion of the renal mass is damaged before any biochemical evidence of renal dysfunction is appreciated, because the relationship between the GFR and the serum creatinine level is not linear, especially early in disease; the rise of serum creatinine may not be evident before 50% of the GFR is lost.
The Acute Renal Failure Trial Network (ATN) Study, completed in 2008, was designed to compare clinical outcomes between patients allocated to an intensive dose versus a less-intensive dose of renal replacement therapy.]No additional benefit (morbidity/mortality) was conferred to patients who received more intensive dialysis (either intermittent or continuous dialysis). The best evidence suggests that patients with dialysis-dependent AKI should receive at least 3 hemodialysis treatments per week with delivered Kt/V value of 1.2 or continuous hemodialysis (continuous venovenous hemodialysis or hemofiltration) of 20 mg/kg/h (prescribed).
Maintenance of volume homeostasis and correction of biochemical abnormalities remain the primary goals of treatment. Daily fluid intake should equal urinary output plus an additional 500ml to cover insensible loses. Fluid intake and urinary output should be measured and patient should be weighed daily. Furosemide can be used to correct volume overload when the patients are still responsive; this often requires high intravenous (IV) doses.
NSAIDS ACE inhibitors Radiocontrasts agents Aminoglycosides and other antibiotics Heavy metal preparations Chemotherapeutic Agents Similarly, all medications cleared by renal excretion should be avoided or their doses should be adjusted appropriately.
A prophylactic strategy shown to decrease the incidence of contrast nephropathy is the IV administration of fluids. Normal saline solution of 1 ml/kg/h administered 12 hours before the procedure and then 12 hours after the procedure is recommended. In patients who are at high risk for volume overload, isotonic NaHCO3 solution should be administered before and after the procedure. Another prophylactic agent, used with varying success, is N -acetylcysteine at a dosage of 1200 mg PO q12h. This is administered to high-risk patients the day before a contrast study is performed and is continued the day of the procedure. Diuretics, NSAIDs, and possibly ACEIs should be withheld near the time of the procedure.
Correcting severe acidosis with bicarbonate administration can be important as a bridge to dialysis. Hyperkalemia, which can be life-threatening, should be treated by decreasing the intake of potassium in diet or tube feeds, exchanging potassium across the gut lumen using potassium-binding resins, promoting intracellular shifts in potassium with insulin and dextrose solutions, and instituting dialysis.
Patients with ARF are at risk of intercurrent infection so regular clinical examination and microbial investigationas clinically indicated are required.
Dietary modulation is an important facet of the treatment of acute kidney injury (AKI). Salt and fluid restriction becomes crucial in the management of oliguric renal failure, wherein the kidneys do not adequately excrete either toxins or fluids. In the polyuric phase of AKI, potassium and phosphorus may be depleted, and patients require dietary supplementation and intravenous replacemen
Calculation of the nitrogen balance can be challenging, especially in the presence of volume contraction, hypercatabolic states, GI bleeding, and diarrheal disease. Critically ill patients should receive at least 1 g/kg/d protein intake but should avoid hyperalimentation, which can lead to an elevated BUN level and water loss resulting in hypernatremia.
If there is an obstruction of the urinary tract, relieve the obdtruction.If that is not possible urgent nephrostomy may be done.
Great controversy exists regarding the timing of dialysis. Dialysis, especially hemodialysis, may delay the recovery of patients with AKI. There seems to be no difference in outcome between the use of intermittent hemodialysis and continuous renal replacement therapy (CRRT), but this is currently under investigation. However, CCRT may have a role in patients who are hemodynamically unstable and who have had prolonged renal failure after a stroke or liver failure. Such patients may not tolerate the rapid shift of fluid and electrolytes caused during conventional hemodialysis. Although not frequently used, peritoneal dialysis can also technically be used in acute cases and probably is tolerated better hemodynamically than conventional hemodialysis.
Indications for dialysis in patients with AKI are as follows: Volume expansion that cannot be managed with diuretics Hyperkalemia refractory to medical therapy Correction of severe acid-base disturbances that are refractory to medical therapy Severe azotemia (BUN >80-100) Uremia
Pulmonary complications Pulmonary complications have been reported in approximately 54% of patients with AKI and are the single most significant risk factor for death in patients with AKI. Hypoxia commonly occurs during hemodialysis and can be particularly significant in the patient with pulmonary disease. This dialysisrelated hypoxia is thought to occur secondary to white blood cell (WBC) lung sequestration and alveolar hypoventilation.
Cardiovascular complications Cardiovascular complications (eg, congestive heart failure [CHF], myocardial infarction, arrhythmias, cardiac arrest) have been observed in as many as 35% of patients with AKI. Fluid overload secondary to oliguric AKI is a particular risk for elderly patients with little cardiac reserve. GI complications GI symptoms of nausea, vomiting, and anorexia are frequent complications of AKI and represent one of the cardinal signs of uremia. GI bleeding occurs in approximately one third of patients with AKI. Most episodes are mild, but GI bleeding accounts for 3-8% of deaths in patients with AKI.
Infectious complications Infections commonly complicate the course of AKI and have been reported to occur in as many as 33% of patients with AKI. Most common sites are pulmonary and urinary tracts. Infections are the leading cause of morbidity and death in patients with AKI. Various studies have reported mortality rates of 11-72% in infections complicating AKI. Neurologic complications Neurologic signs of uremia are a common complication of AKI and have been reported in approximately 38% of patients with AKI. Neurologic sequelae include lethargy, somnolence, reversal of the sleep-wake cycle, and cognitive or memory deficits.
This is indicated by a gradual return of urinary output and subsequent improvement in plasma biochemistry. Some patients primarily those with ATN or after relief of chronic obstruction develop a diuretic phase.This is due in part to the loss of medullary cocentration gradient which normally allows concentration of urine in the collecting duct.Not all patients have diuretic phase depending on the severity of renal damage and rate of recovery.
Renal recovery in most cases is not complete and that the kidneys remain vulnerable to nephrotoxic effects of all therapeutic agents. Therefore, agents with nephrotoxic potential are best avoided. Renal recovery is usually observed within the first 2 weeks, and many nephrologists tend to diagnose patients with end-stage (ie, irreversible) renal failure 6-8 weeks after the onset of acute kidney injury (AKI). It is always better to check these patients periodically, because some patients may regain renal function much later.
THANK YOU
You might also like
- Learning Issue: Acute Kidney InjuryDocument6 pagesLearning Issue: Acute Kidney InjuryAnnisa WidjanarkoNo ratings yet
- Inter'Medic AKIDocument48 pagesInter'Medic AKIMAHEJS HDNo ratings yet
- Acute Renal FailureDocument12 pagesAcute Renal FailureRifa Aprillia CahyaniNo ratings yet
- Acute Kidney InjuryDocument17 pagesAcute Kidney InjuryCha-cha UzumakiNo ratings yet
- Lecture 2. Acute Renal FailureDocument85 pagesLecture 2. Acute Renal FailurePharmswipe KenyaNo ratings yet
- Acute Kidney InjuryDocument8 pagesAcute Kidney InjuryRohitKumarNo ratings yet
- Renal Disease: Acute Kidney Injury (AKI)Document5 pagesRenal Disease: Acute Kidney Injury (AKI)api-142637023No ratings yet
- Lecture - Acute Renal FailureDocument57 pagesLecture - Acute Renal FailureJames StiltonNo ratings yet
- Acute Tubular Necrosis: Causes, Symptoms and DiagnosisDocument15 pagesAcute Tubular Necrosis: Causes, Symptoms and DiagnosisDeepak patelNo ratings yet
- Acute Kidney Injury and Chronic Kidney DiseaseDocument44 pagesAcute Kidney Injury and Chronic Kidney DiseaseshihochanNo ratings yet
- Current Concepts: Cute LiguriaDocument5 pagesCurrent Concepts: Cute Liguriakate blackNo ratings yet
- Acute Kidney InjuryDocument21 pagesAcute Kidney InjuryAtif Gazali100% (1)
- Acute Renal FailureDocument34 pagesAcute Renal Failureaibaloca67% (9)
- Acute Kidney InjuryDocument23 pagesAcute Kidney InjuryBaraka SayoreNo ratings yet
- Acute Kidney InjuryDocument20 pagesAcute Kidney InjuryTishya MukherjeeNo ratings yet
- Acute Kidney Injury - Chronic Kidney DeseaseDocument71 pagesAcute Kidney Injury - Chronic Kidney DeseaseFina Ahmad Fitriana100% (1)
- Acute Renal FailureDocument33 pagesAcute Renal FailureAqsa Akbar AliNo ratings yet
- Acute-Renal-Failure Lecture OnlyDocument17 pagesAcute-Renal-Failure Lecture OnlyeyesontheskyNo ratings yet
- Acute Kidney InjuryDocument62 pagesAcute Kidney InjuryIvan HensonNo ratings yet
- Acute Renal Failure DXDocument7 pagesAcute Renal Failure DXfarid akbarNo ratings yet
- Essential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsDocument5 pagesEssential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsRika Ariyanti SaputriNo ratings yet
- Acute Kidney Injury and Chronic Kidney DiseaseDocument44 pagesAcute Kidney Injury and Chronic Kidney DiseaseIda Bagus Putu Swabawa100% (1)
- College of Nursing: Civil HospitalDocument15 pagesCollege of Nursing: Civil HospitalDipal Jignesh PatelNo ratings yet
- Dr.P.Sankaranarayanan MD: Emeritus Professor of Medicine Acs Medical College & HospitalDocument81 pagesDr.P.Sankaranarayanan MD: Emeritus Professor of Medicine Acs Medical College & HospitalvaishnaviNo ratings yet
- Nephrologi NotesDocument43 pagesNephrologi NotesSigit Harya HutamaNo ratings yet
- Akd & CKDDocument44 pagesAkd & CKDﻣﻠﻚ عيسىNo ratings yet
- Renal Failure and Kidney DiseaseDocument41 pagesRenal Failure and Kidney Disease12046No ratings yet
- Acute Renal FailureDocument13 pagesAcute Renal FailureGlorianne Palor100% (2)
- Acute Kidney Injury: Prerenal Azotemia, Intrinsic Renal Parenchymal Disease, and Postrenal ObstructionDocument11 pagesAcute Kidney Injury: Prerenal Azotemia, Intrinsic Renal Parenchymal Disease, and Postrenal Obstructionnathan asfahaNo ratings yet
- Acute Kidney Injury: Hailemariam Bekele Hayelom MichaelDocument77 pagesAcute Kidney Injury: Hailemariam Bekele Hayelom MichaelShafira WidiaNo ratings yet
- Acute Kidney InjuryDocument21 pagesAcute Kidney InjuryLALITH SAI KNo ratings yet
- Renal Faliure 1Document50 pagesRenal Faliure 1180045No ratings yet
- Aetiology: Save Time & Improve Your PDP On Patient - Co.ukDocument9 pagesAetiology: Save Time & Improve Your PDP On Patient - Co.ukBaihaqi SaharunNo ratings yet
- Renal IndicesDocument6 pagesRenal IndicesSaravanan SridharanNo ratings yet
- Acute Renal Failure - Copy (2)Document38 pagesAcute Renal Failure - Copy (2)chesang507No ratings yet
- Perioperative Oliguria and ATNDocument22 pagesPerioperative Oliguria and ATNmhelmykhafagaNo ratings yet
- Acute Renal Failure: Dr. Sami Abdo RadmanDocument23 pagesAcute Renal Failure: Dr. Sami Abdo RadmanAdeniran CharlesNo ratings yet
- Acute Renal FailureDocument9 pagesAcute Renal FailureananNo ratings yet
- Acute and Chronic Kidney DiseaseDocument20 pagesAcute and Chronic Kidney DiseaseCabdi WaliNo ratings yet
- Failure, Is The Term Used To Encompass The Entire Range of TheDocument2 pagesFailure, Is The Term Used To Encompass The Entire Range of TheeceNo ratings yet
- Aki NotesDocument10 pagesAki NotesGennel Mae GarovilloNo ratings yet
- Nephrology: Omar K MRCP IrelandDocument54 pagesNephrology: Omar K MRCP IrelandManmeet SNo ratings yet
- Hepatorenal syndrome - UpToDateDocument38 pagesHepatorenal syndrome - UpToDateSantiago IllarramendiNo ratings yet
- Manajemen Anestesi Pada Uremic SyndromeDocument27 pagesManajemen Anestesi Pada Uremic SyndromeAdi Nugroho MelyanaNo ratings yet
- Hepatorenal Syndrome - Introduction and DiagnosisDocument38 pagesHepatorenal Syndrome - Introduction and DiagnosisbornflaxNo ratings yet
- Acute Kidney Injuri: Professor Ibrahim UmmateDocument46 pagesAcute Kidney Injuri: Professor Ibrahim UmmateElvis obajeNo ratings yet
- Acute Renal FailureDocument31 pagesAcute Renal FailureODONG MARTINNo ratings yet
- Acute Kidney InjuryDocument18 pagesAcute Kidney InjuryV RakeshreddyNo ratings yet
- Azotemia - StatPearls - NCBI BookshelfDocument1 pageAzotemia - StatPearls - NCBI Bookshelfmellinda anastasyaNo ratings yet
- Acute Renal Failure/ Gagal Ginjal Akut: Tunggul Adi P., M.SC., Apt. Lab Farmasi Klinik, Farmasi, FKIK, UNSOEDDocument27 pagesAcute Renal Failure/ Gagal Ginjal Akut: Tunggul Adi P., M.SC., Apt. Lab Farmasi Klinik, Farmasi, FKIK, UNSOEDPramita Purbandari100% (1)
- Coursematerial 136Document13 pagesCoursematerial 136Nyj QuiñoNo ratings yet
- Acute Kidney Injury Causes and TypesDocument9 pagesAcute Kidney Injury Causes and TypesKacey MandNo ratings yet
- Chronic Kidney DiseaseDocument6 pagesChronic Kidney Diseaseashi leginNo ratings yet
- Presented By: Sonia Dagar: Renal FailureDocument40 pagesPresented By: Sonia Dagar: Renal FailureRavanshi ThakurNo ratings yet
- Etiology and Diagnosis of Prerenal Disease and Acute Tubular Necrosis in Acute Kidney Injury in Adults - UpToDateDocument22 pagesEtiology and Diagnosis of Prerenal Disease and Acute Tubular Necrosis in Acute Kidney Injury in Adults - UpToDatecuentaparatrabajosdelau10No ratings yet
- Acute Kidney Injury (AKI) : Bagian Ilmu Penyakit Dalam Fku UnisbaDocument52 pagesAcute Kidney Injury (AKI) : Bagian Ilmu Penyakit Dalam Fku UnisbaIndrayudha PramonoNo ratings yet
- Acute Renal FailureDocument21 pagesAcute Renal Failureاحمد الهاشميNo ratings yet
- Pathogenesis and Management of Renal Failure and Replacement Therapy For Stage V Chronic Renal DiseaseDocument30 pagesPathogenesis and Management of Renal Failure and Replacement Therapy For Stage V Chronic Renal DiseaseByzantine Wulandari ParubakNo ratings yet
- Hepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Liver Function Test FinalDocument98 pagesLiver Function Test FinalHussain AzharNo ratings yet
- Dengue 2009Document53 pagesDengue 2009Hussain AzharNo ratings yet
- Anam FinalDocument82 pagesAnam FinalHussain AzharNo ratings yet
- Ion SyndromeDocument67 pagesIon SyndromeHussain AzharNo ratings yet
- Copd Final 97-2003hiraaDocument41 pagesCopd Final 97-2003hiraaHussain AzharNo ratings yet
- DVTDocument32 pagesDVTHussain AzharNo ratings yet
- Enteric FeverDocument63 pagesEnteric FeverHussain AzharNo ratings yet
- K HomeosDocument47 pagesK HomeosHussain AzharNo ratings yet
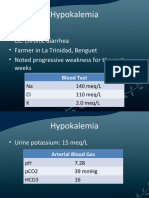
- HypokalemiaDocument12 pagesHypokalemiaMohammad AliNo ratings yet
- DVT&PE Final 1Document59 pagesDVT&PE Final 1Hussain AzharNo ratings yet
- EFFA PRESENTATNhepatic EncephalopathyDocument50 pagesEFFA PRESENTATNhepatic EncephalopathyHussain AzharNo ratings yet
- Case Presentation 2Document53 pagesCase Presentation 2Hussain AzharNo ratings yet
- Electrolyte Disturbaces - Hyponatremia and HypernatremiaDocument41 pagesElectrolyte Disturbaces - Hyponatremia and HypernatremiaMohammad AliNo ratings yet
- DVT - 2 FaizaDocument65 pagesDVT - 2 FaizaHussain AzharNo ratings yet
- DKA Concepts and ManagementDocument22 pagesDKA Concepts and ManagementMohammad AliNo ratings yet
- Dka 31-05-11Document52 pagesDka 31-05-11Hussain AzharNo ratings yet
- Approach To Unconsious PTDocument62 pagesApproach To Unconsious PTHussain AzharNo ratings yet
- Case Presentation ParaplegiaDocument51 pagesCase Presentation ParaplegiaHussain Azhar100% (2)
- Asthma: Presentation By: Dr. Zunaira Nawaz Dr. Nida ShafiqueDocument47 pagesAsthma: Presentation By: Dr. Zunaira Nawaz Dr. Nida ShafiqueMohammad AliNo ratings yet
- AntibioticsDocument49 pagesAntibioticsHussain AzharNo ratings yet
- CP Najma 97Document75 pagesCP Najma 97Hussain AzharNo ratings yet
- Case Presentation Hypokalemic ManDocument61 pagesCase Presentation Hypokalemic ManHussain AzharNo ratings yet
- AnemiaDocument37 pagesAnemiaHussain AzharNo ratings yet
- An Approach To Anemic PatientDocument79 pagesAn Approach To Anemic PatientHussain AzharNo ratings yet
- AKIDocument83 pagesAKIHussain AzharNo ratings yet
- Dr. Adeel Ahmed Waheed: House Officer M-4Document84 pagesDr. Adeel Ahmed Waheed: House Officer M-4Hussain AzharNo ratings yet
- Acute Renal FailureDocument120 pagesAcute Renal FailureHussain AzharNo ratings yet
- ABG S Final and Last TouchDocument88 pagesABG S Final and Last TouchHussain AzharNo ratings yet
- Acute Exacerbation of COPDDocument14 pagesAcute Exacerbation of COPDMohammad AliNo ratings yet
- Chapter 6 CMDocument14 pagesChapter 6 CMLeilani SablanNo ratings yet
- RenalDocument81 pagesRenalandreaNo ratings yet
- Kidney Function Test Essentials HandbookDocument66 pagesKidney Function Test Essentials HandbookVesna Danity100% (1)
- Proteinuria in Adults - A Diagnostic Approach - American Family PhysicianDocument7 pagesProteinuria in Adults - A Diagnostic Approach - American Family PhysicianDr Sumant SharmaNo ratings yet
- Rationale PQ 1Document12 pagesRationale PQ 1ChaNo ratings yet
- Kidney MCQDocument14 pagesKidney MCQNikita Nanwani85% (34)
- Hippo EM Board Review - Renal & GU Written SummaryDocument15 pagesHippo EM Board Review - Renal & GU Written Summarykaylawilliam01No ratings yet
- TextDocument10 pagesTextNIÑA NICOLE PACAMARRANo ratings yet
- UrinalysisDocument15 pagesUrinalysisarchivos primeroNo ratings yet
- AUBF - Module 4Document48 pagesAUBF - Module 4Crisostomo ChelseaNo ratings yet
- Urine Analysis FinalDocument112 pagesUrine Analysis FinalNischita JayarajNo ratings yet
- Hematology India: QuestionsDocument22 pagesHematology India: QuestionsSelim TarekNo ratings yet
- Urine-Sediment-Guide IDEXX PDFDocument2 pagesUrine-Sediment-Guide IDEXX PDFDani Marins0% (1)
- Aubf Mid PPT Topic 2 (Part 2)Document12 pagesAubf Mid PPT Topic 2 (Part 2)Lovely B. AlipatNo ratings yet
- 5 Must To Know in Clinical Micros PDFDocument43 pages5 Must To Know in Clinical Micros PDFYelai CarveroNo ratings yet
- Urinalysis in The Diagnosis of Kidney DiseaseDocument94 pagesUrinalysis in The Diagnosis of Kidney DiseasegibreilNo ratings yet
- Giovanni Fogazzi. The Urinary Sediment. Third EditionDocument269 pagesGiovanni Fogazzi. The Urinary Sediment. Third EditionFco_Sandoval12100% (9)
- AUBF Group 1 Chapter 8Document12 pagesAUBF Group 1 Chapter 8Gerald John PazNo ratings yet
- Lab Final Exam ReviewDocument59 pagesLab Final Exam ReviewManju ShreeNo ratings yet
- Urine Routine Examination: M133207 Id NoDocument1 pageUrine Routine Examination: M133207 Id NoMahia RahmanNo ratings yet
- PSGNPPTDocument70 pagesPSGNPPTJirran CabatinganNo ratings yet
- Aubf MergeDocument164 pagesAubf MergeVia Gail CanlasNo ratings yet
- Acute Kidney InjuryDocument8 pagesAcute Kidney InjuryRohitKumarNo ratings yet
- MCQs For Lab.Document10 pagesMCQs For Lab.Sami Khan86% (43)
- Urinalysis PDFDocument34 pagesUrinalysis PDFAzeli SiquianNo ratings yet
- DAPHNE'S HW CHAPTERS 4-6Document15 pagesDAPHNE'S HW CHAPTERS 4-6Christian Miguel Avila AustriaNo ratings yet
- Urinalysis Chapter 5Document178 pagesUrinalysis Chapter 5Sanket GuptaNo ratings yet
- Urine sediment atlas guide for identifying crystals in cat and dog urine samplesDocument2 pagesUrine sediment atlas guide for identifying crystals in cat and dog urine samplesbnsvet6242100% (1)
- Aubf - CastsDocument4 pagesAubf - CastsAngela LaglivaNo ratings yet
- Study Questions: CHAPTER 8 Microscopic Examination of Urine SedimentDocument7 pagesStudy Questions: CHAPTER 8 Microscopic Examination of Urine SedimentTiara YantaNo ratings yet