Professional Documents
Culture Documents
Type and Indication of IV Therapy 2
Uploaded by
Ruth Jazelle MendozaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Type and Indication of IV Therapy 2
Uploaded by
Ruth Jazelle MendozaCopyright:
Available Formats
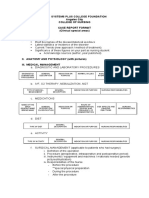
Done by : Salwa Maghrabi Teacher Assistant Nursing Department
Definition of IV therapy Indication of IV therapy Type of IV solution .
Isotonic solution Hypertonic solution Hypotonic solution
Categories of intravenous solutions according to their purpose.
Nutrient solutions
Electrolyte solutions (Crystalloid)
Volume expanders (Colloid)
Parenteral Nutrition (PN)
Clinical indications of parenteral nutrition. IV Infusion Method . Equipment of I.V. therapy. Nursing role in managing patient receiving IV therapy
Nursing assessment . Nursing diagnosis. Implementation
Initiation phase
Maintenance phase
Discontinuing IV infusion .
Recoding and reporting . Evaluation .
Define intravenous therapy . List the indications of IV therapy . Differentiate between the types of IV solutions. Discuss the categories of IV solution according to their purpose . List the IV infusion methods. Discuss the nursing process for the patient who receiving IV therapy .
It is an effective and efficient method of supplying fluid directly into intravenous fluid compartment producing rapid effect with availability of injecting large volume of fluid more than other method of administration.
Maintain or replace body store . Restore acid abase balance Restore the volume of blood component Administer of medication Provide Nutrition Monitor CVP
Type of IV solution
Isotonic
Hypotonic
Hypertonic
A solution that has the same salt concentration as the normal cells of the body and the blood. Ex: 1- 0.9% NaCl . 2- Ringer Lactate . 3- Blood Component . 4- D5W.
A solution with a higher salts concentration than in normal cells of the body and the blood. Ex: 1- D5W in normal Saline solution . 2-D5W in half normal Saline . 3- D10W.
A solution with a lower salts concentration than in normal cells of the body and the blood. EX: 1-0.45% NaCl . 2- 0.33% NaCl .
Nutrient solutions. Electrolyte solutions. Volume expanders.
It contain some form of carbohydrate and water. Water is supplied for fluid requirements and carbohydrate for calories and energy. They are useful in preventing dehydration and ketosis but do not provide sufficient calories to promote wound healing, weight gain, or normal growth of children. Common nutrient solutions are D5W and dextrose in half-strength saline.
fluids that consist of water and dissolved crystals, such as salts and sugar. Used as maintenance fluids to correct body fluids and electrolyte deficit . Commonly used solutions are: -Normal saline (0.9% sodium chloride solution). -Ringers solutions (which contain sodium, chloride, potassium, and calcium. -Lactated Ringers solutions (which contain sodium, chloride, potassium ,calcium and lactate) .
Are used to increase the blood volume following severe loss of blood (haemorrhage) or loss of plasma ( severe burns).
Expanders present in dextran, plasma, and albumin.
Parenteral nutrition is a form of nutritional support that supplies protein, carbohydrate, fat, electrolytes , vitamins, minerals, and fluids via the IV route to meet the metabolic functioning of the body.
Client cannot tolerate internal nutrition as in case of paralytic ileus, intestinal obstruction, persistent vomiting. Client with hyper metabolic status as in case of burns and cancer. Client at risk of malnutrition because of recent weight loss of > 10%, NPO for > 5 days, and preoperative for severely depleted clients.
I.V. Bolus (I.V. push)
IV Infusion Method
Intermittent infusion Continuousdrip infusion
I. Solution containers.
II. I.V. administration sets.
1- assess the solution:
Sterile Clear and not expired No small particles No leakage
2- Reading the label on the solution. 3- Determine the compatibility of all fluid and additives. 4- observe I.V sets
Cracks Holes Missing clamps Expired date
Also, the nurse should assess the patient for : 1- Any allergies and arm placement preference. 2- Any planned surgeries. 3- Patients activities of daily living.
4- Type and duration of I.V therapy, amount, and rate.
Anxiety (mild, moderate, severe) related to threat regarding therapy. Fluid volume excess. Fluid volume deficit. Risk for infection. Risk for sleep pattern disturbance. Knowledge deficit related to I.V therapy.
Identify expected outcomes which focus on: preventing complications from I.V therapy. minimal discomfort to the patient. restoration of normal fluid and electrolyte balance . patients ability to verbalize complications.
I. Implementation during initiation phase A) Solution preparation: the nurse should be: Label the I.V container. Avoid the use of felt-tip pens or permanent markers on plastic bag. Hang I.V bag or bottle .
B) Site preparation: 1- Cleanse infusion site. 2- Excessive hair at selected site should be clipped with scissor . 3- Cleanse I.V site with effective topical antiseptic. 4- Made Venipuncture at a 10 to 30 degree angle.
C) Regulating flow rate: Fluid delivered
IV pump Gravity
The nurse calculate the infusion rate by using the following formula :
volume to be infused (ml/h) gtt/ml(IV set) gtt/min time in minutes (60 min/1h)
II. Implementation during maintenance phase A) Monitoring I.V infusion therapy: the nurse should : inspect the tubing. inspect the I.V set at routine intervals at least daily. Monitor vital signs . recount the flow rate after 5 and 15 minutes after initiation
B) Intermittent flushing of I.V lines
Peripheral intermittent are usually flushed with saline (2-3 ml 0.9% NS.)
C) Replacing equipments (I.V container, I.V set, I.V dressing):
I.V container should be changed when it is empty. I.V set should be changed every 24 hours. The site should be inspected and palpated for tenderness every shift or daily/cannula should be changed every 72hours and if needs. I.V dressing should be changed daily and when needed
III. Implementation during phase of discontinuing an I.V infusion
The nurse never use scissors to remove the tape or dressing. Apply pressure to the site for 2 to 3 minutes using a dry, sterile gauze pad. Inspect the catheter for intactness. The arm or hand may be flexed or extended several times.
Type of fluid, amount, flow rate, and any drug added. Insertion site. Size and type of I.V catheter or needle. The use of pump. When infusion was begun and discontinuing. Expected time to change I.V bag or bottle, tubing, cannula, and dressing.
Any side effect. Type and amount of flush solution. Intake and output every shift, daily weight. Temperature every 4 hours. Blood glucose monitoring every 6 hours, and rate of infusion.
Produce therapeutic response to medication, fluid and electrolyte balance. Observe functioning and patency of I.V system. Absence of complications.
http://www.medterms.com/script/main/art. asp?articlekey=3870 -Carol.T.taylor and carol lillis.R, (2001): Fundamentals of Nursing, 4th ed ,Lippincott, company,Pheladelphia ,pp:180-249.
Thank you for listening
You might also like
- NCPDocument10 pagesNCPCristina L. JaysonNo ratings yet
- NCPDocument3 pagesNCPErica Denice CastilloNo ratings yet
- Leptospirosis: Causes, Incidence, and Risk FactorsDocument6 pagesLeptospirosis: Causes, Incidence, and Risk FactorsJackii DoronilaNo ratings yet
- Leukemias: Care SettingDocument11 pagesLeukemias: Care SettingTinNo ratings yet
- Nasogastric Tube Feeding ML4763 PDFDocument7 pagesNasogastric Tube Feeding ML4763 PDFStereo PodNo ratings yet
- Subjective Data: Baseline Data of Client.: Reference: Nurse's Pocket Guide: Diagnoses, Interventions, and RationalesDocument4 pagesSubjective Data: Baseline Data of Client.: Reference: Nurse's Pocket Guide: Diagnoses, Interventions, and RationalesJor GarciaNo ratings yet
- 51 100Document18 pages51 100Jaessa Feliciano100% (1)
- Compute For The Total Body Surface Area Affected by The BurnsDocument2 pagesCompute For The Total Body Surface Area Affected by The BurnsVAL ASHLIE ACEBARNo ratings yet
- Pathophysiology of Shock Sepsis and Organ Failure PDFDocument1,179 pagesPathophysiology of Shock Sepsis and Organ Failure PDFNotInterested100% (1)
- Case Study Final FractureDocument27 pagesCase Study Final Fracture3amabelle arevaloNo ratings yet
- Cerebral Aneurysm Case Analysis and Concept MapDocument5 pagesCerebral Aneurysm Case Analysis and Concept Mapate NarsNo ratings yet
- NCP CSDocument4 pagesNCP CSJM UncianoNo ratings yet
- The Balanced Skeletal TractionDocument1 pageThe Balanced Skeletal TractionGemarie Adarlo CastilloNo ratings yet
- Gordons TypologyDocument3 pagesGordons TypologyMaxinne Allyssa Cancino RoseñoNo ratings yet
- 2.1. Pharmacological Therapeutics. 2.2. Basic Cardiac Life Support (BCLS) and Advanced Cardiac Life Support (ACLS) in Neonates and ChildDocument3 pages2.1. Pharmacological Therapeutics. 2.2. Basic Cardiac Life Support (BCLS) and Advanced Cardiac Life Support (ACLS) in Neonates and Childclint xavier odangoNo ratings yet
- TahbsoDocument4 pagesTahbsomichZ_13No ratings yet
- MS 3 Case Analysis DownloadableDocument1 pageMS 3 Case Analysis DownloadableCharissa Magistrado De LeonNo ratings yet
- Evidence-Based Nursing: I. Clinical QuestionDocument4 pagesEvidence-Based Nursing: I. Clinical QuestionRay Jorge MarmetoNo ratings yet
- Case Analysis On Respiratory DisordersDocument5 pagesCase Analysis On Respiratory DisordersAaron ConstantinoNo ratings yet
- FNCP On Elevated Blood Pressure 2Document4 pagesFNCP On Elevated Blood Pressure 2Aaron EspirituNo ratings yet
- Wound Healing and Wound CareDocument15 pagesWound Healing and Wound CareNinaNo ratings yet
- A Case Study On Mild Compression Deformity L1Document25 pagesA Case Study On Mild Compression Deformity L1JM UncianoNo ratings yet
- Random Blood Sugar Estimation and Its SignificanceDocument11 pagesRandom Blood Sugar Estimation and Its Significanceapi-38237850% (1)
- Assessment of Immune FunctionDocument3 pagesAssessment of Immune Functionhalloween candyNo ratings yet
- Parenteral Fluid Therapy: Types of Intravenous SolutionDocument18 pagesParenteral Fluid Therapy: Types of Intravenous SolutionKathleen Joy Costales Magtanong100% (1)
- Study Questions: Burn InjuriesDocument2 pagesStudy Questions: Burn InjuriesBELTRAN, JEANNE MAURICENo ratings yet
- Psych - Chapter 23 Into To Milieu ManagementDocument4 pagesPsych - Chapter 23 Into To Milieu ManagementKaren かれんNo ratings yet
- Dec 21 23 Case Study ModuleDocument7 pagesDec 21 23 Case Study ModuleKristian Karl Bautista Kiw-isNo ratings yet
- Hepatocellula R CarcinomaDocument45 pagesHepatocellula R Carcinomamhean azneitaNo ratings yet
- QuestionDocument6 pagesQuestiontravelbeeNo ratings yet
- How Does Radiation Therapy Work?Document5 pagesHow Does Radiation Therapy Work?mikeadrianNo ratings yet
- Pleural Fluid Analysis: How The Test Is PerformedDocument4 pagesPleural Fluid Analysis: How The Test Is PerformedKevin LlorenteNo ratings yet
- WWW - Marychilescollge.edu - PH: 667 F.T. Dalupan Sr. ST., Sampaloc, Manila Philippines Tel. 711 - 4233, 735-5341 To 45Document3 pagesWWW - Marychilescollge.edu - PH: 667 F.T. Dalupan Sr. ST., Sampaloc, Manila Philippines Tel. 711 - 4233, 735-5341 To 45Celyn Nicole Fernandez RollanNo ratings yet
- Compartment Syndrome: Return To TopDocument3 pagesCompartment Syndrome: Return To TopSania Kamal BalweelNo ratings yet
- Types of ShocksDocument33 pagesTypes of Shocksmark OrpillaNo ratings yet
- Impaired Physical MobilityDocument2 pagesImpaired Physical MobilityAl-Qadry NurNo ratings yet
- Impaired Physical Mobility R/T Neuromuscular ImpairmentDocument3 pagesImpaired Physical Mobility R/T Neuromuscular ImpairmentjisooNo ratings yet
- SChapter 1Document4 pagesSChapter 1Quio SaludoNo ratings yet
- Rafols, Janna Mae L. 3F-2C OR QuestionsDocument8 pagesRafols, Janna Mae L. 3F-2C OR QuestionsJan Crizza Dale R. FrancoNo ratings yet
- CraniotomyDocument6 pagesCraniotomychaSephNo ratings yet
- Activity IntoleranceDocument6 pagesActivity IntoleranceRaidis PangilinanNo ratings yet
- Hypervolemia What You Need To Know About Fluid OverloadDocument3 pagesHypervolemia What You Need To Know About Fluid OverloadLorenn AdarnaNo ratings yet
- Brief Description of The Disease/statistical IncidenceDocument2 pagesBrief Description of The Disease/statistical IncidenceLeanne Princess Gamboa100% (1)
- BurnsDocument9 pagesBurnsVincentus BinNo ratings yet
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosis Pathophysiolog Y Planning Interevention Rationale EvaluationDocument1 pageNovilyn C. Pataray BSN - Ii: Assessment Diagnosis Pathophysiolog Y Planning Interevention Rationale EvaluationCharina AubreyNo ratings yet
- Common Surgical Instruments ModuleDocument5 pagesCommon Surgical Instruments ModuleAlokKumarNo ratings yet
- Thoracentesis Reflective EssayDocument2 pagesThoracentesis Reflective EssayAnjae GariandoNo ratings yet
- NCM 112 Computation 2021Document3 pagesNCM 112 Computation 2021Marie Kelsey Acena Macaraig100% (1)
- Discharge PlanDocument4 pagesDischarge PlanKabang MoaNo ratings yet
- Fracture (Cast Care)Document6 pagesFracture (Cast Care)Vane UcatNo ratings yet
- NCPDocument2 pagesNCPMelissa David100% (1)
- Nursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term OutcomesDocument2 pagesNursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term OutcomesDeanne Carla DalilisNo ratings yet
- Gouty Arthritis: Presented By: Petit Ivy Mae B. NacarioDocument21 pagesGouty Arthritis: Presented By: Petit Ivy Mae B. NacarioMarivic DianoNo ratings yet
- Buerger's DiseaseDocument4 pagesBuerger's DiseasesweetyjonasNo ratings yet
- Operating RoomDocument13 pagesOperating RoomrichardNo ratings yet
- Pathophysiology of Acute PancreatitisDocument1 pagePathophysiology of Acute PancreatitisHarvin FrancoNo ratings yet
- NCP Risk InfectionDocument1 pageNCP Risk InfectionEni RahmawatiNo ratings yet
- Postoperative Nursing CareDocument2 pagesPostoperative Nursing CareYeana AlonNo ratings yet
- Hypertension NclexDocument5 pagesHypertension Nclexハニファ バランギNo ratings yet
- Nursing Leadership and ManagementDocument283 pagesNursing Leadership and ManagementRuth Jazelle MendozaNo ratings yet
- Leadership and ManagementDocument16 pagesLeadership and ManagementRuth Jazelle MendozaNo ratings yet
- NHHDocument30 pagesNHHRuth Jazelle MendozaNo ratings yet
- Case With Page Numbers FINALDocument60 pagesCase With Page Numbers FINALRuth Jazelle MendozaNo ratings yet
- MasterSeal 910 Data SheetDocument2 pagesMasterSeal 910 Data Sheetravi100% (1)
- Effect of Mixing On The Properties of Nanocarbon Containing Al2O3 C Continuous Casting RefractoriesDocument8 pagesEffect of Mixing On The Properties of Nanocarbon Containing Al2O3 C Continuous Casting RefractoriesAnonymous gQyrTUHX38No ratings yet
- Furnace AC Example PDFDocument5 pagesFurnace AC Example PDFhanafiNo ratings yet
- Bio T4 DLP KSSM Chapter 13 Homeotasis and The Human Urinary SystemDocument66 pagesBio T4 DLP KSSM Chapter 13 Homeotasis and The Human Urinary SystemNurasyikin SaidinNo ratings yet
- NEW Sonotech UT-X Powder PDFDocument2 pagesNEW Sonotech UT-X Powder PDFanmosNo ratings yet
- Eazistrip Reinforcement Continuity SystemsDocument12 pagesEazistrip Reinforcement Continuity SystemscormolioNo ratings yet
- Thermocouples and SensorsDocument40 pagesThermocouples and SensorsEliasNo ratings yet
- Mechanical Properties of Ultra-High-Performance Concrete Enhanced With Graphite Nanoplatelets and Carbon NanofibersDocument10 pagesMechanical Properties of Ultra-High-Performance Concrete Enhanced With Graphite Nanoplatelets and Carbon NanofibersRUSNA KPNo ratings yet
- Air PollutionDocument41 pagesAir PollutionferzanaNo ratings yet
- MP Filtri Accessories HydraulicsDocument12 pagesMP Filtri Accessories HydraulicsDaniel MarNo ratings yet
- Report Performance Appraisal of Square Pharmaceutical LTDDocument21 pagesReport Performance Appraisal of Square Pharmaceutical LTDMd Hasib A Rahman TonmoyNo ratings yet
- Design and Analysis of Shock AbsorberDocument12 pagesDesign and Analysis of Shock AbsorberSILAMBARASANNo ratings yet
- Samsung Floor Standing Heat PumpDocument1 pageSamsung Floor Standing Heat Pumpe-ComfortUSA100% (1)
- 110 WS Gas Stoichiometry KeyDocument2 pages110 WS Gas Stoichiometry Keyエルミタ ジョイ ファティマ100% (1)
- FlotacionDocument2 pagesFlotacionJose Ariel TorrezNo ratings yet
- Introduction To Surface EngineeringDocument31 pagesIntroduction To Surface Engineeringlogeshboy007No ratings yet
- Steam TurbinesDocument38 pagesSteam Turbinesmanoj100% (1)
- Profile Sections and Molded Parts Made From Elastomers (EPDM) in The Body AreaDocument13 pagesProfile Sections and Molded Parts Made From Elastomers (EPDM) in The Body AreaNagarajan DS100% (1)
- Classification of DyeDocument6 pagesClassification of DyeSalahuddin SaikotNo ratings yet
- Por Si Te Puede ServirDocument7 pagesPor Si Te Puede ServirJordi ClaudioNo ratings yet
- Chapter 6 Thermodynamics: The First Law: Systems, States, and Energy (Sections 6.1-6.8)Document12 pagesChapter 6 Thermodynamics: The First Law: Systems, States, and Energy (Sections 6.1-6.8)MostafaRock100% (2)
- Barbicide MsdsDocument3 pagesBarbicide MsdstudorcerneaNo ratings yet
- Welding Procedure Specification (WPS) : JointsDocument2 pagesWelding Procedure Specification (WPS) : JointsNavanitheeshwaran SivasubramaniyamNo ratings yet
- Flojetpump HandleidingDocument4 pagesFlojetpump HandleidingnitroboozterNo ratings yet
- Arthrex Starfish ™ Scope Rotation Attachment Insert Manual: 950-0036-01 Revision 0 08/2020Document36 pagesArthrex Starfish ™ Scope Rotation Attachment Insert Manual: 950-0036-01 Revision 0 08/2020eliaNo ratings yet
- 2013v12 New Guide PDFDocument4 pages2013v12 New Guide PDFlucianolimapgecivNo ratings yet
- TP7 TP8manualDocument10 pagesTP7 TP8manualJuanita Ariza BernalNo ratings yet
- Vacuum Testing of Fixed Roof Welded Storage Tanks As Per API 650,620Document7 pagesVacuum Testing of Fixed Roof Welded Storage Tanks As Per API 650,620Rakesh RanjanNo ratings yet
- SK HazraDocument18 pagesSK HazraDr Sunipa RoyNo ratings yet
- From Cellulosomes To Cellulosomics: THE Chemical RecordDocument14 pagesFrom Cellulosomes To Cellulosomics: THE Chemical RecordsajjalNo ratings yet