Professional Documents
Culture Documents
Antibiotics
Uploaded by
Nandini GulurOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antibiotics
Uploaded by
Nandini GulurCopyright:
Available Formats
PRINCIPLES OF
ANTIBIOTICS
BY,
MUEEDUL ISLAM
CONTENTS
Definition of antibiotics
Introduction & history
Various terminologies
Oral microbial flora
Classification of antibiotics
Principles of antibiotic administration
Avoiding resistance to antibiotics
Therapeutic uses of antibiotics in OMFS.
Prophylactic antibiotics
Individual drugs
References
Definition:-
Antibiotics are substances
produced by microorganisms which
supress or kill the other microorganisms at
very low concentrations.
Walksman defined an antibiotic as a
chemical substance produced by
microorganisms having the property of
inhibiting the growth of or destroying other
microorganisms in high dilution.
INTRODUCTION AND HISTORY
IClinical potential oI microbial products as therapeutic agents in
1877 Pasteur and Joubert
IPenicillin discovery 1929
I1941 penicillin was commercilly available, golden age oI
antibiotics
IChlortetracycline- introduced in 1948 |Ior rickettsial inIections|
$ir Alexander Fleming's early work on PENCLLN which
became the first "miracle drug and hence innumerable lives
have been saved.
-Paul Ehlrich coined the term chemotherapy.He showed that
certain dyes can destroy microbes.
VARIOUS TERMINOLOGIES
IPharmacology
IChemotherapy
IANTIBIOTICS
IMINIMAL INHIBITORY CONCENTRATION(MIC)
IBACTERIOSTATIC
IBACTERIOCIDAL
IGenerations of a drug
Oral microbial Ilora
W AEROBIC BACTERIA
W Gram-positive cocci-
W Staphylococci sp
W Streptococci sp
W Anginosus sp
W Enterococcus sp [endodontic infections]
W Gram-negative cocci
W Neisseria
W Gram positive rods-
W Bacterionema
W Diptheroids
W Lactobacillus sp
W Gram-negative rods and coccobacilli-
W Actinobacillus actinomycetiescomitans
W Campilobacter sp
W Eiknella corridans
W Helicobacter pylori
W Capnocytophaga
Anaerobic bacteria -
Cram negative rods-
Bacteroids sp
Fusobacterium sp
Porphyromonas sp
Prevotella sp
Centipedia periodontii
Leptotrichia buccalis
Selenomonas sp
Gram negative cocci-
Veillonella sp
Gram-positive rods-
Actinomyces sp
BiIidobacterium dentium
Eubacterium sp
Gram positive cocci-
Peptococcus sp
Peptostreptococcus sp
CLA$$FCATON:-
t can be classified as:-
A)Chemical structure:-
-sulphonamides & related drugs-sulfadiazine & others.
-Diamino Pyrimidines-Trimethoprim,Pyrimethamine.
-Quinalones-Nalidixic acid,Norfloxacin,Ciprofloxacin.
-B-Lactum antibiotics-
Penicillins,Cephalosporins,Monobactums,Carbapenims
-Tetracyclines-Oxytetracyclines,Doxycycline.
-Nitrobenzene derivative-Chloramphenicol.
-Aminoglycosides-$treptomycin,Gentamycin,Neomycin.
-Macrolide Antibiotics-Erythromycin,Roxithromycin,Azithromycin.
-Polypeptide antibiotics-Polymyxin B,bacitracin,Tyrothricin
-Glycopeptides-Vancomycin,Teicoplanin.
-Oxazolidinone-Linezoline
-Nitroimidazoles-Metranidazole,Tinidazole.
-Nicotinic Acid derivatives-soniazid,Pyrazinamide.
B)Mechanism of Action:-
-nhibit cell wall synthesis-
Penicillins,cephalosporins,Cyclosporins,vancomycin,Bacitracn.
-Causes leakage from cell membranes-Polypeptides,Polyenes.
-nhibits protein synthesis-
Tetramycin,Erythromycin,Clindamycin,Chloramphenicol.
-Causes misreading of mRNA code & affects permeability-Aminoglycosides-
$treptomycin,Gentamycin.
-nhibits DNA gyrase-Fluroquinalones-Ciprofloxacin
-nterferes with DNA function-Rifampin,Metronidazole.
-nterferes with DNA synthesis-Acyclovir,Zidovudine.
-nterferes with intermediary Metabolism-$ulphanomides,Trimethoprim.
C)Type of organism against which Primarily active:-
-Antibacterial-Penicillins,Aminoglycosides,Erythromycin.
-Antifungal-Griseofulvin,AmphotericinB,Ketacanazole.
-Antiviral-Acyclovir,Amantedine,Zidovidine
-Antiprotozoal-Chloroquine,Pymithamine
-Antihelminthic-Mebendazole,Pyrantel
D)$pectrum of Activity:-
-Narrow spectrum-
PenicillinG,$pectromycin,Erythromycin.
-ntermediate spectrum-extended
spectrum
Penicillins,Cephalosporins,Aminoglyco
sides,Fluroquinalones.
-Broad spectrum-
Tetracyclines,Chloramphenical.
E)Type of Action:-
-Primarily Bacteriostatic-
$ulphanomides,Tetracyclines,Chlorampheni
col,Erythromycin,Ethambutol,Clindamycin.
-Primarily Bactiricidal-
Penicillin,Aminoglycosides,Rifampin,Cotrima
xazole,Vancomycin,Metranidazole.
F)Antibiotics are obtained from:-
-Fungi-Penicillin,Cephalosporins,Griseofulvins.
-Bacteria-PolymixinB,Colistin,Bacitracin.
-Actinomycetes-
Aminoglycosides,Tetracyclines,
Chloramphenicol.
CLASSIFICATION OF PENICILLIN
1) Natural penicillins :
Penicillin G (Benzyl penicillin),porcain penicillin-g,
benzathine penicillin.
2) Semisynthetic penicillin-
a.Acid resistant penicillins :
Phenoxymethyl penicillin (penicillin V)
b.Penicillinase - resistant penicillins :
Acid labile : Methicillin, nafillin, cloxacillin, dicloxacillin
Acid resistant: flucloxacillin.
c.Extended spectrum penicillins :
a.Carboxypenicillins : Carbenicillin, ticarcillin,
b. Aminopenicillin : Amipicillin, amoxicilllin.
c. Ureidopenicillin : Mezlocillin, piperacillin.
4. Beta lactamase inhibitors : Clavulanic acid, Sulbactum.
ON DURATION OF ACTION
Short acting-Procain benzyl penicillin|1-3hr|
Intermediate acting-FortiIied Benzyl penicillin |12-24 hr|
Long acting- Benzathine penicillin |12- 15 days|
cephalosporins
First generation-
Parenteral-
Cephalothin
CeIazolin
Cephaloridine
Oral-
Cephalexin
Cephadine
CeIadroxil
ore active against gram
positive organism
Second generation- more active against gram positive
and gram negative organisms
Parenteral-
CeIuroxim
CeIoxitin
ral
CeIaclor
CeIuroxim axetal
%ird generation-
Parenteral-
CeIotaxim
CeItizoxime
CeItraxone
CeIoperazone
Oral-
ceIexim
Higly active against gram
negative otganisms
W ourth generation- similar antibacterial activity as
that 0f third generation but highly resistant to beta
lactamases
Parenteral-
ceIepime
ceIiperome
Broad spectrum antibiotics-
Tetracycline; chloramphenicol
Group I-
Chlortetracycline
Tetracycline
Oxytetracycline
Group II-
Demeclocycline
Lymicyline
Grope III-
Doxycycline
Minocycline
Anti-Iungal antibiotics
polyenes-
Amphotricine B, nystatin, hamycin,natamycin
B. heyerocyclic benzoIuran-
GriseoIulvin
PRINCIPLES OF
ANTIBIOTIC THERAPY:-
Principles oI appropriate antibiotic use:-
A)Presence of infection:
Locally the classic signs & symptoms oI pain,swelling,pus Iormation
and limitation oI motion.
NoninIectious conditions similar to the inIectious conditions to be
careIully diagnosed are:
-painIul tooth.
-removal oI 3
rd
molar
-major Maxillo-Iacial procedures perIormed under GA
S%% HS% DSS:
Antibiotics help in situations in which the host has been overwhelmed by
bacteria or especially virulent bacteria are involved, and when patient`s
deIenses are impaired.
Cause oI depressed deIense:
1) Physiological: shock, disturbances in circulation caused in old ages or
obesity and Iluid imbalances.
2) Disease related: malnutrition syndrome (alcoholism), cancers, leukemia,
poorly controlled diabetics.
3) DeIective immune system related: congenital deIects such as
agammaglobulinemia,
Multiplemyeloma, total body irradiation therapy, children who have had
splenectomy.
4) Drug suppression related:
cytotoxic drugs in malignancies, glucocorticoids, cyclosporine.
C) SURGICAL DRAINAGE AND INCISION
Surgical intervention is necessary in both chronic abscess &
acute indurated cellulites.
Many inIections demonstrated both abscess Iormation &
indurated cellulites. In such situations incision & drainage oI the
abscesss result in reduction oI pressure in the area oI cellulitis.
D) THE DECISION TO USE ANTIBIOTIC
THERAPY.
When the clinician is conIronted with a
patient with a possible inIection, each oI the
proceeding Iactors must be weighed careIully.
Only then can an appropriate decision be
made about whether antibiotic therapy is
necessary.
PRINCIPLES FOR CHOOSING THE APPROPRIATE ANTIBIOTIC
Once the decision has been made to use antibiotics as an adjunct to treating
an inIection, the antibiotic should be properly selected.
Some oI the guide lines which can be helpIul in antibiotic selection are:
IDENTIFICATION OF CAUSATIVE ORGANISM:
The typical odontogenic inIection is caused by a mixture oI aerobic and
anaerobic bacteria.
Approximately 70-mixed Ilora
5-pure aerobic
25-pure anaerobic
DETERMINATION OF ANTIBIOTIC
SENSITIVITY
In the treatment oI an inIection that has not
responded to initial antibiotic therapy or a post
op wound inIection, the causative agent must be
precisely identiIied, and the antibiotic sensitivity
must also be determined.
The results oI this provide inIormation needed
to prescribe most appropriate antibiotic.
USE OF SPECIFIC AND NARROW
SPECTRUM ANTIBIOTICS
Antibiotic with the narrowest spectrum oI activity should be
used, which will prevent the development oI resistant organisms.
When broad spectrum antibiotics are used, many diIIerent
bacteria also present in the body are exposed to antibiotic.
But in the case oI narrow spectrum antibiotics only Iewer
organisms have opportunity to become resistant.
Use oI narrow spectrum antibiotics also minimizes the risk oI
supra inIections
PATIENTS DRUG HISTORY
Previous allergic reactions
Previous toxic reactions
Any medication in use
BACTERICIDAL RATHER THAN A BACTERIOSTATIC
DRUG
Bactericidal - immunocompromised conditions.
Bacteriostatic- less chance oI superinIection
USE OF SPECIFIC, NARROW-SPECTRUM ANTIBIOTIC
Narrow spectrum antibiotic
Decreases resistance, decreases superinIections
MINIMAL INHIBITORY CONCENTRATION (MIC)
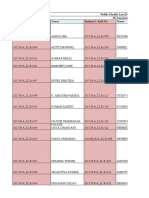
Penicillin G Penicillin V Oxacillin Cefazolin Cephalexin
Streptococcus 0.005 0.015 0.02 0.2 1.0
Staphylococcus (non-penicillinase) 0.03 0.03 0.3 0.6 6.0
Staphylococcus (penicillinase) R R 0.4 0.6 6.0
Penicillin G Erythromycin Clindamycin Metronidazole
Bacteroides oralis 1.6 0.1 0.1 2.8
Bacteroides melaninogenicus 1.0 0.4 0.01 3.0
Bacteroides Iragilis R 2.0 0.2 3.1
Cefazolin Cephalexin Gentamicin
Escherichia coli 0.8 12.0 2.0
Proteus mirabilis 3.0 20.0 1.0
Klebsiella pneumoniae 3.0 20.0 1.5
Pseudomonas aeruginosa ~ 400.0 ~ 100.0 1.5
Dosage
On basis oI body weight-
Individual dose
ody weigt[kgj
70
X average adult dose
Young`s Iormula-
Child dose
ge
ge+12
X adult dose
Dilling`s Iormula
Child dose
ge
2
X dult dose
n basis of age -
MAXIMUM DOSAGE FOR LIFE-THREATENING INFECTIONS
6 2 g Vancomycin
8 3-6 mg/kg Tobramycin
6 2 g Tetracycline
4 10-12 x 10
6
U Penicillin G
4-6 8-12 g Oxacillin
8 21 mg/kg Metronidazole
6 2-4 g Erythromycin
8 3-6 mg/kg Gentamicin
6 2-5 g Clindamycin
6 50 mg/kg Chloramphenicol
4 8-12 g Cephalothin
4 6-12 g CeIoxitin
6 4-8 g
CeIazolin
4 6-12 g CeIamandole
4 24-40 g Carbenicillin
4 12 g/day Ampicillin
8 15-25 mg/kg Amikacin
" Dosage interval (hr) Total daily dosage Antibiotic
PEDIATRIC DOSAGES OF COMMONLY USED ANTIBIOTICS
Drug
Daily dosage
Amoxicillin
20-25 mg/kg/day PO in 3 doses
Ampicillin
25-50 mg/kg/day PO, IM or Iv in 4 doses
Cephalothin
80-160 mg/kg/day PO, IM or IV in 6 doses
Cephalexin
25-50 mg/kg/day PO in 4 doses
Chloramphenicol
75-100 mg/kg/day IV in 4 doses
Clindamycin
10-20 mg/kg/day PO, IM, or IV in 3-4 doses
Cloxacillin
50-100 mg/kg/day PO in doses
Dicloxacillin
12.5-50 mg/kg/day PO in 2 doses
Doxycycline
5.0 mg/kg/day PO in 2 doses
Erythromycin
30-50 mg/kg/day PO in 4 doses
Gentamicin
6.0 mg/kg/day IM in 3 doses
Metronidazole
30-40 mg/kg/day PO
Minocycline
4.0 mg ist day, then 4.0 mg/kg/day in 2 doses
Penicillin G
100,000 U/kg day IM or IV in 3 doses
Penicillin V
50 mg/kg/day PO in 3-4 doses
Streptomycin
20-40 mg/kg/day IM in 3 doses
Tobramycin
3-5 mg/kg/day IM in 3 doses
Vancomycin
50 mg/kg/day IV in 4 doses
TOXIC effects of ANTIBIOTIC
Some antibiotic kill / injure human cells
Penicillin
Amphotericin B
" Cephaloridine
" Aminoglycosides
" Renal urinary system
Hepatitis Erythromycin
Pseudomembranous colitis
Diarrhea Clindamycin
Hepatitis Tetracycline
" Gastrointestinal system
Vertigo Vancomycin
Myoclonic seizures Penicillin and cephalosporin
Vertigo gentamicin
DeaIness tobramycin
" Nervous system
Decreased platelet aggregation Carbenicillin (and ticarcillin)
Leukopenia
Aplastic anemia Chloramphenicol
" Hematologic
" PROBLEM " ANTIBIOTIC
tubular necrosis
Antibiotic-associated colitis (AAC)
Clindamycin, ampicilin-amoxicillin
Cephalosporins
Clinical Ieatures
Watery diarrhea
Cramping abdominal pain, Iever and leukocytosis
Treatment :To discontinue the causative antibiotic, restore Iluid
and electrolyte balance and administer anti-clostridia antibiotics
like the usual choice is oral vancomycin, metronidazole
Superinfection :
When the normal Ilora is altered or eliminated by an antibiotic, the
pathogenic bacteria resistant to the antibiotic may cause a secondary
inIection or superinIection.
Eg: overgrowth oI Candida in the oral cavity
The use oI broad-spectrum antibiotics results in decreased normal
host Ilora
Seen in the Iorm oI bacteremia, U T I, pneumonia owing to the over
growth oI resistent micro-organisms- lebicella, erobacter,
Pseudomonas, Candida
ral signs- stomatitis, glossitis, black airy tongue[stapylococci,
streptococci, bacteroids, candidaj
UNFAVORABLE DRUG INTERACTIONS
Antibiotic
Other drug Effect
Aminglycoside Ethacrynic acid Increased ototoxicity
Cephaloridine Ethacrynic acid
Nephrotoxicity
Furosemide
Tetracycline Coumarin
Increased anticoagulation
Tetracycline Antacids
Absorption inhibited
Bactericidal antibiotic Bacteriostatic antibiotic
Decreased eIIectiveness
ampicillin Estrogen-containing birth
control pills
Decreased eIIectiveness oI
birth control pills
CLINICAL APPLICATION
Antibiotics in medically compromised.
Renal failure :
No major adjustments Cephalexin
Chloramphenocol Cephalothin
Doxycycline CeIamandole
Erythromycin CeIoxitin
Dicloxacilin Carbenicllin
CeIaclor Penicillin G
Minor downward adjustment
Clindamycin Vancomycin
Amoxicillin Gentamycin
Penicillin V
Oxacillin
Significant downward adjustment Minocyline
Aminoglycosides Tetracycline
CeIazolin
Drugs to avoided in liver disorders-
Erythromycin estolate
Tetracyclin
ampicillin
Dose reduction-
Chloramphinicol
Metronidazole
Clindamycin
PREGNANCY AND ANTIBIOTICS
$afe antibiotics
penicillins
cephalosporins
erythromycin
Drugs contraindicated in children-
chloramphinicol
Tetracycline
MONITORING THE PATIENT
Adjunctive surgery
Fluid balance
Response to treatment :
The response begins by the second day, and initially it is a
subjective sense oI Ieeling better.
From that time onward, objective signs oI improvement occur
Duration oI antibiotic therapy 2-3 days
CAUSES OF FAILURE IN TREATMENT OF INFECTION
Inadequate surgical treatment
Depressed host deIenses
Presence oI Ioreign body
Antibiotic problems
Drug not reaching inIection
Dose not adequate
Wrong bacterial diagnosis
Wrong antibiotic
ADVERSE REACTIONS
WAdverse reactions occur all too commonly.
WHypersensitivity reactions occur with all antibiotics.(penicillin,
cephalosporin)
WThese reactions may include accelerated anaphylactic reactions (type 1)
or less severe reactions associated with edema, urticaria, and itching.
WThe less severe reactions that develops as a rash or urticaria may begin
immediately or many hours after exposure (type 2 & 3)
WDelayed hypersensitivity reactions (type 4) are mediated by T-
lymphocytes,
Most common sign is persistent low grade temperature even after pain,
swelling and other problems subsides.
DC-eosinophil count is increased
The temperature elevation resolves in 24 to 48 hrs after the drug is
withdrawn.
Antibiotics frequently causes gastrointestinal distress
Combination antibiotic therapy :
Broad-spectrum exposure that leads to depression oI the normal host
Ilora and increased opportunity Ior resistant bacteria to emerge.
Indications :
When it is necessary to increase the antibacterial spectrum in the
patient with liIe-threatening sepsis oI unknown cause.
When it is desirable to increase the bactericidal eIIect against a
speciIic organism.
In the prevention oI the rapid emergence oI resistant bacteria
Adjunctive treatment :
Endodontic therapy or extraction
Surgical drainage
Many chronic dentoalveolar abscesses need
curettage.
dontogenic infection,
oral and maxillofacial
implications
INFECTION
Initial stage- Aerobic bacteria invade
Cellulitis
Severe inIection-
Aerobic and anaerobic
Abcess
Advanced stage- anaerobic inIection
Therapeutic uses of antibiotics in maxillofacial surgery :
Pericoronitis :
Acute pericoronitis, iI severe, may require antibiotic therapy.
Again Penicillin is the drug oI choice.
Treatment - debridement, drainage oI the site, penicillin 500 mg qid,
amoxacillin 500mg qid, clindamycin 300mg qid
Abscess :
Acute dentoalveolar abscess and cellulitis
Penicillin is the drug of choice
Soft tissue wounds :
II a wound has been open Ior six hours or more, it should be
considered inIected, and iI primary closure is elected, a delayed
primary closure is the method oI choice. II the delayed technique
cannot be utilized, antibiotic support is helpIul.
II early primary closure is necessary, amoxicillin with clavulanic acid
is the drug oI choice.
Chronic inIlammatory periodontal diseases-
TOPICAL MEASURES Tetracyclins, metronidazole250mg tid, ,
penicillins500mg qid, cephalosporins
ANUG-Topical measures with systemic antibiotic penicillin,
metronidazle400mg qid,
Osteomyelitis :
IdentiIy the causative organisms
Must be treated with antibiotics Ior a much longer period than soIt
tissue inIections
Jaws that require special therapy
Actinomycosis
Fungal inIections
Fractures :
Antibiotics must be given in therapeutic doses Ior 10 to 14 days
Administration oI the antibiotic should begin as early as possible
aIter diagnosis
Antibiotic regimen Ior
osteomyelitis
or ospitalalized/ wen inta-venous terapy is indicated-
Aqueous penicillin, 2 million U IV 6h, metronidazole 500mg 6h Ior 4 - 6
weeks
OR
Ampicillin/sulbactum 1.5 to 3.0 gm IV 6h Ior 2 days then
amoxacillin/clavulanate (augmentin)875, 125.mg PO bd Ior 4 to 6 weeks
for out patient treatment
penicillin V 2gm metronidazole 500mg 8h Ior 2 to 4 weeks aIter last
sequestrum removal and patient with out symptons.
OR
ceIoxitin 1 gm q8h IV OR IM
cephalexin 500mg 6h PO Ior 2 to 4 weeks
OR
clindamycin 600, 900mg 6h IV then clindamycin 300, 450 mg 6h PO
#egimen for fracture
Pre-opratively
penicillin 2 million units or ceIazolin 0.5 gm-1.5 gm 12 hr |25- 50
mg/kg|
Post-operatively
Penicillin 500mg 6 hr |30-40 mg /kg|
Cephalexin 500mg 6 hr |25- 50 mg/kg|
In suspected intra-cranial contamination-
Pre-operatively- naIicillin 2-6 gm 6hr gentamycin 3-5mg/kg 8 hr
Post-operatrively- cephalexin 500mg 6 hr|25-50 mg/kg|
PROPHYLACTIC ANTIBIOTICS
Advantages :
Prevention oI inIection
Decreased patient morbidity
Decreased patient mortality
Decreased medical costs
Decreased total antibiotic usage
Disadvantages :
Failure oI prophylaxis
Development oI increased numbers oI resistant bacteria
Masking oI inIection
Principles for the use of prophylactic antibiotics :
The operative procedure must have a risk oI signiIicant bacterial
contamination and a high incidence oI inIection.
The organism most likely to cause the inIection must be known.
The antibiotic susceptibility oI the causative organism must be known.
To be eIIective and to minimize adverse eIIects, the antibiotic must be
in the tissue at the time oI contamination (operation) and it must be
continued Ior no more than Iour hours aIter cessation oI contamination.
The drug must be given in dosages suIIicient to reach Iour times the
MIC oI the causative organisms.
THE AMERICAN ACADEMY OF PEDIATRIC DENTISTRY
(AAPD)
Antibiotic prophylactic regimens
" Clindamycin 20mg/kg (maximum
600mg) IV or IM or ceIazolin 25mg/kg
(maximum 1g) IV or IM within 30 min
beIore dental procedure
" Children allergic to penicillin and
unable to take oral medications
" Clindamycin 20mg/kg (maximum
600mg) orally 1 h prior to dental
procedure
" Children allergic to penicillin
Ampicillin 50mg /kg (maximum 2g) IV or
IM within 30 min beIore dental procedure
Children not allergic to penicillin and
unable to take oral medications
Amoxicillin 50mg/kg (maximum 2g)
orally 1 hr prior to dental procedure
Children not allergic to penicillin
PROPHYLAXIS REGIMEN IN PATIENTS WITH
PROSTHETIC VALVE
I) Standard Regimen
A) Preoperatively : 30 minutes beIore surgery
Ampicillin 1.0-2.0 g IM or IV and
Gentamicin 1.5 mg/kg IM or IV
B) Postoperatively
Penicillin V 1.0 g PO 6 hours aIter initial dose or
Repeat preoperative regimen 8 hours aIter initial dose
II) Penicillin - allergic patient
A) Vancomycin
Preoperatively : 1.0 g by slow IV drip (over 6 hour period). Begin 1
hour beIore surgery
Postoperatively : No repeat doses
III) Pediatric dosage
A) Standard regimen
Ampicillin : 50 mg/kg per dose
Gentamicin : 2.0 mg/kg per dose
Penicillin V : 500 mg per dose
B) Penicillin Allergic patient
Vancomycin 20 mg/kg per dose
PROPHYLAXIS FOR WOUND INFECTION IN ORAL AND
MAXILLOFACIAL SURGERY
Burke (1973) : 'preventive antibiotics are indicated iI there is a high
probability that a patient`s natural resistance to bacterial invasion will
not overcome the combined bacterial and physiological challenge oI a
surgical procedure.
In general, routine oIIice oral surgical procedures perIormed on the
normal patient do not require antibiotic prophylaxis.
Patient with normal defenses may require prophylaxis for some
procedures :
Long (over three hours) procedure requires the use oI prophylactic.
Bone graIt procedures.
Patients who receive large implants oI metal, plastic or other
alloplastic material.
Immucocompromised host.
Patients on cytotoxic cancer chemotherapy.
On immunosuppressive drugs such as glucocorticoids, azathioprine
(Imuran), or cyclosporine.
For intraoral procedures, the drug oI choice is penicillin given
parenterally, one or two million units preoperatively and an additional
dose every one and a halI to two hours. The last dose is given aIter
complete recovary.
W Surgical prophylaxis-
W Under L.A
W Amoxacillin 3 gm or clindamycin 600mg 1 hr pre- operatively
and amoxacillin 1gm after 6 hr
W Under G.A
W Amoxacillin 0.5 gm IM after 6 hr or 3 gm 4 hr + 1 gm probensid
post-operatively.
#
W larithromycin 500mg or azithromycin 2 gm 6 hr post-
operatively.
W With previous history of infective endocarditis-
W Amox 1gm+ gentamycin 120mg IM and Amox 0.5 oral gm after
6 hr
#
W 'ancomycin I' 1gm + gentamycin 120 mg 6 hr post-
operatively.
INDIVIDUAL ANTIBIOTICS
effective against gram positive organisms
[Beta-lactum antibiotics] Penicillin
Basic structure Consist oI thiazolidine ring Iused with a beta
lactum ring.|6 amino-penicilanic acid- essential Ior the
antibacterial activity|
Semi synthetic penicillins are produced by altering the
composition oI side chain, in addition gives stability against
degradation by gastric acid and by enzyme
penicillinase|betalactamase|
60/ bound to plasma albumin.| inactive Iorm|
Eliminated by kidney.
The drug oI choice Ior the initial empirical management oI
odontogenic inIections remains penicillin
It is bactericidal bind to peptidoglycan-unique in bacterial cell
wall~
Narrow but appropriate spectrum, absorbed- Irom duodenum.
Food interIeres absorption - oral dose to be given 30 min beIore or
2-3 hr aIter Iood.
On parenteral administration- level oI the drug in lymph rise slowly
but persist longer compared to plasma.
High conc. in - kidney,
SigniIicant conc. in- bile, liver, intestine, skin
W PeniciIIin V, potassium phenoxyethyI peniciIIIin, azidociIIin
- peniciIIinase resistent acid IabiIe form
W Potassium saIt form
W More rapidIy absorbed
W Less active than benzyI peniciIIin
W Not used in management of severe infection.
W
Methicillin-
effective against penicillinase producing organism
community acquired S. aureus are sensitive.
Methicillin resistant staphyococci are resistant to all betalactum
antibiotics. also known as beta-lactum antibiotic resistant]
naIicillin - more active than methicillin but less active than benzyl
penicillin
It is bound with plasma protien
excreted by the liver
cloxacillin-5-10 times more active than methicillin
90- 95 / is plasma protien bound
diclozacilln-blood level is twice as that oI cloxacillin
95/ plasma protien bound.
Flucloxacillin-simillar to dicloxacillin
Less protein bound
Staphyloccal resistant to the above penicillinase resistant
penicillin is by chromosomal mediated production of a new
Penicillin binding protien.
Ampicilin- antibacterial activity is simillar to benzyl penicillin
More active against gram negative micro-organisms
It is water soluble and acid resistant
Food do not interfere absorption, but incompletely absorbed
excreted by kidney
In infants and children excretion is delayed
Parenteral solution deteriorates fast
Talampicillin-is a carboxylic ester of ampicillin
Rapidly absorbed from gut
Hydrolyzed by tissue esterase in to active form.
Amoxicillin- it is amio-p- hydroxy-benzyl penicillin
Broad spectrum of activity simillar to ampicillin
Orally effective, and blood levels are twice as that of ampicillin
Carbenicillin- weaker antibacterial spectrum than ampicillin.
Advantage over ampicillin is that it is eIIective against all strains
oI proteus, pseudomonas aeruginosa.
It is penicillinase susceptable.
It`s acid labile and must be given parentarilly.
%icarcillin- it is thienyle analogue oI carbenicillin.
antimicrobial activity is twice that oI carbenicillin.
Piperacilllin- it is betalactamase sensitive.
broad spectrum activity against gram negative
it is acid labile.
Clavulanic acid -it is well absorbed on oral administration.
It has only a weak antibacterial activity.
It is potent and irreversible inhibitor oI many betalactamase and
protect betalactum antibiotic Irom inactivation.
Used in combination with amoxacillin and ticarcillin.
Cepazolin-more active against klebicella, E.coli.
Susceptable to staphylococcal beta lactamases.preIIered Ior surgical
prophylaxis. T - 2 hr.
cepalexin- orally eIIective Iirst generation cephalosporin.
Has similar spectrum oI activity.T1/2- 1hr.
Cepadroxil- has good tissue penetration.
Has sustained action at the site oI
inIection.
Cefoxitin, cefuroxime- produced by actinomycete.
Highly resistant to beta lactamases produced by gram negative organisms.
Used in treatment oI anaerobic inIection, surgical inIection.T - 2 hr.
Cefuroxim axetil- orally eIIective.
Cefotaxime- It is the prototype oI the third generation
exerts potent action on anaerobic as well some gram positive bacteria
Not so active on anaerobes
prominent indications are meningitis caused by gram negative bacilli, liIe
threatening /hospital acquired inIections.septicaemias and inIections in
immunocompromised patients.
Cefpirome- used in serious and resistant hospital acquired inIections
including septiciemias .
it is eIIective on all gram negative bacterias .
Monobactams- inhibits gram negative bacilli .
It is resistant to gram negative beta-lactemases .
The main inIections are hospital acquired inIections.
T1/2 1.8 hrs
imipenem - it is extremely potent and most broad spectrum beta-lactam
antibiotic
Clindamycin :
Is a lincosamide
Widely distributed in tissue Iluids and tissues, including bone.
Avoid in the routine odontogenic inIection
An excellent alternative drug in penicillin-resistant anaerobic
inIections
Used in Osteomyelitis oI the jaws
Antimicrobial activity in colon is Ior 5days.
'ancomycin- primarily active against gram positive bacteria.
It is a bacteriostatic drug, in combination with gentamycin or tobramycin -
bactericidal.
Poorly absorbed aIter oral absorption, always given I.V.
HalI liIe 6 hr. Peak concentration is 60 micrograms/ml, higher
concentration causes ototoxicity.
Newborn- 15mg/kg 12 hourly, inIants- |8-30 days older| 15 mg/kg 8
hourly, children-10mg/kg 6 hourly, adult- 125- 250mg/kg 6 hourly.
Given orally in conditions like pseudomembranus colitis.
EIIective alternative Ior the treatment oI endocarditis, in penicillin allergic
patients.
%eicoplanin- used in Osteomyelitis, endocarditis, methicillin resistant
strains inIections.
Can be given I.M.
Bacitracin- active against gram positive bacteria.
Only topically used
Used in opthalmical inIection, inIected ulcers, and in dressing oI wound
aIter debridemant.
ystatin- highly toxic
Used Ior topically application.
Not absorbed on oral administraton, can be used in monilial
diarrhoea |super inIection|
%etracycline-
Broad spectrum antibiotic.
Low bsorption through git.
Rapid renaI excretion,
Low phototoxic
Markad aIteration of intestinaI bacteria.
emiclocycline-
Intermediate potency.
High pIasma binding capacity.
SIower renaI excretion.Highest phototoxic.
Doxicycline-
High potency.
Complete absorbtion from intestine.
High plasma binding.
T1/2- 18-24 hr.
Least alteration of intestinal flora.
Low toxix\city.metabolised in liver.
lorampinicol
Is not a Iirst -line oI antibiotic
Causes potential toxicity- aplastic anemia,gray baby syndrome.
Indicated Ior liIe thratning conditions-bacterial meningitis,
rickettsial inIections.
[Macrolides] Erythromycin-
anti bacteriaI spectrum is simiIIar to peniciIIin.
The drug is effective against peniciIin resistant staphyIococci.
Absorbed from smaII intestine.
The drug is partiaIIy destroyed by gastric juice, and has to be
administered in the form of enteric coated tabIets.
EstoIate form is the most resistant to inactivation by gastric acid.
Various preparation- enteric coated tabIets
EstoIate form
Sterate
EthyIsuccinate [parenteraI]
GIucoheptonate[parenteraI ]
drugs beIonging to this group- oIindomycin
Spiramycin
Anti microbiaI activity is higher than erythromycin.
New macroIids- roxithromycin, cIarithromycin
SimiIIar spectrum of activity as that of erythromycin
More resistant to acid hydroIysis.
Better tissue IeveI are achaived.
W Newer macroIides [azalids] azithromycin-
W ChemicaIIy differ from the macroIide group in that the
Iactone ring contains a nitrogen atom.
W It has simiIIar activity that of erythromycin.
W It has better tissue penetration.
W It has Ionger haIf Iife thaan erythromycin.
W larithromycin-
W Differ from erythromycin onIy in methyIation of hydroxyI
group.
W RapidIy absorbed from gut.
W Has Iinger haIf Iife and better tissue penetration.
Gentamicin (t 2.0 hrs):
Administered M as there is a better control on absorption and avoids high
serum concentration. t is effective against gram positive and negative bacteria
including penicillinase resistant staphylococci. The combined effects of
ampicillins and gentamicin are effective against a wide spectrum of gram +ve
bacteria including streptococci and staphylococci and gram-ve bacteria.
Gentamicin and ampicillin should be administered separately coz gentamicin
gets destroyed.
t is indicated in severe anaerobic infections.
Dose Adult 3-7mg/kg/day in 2-3 divided dose.
Child 1-3mg/kg/day in 2-3 divided dose.
Toxicity t causes ototoxicity (vestibular and cochlear). f serum
concentrations exceed 10mg/ml transient tinnitus may occur.
When used over a weak, nephrotoxicity occurs.
Allergic reactions not recommended in lactating mothers.
METRONIDAZOLE(t 4.0hr) MIC<3.0:
Mechanism of action: t enters the microorganisms by diffusion, gets
reduced to intermediate compounds which causes cytotoxicity by
damaging DNA. t also inhibits cell mediated immunity to induce
mutagenesis and cause radiosensitization.
Effective in anaerobic infections and ANUG. t is used with one of
the penicillins to treat orofacial infections. t can also be used with
cephalosporins in penicillin allergic patients.
t is effective against gram +ve and ve bacteria including
bacteriodes, clostridia and spirochetes.
t is absorbed from GT and competes with food. t is excreted in
urine which may be coloured red brown. mpaired renal and hepatic
function can prolong presence of drug in serum. Also excreted in saliva
and breast milk in similar concentration to plasma.
LOUROQUINOLONES.
The fluoroquinolones are broad-spectrum antibiotics with
particular activity against gram-negative organisms, especially
Pseudomonas aeruginosa. These agents are well absorbed
when given orally. Because tissue and fluid concentrations often
exceed the serum drug concentration, these antibiotics are
particularly useful for certain infections, such as pneumonia.
Fluoroquinolones are usually well tolerated, with few side
effects. However, they can have serious adverse effects.
REFERENCES
The pharmacological bases of therapeutics - Goodman and
Gilamns.
Essentials of Medical Pharmacology - KD Tripathi.
The short Textbook of Medical Microbiology - Satish Gupte.
Textbook of pharmacology - Topazian
Text of pharmacology and pharmacothraputics-Satoskar
You might also like
- Intraventricular Hemorrhage (IVH) : Intensive Care Nursery House Staff ManualDocument3 pagesIntraventricular Hemorrhage (IVH) : Intensive Care Nursery House Staff Manualjimzz44No ratings yet
- CV Petrangolini enDocument8 pagesCV Petrangolini enTeresa PetrangoliniNo ratings yet
- Target Heart Rate Lesson PlanDocument4 pagesTarget Heart Rate Lesson PlanEryn YeskeNo ratings yet
- ACOG - External Cephalic Version PDFDocument10 pagesACOG - External Cephalic Version PDFPat CabanitNo ratings yet
- AntibioticsDocument54 pagesAntibioticsYvan MercedNo ratings yet
- Chapter 11Document23 pagesChapter 11Hannah BuquironNo ratings yet
- Chapter 16 Anti InflammDocument36 pagesChapter 16 Anti InflammAngela Joy AmparadoNo ratings yet
- Fluid and Elctrolyte Balance.... Power PointDocument40 pagesFluid and Elctrolyte Balance.... Power PointMarwan M.100% (1)
- SepsisDocument33 pagesSepsisv_vijayakanth7656No ratings yet
- Anal FistulaDocument26 pagesAnal FistulaBeverly PagcaliwaganNo ratings yet
- Peptic Ulcers: DR Yotham Phiri Mmed (Surg)Document46 pagesPeptic Ulcers: DR Yotham Phiri Mmed (Surg)Emmanuel MukukaNo ratings yet
- Poisoning II FinalDocument45 pagesPoisoning II FinalBi PinNo ratings yet
- In The Name of Allah, The Most Beneficent and MercifulDocument35 pagesIn The Name of Allah, The Most Beneficent and MercifulAhmedMenshawyNo ratings yet
- Amniotic Fluid Embolism: Women's Hospital School of Medicine Zhejiang Un Iversity Wang ZhengpingDocument19 pagesAmniotic Fluid Embolism: Women's Hospital School of Medicine Zhejiang Un Iversity Wang ZhengpingPoonam RanaNo ratings yet
- 1 Principles of First Aid and Its PracticeDocument118 pages1 Principles of First Aid and Its PracticeMohamed SamyNo ratings yet
- Drugs Used in TuberculosisDocument27 pagesDrugs Used in Tuberculosisapi-3705123No ratings yet
- Cough: PHR Sangita ShakyaDocument21 pagesCough: PHR Sangita ShakyaCurex QANo ratings yet
- PancreatitisDocument12 pagesPancreatitismardsz100% (5)
- Acute TonsillitisDocument54 pagesAcute TonsillitissuciNo ratings yet
- Chapter 12Document24 pagesChapter 12Hannah BuquironNo ratings yet
- Case Presentation-ChickenpoxDocument41 pagesCase Presentation-ChickenpoxShaliniNo ratings yet
- History of Old ClientDocument33 pagesHistory of Old ClientMuhammad Aamir100% (1)
- 1 RicketsDocument32 pages1 RicketsDarina Ismakaieva100% (1)
- Muscle Strength TestingDocument3 pagesMuscle Strength TestingGiselle Chloe Baluya ico100% (1)
- Emergency DrugsDocument10 pagesEmergency DrugsnieacatleyaNo ratings yet
- Management of CholeraDocument69 pagesManagement of CholeraNatalia LawrenceNo ratings yet
- Sepsis and Septic Shock: Elise Mittleman Boller, - Cynthia M. OttoDocument9 pagesSepsis and Septic Shock: Elise Mittleman Boller, - Cynthia M. OttoIan SabogalNo ratings yet
- Pyogenic MeningitisDocument46 pagesPyogenic MeningitisShahnaaz ShahNo ratings yet
- CAD - EBM September 2020 EditionDocument17 pagesCAD - EBM September 2020 EditionNaga Venkatamanoj Kumar PakalapatiNo ratings yet
- Antiinflammatory Drugs: Toya AriawanDocument27 pagesAntiinflammatory Drugs: Toya Ariawanlast100% (1)
- 12.hypersensitivity 2013Document58 pages12.hypersensitivity 2013lookmoo100% (1)
- Vaccination or ImmunizationDocument4 pagesVaccination or ImmunizationPrincessNo ratings yet
- Coagulation Tests: Clotting Time, Bleeding Time, Prothrombin Time, Activated Partial Thromboplastin TimeDocument15 pagesCoagulation Tests: Clotting Time, Bleeding Time, Prothrombin Time, Activated Partial Thromboplastin TimeAnastasiaNo ratings yet
- Gastrointestinal DrugsDocument2 pagesGastrointestinal DrugsJannah Mikhaela Alibay VillarinNo ratings yet
- Antihyperlipidemic Drugs: Key Terms Chapter ObjectivesDocument9 pagesAntihyperlipidemic Drugs: Key Terms Chapter ObjectivesSasa AbassNo ratings yet
- Preanesthetic Medication JasminaDocument44 pagesPreanesthetic Medication Jasminaanjali sNo ratings yet
- Tuberculosis Power PointDocument20 pagesTuberculosis Power PointLeena LapenaNo ratings yet
- OMCDocument37 pagesOMCyurie_ameliaNo ratings yet
- 18 Measles (Rubeola)Document12 pages18 Measles (Rubeola)Sheryl ElitaNo ratings yet
- Chapter 14 AntineoplasticDocument37 pagesChapter 14 AntineoplasticAngela Joy AmparadoNo ratings yet
- Chapter 09 AntibioticsDocument77 pagesChapter 09 AntibioticsAngela Joy AmparadoNo ratings yet
- Management of Inflammatory Bowel Disease: Dr. Sumithra AppavaDocument43 pagesManagement of Inflammatory Bowel Disease: Dr. Sumithra AppavadrcumeeNo ratings yet
- Maricris Q. Marquita-Uy R.N, M.DDocument42 pagesMaricris Q. Marquita-Uy R.N, M.DAdrian Mai AlanNo ratings yet
- Hirschprung DiseaseDocument9 pagesHirschprung DiseaseRajeev JhaNo ratings yet
- CystitisDocument16 pagesCystitismail2manshaaNo ratings yet
- Anti-Cholinergic Drugs and Cholinesterase InhibitorsDocument24 pagesAnti-Cholinergic Drugs and Cholinesterase InhibitorsKhalid I. Abdullah100% (1)
- Case Presentation: by Michael ArmstrongDocument21 pagesCase Presentation: by Michael ArmstrongWirawan Amirul BahriNo ratings yet
- UntitledDocument6 pagesUntitledFritz Angelo BullonNo ratings yet
- Personal Data of Patient: Intensive Nursing Practicum - Pediatric Ward (BMC) CASE STUDY 5: Pediatric OncologyDocument12 pagesPersonal Data of Patient: Intensive Nursing Practicum - Pediatric Ward (BMC) CASE STUDY 5: Pediatric OncologyromelynNo ratings yet
- Drugs For GUTDocument11 pagesDrugs For GUTAyesha LiaqatNo ratings yet
- Inflammatory Bowel DiseasesDocument30 pagesInflammatory Bowel DiseasesMohammedHuzairIbunuAbidNo ratings yet
- Reye SyndromeDocument10 pagesReye SyndromeDanil KhairulNo ratings yet
- Nephrotic Syndrome 2016Document45 pagesNephrotic Syndrome 2016alaaNo ratings yet
- Airway Emergencies: ORL PostingDocument58 pagesAirway Emergencies: ORL PostingKimberlyLaw95No ratings yet
- Refkas CondylomaAccuminataDocument18 pagesRefkas CondylomaAccuminatamichelle1945No ratings yet
- Inguinal Hernias and Abdominal Wall Defects: Murad Nuserat & Abd AL-Rahman AlhelwDocument51 pagesInguinal Hernias and Abdominal Wall Defects: Murad Nuserat & Abd AL-Rahman AlhelwRashed ShatnawiNo ratings yet
- Pharma Unit 1-2 Anti - Adrenergic DrugsDocument21 pagesPharma Unit 1-2 Anti - Adrenergic DrugsMIbrahimNo ratings yet
- Cataract - Case PresentationDocument80 pagesCataract - Case PresentationNEILVEL KNo ratings yet
- CellulitisDocument5 pagesCellulitisaimigdragonNo ratings yet
- Module 5A: Dental Management of Patients With Asthma: Prepared By: Dr. Maria Luisa Ramos - ClementeDocument27 pagesModule 5A: Dental Management of Patients With Asthma: Prepared By: Dr. Maria Luisa Ramos - Clementeelaine100% (1)
- Wilms TumorDocument12 pagesWilms TumorKath CamachoNo ratings yet
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- Experience Blissful Sleep Tonight - Maharishi Ayurveda BlogDocument2 pagesExperience Blissful Sleep Tonight - Maharishi Ayurveda BlogRory BolleursNo ratings yet
- ACS Final DraftDocument33 pagesACS Final Draftomcm17006No ratings yet
- g8 Health q3 LM Disease 130908005904 PDFDocument64 pagesg8 Health q3 LM Disease 130908005904 PDFkenneth cannillNo ratings yet
- الصحة PDFDocument17 pagesالصحة PDFGamal MansourNo ratings yet
- Pharmaceuticals Manufacturing - What Do We Know About The Occupational Health and Safety Hazards For Women Working in The Industry PDFDocument61 pagesPharmaceuticals Manufacturing - What Do We Know About The Occupational Health and Safety Hazards For Women Working in The Industry PDFCostas JacovidesNo ratings yet
- PARS 19 - Slide PDFDocument23 pagesPARS 19 - Slide PDFNorsyaliza Abd Razak100% (1)
- Chapter 2 Lesson 1Document3 pagesChapter 2 Lesson 1John Carldel VivoNo ratings yet
- A Combined Patient and Provider Intervention For Management of Osteoarthritis in VeteransDocument13 pagesA Combined Patient and Provider Intervention For Management of Osteoarthritis in VeteransHarshoi KrishannaNo ratings yet
- Topic ListDocument6 pagesTopic ListEdwinNo ratings yet
- SuctioningDocument6 pagesSuctioningCriselda Ultado100% (2)
- MSDS Aceite CastorDocument6 pagesMSDS Aceite CastorwaddydiNo ratings yet
- Adani Targets Debt Cuts, Income Boost Coastal Shipping To Get Infra Status, Says SonowalDocument20 pagesAdani Targets Debt Cuts, Income Boost Coastal Shipping To Get Infra Status, Says SonowalboxorNo ratings yet
- Lecture 1 Health, Safety & Environment (HSE)Document23 pagesLecture 1 Health, Safety & Environment (HSE)A to z type videosNo ratings yet
- ADS Dec 27Document1,946 pagesADS Dec 27Robert Andrew BaldadoNo ratings yet
- 2020 HivDocument1 page2020 HivhenkNo ratings yet
- GENDER Reseach 100%3Document46 pagesGENDER Reseach 100%3Mesud GemechuNo ratings yet
- Laparoscopic Appendectomy SurgeryDocument2 pagesLaparoscopic Appendectomy SurgeryNycoNo ratings yet
- IJHPM - Volume 7 - Issue 12 - Pages 1073-1084 Complex LeadershipDocument12 pagesIJHPM - Volume 7 - Issue 12 - Pages 1073-1084 Complex Leadershipkristina dewiNo ratings yet
- State of The World's Midwifery 2014: A Universal Pathway - A Woman's Right To HealthDocument228 pagesState of The World's Midwifery 2014: A Universal Pathway - A Woman's Right To HealthUNFPA SoWMYNo ratings yet
- Overcoming Obesogenic Environments: A Qualitative Study Exploring Mechanisms of Healthy EatersDocument10 pagesOvercoming Obesogenic Environments: A Qualitative Study Exploring Mechanisms of Healthy EatersCristina Saldias PorrasNo ratings yet
- Health Declaration FormDocument1 pageHealth Declaration FormUzair KhalidNo ratings yet
- Fatal Airway Obstruction Due To Ludwig'sDocument6 pagesFatal Airway Obstruction Due To Ludwig'sRegina MugopalNo ratings yet
- PneumoconiosisDocument19 pagesPneumoconiosisgabriela.was.gabbbieNo ratings yet
- 1120161049855Document16 pages1120161049855Ruchi SharmaNo ratings yet
- Domestic Violence Cycle of Violence Types of Families-2Document22 pagesDomestic Violence Cycle of Violence Types of Families-2api-340420872No ratings yet
- Pattern Before Hospitalization During HospitalizationDocument2 pagesPattern Before Hospitalization During HospitalizationJean WinNo ratings yet
- Lab Report 15438869 20231127064225Document1 pageLab Report 15438869 20231127064225carilloabhe21No ratings yet