Professional Documents
Culture Documents
PRF
Uploaded by
Omar DarwishCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PRF
Uploaded by
Omar DarwishCopyright:
Available Formats
1952 In France. Diploma: Medecine 1979. Study of Management of Pain 1986. Private Pain therapy Center.
Platelet Rich Plasma ( PRP ) 1st Generation
Platelet Rich Fibrin ( PRF ) 2nd Generation
Are used for acceleration of Soft and Hard tissue healing.
Reconstructive Dental Surgeons are constantly looking for :
Bone morphogenetic protein-2 (BMP-2). Recombinant platelet derived growth factor. Platelet rich plasma ( PRP ). Plasma rich in growth factors (PRGF).
I dont know And this Presentation will not provide the answer. But it will serve to introduce :
Is blood plasma that has been enriched with platelets. contains several different growth factors and other cytokines. Made by mixing platelets and fibrinogen centrifuged from whole blood with thrombin and calcium chloride.
(PRP) was proposed as a method of introducing concentrated of platelets & growth factors to the surgical site.
Enriching the natural blood clot in order to accelerate wound healing and stimulate bone regeneration
(PRP has been used in conjunction with different grafting materials in bone augmentation procedures.
To date, the results from these studies are controversial and no conclusions can be drawn regarding the bone regenerative effect of PRP
Pre-implant reconstruction of the deficient alveolar ridge Predictable bone regeneration is dependent upon 4 major biologic principles:
Primary wound closure
Blood supply
Space maintenan ce
Wound stability
Blood supply
Blood supply provides the necessary cells, growth factors, and inhibitors to initiate the osteogenic biomineralization cascade. Injury to blood vessels during oral surgical procedures causes blood extravasation, subsequent platelet aggregation, and fibrin clot formation.
Hemostasis. Provides a matrix for the migration of fibroblasts and endothelial cells that involved in :
Angiogenesis and responsible for remodeling of new tissue.
PRF production protocol attempts to accumulate platelets and released cytokines in a fibrin clot.
How?
9ml blood is drawn into the tubes without anticoagulant and is immediately centrifuged.
Within a few minutes, the absence of anticoagulant allows activation of the majority of platelets contained in the sample to trigger a coagulation cascade.
Fibrinogen
Thrombin
Fibrin Network.
The result is a fibrin clot containing the platelets located in middle of the tube, just between the red blood cell layer at the bottom and acellular plasma at the top.
Pliers are inserted into the tube to gently grab the fibrin clot with attached RBCs.
Fibrin clots are transferred to sterile metal surface and RBCs are gently scraped away and discarded.
PRF is placed on the grid in the PRF Box
PRF Box is used to create PRF membranes. Serum exudate collects in the bottom of the box beneath the grid.
We
have :
Nine sinus floor augmentations
( Test Group ) 6 sinuses receiving PRF + FDBA particles.
( controlled Group ) 3 sinuses receiving FDBA without PRF.
( After 4 M )
( After 8 M )
(Test Group) After 4 M
Histologic maturation
Identicat =
(Controlled G) After 8 M with the quantities of newly formed bone equivalent between the two protocols.
The use of PRF in combination with FDBA to perform sinus floor augmentation seemed to : Accelerate bone regeneration Accelerating the healing of the soft tissues. Protect and stabilize the graft materials Act as fibrin bandages. Facilitating the rapid closure of the incision.
Reconstructive Dental Surgeons are constantly looking for :
PRF fragments were mixed with the graft particles functioning as a biological connector between the different elements of the graft, and as a matrix which favors neo-angiogenesis: High degree of gingival maturation after healing. Reduce postoperative pain and edema. limited even minor infectious phenomena.
protecting extraction sites:
inserted into residual extraction defects to accelerate soft tissue healing in site preservation procedures permitting ideal prosthetic implant placement.
The intrinsic incorporation of cytokines within the fibrin mesh allows for their progressive release over time (7-11 days), as the network of fibrin disintegrates. PRF membrane acts as fibrin bandage, serving as a matrix to accelerate the healing of wond edges. It also provides a significant postoperative protection of the surgical site and seems to accelerate the integration and remodeling of the grafted biomaterial.
PRF improves: Early wound closure, maturation of bone grafts, final esthetic result of the peri-implant and periodontal soft tissues. Additional reports are forthcoming, highlighting the many clinical applications and healing benefits of this second generation platelet concentrate
Awad Bin Hatem
Adam Mohamed
Ryham el Sadeq
Omar Darwish
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Diversity and InclusionDocument23 pagesDiversity and InclusionJasper Andrew Adjarani80% (5)
- Unit 11 LeadershipDocument4 pagesUnit 11 LeadershipMarijana DragašNo ratings yet
- Class 11 English Snapshots Chapter 1Document2 pagesClass 11 English Snapshots Chapter 1Harsh彡Eagle彡No ratings yet
- One Shot To The HeadDocument157 pagesOne Shot To The HeadEdison ChingNo ratings yet
- Multiple Choice Test - 66253Document2 pagesMultiple Choice Test - 66253mvjNo ratings yet
- A Study of Outdoor Interactional Spaces in High-Rise HousingDocument13 pagesA Study of Outdoor Interactional Spaces in High-Rise HousingRekha TanpureNo ratings yet
- Giles. Saint Bede, The Complete Works of Venerable Bede. 1843. Vol. 8.Document471 pagesGiles. Saint Bede, The Complete Works of Venerable Bede. 1843. Vol. 8.Patrologia Latina, Graeca et Orientalis100% (1)
- Q2 SHS Intro To World Religion - Module 2Document19 pagesQ2 SHS Intro To World Religion - Module 2jan roiNo ratings yet
- Williams-In Excess of EpistemologyDocument19 pagesWilliams-In Excess of EpistemologyJesúsNo ratings yet
- Modul Kls XI Sem IDocument6 pagesModul Kls XI Sem IAnonymous WgvOpI0CNo ratings yet
- 02 Cost of Capital QBDocument26 pages02 Cost of Capital QBAbhi JayakumarNo ratings yet
- Cartha Worth SharingDocument27 pagesCartha Worth SharingtereAC85No ratings yet
- English Vocabulary For MedicineDocument5 pagesEnglish Vocabulary For MedicineDentistryuv 2020100% (1)
- Malouf Explores Complex Nature of IdentityDocument1 pageMalouf Explores Complex Nature of Identitymanoriii0% (1)
- Assalamu'alaikum WR WB.: Emcee Script (1) Pre - AnnouncementDocument3 pagesAssalamu'alaikum WR WB.: Emcee Script (1) Pre - AnnouncementGian AlfaNo ratings yet
- BRM 6Document48 pagesBRM 6Tanu GuptaNo ratings yet
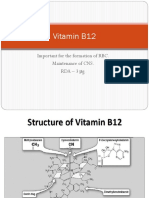
- Vitamin B12: Essential for RBC Formation and CNS MaintenanceDocument19 pagesVitamin B12: Essential for RBC Formation and CNS MaintenanceHari PrasathNo ratings yet
- Course Outline IST110Document4 pagesCourse Outline IST110zaotrNo ratings yet
- So Neither or NorDocument2 pagesSo Neither or NorMita KusniasariNo ratings yet
- Detailed Lesson Plan in Science 10Document7 pagesDetailed Lesson Plan in Science 10Glen MillarNo ratings yet
- The ADDIE Instructional Design ModelDocument2 pagesThe ADDIE Instructional Design ModelChristopher Pappas100% (1)
- Basic Musicianship ChecklistDocument1 pageBasic Musicianship ChecklistStefanie MeijerNo ratings yet
- HexaflexDocument10 pagesHexaflexCharlie Williams100% (1)
- ProbabilityDocument2 pagesProbabilityMickey WongNo ratings yet
- Digoxin FABDocument6 pagesDigoxin FABqwer22No ratings yet
- Asian Paints Research ProposalDocument1 pageAsian Paints Research ProposalYASH JOHRI-DM 21DM222No ratings yet
- PbisDocument36 pagesPbisapi-257903405No ratings yet
- Module 1 Ba Core 11 LessonsDocument37 pagesModule 1 Ba Core 11 LessonsLolita AlbaNo ratings yet
- Newton-Raphson MethodDocument32 pagesNewton-Raphson MethodnafisbadranNo ratings yet